Abstract
The unprecedented spread of highly pathogenic avian influenza virus subtype H5N1 in Asia and Europe is threatening animals and public health systems. Effective diagnosis and control management are needed to control the disease. To this end, we developed a panel of monoclonal antibodies (MAbs) against the H5N1 avian influenza virus (AIV) and implemented an antigen-capture enzyme-linked immunosorbent assay (AC-ELISA) to detect the H5 viral antigen. Mice immunized with denatured hemagglutinin (HA) from A/goose/Guangdong/97 (H5N1) expressed in bacteria or immunized with concentrated H5N2 virus yielded a panel of hybridomas secreting MAbs specific for influenza virus HA. The reactivity of each MAb with several subtypes of influenza virus revealed that hybridomas 3D4 and 8B6 specifically recognized H5 HA. Therefore, purified antibodies from hybridomas 3D4 and 8B6, which secrete immunoglobulin G (IgG) and IgM, respectively, were used as the capture antibodies and pooled hyperimmune guinea pig serum IgG served as the detector antibody. The specificity of the optimized AC-ELISA was evaluated by using AIV subtypes H5 H3, H4, H7, H9, and H10. Specimens containing AIV subtype H5 subtype yielded a specific and strong signal above the background, whereas specimens containing all other subtypes yielded background signals. The detection limits of the AC-ELISA were 62.5 ng of bacterium-expressed H5N1 HA1 protein and 124, 62, and 31 50% tissue culture infective doses of influenza virus subtypes H5N1/PR8, H5N2, and H5N3, respectively. Reconstituted clinical samples consisting of H5 AIVs mixed with pharyngeal-tracheal mucus from healthy chickens also yielded positive signals in the AC-ELISA, and the results were confirmed by reverse transcription-PCR. The tracheal swab samples from H9N2-infected chickens did not give positive signals. Taken together, the newly developed MAb-based AC-ELISA offers an attractive alternative to other diagnostic approaches for the specific detection of H5 AIV.
Highly pathogenic avian influenza (HPAI) viruses have emerged in poultry and wildlife worldwide, causing sporadic but serious and devastating outbreaks. These viruses have been restricted to hemagglutinin (HA) subtypes H5 and H7, although not all viruses of these subtypes are highly pathogenic. An outbreak of H5N1 HPAI in the live bird markets of Hong Kong in 1997 resulted in 18 human infections, 6 of them fatal (5, 29). Similar H5N1 HPAI viruses have reemerged in several countries in Asia since 2001 and have continued to spread through Asia and into the Middle East and Eastern Europe (21, 22). In addition to their geographic spread, H5N1 HPAI viruses were found in multiple animal species, such as poultry, wild birds, tigers, and leopards (5, 15, 24, 25; http://www.who.int/csr/disease/avian-influenza/guidelines/handlingspecimens/en/index.html). Besides these devastating consequences for animal health, H5N1 infections have resulted in 256 laboratory-confirmed infected people, including 167 deaths (28). Human infections are generally the result of exposure to H5N1-infected poultry. Reducing the prevalence of H5N1 in poultry would have a favorable impact on public health.
The accurate and prompt diagnosis of H5N1 infection in birds is a critical component of a disease control plan. Currently, virus isolation in embryonated eggs or in Madin-Darby canine kidney (MDCK) cells and subsequent HA and neuraminidase subtyping by serological methods constitute the standard for avian influenza virus (AIV) detection and serological classification. However, conventional culture methods require special collection and transport conditions to ensure virus viability, and the recovery of the results may take 1 to 2 weeks, by which time the results may no longer be relevant. Molecular detection methods, such as standard reverse transcription-PCR (RT-PCR), have previously been applied for the diagnosis of AIV infections and HA subtype identification (2, 11, 14, 17). Additionally, real-time PCR assays and a DNA microarray analysis for the detection of influenza virus have been developed (16). However, these methods are technically demanding, and false-positive results may arise from cross contaminations between samples. Antigen detection methods have repeatedly shown their value in the diagnosis of various infectious diseases. The currently available antigen detection methods, such as the FLU OIA TEST (Biostar) and the Directigen FLU A kit (BD, Biosciences) (2, 11), are based on the detection of the viral nucleoprotein, which is conserved in all influenza A viruses and which is therefore not specific for the H5 subtype influenza virus (29). Detection of the H5 antigen would provide strong evidence of AIV subtype H5 infection. This report describes the production and characterization of monoclonal antibodies (MAbs) against HA and the development of an antigen-capture enzyme-linked immunosorbent assay (AC-ELISA) for the detection of AIV H5 in pure culture and in reconstituted clinical samples. The specificity and sensitivity of the assay were evaluated.
MATERIALS AND METHODS
Viruses and cells.
AIV H5N1 (A/goose/Guangdong/97) was inactivated with beta-propiolactone (9) and was used for RNA extraction to amplify the HA1 domain in HA gene. A nonpathogenic H5N1 virus (H5N1/PR8), a PR8 strain-based recombinant influenza virus harboring the HA and the neuraminidase genes of H5N1 Vietnam isolate (A/Vietnam/1203/2004) (23), and AIV subtypes H5N2, H5N3, H3N2, H4N1, H7N1, H9N2, and H10N5 were obtained from the Agri-Food and Veterinary Authority of Singapore (Table 1).
