Abstract
Background
Children who report episodes of binge eating gain more weight than do children not reporting binge eating. However, how binge eating affects children’s food intake at meals is unknown.
Objective
We compared the energy intake and postmeal satiety of children with and without a history of binge eating during buffet meals.
Design
Sixty overweight children aged 6–12 y were categorized into those reporting past binge-eating episodes (n = 10) and those reporting no such episodes (n = 50). Children selected lunch twice from a multiple-item, 9835 kcal, buffet meal: after an overnight fast and after a standardized breakfast. Children ate ad libitum, until they reported they were full. The main outcome measures were energy intake during meals and duration of postmeal satiety, after adjustment for covariates, including age, race, sex, socioeconomic status, and body composition.
Results
After the overnight fast, children in the binge-eating group consumed more energy [x̄ (±SD): 1748 ± 581 compared with 1309 ± 595 kcal; P = 0.04] and exhibited a shorter satiety duration (194 ± 84 compared with 262 ± 89 min; P = 0.03) than did children in the non-binge-eating group. After the standardized breakfast, binge-eating children reported a shorter satiety duration (75 ± 62 compared with 132 ± 62 min; P = 0.01) and consumed more energy at the postbreakfast meal (1874 ± 560 compared with 1275 ± 566 kcal; P = 0.004).
Conclusion
The ability to consume large quantities of palatable foods, coupled with decreased subsequent satiety, may play a role in the greater weight gain found in binge-eating children.
Keywords: Child, obesity, binge eating, energy intake, satiety, satiation, eating behavior
INTRODUCTION
Overweight children who seek weight-loss treatment commonly report episodes of binge eating, during which they consume large amounts of food and experience loss of control over their eating. Between 10% and 30% of overweight children who have a body mass index (BMI; in kg/m2) ≥ 95th percentile for age and sex (1) describe ≥1 episode of binge eating in a period of 6 mo (2–4), even though few meet the diagnostic frequency criterion for binge-eating disorder (binge eating ≥2 times/wk) (5). Adults (6) and children (3, 7, 8) who report binge eating or loss of control over eating were found to be heavier and to have greater adiposity than those who deny such behaviors. When followed prospectively, children and adolescents with binge-eating episodes were also shown to gain more weight (9–11) and fat mass (12) than did children who do not binge eat, which suggests that binge eating may be a factor that contributes to the development of overweight during childhood.
Children who have problems with binge eating report high scores on measures of disinhibited eating (eating in response to cognitive, environmental, and affective stimuli) (2), which suggests that they are disproportionately affected by external food cues, such as the sight and smell of food. Children who report binge eating may therefore be expected to overeat to an even greater extent than children who do not binge eat when offered free access to large quantities of palatable foods, as is commonly the case at restaurant buffet meals. Some studies also suggest obese adults with binge-eating disorder have larger gastric capacities (13) and lesser nociperception (14) than do obese adults without binge-eating disorder and thus may have an impaired ability to sense fullness. We therefore examined the energy intake and satiety duration of overweight children during lunch-time meals. We hypothesized that children who report binge eating would consume more energy when offered large quantities of palatable foods than would similarly overweight children who reported no binge-eating episodes. We further hypothesized that, compared with children who do not binge eat, children who report binge eating would become hungry more rapidly after eating to the point of satiation.
SUBJECTS AND METHODS
Participants
A convenience sample of overweight children aged 6–12 y was recruited through newspaper advertisements and letters mailed to local family physicians and pediatricians for a weight-loss study that examined the effects of metformin hydrochloride (15). Children were eligible if they had a BMI ≥95th percentile for age and sex (1) and were healthy other than having evidence of insulin resistance (fasting insulin ≥15 μU/L). Binge eating was not mentioned in any advertisement. Participants were studied before they started weight-reduction treatment. All participants were given written and oral explanations of the purposes, procedures, and potential risks of the study. Each child provided written assent, and parents gave written consent for their participation. The present study was approved by the National Institutes of Child Health and Human Development Institutional Review Board. Data were collected between October 2000 and September 2005.
Procedures
The participants were admitted for a 3-d inpatient stay during which each participant ate from a standardized lunch buffet twice, 2 d apart. Weight and height were measured as described previously (16) with the use of calibrated electronic instruments. BMI was calculated. BMI SD scores (BMI z scores) were calculated according to the Centers for Disease Control and Prevention 2000 growth charts (1). Body composition was measured as previously described (16, 17) with the use of air-displacement plethysmography (Life Measurement Inc, Concord, CA) to determine fat-free mass and body fat mass.
To assess binge eating, each child completed the Questionnaire of Eating and Weight Patterns–Adolescent Version (QEWP-A) (18). The QEWP-A has been used with children as young as 6 y (19–21) and has adequate concurrent validity when correlated with measures of abnormal eating attitudes (18) as well as acceptable test-retest reliability (22). On the basis of their responses to the QEWP-A, children were categorized into 2 eating behavior groups for analysis: those who reported binge-eating episodes (overeating with loss of control) within the past 6 mo and those with no reported binge-eating episodes. The participants also completed the Three-Factor Eating Inventory (23), a 51-item questionnaire designed to measure 3 dimensions of human eating behavior: cognitive restraint, disinhibition, and hunger. To ensure that the participants found foods offered on the buffet acceptable, participants completed a food-preference questionnaire that used a 10-point Likert scale (24) to rate how much they liked 57 foods children commonly consume (25), which included the foods offered on the buffet.
