Abstract
Background/Objective:
To determine whether a new upper extremity exercise device integrated with a video game (GameCycle) requires sufficient metabolic demand and effort to induce an aerobic training effect and to explore the feasibility of using this system as an exercise modality in an exercise intervention.
Design:
Pre-post intervention.
Setting:
University-based research facility.
Subject Population:
A referred sample of 8 adolescent subjects with spina bifida (4 girls, 15.5 ± 0.6 years; 4 boys, 17.5 ± 0.9 years) was recruited to participate in the project. All subjects had some level of mobility impairment that did not allow them to participate in mainstream sports available to their nondisabled peers. Five subjects used a wheelchair full time, one used a wheelchair occasionally, but walked with forearm crutches, and 2 were fully ambulatory, but had impaired gait.
Main Outcome Measures:
Peak oxygen uptake, maximum work output, aerobic endurance, peak heart rate, rating of perceived exertion, and user satisfaction.
Results:
Six of the 8 subjects were able to reach a Vo2 of at least 50% of their Vo2 reserve while using the GameCycle. Seven of the 8 subjects reached a heart rate of at least 50% of their heart rate reserve. One subject did not reach either 50% of Vo2 reserve or 50% of heart rate reserve. Seven of the 8 subjects increased their maximum work capability after training with the GameCycle at least 3 times per week for 16 weeks.
Conclusions:
The data suggest that the GameCycle seems to be adequate as an exercise device to improve oxygen uptake and maximum work capability in adolescents with lower extremity disability caused by spinal cord dysfunction. The subjects in this study reported that the video game component was enjoyable and provided a motivation to exercise.
Keywords: Upper extremity exercise, Aerobic training, Spinal cord dysfunction, Spina bifida, Paraparesis, Adolescents, Disability
INTRODUCTION
Spinal cord injury and congenital paraparesis caused by disorders such as spina bifida result in physical inactivity that is potentially costly in health and economic terms. When the ability to be physically active and mobile is compromised, independence is lost (1,2) and emotional well-being is reduced (3). Regular habitual activity is a missing component of the lives of most persons with disabilities (4). Coyle and Santiago concluded that physical inactivity was a major contributing factor in the deteriorating physical health of persons with disabilities (5). Other studies found that a sedentary lifestyle makes ambulation in a wheelchair a more stressful event when fitness levels are low (6–9). A primary goal of many medical treatments and rehabilitation programs for children and adolescents with disabilities is to restore patients' ability to be physically active.
Improvement in physical fitness through increased physical activity has been shown to be important for health maintenance and disease prevention. Improvement in cardiopulmonary endurance, body composition, muscle strength and endurance, and flexibility are associated with reductions of risk factors for various disease stages. Epidemiological studies in adults suggest that regular physical activity contributes to longevity and decreases the risk of death from a variety of causes (10–13). With respect to cardiovascular heart disease, inactivity has been shown to be the second most costly risk factor (14,15). Physical activity is associated most strongly with the prevention and control of coronary artery disease (16), hypertension (17,18) non–insulin-dependent diabetes mellitus, (19), osteoporosis (20,21), obesity (22), and mental health problems (23–28).
In recent years, the Centers for Disease Control and Prevention (29), the American College of Sports Medicine (ACSM) (30), the US Public Health Service (31), the National Institutes of Health (32), the US Department of Health and Human Service (2), and the American Heart Association (33) have all published recommendations for increased physical activity based on health concerns and minimum guidelines for exercise and activity. Recently, the ACSM pointed out that the quantity and quality of exercise needed to attain health-related benefits may differ from what is recommended for fitness benefits. Research now indicates that lower levels of physical activity (particularly with reference to intensity) confer significant health-related benefits to sedentary persons (30).
The most recent (June 1998) position statement by ACSM regarding the recommended quantity and quality of exercise represents the latest synthesis of research knowledge in this area (30). In comparison with the previous ACSM position statement released in 1990 (34), the current statement modifies the recommendations to accommodate sedentary individuals at low fitness levels. The ACSM position recommends the following minimum standards for aerobic exercise for sedentary individuals: (a) frequency of training: 3 d/wk; (b) duration of training: 20 minutes total, with minimum bouts of no less than 10 minutes; and (c) intensity of training: at least 50% of maximum oxygen uptake reserve (Vo2R) or 50% of maximum heart rate reserve (HRR). Many studies have correlated this intensity level with a Rating of Perceived Exertion (RPE) of 12 to 14 (30).