TABLE 1.
Avian influenza viruses used in the experiment
| Antigen | Virus strain (subtype) | Gene/expression system |
|---|---|---|
| rHA1 | A/goose/Guangdong/97 (H5N1) | HA1 domain |
| H5N2 | A/chicken/Singapore/98 | HA |
| H5N1/PR8 | HA and NA from A/Vietnam/1203/2004, internal genes from A/Puerto Rico/8/1934 | HA |
| H5N3 | A/chicken/Singapore/97 | HA |
| H3N2 | A/chicken/Singapore/02 | HA |
| H4N1 | A/chicken/Singapore/92 | HA |
| H7N1 | A/chicken/Singapore/94 | HA |
| H9N2 | A/chicken/Singapore/98 | HA |
| H10N5 | A/chicken/Singapore/93 | HA |
MDCK cells were obtained from the American Type Culture Collection. The cells were propagated in Dulbecco's minimal essential medium (DMEM) supplemented with 10% fetal bovine serum. Virus stocks were grown in 11-day-old embryonated chicken eggs or MDCK cells in DMEM supplemented with 0.5% bovine serum albumin and 1 μg/ml of trypsin. Virus titers were determined by HA assays by first serially diluting the virus stocks and inoculating either MDCK cells or chicken embryos, followed by a 48-h incubation. Virus was then collected from cell-free supernatants or allantoic fluid and was used for HA determinations. When required, AIV H5N2 was concentrated by ultracentrifugation at 450,000 × g for 2 h. The virus pellet was then resuspended in phosphate-buffered saline (PBS) and stored at −80°C.
All experiments with live viruses were performed in a biosafety level 3 containment laboratory, in compliance with CDC/NIH and WHO recommendations (4, 26), and were also approved by the Agri-Food and Veterinary Agency and Ministry of Health of Singapore.
Molecular cloning.
RNA was extracted from inactivated AIV H5N1 (A/goose/Guangdong/97) by using TRIzol (Invitrogen, Carlsbad, CA). cDNA was synthesized, followed by amplification of the HA1 gene by PCR with gene-specific primers (forward primer, 5′-CGGGATCCATGGAGAAAATAGTGCTTCTTC-3′; reverse primer, 5′-ATAAGAATGCGGCCGCTTATTGAGGGACA-3′) designed according to published data (GenBank accession no. AY555153). PCR was initiated by denaturation at 95°C for 5 min, followed by 35 cycles of 94°C for 45 s, 55°C for 45 s, and 72°C for 1 min. The amplified products were further elongated at 72°C for 10 min. RT-PCR products were cloned into the pET-30 vector (QIAGEN, Hilden, Germany) and transformed into Escherichia coli BL-21 competent cells to express the protein. The same amplicon was also cloned into pFASTBACHT, a vector used to construct a recombinant baculovirus harboring the H5N1 HA1 gene, which was then used to infect Sf-9 cells propagated in Sf-900 II medium for the development of an immunofluorescence assay (IFA) to screen for H5-specific MAbs.
Production and purification of recombinant H5N1 HA1 protein (rHA1).
The transformed E. coli BL-21 cells were grown at 37°C to an optical density (OD) at 600 nm of 0.5 to 0.6 in Luria-Bertani medium containing ampicillin (100 μg/ml), protein expression was induced by the addition of 0.10 mM isopropyl-β-d-thiogalactopyranoside for 5 h with shaking, and the cells were pelleted and resuspended in PBS. The sonicated cell lysate was centrifuged at 20,000 × g for 10 min. The insoluble protein was purified from the pellet with an electroeluter (model 422; Bio-Rad), according to the manufacturer's instructions. HA1 was resuspended in solubilization solution (Pierce, Rockford, IL) for analysis by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and Western blotting, in which rabbit anti-H5N1 antiserum or mouse antihistidine MAb was used as the primary antibody and horseradish peroxidase (HRP)-conjugated goat anti-rabbit immunoglobulin (Ig) or rabbit anti-mouse Ig was used as the secondary antibody.
Preparation and purification of MAbs.
BALB/c mice were immunized twice intramuscularly with 25 μg of rHA1 or purified AIV H5N2 in 0.1 ml of PBS which was emulsified with an equal volume of adjuvant (SEPPIC, France). An intraperitoneal booster of the same dose of rHA1 or H5N2 virus was given 3 days before splenocytes were collected and fused to SP/2.0 myeloma cells, as described previously (33). The hybridoma culture supernatants were screened by IFAs with mock-infected or recombinant baculovirus-infected Sf-9 cells and H5N1/PR8-, H5N2-, and H5N3-infected MDCK cells as the antigen, as described below. Hybridomas that produced a specific antibody were cloned by limiting dilution and expanded and cultured in 75-cm2 flasks. One week later, the hybridoma cultures were harvested and the cell debris was removed by centrifugation at 400 × g for 10 min. The supernatant was collected and stored at −20°C.