Lunchtime buffet meals
The participants were asked to select their lunch from a multiple-item buffet meal on 2 occasions during their 3-d inpatient admission. Energy offered at all other meals between the 2 buffet meal studies was selected by a registered dietitian to maintain current body weight. On the first day, the participants were offered the buffet meal at 1130 after an overnight fast (the post-fast meal). Two days later, children were offered the buffet meal, which was given at 0930 (the postbreakfast meal), after they had ingested a standardized breakfast shake meal (Scandishake; Ax-can Pharma Inc, Birmingham, AL; 787 kcal, 52% carbohydrates, 11% protein, 37% fat).
The buffet meals offered a variety of foods children commonly eat that differed greatly in macronutrient composition (Figure 1); together, the foods supplied 9835 kcal for ingestion (Table 1), which is substantially more than any child would be likely to consume during one meal. Children were tested individually. When each child entered the room that contained the buffet, the following instruction was read aloud verbatim: “Please let yourself go and eat as much as you would like. You may eat as much of anything as you would like to, but you do not have to eat anything that you do not like.” The participants were then left alone in the room that contained the buffet to eat ad libitum. Time spent eating was measured with the use of a stopwatch. The amount of food consumed was calculated by using the differences in weight of each food item before and after the meal. The nutrient composition for each food was determined according to information from PRONUTRA 3.1 (Viocare Technologies Inc, Princeton, NJ), a metabolic diet study management system that uses the US Department of Agriculture Nutrient Database for Standard Reference (Release 16). Immediately before and, again, after eating, children were asked to rate their hunger, fullness, and desire to eat (26). For prompts pertaining to hunger and fullness, each participant was asked to place marks on a visual analog scale that ranged from “not at all” to “extremely.” Children indicated how much more food they felt they could eat on a visual analog scale that ranged from “a very small amount” to “a very large amount.” These questionnaires were completed in a room devoid of food or food-containing images.
FIGURE 1.
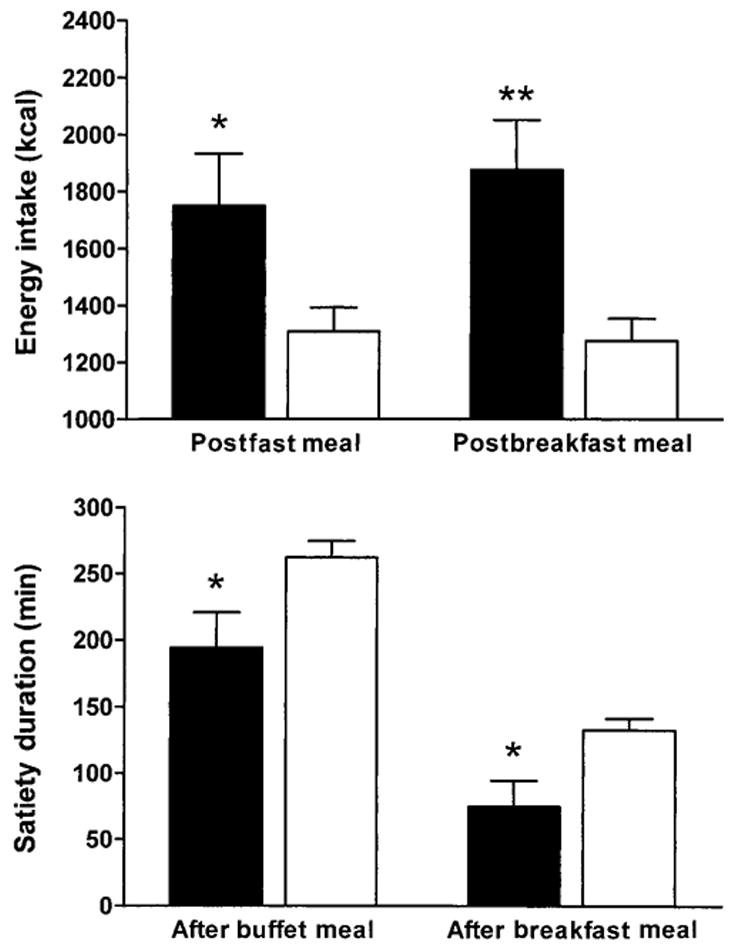
Adjusted mean (±SEM) for energy intake and satiety duration in children who reported binge-eating episodes (■; n = 10) and children who reported no binge-eating episodes (□; n = 50). *,**Significantly different from children with no binge-eating episodes (analysis of covariance for main effect of binge-eating status on mean energy intake or satiety duration): *P < 0.05, **P < 0.01.
TABLE 1.