In 1999, Gater and Ugalde (35) reviewed several studies incorporating upper extremity aerobic exercise in individuals with paraplegia and tetraplegia. Although many of the studies found that various aerobic exercise protocols using arm crank ergometry, wheelchair ergometry, or wheeling on a track improved aerobic capacity, power output, or both, the most appropriate dosing for this population with regard to intensity, duration, and frequency remains unclear. However, based on their evaluation of the studies and in response to the 1995 Joint Centers for Disease Control/ACSM (36–38) recommendation that “every US adult should accumulate 30 minutes or more of moderate physical activity on most, preferably all, days of the week,” the authors suggested 20 to 60 minutes at an exercise intensity of about 12 to 13 (somewhat hard) on the Borg Rating of Perceived Exertion scale (RPE), preceded and followed by a 10-minute warm-up/cool-down. They go on to say that “the most important consideration in creating an exercise prescription is patient compliance (and) the most important factors in extended exercise compliance are that the activity be ‘enjoyable and employable’.”
Available options for aerobic exercise using only the upper body have significant limitations for populations with paraparesis and other mobility impairments. Hand cycles, for instance, are fairly large and expensive and can be used only in very specific locations (ie, a paved path with no automobile traffic, sharp turns, or steep hills). Weather is a consideration for individuals living in northern climates. Depending on the user's level of function, a user may require assistance to transfer in and out of the cycle, significantly impacting safety and independence. Tabletop arm ergometers are much smaller, cheaper, and require little assistance to access, but can be quite boring, decreasing compliance.
A new product available seeks to satisfy adolescents' need for enjoyment from exercise by integrating computer video game challenge and aerobic exercise. The GameCycle (Three Rivers Ltd, Mesa, AZ) combines the crank mechanism from a hand cycle with a commercially available game system (GameCube; Nintendo Co., Ltd, Kyoto, Japan) to play a car racing game (Need for Speed II; EA Games, Redwood City, CA). The user cranks the handles to control the speed of the car in the video game. Direction is controlled by tilting the crank handles, similar to steering a hand cycle. The crank resistance can be altered to increase the work required, and crank speed can be calibrated to increase the aerobic effort.
Preliminary experimental results using an early version of the GameCycle indicate that users can experience aerobic training effects with the GameCycle and find the product fun and motivating (39). Fitzgerald et al (39) tested and surveyed a select group of wheelchair athletes using the GameCycle with and without the video game. All participants believed that the GameCycle would help to motivate manual wheelchair users to exercise, and 77% of the participants stated that the GameCycle would aid in the frequency and motivation of their own exercise habits.
The purposes of this study were to (a) determine if the GameCycle requires sufficient effort, as outlined by the ACSM, to induce an aerobic training effect and (b) to assess the effectiveness, practicality, and satisfaction of the GameCycle as part of a 4-month, home-based exercise intervention for adolescents with lower extremity mobility impairments caused by spinal cord dysfunction.
METHODS
Subjects
Eight adolescent subjects with spina bifida (4 girls, 15.5 ± 0.6 years; 4 boys, 17.5 ± 0.9 years) were recruited from the Spina Bifida Clinic at Shriners Hospital for Children Northern California to participate in the project. All subjects had some level of mobility impairment that did not allow them to participate in mainstream sports available to their nondisabled peers. Five subjects used a wheelchair full time, 1 used a wheelchair for distances but walked with forearm crutches, and 2 were fully ambulatory, but had impaired gait. The study's protocol was approved by the institutional review board, and all subjects and/or a parent provided written assent and consent.
GameCycle
The GameCycle (Figure 1a and b) uses the same crank mechanism as used on many 3-wheeled exercise bikes as the controller for the video game. The user can sit in his/her own wheelchair or other chair, adjust the crank handles up or down, and increase or decrease the resistance. The forward and reverse crank speeds required to achieve maximum car speed in the game and the sensitivity of the steering can be set during a short calibration procedure. The game is played by cranking the handles forward to increase the speed of the car while steering is achieved by tilting the handles side-to-side.
Figure 1. a. The GameCycle device. b. A wheelchair user operates the GameCycle guided by the video screen.
Measurements
There are no prediction equations available that can be used to estimate values for peak oxygen uptake (Vo2peak) or anaerobic threshold (AT) in adolescents with disabilities using upper extremity exercise. Therefore, Vo2peak and AT were determined for each subject by a standard ramp protocol on a magnetically braked arm ergometer (Lode BV, Groningen, The Netherlands). AT is a useful tool in exercise prescription because it correlates strongly with an RPE of 12 to 13, which, in turn, meets the ACSM guidelines for the recommended intensity of exercise (40).