Ascitic fluid was prepared from pristane-primed BALB/c mice inoculated with hybridomas, as described previously (33), and was stored in 1% glycerol at −20°C. IgG and IgM were purified from clarified ascitic fluid by using a protein A affinity column (Sigma) and an Immnopure IgM purification kit (Pierce), in accordance with the manufacturers’ instructions. Ig concentrations were determined spectrophotometrically (Nanodrop).
IFA.
Sf-9 cells in 96-well plates were infected with recombinant baculovirus harboring the truncated H5N1 HA1 gene, and MDCK cells in 96-well plates were infected with AIV H5N1/PR8, H5N2, and H5N3, respectively. At 36 h (for Sf-9 cells) and 72 h (for MDCK cells) postinfection, the cells were fixed with absolute ethanol for 30 min at room temperature and washed three times with PBS, pH 7.4. The fixed cells were incubated with hybridoma culture fluid at 37°C for 1 h. The cells were rinsed three times with PBS and incubated with a 1:40 dilution of fluorescein isothiocyanate (FITC)-conjugated rabbit anti-mouse Ig (Dako, Demark). The cells were rinsed again in PBS, before the results were scored in an epifluorescence microscope (Olympus, Japan) with appropriate barrier and excitation filters for optimized visualization with FITC.
Immunoblotting.
rHA1 and purified H5N1/PR8, H5N2, and H5N3 were subjected to 12% SDS-PAGE. The separated proteins were electrotransferred and immobilized onto nitrocellulose membrane. The membrane was blocked with 5% nonfat milk in PBS containing 0.1% Tween 20 (PBST) at 37°C for 1 h. The membrane was subsequently incubated with ascitic fluid or hybridoma supernatant, rinsed in PBST, and incubated with HRP-conjugated rabbit anti-mouse Ig. The membrane was developed by incubation with 3,3′-diaminobenzidine (DAB) and hydrogen peroxide, as described previously (8).
HI test.
MAbs 3D4 and 8B6 were subjected to the hemagglutination-inhibition (HI) test, according to the standard method (26).
Isotyping of MAb.
Isotyping was performed by using a mouse MAb isotyping kit (Amersham Bioscience, England).
Production of monospecific polyclonal antibodies and IgG extraction.
Guinea pigs were immunized with 100 μg of purified rHA1. Booster injections were administered at 2-week intervals. Serum samples collected 10 days after the last immunization were evaluated for antibodies against rHA1 by IFAs, as described above. Subsequently, extraction and determination of the IgG concentrations were performed by using the same protocols used for MAb 3D4. The reactivity of the IgG with purified rHA1 was assessed by an AC-ELISA, as described below.
Dot blot assay for antigen detection.
Five microliters of purified MAb 3D4 IgG (approximately 8 ng of protein) was spotted onto a nitrocellulose membrane. After the membrane was air dried, it was blocked with 5% nonfat milk; placed in a six-well plate; and incubated with H5N2, H5N3, H7N1, and H9N2 at 37°C for 1 h. The membrane was rinsed extensively and incubated with guinea pig anti-rHA1 polyclonal antibodies for another 1 h. The membrane was rinsed five times and further incubated with HRP-conjugated rabbit anti-guinea pig Ig. Bound antibodies were detected by the addition of DAB and H2O2 as the substrate, as described previously (8).
Development of AC-ELISA.
Ninety-six-well round-bottom microtiter plates (Nunc, Roskilde, Demark) were coated with twofold serial dilutions of purified IgG (MAb 3D4) and IgM (MAb 8B6) in 50 μl carbonate buffer (73 mM sodium bicarbonate and 30 mM sodium carbonate) and incubated at 37°C for 1 h or at 4°C overnight. Between all subsequent incubation steps, the plates were washed three times with PBST, and all dilutions were made in PBST containing 1% nonfat milk. The plates were blocked by incubation with 50 μl of blocking solution (5% nonfat milk in PBST) at 37°C for 1 h, rinsed, and incubated with 50 μl of purified rHA1 (100 ng) or AIV H5 subtypes (H5N1/PR8, H5N2, and H5N3) at 37°C for 1 h. After the plates were rinsed, 50 μl of guinea pig monospecific IgG antibody (1:480 dilution) was added; and the mixture was incubated for 1 h at 37°C, washed, and further incubated with 50 μl of HRP-conjugated rabbit anti-guinea pig Ig (diluted 1:1,000). Color development was performed by the addition of 50 μl of freshly prepared substrate solution (o-phenylenediamine); the absorbance at 490 nm was read with an ELISA reader (Tecan, Switzerland). The working concentrations of the MAbs and the monospecific antibodies were determined by checkerboard titration by comparison of the highest signal-to-noise ratio for the detection of H5 (H5N1, H5N2, and H5N3) and non-H5 AIV (H7N1 and H9N2) subtypes. The signal-to-noise ratio was calculated by dividing the absorbance of the homologous antigen by that of the heterologous antigen.
Analytical sensitivity of AC-ELISA.