Energy of meal items presented at the buffet meals1
| Item | Energy |
|---|---|
| kcal | |
| 12 Slices white bread | 801.0 |
| 180 g Ham | 216.0 |
| 180 g Turkey | 282.6 |
| 240 g American cheese | 901.1 |
| 200 g Chicken nuggets | 550.8 |
| 120 g Peanut butter | 711.6 |
| 120 g Grape jelly | 339.6 |
| 200 g Tomatoes | 42.0 |
| 50 g Lettuce | 6.0 |
| 3 Medium bananas | 325.7 |
| 250 g Grapes | 177.5 |
| 3 Medium oranges | 184.7 |
| 12 Oreo cookies2 | 566.4 |
| 12 Vanilla wafer cookies | 206.3 |
| 90 g Mayonnaise | 645.1 |
| 90 g Mustard | 59.4 |
| 90 g Light ranch dressing | 240.0 |
| 90 g Barbeque sauce | 67.5 |
| 250 g Mild salsa | 70.0 |
| 200 g Baby carrots | 76.0 |
| 120 g Tortilla chips | 601.2 |
| 150 g Pretzels | 571.5 |
| 120 g Jellybeans | 440.4 |
| 120 g M & M’s candy3 | 590.4 |
| 850 g Bottled water | 0.0 |
| 850 g 2% Milk | 422.2 |
| 850 g Apple juice | 400.0 |
| 850 g Lemonade | 340.0 |
The total energy content was 9835 kcal.
Kraft Foods, Northfield, IL.
Mars, Inc, Masterfood USA, Hackettstown, NJ.
After the postfast and the postbreakfast meals, satiety duration (time between cessation of eating and onset of hunger) was recorded. The time when the postbreakfast meal was offered depended on when the child reported being hungry enough to eat, but no child was allowed to eat the postbreakfast meal before 1115.
Statistical methods
Statistical analyses were conducted with the use of SUPER-ANOVA (version 1.11; Abacus Concepts Inc, Berkeley, CA) and STATVIEW (version 5.01; SAS Institute Inc, Cary, NC) software. The primary study analyses were comparisons between the binge-eating and non-binge-eating groups in satiety duration after the postfast meal and after the standardized breakfast shake meal, satiation time (time spent eating before participants reported fullness) for the 2 buffet meals, and energy consumption during the 2 buffet meals. Analyses of covariance were performed with group as the main factor and age, race, sex, the interaction between sex and age, socioeconomic status (27), fat-free mass (in kg), body fat mass (in kg), and number of buffet meal foods rated acceptable as covariates. A secondary analysis excluded data from the 10 children who did not rate ≥50% of the foods offered on the buffets ≥6 of the 10-point scale. Because neither the direction nor the significance of any result changed compared with analyses that included all subjects, data from all subjects are reported. By using a 5% type I error rate, we estimated that a sample of 60 participants would provide 80% power to detect a between-group difference in energy intake of ≈250 kcal and a group difference in satiety duration of 30 min. All results are presented as adjusted (least squares) means (±SDs) unless otherwise indicated. Statistical significance was defined as a two-tailed P ≤ 0.05, adjusted for multiple comparisons, so the false discovery rate would be 5% (28).
RESULTS
Sixty children participated in the study (Table 2). One child did not participate in the second buffet meal. No significant differences in age, sex, race, BMI z score, percentage fat, fat-free mass, socioeconomic status (27), or pubertal stage were observed between the binge-eating and non-binge-eating participants.
TABLE 2.
Characteristics of study participants1
| Children with reported binge-eating episodes (n = 10) | Children without reported binge-eating episodes (n = 50) | P2 | |
|---|---|---|---|
| Age (y) | 10.1 ± 1.6 | 10.4 ± 1.4 | 0.57 |
| Sex | 0.10 | ||
| Male (%) | 70 | 45 | |
| Female (%) | 30 | 55 | |
| Race | 0.60 | ||
| White (%) | 50 | 48 | |
| Black (%) | 30 | 42 | |
| Other (%) | 20 | 10 | |
| Socioeconomic status units | 3.2 ± 2.1 | 2.9 ± 1.4 | 0.42 |
| BMI z score3 | 2.7 ± 0.2 | 2.6 ± 0.2 | 0.11 |
| Fat mass (%) | 52.9 ± 5.7 | 48.9 ± 5.6 | 0.09 |
| Fat-free mass (%) | 47.7 ± 5.7 | 51.1 ± 6.4 | 0.09 |
Values are expressed as frequency for categorical variables and x̄ ± SD for continuous variables.
Chi-square tests for categorical variables and t tests for continuous variables were used to compare children with and without reported binge eating-episodes. Socioeconomic status was determined based on parents’ education and employment history.
BMI z score is a SD score for children’s BMI accounting for age and sex, calculated according to a formula from the Centers for Disease Control and Prevention (1).