For the Vo2peak determination, subjects were asked to crank the arm ergometer at a constant speed of 70 rpm for 2 minutes at 0 W of resistance. The resistance was increased in a ramp fashion at a rate of 10 W/min. Subjects were verbally encouraged to continue until exhaustion. Heart rate (HR), oxygen uptake (Vo2), and carbon dioxide production (CO2) were recorded breath-by-breath with a metabolic cart (Medgraphics, St Paul, MN) using a facemask. RPE, using the Borg original scale of 6 to 20, was recorded at every minute (41). Additionally, the maximum power output was recorded.
After a rest period of 30 to 60 minutes, the subjects were required to crank the GameCycle (without the video game playing) at a constant rate of 70 rpm while HR, Vo2, and CO2 were recorded with the same metabolic system. The subjects were not measured during video game play because they were not well experienced with the game itself. Novice game players often get frustrated and need to stop and reverse as they learn the game, causing highly variable Vo2 and HR values. The subjects cranked for 1 minute at each of 10 levels of resistance (0–9) available on the GameCycle. Subjects were also asked to rate their RPE halfway through each minute. Data were averaged over each minute.
The HR and Vo2 values obtained from the GameCycle were compared with the highest oxygen uptake and heart rates obtained with the arm ergometer to determine at what resistance level, if at all, the subject showed a physiologic response to meet the ACSM guidelines previously described. Additionally, using the data from the arm crank ergometer, the HR and Vo2 values at the AT were calculated using the V-slope method (42). The GameCycle resistance level that elicited a response at or just below the anaerobic threshold values was determined for each subject and used as the starting point for the training regimen.
One of the difficulties in performing a valid Vo2peak test using an arm ergometer is the high probability of inducing local muscular fatigue before fully stressing the cardiorespiratory mechanism. This is caused mainly by the smaller muscle mass and smaller, more constrictive vascular bed in the upper extremities compared with the lower extremities used in running or cycling (43,44). To explore the contribution of arm strength to the changes in aerobic fitness, initial strength values were recorded. Peak dynamic strength values were obtained for each subject for concentric elbow flexion/extension using a LIDO Multi-Joint Dynamometer (Loredan Biomedical, Sacramento, CA). Subjects were asked to perform 3 maximal efforts for elbow flexion/extension in a supine position. Measurements were recorded in foot-pounds and averaged between right and left arms.
After completing the laboratory measurements, a GameCycle was delivered to each individual's home. Each subject was instructed on the proper adjustment and use of the GameCycle. The subjects were instructed to play the GameCycle at least 3 times per week, at least 20 minutes per session, for 16 weeks. Each subject was told to set the resistance at the level previously determined to be at or just below their anaerobic threshold. Subjects were encouraged to play the GameCycle as often as they wanted and to place the unit in a location accessible by all members of the family. This would help to motivate the subject by encouraging more family and friend interaction.
The subjects were provided with a HR monitor (Polar Electro, Vantaa, Finland) and instructed to wear it each time they played the GameCycle. The HR monitor (HRM) provided an immediate feedback to the subject during game play to assist them in maintaining the proper exercise intensity. Subjects were instructed to maintain their heart rate at their AT level. If they were unable to achieve that heart rate during game play, they were instructed to increase the resistance level. Also, if their HR consistently exceeded their target HR, they were instructed to reduce the resistance level.
The HRM also recorded the average HR every minute. The subjects brought the HRM to the laboratory every 2 weeks where the monitors were downloaded to a computer and examined to determine the amount of time the GameCycle was played and their average HR during each session. If their average HR was not near the target HR, they were instructed to adjust the GameCycle resistance level accordingly. In addition to the HRM, every 2 weeks, both the parents and the subjects were verbally queried regarding the number of sessions the subjects completed, the amount of time they exercised each session, the HR the subjects achieved during the sessions, and the resistance setting used on the GameCycle.
After completing the 16-week program, each subject returned to the laboratory and repeated all of the preintervention measurements. They also completed a 20-question subjective survey about their opinion of the GameCycle as an exercise modality. This was the same questionnaire used in Fitzgerald et al (39) and assessed an individual's perception of satisfaction and enjoyment while using the GameCycle. An additional 3 questions allowed the respondent to comment on likes, dislikes, and suggestions for improvements.
Statistical Analysis
A pre-post repeated-measures analysis (paired t-tests) was used to assess the maximum work that subjects were able to perform before and after the GameCycle intervention. Significance was accepted at P < 0.05. Pearson correlation coefficients were calculated for the relationship between initial arm strength and aerobic improvement.