Tenfold serial dilutions of purified rHA1 in PBST and 1% nonfat milk and twofold serial dilutions of H5N1/PR8, H5N2, and H5N3 in allantoic fluid were used as the antigens in the capture ELISA. The diluent and mock-inoculated allantoic fluids were used as blank controls. The detection limits for rHA1 and the AIV H5 subtypes were determined according to the cutoff value, which was calculated by the formula mean ± 2 standard deviations (SDs).
Analytical specificity of AC-ELISA.
AIV subtypes H3N2, H4N1, H7N1, H9N2, and H10N5 were propagated in specific-pathogen-free embryos (Charles River, Inc). Debris was removed from the harvested virus supernatant by centrifugation at 20,000 × g for 30 min. The viruses containing supernatants were subjected to our AC-ELISA, and the results were judged according to the cutoff value.
H9N2 was used to infect chickens because H9N2 is an etiological agent for avian influenza cases (1, 19) and was isolated from a Hong Kong poultry market. The virus has genomic segments similar to those of the 1997 H5N1-like virus. To further exclude the possibility of false-positive signals for the detection of non-H5 AIV in clinical samples, 20 chickens were infected with H9N2 by the oral and intramuscular routes. Tracheal swab specimens were collected daily until day 7 after infection and were kept in PBS at −80°C. Another 20 chickens without infection served as negative controls. After the swabs were frozen-thawed twice, the swabs were vortexed to dislodge viruses, followed by centrifugation at 10,000 × g for 10 min to remove the cell debris. The clarified supernatants were subjected to AC-ELISA.
Detection of H5N1/PR8, H5N2, and H5N3 in clinical reconstituted samples.
To mimic clinical samples, pharyngeal-tracheal swab specimens were collected from healthy and AIV antibody-free chickens and spiked with H5N1/PR8, H5N2, and H5N3. Mucus that had been collected with swabs and diluted in PBS was frozen-thawed twice and serially diluted for analysis by the AC-ELISA and RT-PCR.
RNA was isolated from the mucus eluted from the swabs with TRIzol (Invitrogen) and was used as the template for RT-PCR with the Titan One Tube RT-PCR system (Roche, Mannheim, Germany). The H5-specific primers (forward primer, 5′-CGCGGATCCGTTACACATGCCCAAGACATAC-3′; reverse primer, 5′-ACGCGTCGACCGCATCATTAGGATGGTGAATCCC-3′) were designed according to the published sequence in the GenBank database (GenBank accession no. AY555153). The amplified HA amplicon (479 bp), which was specific for H5 AIV, was amplified and analyzed by agarose gel electrophoresis.
RESULTS
Amplification of AIV H5N1 HA1 gene and protein expression.
The HA1 domain (0.938 kb) of the H5 HA was amplified by RT-PCR (Fig. 1A) and cloned into a prokaryotic expression vector, pQE-30. The transformant E. coli isolate expressed the histidine-fusion HA1 protein of the expected size in an insoluble form. rHA1 was recognized by both rabbit anti-H5N1 serum and mouse antihistidine MAb (Fig. 1B). The rHA1 protein was also expressed in Sf-9 cells infected with recombinant baculovirus and demonstrated the same Western blot patterns as rHA1 expressed in E. coli (data not shown). The rHA1 proteins expressed in E. coli were further purified with an electroeluter and were used as the antigen to immunize mice for the purpose of MAb production, while the Sf-9 cells that expressed rHA1 at a peak level at 36 to 48 h postinfection were used for IFA development.
FIG. 1.
Amplification of AIV H5N1 HA1 gene (A) and protein expression (B). The HA1 fragment, with a size of 0.938 kb, was amplified from A/goose/Guangdong/96 (H5N1) by RT-PCR. rHA1 was expressed and recognized by Western blotting with rabbit anti-H5N1 serum and a mouse antihistidine MAb, respectively. Lanes M, molecular size markers.
Characterization of MAbs.
A panel of hybridoma clones secreting MAbs to the H5 antigen was generated by screening supernatants by an Sf-9 based IFA. The highest antibody titers in the IFA were obtained with MAbs 3D4 and 8B6, and these were thus selected for subsequent experiments.
The specific recognition of both native HA1 of AIV H5 and rHA1 by MAb 3D4 was demonstrated in the Western blot (Fig. 2A), identical to the results for the guinea pig monospecific antiserum against H5N1 rHA1 (Fig. 2B). Additionally, after the staining of cells with MAbs 3D4 and 8B6, AIV H5-infected MDCK cells and recombinant baculovirus-infected Sf-9 cells yielded positive cytoplasmic immuofluorescence patterns, identical to those obtained with rabbit anti-H5N1 serum. Mock H9N2-infected MDCK cells and Sf-9 cells did not give a fluorescence signal (Fig. 3). The isotypes of MAbs 3D4 and 8B6 were determined to be IgG1 and IgM, respectively. Both MAbs 3D4 and 8B6 reacted with H5 AIV, but MAb 8B6 showed a stronger reactivity than MAb 3D4 when they were each used at a concentration of 2.0 μg/ml (see Fig. 5A). MAb 8B6 reacted against the confirmation epitope, and it also possessed HI activity (1:32), whereas MAb 3D4 did not. In addition, MAb 3D4 could be used as the capture antibody to develop a dot blot assay for the detection of H5N2 and H5N3 because it also specifically reacted with the two H5 subtypes viruses (Fig. 4).