Postfast meal
Self-reported ratings of hunger and fullness before the postfast meal and the duration of the meal were not significantly different between groups (Table 3). However, children in the binge-eating group reported a significantly greater desire to eat before the meal than did children in the non-binge-eating group (P = 0.004). Total intake during the postfast meal, adjusted for covariates (see Subjects and Methods), was significantly greater in children who reported binge eating than in children who did not binge eat (1748 ± 581 compared with 1309 ± 594 kcal; P = 0.04; Figure 1). No significant differences in the macronutrient composition of the foods consumed or in ratings of hunger, fullness, or desire to eat immediately after the meal were observed between the 2 groups (Table 3); however, the participants in the binge-eating group reported an earlier onset of hunger after the meal (194 ± 84 compared with 262 ± 89 min; P = 0.03; Figure 1). Body composition, included as a covariate in all analyses, was not significantly associated with energy intake (fat mass, P = 0.91; lean mass, P = 0.52), with satiety duration, or with ratings of hunger, fullness, or desire to eat.
TABLE 3.
Appetite ratings, duration of consumption, and macronutrient intake of meals1
| Children with reported binge-eating episodes (n = 10) | Children without reported binge-eating episodes (n = 50) | P2 | |
|---|---|---|---|
| Postfast meal | |||
| Hunger before meal (mm) | 78.1 ± 25.3 | 71.7 ± 19.1 | 0.50 |
| Fullness before meal (mm) | 18.5 ± 27.8 | 21.2 ± 25.4 | 0.63 |
| Desire to eat before meal (mm) | 77.6 ± 17.7 | 59.4 ± 14.8 | 0.004 |
| Duration (min) | 21.0 ± 6.0 | 17.1 ± 6.4 | 0.07 |
| Rate of eating (kcal/min) | 91.7 ± 40.8 | 80.2 ± 29.0 | 0.91 |
| Macronutrient content of meal consumed | |||
| Carbohydrate (%) | 44.2 ± 11.1 | 43.1 ± 7.8 | 0.69 |
| Protein (%) | 17.7 ± 4.7 | 14.8 ± 2.8 | 0.08 |
| Fat (%) | 38.1 ± 7.6 | 42.2 ± 6.4 | 0.07 |
| Hunger after meal (mm) | 3.3 ± 2.2 | 4.1 ± 4.9 | 0.77 |
| Fullness after meal (mm) | 91.7 ± 8.5 | 78.6 ± 27.6 | 0.12 |
| Desire to eat after meal (mm) | 4.1 ± 6.0 | 10.4 ± 17.7 | 0.11 |
| Breakfast shake meal | |||
| Hunger before shake (mm) | 58.1 ± 32.9 | 56.0 ± 26.9 | 0.68 |
| Fullness before shake (mm) | 5.5 ± 7.9 | 14.7 ± 19.1 | 0.19 |
| Desire to eat before shake (mm) | 71.7 ± 23.4 | 57.1 ± 19.1 | 0.09 |
| Duration (min) | 5.9 ± 6.3 | 6.6 ± 4.9 | 0.95 |
| Hunger after shake (mm) | 32.3 ± 40.2 | 22.0 ± 24.0 | 0.29 |
| Fullness after shake (mm) | 39.9 ± 40.2 | 47.6 ± 34.6 | 0.90 |
| Desire to eat after shake (mm) | 42.5 ± 39.5 | 31.6 ± 24.7 | 0.32 |
| Postbreakfast meal3 | |||
| Hunger before meal (mm) | 70.8 ± 37.3 | 67.3 ± 23.3 | 0.20 |
| Fullness before meal (mm) | 11.7 ± 25.0 | 11.3 ± 14.1 | 0.21 |
| Desire to eat before meal (mm) | 82.9 ± 22.4 | 60.3 ± 21.2 | 0.006 |
| Duration (min) | 22.1 ± 9.2 | 17.8 ± 7.1 | 0.12 |
| Rate of eating (kcal/min) | 92.8 ± 35.4 | 76.3 ± 32.5 | 0.48 |
| Macronutrient content | |||
| Carbohydrate (%) | 43.4 ± 13.3 | 42.3 ± 9.2 | 0.41 |
| Protein (%) | 15.1 ± 5.7 | 14.9 ± 3.5 | 0.64 |
| Fat (%) | 41.5 ± 9.8 | 42.8 ± 7.8 | 0.34 |
| Hunger after meal (mm) | 4.2 ± 4.1 | 4.5 ± 4.9 | 0.55 |
| Fullness after meal (mm) | 78.4 ± 25.3 | 72.2 ± 32.5 | 0.42 |
| Desire to eat after meal (mm) | 7.8 ± 8.8 | 9.5 ± 18.4 | 0.36 |
All values are adjusted x̄ ± SD.
Children with and without reported binge eating were compared by using analyses of covariance, accounting for demographic variables. Analyses of covariance were performed with group as the main factor and age, race, sex, the interaction between sex and age, socioeconomic status, fat-free mass (in kg), body fat mass (in kg), and number of buffet meal foods rated acceptable as covariates.
For the postshake buffet meal, 9 children with binge eating behavior participated.