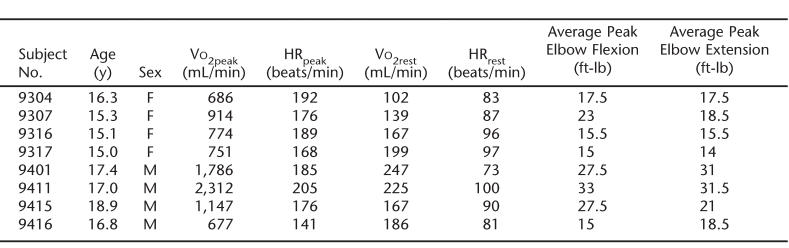
RESULTS
The values obtained for Vo2peak and peak HR (HRpeak) during the arm crank ergometry (ACE) were used as a proxy measures for Vo2max and HRmax because standards have not yet been established for predicting Vo2max or HRmax for adolescents with disabilities during arm crank ergometry (43,45). These values were used to calculate the percentage of heart rate reserve (%HRR) and oxygen uptake reserve (%Vo2R):
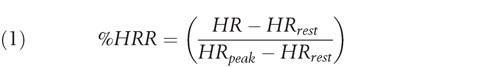 |
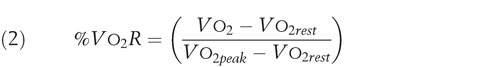 |
Once 50% of Vo2R was calculated for each subject, it was compared with the average Vo2 at each GameCycle resistance for that subject. The same was done for HRR and RPE.
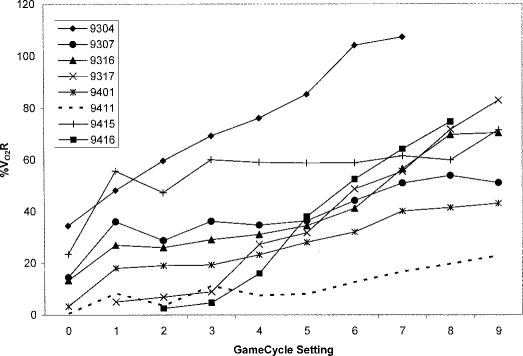
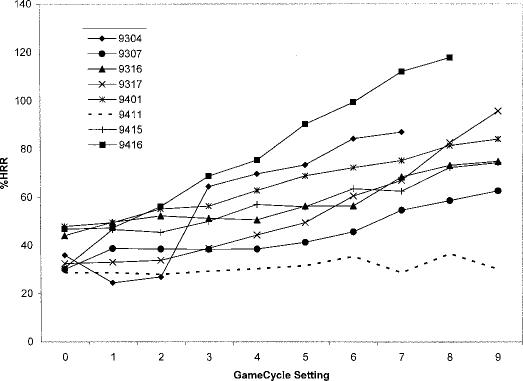
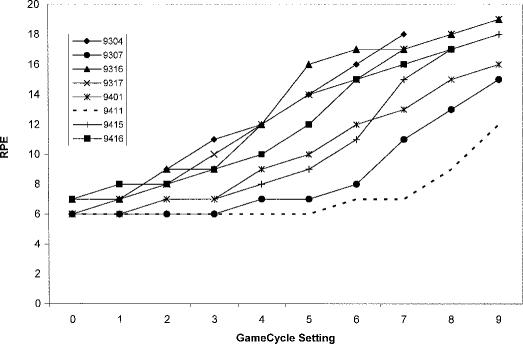
Before the 16-week home training program, 6 of the 8 subjects reached a Vo2 of at least 50% of their Vo2 reserve while cranking the GameCycle (Figure 2), the level recommended by the ACSM to be sufficient to induce a training effect. Seven of the 8 subjects reached a HR of at least 50% of their HRR (Figure 3). Only 1 subject did not reach the 50% level for either HRR or Vo2R. All subjects reached an RPE level of at least 12 (Figure 4).
Figure 2. Percent of oxygen uptake reserve at each GameCycle™ resistance setting.
Figure 3. Percent of heart rate reserve at each GameCycle™ resistance setting.
Figure 4. Rating of Perceived Exertion reported by the subjects at each GameCycle™ resistance setting.