FIG. 2.
Recognition of H5 AIV by MAb 3D4 and guinea pig monospecific serum against rHA1 by Western blotting. AIV H5N1/PR8, H5N2, and H5N3 purified from allantoic fluid by centrifugation were analyzed by SDS-PAGE and immobilized onto a nitrocellulose membrane. No-virus (negative control) H7N1 HA was not recognized by the antiserum (MAb 3D4 and anti-rHA1), which shows the specificities of the antibodies for the H5 subtypes.
FIG. 3.
Recognition of native HA in AIV H5-infected MDCK cells and baculovirus-expressed rHA1 (Bac/HA1) by MAbs 3D4 and 8B6 by IFA. MDCK and Sf-9 cells were infected with the H5 subtypes and recombinant baculoviruses, respectively. The controls were H9N2-infected MDCK cells and Sf-9 cells.
FIG. 5.
Reactivities of capture and detector antibodies in AC-ELISA format. (A) Equal amounts (1,000 TCID50s) of H5N1/PR8, H5N2, and H5N3 were used in the assay. Both MAbs 3D4 and 8B6 could react with the H5 subtypes, whereas MAb 8B6 possessed a stronger capability of binding to live viruses, and use of the combination of the two MAbs gave higher absorbances. (B) Different concentrations of purified IgG (from a 1:10 dilution to a 1:640 dilution; the concentrations of IgG were 3,200 ng, 1,600 ng, 800 ng, 400 ng, 200 ng, 100 ng, and 50 ng per well, respectively) and approximately 200 ng of rHA1 protein per well was used as the detector antibody in the AC-ELISA.
FIG. 4.
Recognition of AIV H5N2, H5N3, H7N1, and H9N2 (HA titers, 256) by MAb 3D4. The membrane was dotted with a twofold dilution of purified MAb 3D4, followed by incubation with AIV harvested from allantoic fluid, purified guinea pig anti-rHA1 serum, and finally, FITC-conjugated antibodies. The membrane was developed by using DAB as the substrate.
Combination of MAbs in AC-ELISA.
The MAbs and polyclonal antibodies were used interchangeably as capture and detector antibodies in order to optimize the AC-ELISA. When the microtiter plate was coated with guinea pig anti-rHA1 IgG, a much lower absorbance was recorded compared to that recorded when the microtiter plate was coated with MAb as the capture antibody, Therefore, the MAbs were used as the capture antibody, while polyclonal IgG served as the detector antibody.
MAbs 3D4 and 8B6 were evaluated alone or in combination for their abilities to capture antigen efficiently. Different concentrations of MAbs (500 ng, 250 ng, 150 ng, 100 ng, 50 ng, and 25 ng) were used before the optimal concentration was confirmed. MAb 8B6 showed stronger reactivity than MAb 3D4 in the ELISA. However, the combination of MAbs 3D4 and 8B6, used as capture antibodies, gave stronger detection signals than either of the MAbs alone (Fig. 5A). After checkerboard titration, the optimal antibody concentrations for the capture ELISA were determined to be 100 ng per well for each MAb as the capture antibody and 800 ng per well for guinea pig anti-rHA1 IgG as the detector antibody. The signal-noise ratio obtained by using 1,000 50% tissue culture infective doses (TCID50s) of either H5N1, H5N2, or H5N3 compared to that obtained by using allantoic fluid were 5.38, 9.72, and 8.6, respectively, indicating that infected samples are readily distinguishable from uninfected samples by this assay.
Reactivity of guinea pig anti-rHA1 IgG.
Purified guinea pig anti-rHA1 IgG reacted specifically with the AIV H5 subtypes and rHA1 in the ELISA format (Fig. 5B). The absorbance was proportional to the concentrations used in the ELISA. The specificity of the antiserum was further confirmed by Western blot assay with AIV H5 virus (data not shown).
Determination of analytical specificity.
AIV subtypes H5N1/PR8, H5N2, and H5N3 in allantoic fluid could be detected by our AC-ELISA, whereas other AIV subtypes, such as H3N2, H4N1, H7N1, and H9N2, did not yield positive results (Fig. 6). This indicated the absence of false-positive results with other subtypes of AIVs.
FIG. 6.

Specificity of AC-ELISA. Equal amounts (1,000 TCID50s) of H5 subtype and non-H5 subtype viruses were tested by the AC-ELISA. Numbers represent the mean absorbances from triplicate wells. The dotted line indicates the cutoff value.
The absorbances of the H9N2-infected chicken tracheal swabs collected from days 1 to 7 after infection and the negative control chicken tracheal swabs, also collected from days 1 to 7, were determined. The means ± 2 SDs were calculated for the OD values of each control type. Not much difference was found between the means for the H9N2-infected control chickens (0.178 ± 0.072) and the noninfected chickens (0.152 ± 0.068), while RT-PCR-positive samples were detected 3 days after infection, indicating that no false-positive results were observed by the AC-ELISA for the detection of non-H5 AIV.