Breakfast shake meal
Self-reported ratings of hunger, fullness, and desire to eat before the breakfast shake, the amount of the shake consumed (751 ±152 kcal for the binge-eating group compared with 755 ± 1495 kcal for the non-binge-eating group; P =0.94), and ratings of hunger, fullness, and desire to eat immediately after the breakfast shake meal were not significantly different between the groups (Table 3). However, the children in the binge-eating group again reported an earlier onset of hunger after consumption of the breakfast meal than did the children in the non-binge-eating group (75 ± 62 compared with 132 ± 62 min; P = 0.01; Figure 1).
Postbreakfast meal
Children in the binge-eating and non-binge-eating groups did not differ significantly in the mean time at which they were offered the postbreakfast meal [binge-eating group: 1212 (4 min); non-binge-eating group: 1230 (8 min); P = 0.11]. Although no significant differences were observed in premeal ratings of hunger or fullness between the binge-eating and non-binge-eating groups (Table 3), the children in the binge-eating group reported a greater desire to eat before the postbreakfast meal than did the children in the non-binge-eating group (P = 0.006). The same pattern was seen for total energy intake with the postfast meal: children in the binge-eating group consumed significantly more energy than did children in the non-binge-eating group (1874 ± 560 compared with 1275 ± 566 kcal; P =0.004; Figure 1). Body composition, included as a covariate in all analyses, was not associated with energy intake (fat mass, P =0.85; lean mass, P =0.14) or with ratings of hunger, fullness, or desire to eat.
Three-factor eating inventory
Results of the three-factor eating inventory are shown in Figure 2. Children who reported binge eating (n = 8) did not differ significantly from non-binge-eating participants (n = 40) in restraint scale scores (6.9 ± 4.7 compared with 7.4 ± 4.9; P = 0.80). However, the binge-eating children reported significantly higher levels of disinhibition (9.8 ±3.5 compared with 5.7 ± 3.5; P = 0.003) and hunger (10.7 ± 4.1 compared with 5.3 ± 11.8; P < 0.001).
FIGURE 2.
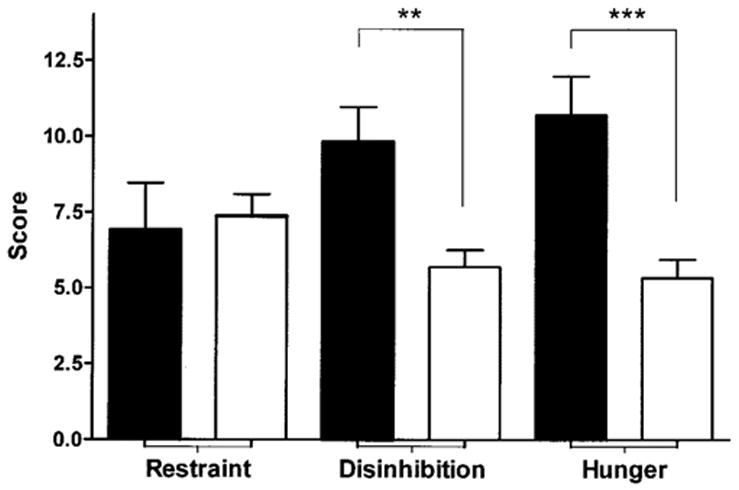
Mean scores (±SEM) from the Three-Factor Eating Inventory, which assesses dietary restraint, disinhibition, and hunger, in children who reported binge-eating episodes (■; n = 8) and children who reported no binge-eating episodes (□; n = 40). **,***Significantly different from children with no binge-eating episodes (ANCOVA for the effect of binge-eating status on each of the 3 factors contained in the questionnaire): **P < 0.01, ***P < 0.001.
DISCUSSION
More than 30% of children and adolescents in the United States are now classified as overweight or at risk of overweight (29), and most of these children are predicted to become overweight or obese adults (30, 31). Among the sociocultural factors believed to promote pediatric weight gain is the increasing tendency for foods to be purchased in restaurants and from other purveyors of prepared foods. More than 40% of money spent on food by families is now used to purchase food prepared outside the home (32), 75% of adolescents report eating ≥1 fast-food meal/wk (33), and as much as 30% may eat a fast-food meal >3 times/wk (33, 34). Portion size and energy density tend to be greater in meals prepared and eaten away from home (35, 36). Because larger portion sizes lead to greater intake for children aged ≥4 y (37–40), it is perhaps not surprising that the number of quick-service meals consumed was found to predict girls’ weight gain (41). In the present study, we found that when overweight children who reported binge eating were asked to choose their lunch from a buffet that contained large portions of palatable foods, they overate to a significantly greater extent than did equally overweight children not reporting binge eating. Children with a history of binge eating ate >400 kcal more than did children who did not report binge eating. Despite their greater energy intake, the children who reported binge eating became hungry ≈1 h earlier than did the children who did not report binge eating.