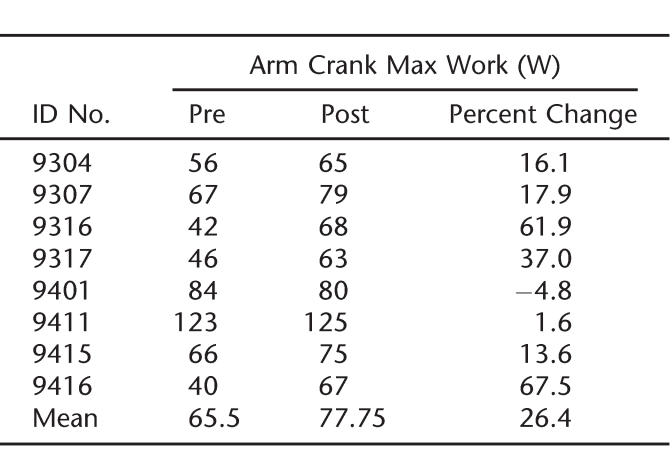
After completing the 16-week home-training program, 6 of the 8 subjects substantially increased the work they were able to achieve during the maximal arm crank ergometer test (Table 1) and the mean maximum work achieved by the group significantly increased from 65.5 ± 9.7 to 77.7 ± 7.1 W (P < 0.015). One individual only increased by 1.6%, and 1 subject showed a decrease of 4.8%. The 2 subjects who showed the least amount of improvement or no improvement had the highest initial values for strength and aerobic capacity during the pretest evaluation. Overall, the amount of aerobic improvement was inversely correlated (r = −0.60) with initial elbow flexion strength.
Table 1.
Change in Maximum Work Level Achieved During Maximal Arm Crank Ergometry Test
Analysis of the HR during the GameCycle monitoring was not feasible because of an excessive amount of missing data. Large amounts of data were missing because the subjects either forgot to put on the HRM when playing the GameCycle, did not start the recording correctly, or had technical problems from electromagnetic interference. Because of these difficulties, it was necessary to rely on the verbal reports of the subjects and their parents regarding HR targets and compliance.
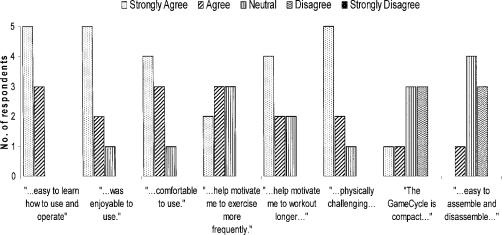
Most of the subjects reported that they completed the exercises as directed and were able to reach their target HR. All but one subject felt the GameCycle was physically challenging enough to reach their target training zone. Most subjects (69%) agreed that the GameCycle would help motivate them to exercise more often and for longer periods of time. Most of the negative responses were related to the size and weight of the GameCycle frame. Most of the subjects (92%) agreed that the GameCycle was easy to use, enjoyable, motivating, and comfortable (Figure 5).
Figure 5. Sample responses to GameCycle™ user satisfaction survey.
DISCUSSION
Most of the subjects were able to reach an intensity level sufficient to initiate an aerobic training effect as recommended by the ACSM. All 8 subjects achieved an RPE of at least 12. Some researchers indicate that video game playing alone evokes a physiologic heart rate response similar to low-intensity exercise (46–48). Segal and Dietz (47) determined that the energy cost of video game playing was similar to slow walking but concluded there was not sufficient cardiorespiratory stress to improve fitness. It is unknown whether this incremental HR effect, presumably induced by emotional factors, has any additive training effect to upper extremity exercise alone. However, Fitzgerald et al (39) tested subjects on the GameCycle with and without the video game playing and reported a significance increase in mean Vo2 when the subjects played the GameCycle with the video game playing. During play, many users will crank at speeds up to 100 rpm, suggesting that users may benefit aerobically at lower resistance levels. The 70-rpm speed during the GameCycle assessment was selected to compare the data from the arm crank ergometer test. However, most of the subjects found the speed uncomfortably slow when exercising and playing the video game on the GameCycle.
The 2 subjects who did not reach the ACSM guidelines for Vo2 had the highest baseline strength values (Table 2) and had well-developed shoulder, arm, and chest musculature. These individuals also had the lowest percent increases in maximum power output after 4 months of training. One of these 2 subjects also reported that the GameCycle was not physically challenging despite having the GameCycle set at the highest resistance level during the intervention. This illustrates a possible shortcoming of the GameCycle as an aerobic exercise modality for adults or adolescents with well-developed upper bodies. In these populations, a higher initial GameCycle setting and/or longer duration of exercise may enable them to experience greater aerobic training effects. Further exploration in faster crank speeds is needed, as well as energy consumption during actual game play. In contrast, those individuals with weaker initial strength values and lower cardiorespiratory fitness measurements exhibited a steeper increase in HR and Vo2 with increasing resistance levels and showed a greater improvement in maximum power output on the arm crank ergometer over 16 weeks of training. This is a common phenomenon seen in many exercise intervention studies (ie, those subjects with the lowest initial fitness measures show the greatest initial improvement over baseline).
Table 2.