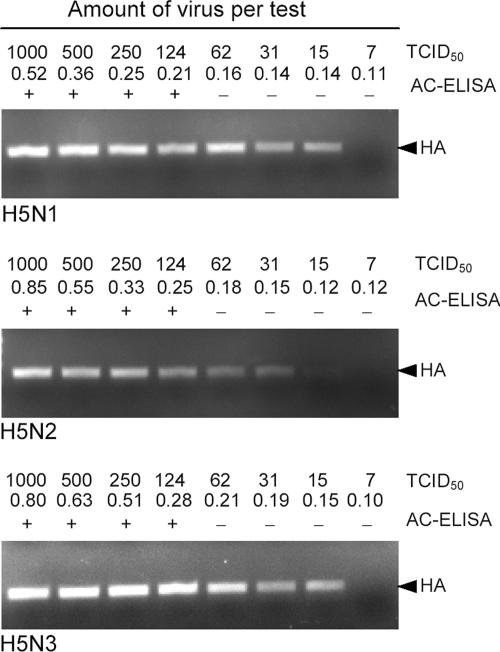
Determination of analytical sensitivity.
On the basis of the cutoff value, our AC-ELISA could detect 124, 62, and 31 TCID50s of the H5N1/PR8, H5N2, and H5N3 viruses in allantoic fluid, respectively (Fig. 7A), and as little as 62.5 ng of purified rHA1 (Fig. 7B). The coefficient values for H5 detection were 0.9952, 0.9989, and 0.9997, respectively, indicating a good corelationship between the values for H5 detection and the standard curve for rHA1 detection.
FIG. 7.

Sensitivity of AC-ELISA. (A) Detection limits of H5N1/PR8 (⧫), H5N2 (▪), and H5N3 (▴); (B) detection limit for rHA1. Filled bars, means of absorbance from three independent tests; error bars, SDs; dotted lines, cutoff values.
Detection of H5N1/PR8, H5N2, and H5N3 in clinically reconstituted samples.
The AIV H5 subtypes were consistently detected in reconstituted clinical samples. The minimum detection limits of H5N1/PR8, H5N2, and H5N3 in reconstituted samples were also 124, 62, and 31 TCID50s of virus, respectively (Fig. 8), the same as those obtained in the sensitivity tests described above. These results were further confirmed by a RT-PCR. In the case of H5N1/PR8 and H5N2, the RT-PCR was more sensitive than the AC-ELISA because for the AC-ELISA-negative samples, the viruses could be detected by RT-PCR.
FIG. 8.
Detection of reconstituted samples by AC-ELISA and RT-PCR in parallel. The absorbance obtained by testing each dilution of the H5 subtypes by AC-ELISA and the positive or negative results are given according to the cutoff value. The 479-bp HA fragment was detected by RT-PCR.
DISCUSSION
To improve the ability to detect influenza virus as well as for disease control, laboratories need more rapid and less cumbersome methods for the direct identification of the AIV H5 subtype in clinical samples. However, the currently available antigen detection methods are deficient in their abilities to differentiate subtypes of AIVs, which might cause unnecessary concerns over non-H5 AIV infections. Of the numerous techniques developed for the rapid diagnosis of viral infections in recent years, the AC-ELISA provides a platform capable of mass screening of clinical samples. It also offers well-documented advantages over more traditional antigen detection methods, such as immunofluorescence assays, which rely on the inoculation of clinical samples into MDCK cells or embryonated eggs, and the hemagglutination assay, which may lead to false-negative results due to the inactivation of viruses.
The availability of an MAb with strong reactivity to the target antigen is a crucial component for AC-ELISA development. Due to the possible presence of both conformational and linear HA antigens from live viruses or inactivated and lysed viruses in clinical samples, the recognition of the two forms of the HA antigens by MAbs is extremely important for successful detection. In this study, the gene encoding the H5N1 HA1 protein was cloned from an inactivated highly pathogenic H5N1 strain isolated in Guangdong, China. Subsequently, H5N1 rHA1 was expressed, and a denatured purified protein was used to generate MAbs. One of the resultant MAbs, MAb 3D4, could react with denatured rHA1 and three H5 viruses, but it did not possess HI activity, which indicated that 3D4 was binding to a linear epitope on the HA antigen. Meanwhile, purified live H5N2 viruses were used to immunize mice for the production of MAbs against conformational epitopes on the HA antigen. The use of H5N2 viruses and not H5N3 viruses was based on (i) the observation that good protection against H5N1 infection in chickens could be conferred by an H5N2 inactivated vaccine, indicating the similarity of the HA proteins between H5N2 and H5N1, and (ii) the fact that more disease outbreaks caused by H5N2 than by H5N3 have been documented recently. After screening of hybridomas, numerous MAbs with HI or neutralization activity were produced. Among these MAbs, MAb 8B6 possessed the highest HI titer and showed the strongest ability to recognize H5N1/PR8, H5N2, and H5N3. However, it did not bind either to denatured HA1 protein in the AC-ELISA or to H5 subtypes in Western blots. This indicated that MAb 8B6 reacted with a conformational epitope.