The greater energy intakes we observed in children with a history of binge eating during the 2 buffet meals are consistent with data from laboratory studies of adults with binge-eating disorder who, when instructed to binge eat, consume significantly more energy than adults who do not engage in binge eating (42–44). More important, the greater intake of children with a history of binge eating and the shorter time for which they remain sated may explain why children and adolescents who report binge eating are heavier (3, 7, 8) and gain more weight over time (9–12) than children and adolescents with no such history. Children who report binge-eating behaviors appear to have deficits in appetite regulation that put them at risk for the development of obesity because of their capacity to consume more energy and become hungry more rapidly than children without binge-eating behaviors. Future studies are needed to elucidate the behavioral, genetic, and neurohumoral (45) mechanisms for these observations. Children with binge eating behavior also reported significantly greater scores on the Three-Factor Eating Inventory disinhibition scale, which is a measure of responsiveness to external food stimuli and emotional states, than did children who did not binge eat. This observation suggests that children who report binge eating may be responding less to internal physiologic hunger cues and more to sensory cues or their own affective and cognitive statuses. Functional neuroimaging studies conducted in adults suggest those with binge eating have greater activation of the premotor cortex when stimulated by food cues than do those with no binge eating (46, 47). Interventions that focus on training children to attend to physical hunger signals (48) may then be proposed as a method for slowing the progression of weight gain in children with binge eating.
Among the strengths of the present study are the similar body composition of children with and without reported binge eating who participated and the evaluation of actual food intake under controlled conditions rather than reliance on self-reports of intake (49). Because children were admitted to the Clinical Research Center for study, energy intake and duration of satiety could be measured accurately twice, with energy intake at intervening meals controlled. Limitations of the study include the relatively small number of participants, particularly in the binge-eating category, and the use of a questionnaire, rather than an interview, to determine binge-eating status. Because of the design of the questionnaire used, we were unable to elucidate whether the greater energy intake and the shorter satiety time observed in the children in the binge-eating group can be attributed to eating an objectively large amount of food or to experiencing a loss of control over eating. Previous studies that examined binge eating in children have reported that loss of control, rather than the amount of food ingested, appears to be the factor most often associated with increased eating-related emotional distress (50) and greater body weight (3) than eating episodes that do not contain the element of a loss of control. Although sex was included in all statistical models and was not significantly different between the 2 groups, given the somewhat large number of boys in the binge-eating group, it is possible that these findings are more descriptive of male binge eaters. Additional laboratory studies that include larger numbers of female binge eaters are needed to determine potential sex differences in binge-eating behavior. Finally, because the children in the present study were tested individually, we could not examine the complex behavioral interactions that may stimulate or inhibit intake when children eat with others.
In conclusion, treatment-seeking, overweight children who report binge eating appear to be at particular risk of overeating when offered large quantities of palatable foods. Future studies are needed to examine methods that may help overweight children with binge eating moderate their food intake and thus prevent their continued excessive weight gain.
Acknowledgments
We thank the families who participated in these studies and the staff of the metabolic kitchen at the National Institutes of Health Clinical Center.
JAY and MS are commissioned officers in the United States Public Health Service, Department of Health and Human Services.
MCM, MT-K, and JAY conducted the data analysis. JAY, JRM, and SZY conceived the hypothesis for this article. JK and JAY were primarily responsible for developing the study design, supervised the data collection, and provided critical input. MS and KRT contributed to data collection and provided critical input on data analyses and on versions of the manuscript. All authors participated in the interpretation of the results and approved the final version of the manuscript. None of the authors had any conflicts of interest.
Footnotes
Address reprint requests to JA Yanovski, Unit on Growth and Obesity, DEB, NICHD, NIH, CRC, Room 1-3330, 10 Center Drive, MSC-1103, Bethesda, MD 20892-1103. E-mail: jy15i@nih.gov.
From the Growth and Obesity, Developmental Endocrinology Branch, National Institute of Child Health and Human Development (NICHD) (MCM, MJMcD, SZY, MT-K, KRT, and JAY); the Division of Digestive Diseases and Nutrition, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (SZY); the Nutrition Department, Hatfield Clinical Research Center (MS); and the Phoenix Epidemiology and Clinical Research Branch, NIDDK (JK), National Institutes of Health, Department of Health and Human Services, Bethesda, MD.
The funding organization played no role in design and conduct of the study; in collection, management, analysis, and interpretation of the data; or in preparation or review of the manuscript. The opinions expressed are those of the authors and do not necessarily reflect the viewpoint of the Indian Health Service or the US Public Health Service.
Supported by the Intramural Research Program of the NIH, grant ZO1-HD-00641 (NICHD) to JAY.