Vo2, HR, and Strength Values
A weakness of this project was the use of self- and parent-report data to measure compliance instead of an objective, quantitative method such as HR monitoring. Future studies should explore more dependable methods of gathering objective quantitative information on usage such as data recorders incorporated into or attached to the GameCycle. Monitoring compliance in any home-based exercise program is problematic, which leads many investigators to design interventions that require subjects to attend exercise sessions at a laboratory or facility. This is especially difficult with an adolescent population with disabilities because many of them may not have the ability to get to the testing center consistently.
CONCLUSION
The subjects, as a group, showed a significant improvement in maximal power output on the arm crank ergometry test. Various other studies have also shown benefits from upper body training regimens on individuals with lower extremity paraparesis (49–52). None of these studies, however, were performed with adolescents. The improvements seen in this study, along with the positive association of enjoyment from playing the video game, have potential for motivating the subjects to maintain a habit of physical activity that could contribute to health benefits if this form of exercise was combined with other fitness measures, such as nutrition interventions, documented to improve health.
Although the size of the subject group was small, and compliance was ascertained by self-report and parent-report, which limit the conclusions taken from these data, these preliminary results show excellent promise for the GameCycle as a viable exercise alternative to the limited options available to adolescents with mobility impairment. Currently, the GameCycle is not widely available and is cost-prohibitive for many families. As with most technology, costs and availability may improve rapidly over time. The GameCycle has other benefits beyond an exercise modality. It is entertaining and can be used by all family members (with additional ports for competitive gaming). Thus, there may be benefits in terms of increased socialization and reduced isolation. Future studies should include subjects groups with greater numbers and diversity.
Further development work should explore various crank speeds on oxygen uptake cost (especially for stronger individuals), additional games to add variety, additional capabilities such as HR display for feedback regarding exercise intensity to participants, the possibility of internet competition, as well as options for increasing the resistance beyond the current settings. An additional feature that would be helpful for researchers is a quantitative monitoring system that does not require user input. Finally, fitness intervention programs for younger disabled populations may want to incorporate home or community use of the GameCycle as an exercise intervention to complement nutrition interventions, counseling, and promotion of family involvement.
Acknowledgments
The GameCycle was developed by Three Rivers Ltd., Mesa, AZ, with support from National Institutes of Health Grant HD3935-02A1.
Footnotes
This study was supported by Grant 8600 from Shriners Hospitals for Children.
REFERENCES
- Asher M, Olson J. Factors affecting the ambulatory status of patients with spina bifida cystica. J Bone Joint Surg Am. 1983;65:350–356. [PubMed] [Google Scholar]
- Gettman LR. Economic benefits of physical activity. President's Council on Physical Fitness and Sports Research Digest. 1996. Available at: http://www.fitness.gov/economic.pdf. Accessed July 19, 2006. [PMC free article] [PubMed]
- Lezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility difficulties are not only a problem of old age. J Gen Intern Med. 2001;16:235–243. doi: 10.1046/j.1525-1497.2001.016004235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DR, Yore MM, Ham SA, Macera CA. Physical activity among adults :50 yr with and without disabilities, BRFSS 2001. Med Sci Sports Exerc. 2005;37:620–629. doi: 10.1249/01.mss.0000158189.17546.ed. [DOI] [PubMed] [Google Scholar]
- Coyle CP, Santiago MC. Aerobic exercise training and depressive symptomatology in adults with physical disabilities. Arch Phys Med Rehabil. 1995;76:647–652. doi: 10.1016/s0003-9993(95)80634-2. [DOI] [PubMed] [Google Scholar]