To acquire the strongest signal for H5 detection by the AC-ELISA, different combinations of MAbs were evaluated. It was found that a combination of MAb 3D4 and MAb 8B6 as capture antibodies could give higher OD readings for the detection of three H5 AIVs than any other combinations or either MAb 3D4 alone or MAb 8B6 alone. It was assumed that MAbs 3D4 and 8B6 were directed to different epitopes on the HA1 protein or that MAbs 3D4 and 8B6 recognized epitopes on HA1 and HA2, respectively. However, this needs further investigation, for example, by epitope mapping. Furthermore, subtyping analysis demonstrated that MAbs 3D4 and 8B6 belong to the IgG1 and IgM subclasses, respectively. IgG is a monomer and has 2 epitope-binding sites, while IgM is a pentamer and has 10 epitope-binding sites. Hence, use of the combination of MAbs 3D4 and 8B6 in the AC-ELISA could increase the number of epitope-binding sites compared to the number obtainable with a single MAb. Moreover, an MAb that recognizes conformational epitopes maintains important biological functions, such as HI and neutralization activities, while an MAb that recognizes a linear epitope could also meet diagnostic requirements (31). Therefore, the application of MAbs 3D4 and 8B6 in combination might contribute greatly to the sensitivity of the AC-ELISA since it could recognize both kinds of epitopes. It is expected that the two MAbs could also be used to develop other immunological methods for the detection of H5 viruses, for instance, by dot blot and in situ hybridization. Furthermore, our AC-ELISA could detect the HA antigens from both poultry and human isolates of H5N1, although this will require more clinical trials.
Compared to the sensitivity for H5N2 and H5N3 detection, a twofold lower sensitivity for H5N1/PR8 detection was observed. This may be explained, first, by differences in the HA proteins between viruses. MAb 3D4 was produced from mice immunized with the denatured HA1 protein of a goose-derived AIV H5N1 strain in China, and H5N1/PR8 is a human influenza virus vaccine candidate, constructed by reverse genetics, and carries the HA and neuraminidase genes of AIV H5N1 isolated from an infected human in Vietnam. Therefore, some minor differences might exist between the HA proteins of the two different H5N1 strains. Second, the differences in sensitivity may be explained by the inability of an MAb to bind to conformation epitopes. Immunization of mice with a denatured protein may not lead to the production of an MAb against a conformational epitope. The way to address these questions is to produce an MAb against the H5N1 HA protein by immunization of mice with live highly pathogenic H5N1 or attenuated H5N1/PR8 in an animal biosafety level 3 laboratory.
Due to the strict regulations that are applied to chicken infection experiments with highly pathogenic H5N1 and the lack of virus shedding in H5N1/PR8-infected chickens (19), we spiked three subtypes of H5 viruses into pharyngeal-tracheal swab specimens from healthy chickens to mimic clinical samples. The successful detection of AIV H5 in reconstituted samples, which was further confirmed by multiplex RT-PCR, and no false-positive signals for H9N2 in chicken swabs confirmed the potential clinical use of the of AC-ELISA. We developed an MAb-based AC-ELISA for the specific detection of AIV H5 subtypes. The AC-ELISA can be incorporated into a rapid dipstick-type diagnostic test, which enables untrained staff to perform the test for the diagnosis of virus infection. This paper describes a cost-effective H5 antigen detection method with a good specificity and a high sensitivity. It can be completed within 3 to 4 h, thus providing an alternative for the clinical detection of AIV H5 infections.
Acknowledgments
We thank Liu Jue and Lu Liqun for helpful discussions and technical assistance.
Footnotes
Published ahead of print on 7 March 2007.
REFERENCES
- 1.Bano, S., K. Naeem, and S. A. Malik. 2003. Evaluation of pathogenic potential of avian influenza virus serotype H9N2 in chickens. Avian Dis. 47(3 Suppl.):817-822. [DOI] [PubMed] [Google Scholar]
- 2.Boivin, G., L. Hardy, and A. Kress. 2001. Evaluation of a rapid optical immunoassay for influenza viruses (FLU OIA TEST) in comparison with cell culture and reverse transcription PCR. J. Clin. Microbiol. 39:730-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reference deleted.
- 4.Centers for Disease Control and Prevention and National Institutes of Health. 1999. Biosafety in microbiological and biomedical laboratories, 4th ed. U.S. Government Printing Office, Washington, DC.
- 5.Chen, H., G. J. D. Smith, S. Y. Zhang, K. Qin, J. Wang, K. S. Li., R. G. Webster, J. S. M. Peiris, and Y. Guan. 2005. H5N1 virus outbreak in migratory waterfowl. Nature 436:191-192. [DOI] [PubMed] [Google Scholar]
- 6.Reference deleted.
- 7.Reference deleted.