References
- 1.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 2.Berkowitz R, Stunkard AJ, Stallings VA. Binge-eating disorder in obese adolescent girls. Ann N Y Acad Sci. 1993;699:200–6. doi: 10.1111/j.1749-6632.1993.tb18850.x. [DOI] [PubMed] [Google Scholar]
- 3.Morgan CM, Yanovski SZ, Nguyen TT, et al. Loss of control over eating, adiposity, and psychopathology in overweight children. Int J Eat Disord. 2002;31:430–41. doi: 10.1002/eat.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Decaluwe V, Braet C, Fairburn CG. Binge eating in obese children and adolescents. Int J Eat Disord. 2003;33:78–84. doi: 10.1002/eat.10110. [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic statistical manual of mental disorders, DSM-IV-TR. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 6.Smith DE, Marcus MD, Lewis CE, Fitzgibbon M, Schreiner P. Prevalence of binge eating disorder, obesity, and depression in a biracial cohort of young adults. Ann Behav Med. 1998;20:227–32. doi: 10.1007/BF02884965. [DOI] [PubMed] [Google Scholar]
- 7.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. J Consult Clin Psychol. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Decaluwe V, Braet C. Prevalence of binge-eating disorder in obese children and adolescents seeking weight-loss treatment. Int J Obes Relat Metab Disord. 2003;27:404–9. doi: 10.1038/sj.ijo.0802233. [DOI] [PubMed] [Google Scholar]
- 9.Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psychol. 1999;67:967–74. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- 10.Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: a 2-year prospective investigation. Health Psychol. 2002;21:131–8. [PubMed] [Google Scholar]
- 11.Field AE, Austin SB, Taylor CB, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112:900–6. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- 12.Tanofsky-Kraff M, Cohen M, Yanovski SZ, et al. A prospective study of psychological and behavioral predictors for weight change in children at-risk for obesity: depression, dieting and binge eating and disordered eating attitudes. Pediatrics. 2006;117:1203–9. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hellstrom PM, Geliebter A, Naslund E, et al. Peripheral and central signals in the control of eating in normal, obese and binge-eating human subjects. Br J Nutr. 2004;92(suppl):S47–57. doi: 10.1079/bjn20041142. [DOI] [PubMed] [Google Scholar]
- 14.Raymond NC, de Zwann M, Faris PL, et al. Pain thresholds in obese binge-eating disorder subjects. Biol Psychiatry. 1995;37:202–4. doi: 10.1016/0006-3223(94)00244-w. [DOI] [PubMed] [Google Scholar]
- 15.NIH Clinical Research Studies, protocol no. 00-CH-0134. Bethesda, MD: National Institute of Child Health and Human Development; 2005. Effects of metformin on energy intake, energy expenditure, and body weight in overweight children with insulin resistance. [Google Scholar]
- 16.Nicholson JC, McDuffie JR, Bonat SH, et al. Estimation of body fatness by air displacement plethysmography in African American and white children. Pediatr Res. 2001;50:467–73. doi: 10.1203/00006450-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Dempster P, Aitkens S. A new air displacement method for the determination of human body composition. Med Sci Sports Exerc. 1995;27:1692–7. [PubMed] [Google Scholar]
- 18.Johnson WG, Grieve FG, Adams CD, Sandy J. Measuring binge eating in adolescents: adolescent and parent versions of the questionnaire of eating and weight patterns. Int J Eat Disord. 1999;26:301–14. doi: 10.1002/(sici)1098-108x(199911)26:3<301::aid-eat8>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 19.Tanofsky-Kraff M, Morgan CM, Yanovski SZ, Marmarosh C, Wilfley DE, Yanovski JA. Comparison of assessments of children’s eating-disordered behaviors by interview and questionnaire. Int J Eat Disord. 2003;33:213–24. doi: 10.1002/eat.10128. [DOI] [PubMed] [Google Scholar]
- 20.Steinberg E, Tanofsky-Kraff M, Cohen ML, et al. Comparison of the child and parent forms of the Questionnaire on Eating and Weight Patterns in the assessment of children’s eating-disordered behaviors. Int J Eat Disord. 2004;36:183–94. doi: 10.1002/eat.20022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tanofsky-Kraff M, Yanovski SZ, Yanovski JA. Comparison of child interview and parent reports of children’s eating disordered behaviors. Eat Behav. 2005;6:95–9. doi: 10.1016/j.eatbeh.2004.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson WG, Kirk AA, Reed AE. Adolescent version of the questionnaire of eating and weight patterns: reliability and gender differences. Int J Eat Disord. 2001;29:94–6. doi: 10.1002/1098-108x(200101)29:1<94::aid-eat16>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 23.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 24.Hetherington M, Rolls BJ. Methods of investigating human behavior. In: Toates F, Rowland N, editors. Feeding and drinking. Amsterdam, Netherlands: Elsevier Science Publishers BV; 1987. pp. 77–109. [Google Scholar]