- McDonald CM, Widman LW, Walsh SA, Page P, Abresch RT. Energy cost of wheelchair locomotion in thoracic and lumbar myelomeningocele and spinal cord injury—impact of diagnosis, gender, and body composition. Dev Med Child Neurol. 2001;43:8. Abstract. [Google Scholar]
- McDonald CM, Walsh SA, Widman LW, Walsh D, Abresch RT. Assessment of energy cost under various modes of locomotion in children with spinal cord injuries and able-bodied controls [abstract] Gait Posture. 2001;13:289. [Google Scholar]
- Garrel DR, Jobin N, de Jonge LH. Should we still use the Harris and Benedict equations? Nutr Clin Pract. 1996;11:99–103. doi: 10.1177/011542659601100399. [DOI] [PubMed] [Google Scholar]
- Kocina P. Body composition of spinal cord injured adults. Sports Med. 1997;23:48–60. doi: 10.2165/00007256-199723010-00005. [DOI] [PubMed] [Google Scholar]
- Leon AS, Connett J, Jacobs DR, Jr, Rauramaa R. Leisure-time physical activity levels and risk of coronary heart disease and death. The Multiple Risk Factor Intervention Trial. JAMA. 1987;258:2388–2395. [PubMed] [Google Scholar]
- Paffenbarger RS, Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Popkin BM. Longitudinal physical activity and sedentary behavior trends: adolescence to adulthood. Am J Prev Med. 2004;27:277–283. doi: 10.1016/j.amepre.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Activity and Health Research. Allied Dunbar National Fitness Survey. London: Health Education Authority/Sports Council; 1992. [Google Scholar]
- Hahn RA, Teutsch SM, Rothenberg RB, Marks JS. Excess deaths from nine chronic diseases in the United States, 1986. JAMA. 1990;264:2654–2659. [PubMed] [Google Scholar]
- Roberts CK, Barnard RJ. Effects of exercise and diet on chronic disease. J Appl Physiol. 2005;98:3–30. doi: 10.1152/japplphysiol.00852.2004. [DOI] [PubMed] [Google Scholar]
- Powell KE, Thompson PD, Caspersen CJ, Kendrick JS. Physical activity and the incidence of coronary heart disease. Ann Rev Public Health. 1987;8:253–287. doi: 10.1146/annurev.pu.08.050187.001345. [DOI] [PubMed] [Google Scholar]
- Blair SN, Goodyear NN, Gibbons LW, Cooper KH. Physical fitness and incidence of hypertension in healthy normo-tensive men and women. JAMA. 1984;252:487–490. [PubMed] [Google Scholar]
- Paffenbarger RS, Jr, Wing AL, Hyde RT, Jung DL. Physical activity and incidence of hypertension in college alumni. Am J Epidemiol. 1983;117:245–257. doi: 10.1093/oxfordjournals.aje.a113537. [DOI] [PubMed] [Google Scholar]
- Taylor R, Ram P, Zimmet P, Raper LR, Ringrose H. Physical activity and prevalence of diabetes in Melanesian and Indian men in Fiji. Diabetologia. 1984;27:578–582. doi: 10.1007/BF00276971. [DOI] [PubMed] [Google Scholar]
- Dalen N, Olsson KE. Bone mineral content and physical activity. Acta Orthop Scand. 1974;45:170–174. doi: 10.3109/17453677408989136. [DOI] [PubMed] [Google Scholar]
- Recker RR, Davies KM, Hinders SM, Heaney RP, Stegman MR, Kimmel DB. Bone gain in young adult women. JAMA. 1992;268:2403–2408. [PubMed] [Google Scholar]
- Thompson JK, Jarvie GJ, Lahey BB, Cureton KJ. Exercise and obesity: etiology, physiology, and intervention. Psychol Bull. 1982;91:55–79. [PubMed] [Google Scholar]
- Brown DR, Wang Y. The relationships among exercise training, aerobic capacity, and psychological well-being in the general population. Med Exerc Nutr Health. 1992;1:125–142. [Google Scholar]
- Folkins CH, Sime WE. Physical fitness training and mental health. Am Psychol. 1981;36:373–389. doi: 10.1037//0003-066x.36.4.373. [DOI] [PubMed] [Google Scholar]
- Spungen AM, Bauman WA, Wang J, Pierson RN., Jr. Measurement of body fat in individuals with tetraplegia: a comparison of eight clinical methods. Paraplegia. 1995;33:402–408. doi: 10.1038/sc.1995.90. [DOI] [PubMed] [Google Scholar]
- Sallis JF. Epidemiology of physical activity and fitness in children and adolescents. Crit Rev Food Sci Nutr. 1993;33:403–408. doi: 10.1080/10408399309527639. [DOI] [PubMed] [Google Scholar]
- Janz KF, Witt J, Mahoney LT. The stability of children's physical activity as measured by accelerometry and self-report. Med Sci Sports Exerc. 1995;27:1326–1332. [PubMed] [Google Scholar]
- Trost SG, Pate RR, Freedson PS, Sallis JF, Taylor WC. Using objective physical activity measures with youth: how many days of monitoring are needed? Med Sci Sports Exerc. 2000;32:426–431. doi: 10.1097/00005768-200002000-00025. [DOI] [PubMed] [Google Scholar]