- 8.Gallgher, S., S. E. Winston, S. A. Fuller, and J. G. R. Hurrell. 2004. Immunoblotting and immunodetection, p. 10.8.1-10.8.24. In F. M. Ausubel, R. Brent, R. E. Kingston, D. D. Moore, J. G. Seidman, J. A. Smith and K. Struhl (ed.), Current protocols in molecular biology. John Wiley & Sons, Inc., Newcastle, United Kingdom.
- 9.Goldstein, M. A., and N. M. Tauraso. 1970. Effect of formalin, beta-propiolactone, merthiolate, and ultraviolet light upon influenza virus infectivity chicken cell agglutination, hemagglutination, and antigenicity. Appl. Microbiol. 19:290-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reference deleted.
- 11.Kaiser, L., M. S. Brisones, and F. G. Hayden. 1999. Performance of virus isolation and Directigen®FLU A to detect influenza A virus in experimental human infection. J. Clin. Virol. 14:191-197. [DOI] [PubMed] [Google Scholar]
- 12.Reference deleted.
- 13.Reference deleted.
- 14.Lee, C. W., D. A. Senne, and D. L. Suarez. 2004. Effect of vaccine use in the evolution of Mexican lineage H5N2 avian influenza virus. J. Virol. 78:8372-8381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee, S., P. Chang, J. Shien, M. Cheng, and H. Shieh. 2001. Identification and subtyping of avian influenza viruses by reverse transcription-PCR. J. Virol. Methods 97:13-22. [DOI] [PubMed] [Google Scholar]
- 16.Li, J., S. Chen, and D. H. Evans. 2001. Typing and subtyping influenza virus using DNA microarrays and multiplex reverse transctiptase PCR. J. Clin. Microbiol. 39:696-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu, J., H. Xiao, F. Lei, Q. Zhu, K. Qin, X.-W. Zhang, X.-L. Zhang, D. Zhao, G. Wang, Y. Feng, J. Ma, W. Liu, J. Wang, and G. F. Gao. 2005. Highly pathogenic H5N1 influenza virus infection in migratory birds. Science 309:1206. [DOI] [PubMed] [Google Scholar]
- 18.Reference deleted.
- 19.Nili, H., and K. Asasi. 2003. Avian influenza (H9N2) outbreak in Iran. Avian Dis. 47(3 Suppl.):828-831. [DOI] [PubMed] [Google Scholar]
- 20.Reference deleted.
- 21.Selleck, P. W., S. L. Lowther, G. M. Russell, and P. T. Hooper. 2003. Rapid diagnosis of highly pathogenic avian influenza using pancreatic impression smears. Avian Dis. 47(3 Suppl.):1190-1195. [DOI] [PubMed] [Google Scholar]
- 22.Spackman, E., and D. A. Senne. 2002. Development of a real time reverse transcriptase PCR assay for type A virus and the avian H5 and H7 hemagglutinin subtypes. J. Clin. Microbiol. 40:3256-3260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subbarao, K., H. Chen, D. Swayne, L. Mingay, E. Fodor, G. Brownlee, X. Xu, X. Lu, J. Katz, N. Cox, and Y. Matsuoka. 2003. Evaluation of a genetically modified reassortant H5N1 influenza a virus vaccine candidate generated by plasmid-based reverse genetics. Virology 35:192-200. [DOI] [PubMed] [Google Scholar]
- 24.Thanawongnuwech, R., A. Amonsin, R. Tantilertcharoen, S. Damrongwatanapokin, A. Theamboonlers, S. Payungporn, K. Nanthapornphiphat, S. Ratanamungklanon, E. Tunak, T. Songserm, V. Vivatthanavanich, T. Lekdumrongsak, S. Kesdangsakonwut, S. Tunhikorn, and Y. Poovorawan. 2005. Probable tiger-to-tiger transmission of avian influenza H5N1. Emerg. Infect. Dis. 11:699-701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Borm, S., I. Thomas, G. Hanquet, B. Lambrecht, M. Boschmans, G. Dupont, M. Decaestecker, R. Snacken, and T. Van den Berg. 2005. Highly pathogenic H5N1 influenza virus in smuggled Thai eagle, Belgium. Emerg. Infect. Dis. 11:702-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. 2004. Laboratory biosafety manual, 3rd ed. World Health Organization, Geneva, Switzerland.
- 27.Reference deleted.
- 28.World Health Organization. 2005. Inter-country consultation on influenza A/H5N1 in Asia. www.who.int/csr/disease/avian_influenza.
- 29.World Health Organization. 2005. Evolution of H5N1 avian influenza viruses in Asia. Emerg. Infect. Dis. 11:1515-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reference deleted.
- 31.World Health Organization, Collaborating Centre for Reference and Research on Influenza. 2005. Reagents for influenza virus diagnosis. www.influenzacentre.org.
- 32.Reference deleted.
- 33.Yokoyama, W. M. 2001. Production of monoclonal antibody, p. 2.5.1-2.5.17. In J. E. Coligan, A. M. Kruisbeek, D. H. Margulies, E. M. Shevach, and W. Strober (ed.), Current protocols in immunology. John Wiley & Sons, Inc., Newcastle, United Kingdom.