- 25.Block G, Norris JC, Mandel RM, DiSogra C. Sources of energy and six nutrients in diets of low-income Hispanic-American women and their children: quantitative data from HHANES, 1982–1984. J Am Diet Assoc. 1995;95:195–208. doi: 10.1016/S0002-8223(95)00048-8. [DOI] [PubMed] [Google Scholar]
- 26.Silverstone T. Anorectic drugs. In: Silverstone T, editor. Obesity, its pathogenesis and management. Acton, MA: Publishing Sciences Group, Inc; 1975. pp. 193–227. [Google Scholar]
- 27.Hollingshead AB. Hollingshead two factor index of social position 1957. In: Miller DC, editor. Handbook of research design and social measurement. 5. Newbury Park, CA: Sage Publications; 1991. pp. 351–9. [Google Scholar]
- 28.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc B. 1995;57:289–300. [Google Scholar]
- 29.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 30.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 31.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Racial differences in the tracking of childhood BMI to adulthood. Obes Res. 2005;13:928–35. doi: 10.1038/oby.2005.107. [DOI] [PubMed] [Google Scholar]
- 32.Lin B, Guthrie JF, Frazao E. Quality of children’s diets at and away from home: 1994–96. Food Rev. 1999;22:2–10. [Google Scholar]
- 33.French SA, Story M, Neumark-Sztainer D, Fulkerson JA, Hannan P. Fast food restaurant use among adolescents: associations with nutrient intake, food choices and behavioral and psychosocial variables. Int J Obes Relat Metab Disord. 2001;25:1823–33. doi: 10.1038/sj.ijo.0801820. [DOI] [PubMed] [Google Scholar]
- 34.Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113:112–8. doi: 10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- 35.Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health. 2002;92:246–9. doi: 10.2105/ajph.92.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ebbeling CB, Sinclair KB, Pereira MA, Garcia-Lago E, Feldman HA, Ludwig DS. Compensation for energy intake from fast food among overweight and lean adolescents. JAMA. 2004;291:2828–33. doi: 10.1001/jama.291.23.2828. [DOI] [PubMed] [Google Scholar]
- 37.Rolls BJ, Engell D, Birch LL. Serving portion size influences 5-year-old but not 3-year-old children’s food intakes. J Am Diet Assoc. 2000;100:232–4. doi: 10.1016/S0002-8223(00)00070-5. [DOI] [PubMed] [Google Scholar]
- 38.Orlet Fisher J, Rolls BJ, Birch LL. Children’s bite size and intake of an entree are greater with large portions than with age-appropriate or self-selected portions. Am J Clin Nutr. 2003;77:1164–70. doi: 10.1093/ajcn/77.5.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rolls BJ, Roe LS, Meengs JS, Wall DE. Increasing the portion size of a sandwich increases energy intake. J Am Diet Assoc. 2004;104:367–72. doi: 10.1016/j.jada.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 40.Wansink B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annu Rev Nutr. 2004;24:455–79. doi: 10.1146/annurev.nutr.24.012003.132140. [DOI] [PubMed] [Google Scholar]
- 41.Thompson OM, Ballew C, Resnicow K, et al. Food purchased away from home as a predictor of change in BMI z-score among girls. Int J Obes Relat Metab Disord. 2004;28:282–9. doi: 10.1038/sj.ijo.0802538. [DOI] [PubMed] [Google Scholar]
- 42.Yanovski SZ, Leet M, Yanovski JA, et al. Food selection and in take of obese women with binge-eating disorder. Am J Clin Nutr. 1992;56:975–80. doi: 10.1093/ajcn/56.6.975. [DOI] [PubMed] [Google Scholar]
- 43.Goldfein JA, Walsh BT, LaChaussee JL, Kissileff HR, Devlin MJ. Eating behavior in binge eating disorder. Int J Eat Disord. 1993;14:427–31. doi: 10.1002/1098-108x(199312)14:4<427::aid-eat2260140405>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 44.Walsh BT, Boudreau G. Laboratory studies of binge eating disorder. Int J Eat Disord. 2003;34(suppl):S30–8. doi: 10.1002/eat.10203. [DOI] [PubMed] [Google Scholar]
- 45.Geliebter A, Gluck ME, Hashim SA. Plasma ghrelin concentrations are lower in binge-eating disorder. J Nutr. 2005;135:1326–30. doi: 10.1093/jn/135.5.1326. [DOI] [PubMed] [Google Scholar]
- 46.Karhunen LJ, Vanninen EJ, Kuikka JT, Lappalainen RI, Tiihonen J, Uusitupa MI. Regional cerebral blood flow during exposure to food in obese binge eating women. Psychiatry Res. 2000;99:29–42. doi: 10.1016/s0925-4927(00)00053-6. [DOI] [PubMed] [Google Scholar]
- 47.Geliebter A, Ladell T, Logan M, Schweider T, Sharafi M, Hirsch J. Responsivity to food stimuli in obese and lean binge eaters using functional MRI. Appetite. 2006;46:31–5. doi: 10.1016/j.appet.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 48.Johnson SL. Improving preschoolers’ self-regulation of energy intake. Pediatrics. 2000;106:1429–35. doi: 10.1542/peds.106.6.1429. [DOI] [PubMed] [Google Scholar]
- 49.Anderson DA, Williamson DA, Johnson WG, Grieve CO. Validity of test meals for determining binge eating. Eat Behav. 2001;2:105–12. doi: 10.1016/s1471-0153(01)00022-8. [DOI] [PubMed] [Google Scholar]
- 50.Tanofsky-Kraff M, Faden D, Yanovski SZ, Wilfley DE, Yanovski JA. The perceived onset of dieting and loss of control eating behaviors in overweight children. Int J Eat Disord. 2005;38:112–22. doi: 10.1002/eat.20158. [DOI] [PMC free article] [PubMed] [Google Scholar]