- Pate RR, Pratt M, Blair SN et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. Position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;6:975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Healthy People 2000 Final Review. Hyattsville, Maryland: Public Health Service; 2001. Library of Congress Catalog Card Number 76-641496. [Google Scholar]
- NIH Consensus Development Program. Physical activity and cardiovascular health. NIH Consensus Statement. 1995;13:1–33. [PubMed] [Google Scholar]
- Fletcher GF, Balady G, Blair SN et al. Statement on exercise: benefits and recommendations for physical activity programs for all Americans. A statement for health professionals by the Committee on Exercise and Cardiac Rehabilitation of the Council on Clinical Cardiology, American Heart Association. Circulation. 1996;94:857–862. doi: 10.1161/01.cir.94.4.857. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. Position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness in healthy adults. Med Sci Sports Exerc. 1990;22:265–274. [PubMed] [Google Scholar]
- Jacobs PL, Nash MS, Rusinowski JW. Circuit training provides cardiorespiratory and strength benefits in persons with paraplegia. Med Sci Sports Exerc. 2001;33:711–717. doi: 10.1097/00005768-200105000-00005. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Guidelines for school and community programs to promote lifelong physical activity among young people. MMWR Recomm Rep. 1997;46:1–36. [PubMed] [Google Scholar]
- American College of Sports Medicine. Guidelines for Graded Exercise Testing and Exercise Prescription. Philadelphia, PA: Lea & Febiger; 1995. [Google Scholar]
- Roetert EP, Piorkowski PA, Woods RB, Brown SW. Establishing percentiles for junior tennis players based on physical fitness testing results. Clin Sports Med. 1995;14:1–21. [PubMed] [Google Scholar]
- Fitzgerald SG, Cooper RA, Thorman T, Cooper R, Guo S, Boninger ML. The GAME(Cycle) exercise system: comparison with standard ergometry. J Spinal Cord Med. 2004;27:453–459. doi: 10.1080/10790268.2004.11752237. [DOI] [PubMed] [Google Scholar]
- Spungen AM, Wang J, Pierson RN, Jr, Bauman WA. Soft tissue body composition differences in monozygotic twins discordant for spinal cord injury. J Appl Physiol. 2000;88:1310–1315. doi: 10.1152/jappl.2000.88.4.1310. [DOI] [PubMed] [Google Scholar]
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- Wasserman K, Hansen JE, Sue DY, Casaburi R, Whipp BJ. Principles of Exercise Testing and Interpretation. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- Cerny FJ, Ucer C. Arm work interferes with normal ventilation. Appl Ergon. 2004;35:411–415. doi: 10.1016/j.apergo.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Balady GJ, Weiner DA, McCabe CH, Ryan TJ. Value of arm exercise testing in detecting coronary artery disease. Am J Cardiol. 1985;55:37–39. doi: 10.1016/0002-9149(85)90295-4. [DOI] [PubMed] [Google Scholar]
- Martin TW, Zeballos RJ, Weisman IM. Gas exchange during maximal upper extremity exercise. Chest. 1991;99:420–425. doi: 10.1378/chest.99.2.420. [DOI] [PubMed] [Google Scholar]
- Emes CE. Is Mr Pac Man eating our children? A review of the effect of video games on children. Can J Psychiatry. 1997;42:409–414. doi: 10.1177/070674379704200408. [DOI] [PubMed] [Google Scholar]
- Segal KR, Dietz WH. Physiologic responses to playing a video game. Am J Dis Child. 1991;145:1034–1036. doi: 10.1001/archpedi.1991.02160090086030. [DOI] [PubMed] [Google Scholar]
- O'Connor TJ, Fitzgerald SG, Cooper RA, Thorman TA, Boninger ML. Does computer game play aid in motivation of exercise and increase metabolic activity during wheelchair ergometry? Med Eng Phys. 2001;23:267–273. doi: 10.1016/s1350-4533(01)00046-7. [DOI] [PubMed] [Google Scholar]
- Cooney MM, Walker JB. Hydraulic resistance exercise benefits cardiovascular fitness of spinal cord injured. Med Sci Sports Exerc. 1986;18:522–525. [PubMed] [Google Scholar]
- Gass GC, Watson J, Camp EM, Court HJ, McPherson LM, Redhead P. The effects of physical training on high level spinal lesion patients. Scand J Rehabil Med. 1980;12:61–65. [PubMed] [Google Scholar]
- Hooker SP, Wells CL. Effects of low- and moderate-intensity training in spinal cord-injured persons. Med Sci Sports Exerc. 1989;21:18–22. doi: 10.1249/00005768-198902000-00004. [DOI] [PubMed] [Google Scholar]
- Keyser RE, Rasch EK, Finley M, Rodgers MM. Improved upper-body endurance following a 12-week home exercise program for manual wheelchair users. J Rehabil Res Dev. 2003;40:501–510. doi: 10.1682/jrrd.2003.11.0501. [DOI] [PubMed] [Google Scholar]