Abstract
Bacillus anthracis is the causative agent of anthrax, a disease that affects wildlife, livestock, and humans. Protection against anthrax is primarily afforded by immunity to the B. anthracis protective antigen (PA), particularly PA domains 4 and 1. To further the development of an orally delivered human vaccine for mass vaccination against anthrax, we produced Salmonella enterica serovar Typhimurium expressing full-length PA, PA domains 1 and 4, or PA domain 4 using codon-optimized PA DNA fused to the S. enterica serovar Typhi ClyA and under the control of the ompC promoter. Oral immunization of A/J mice with Salmonella expressing full-length PA protected five of six mice against a challenge with 105 CFU of aerosolized B. anthracis STI spores, whereas Salmonella expressing PA domains 1 and 4 provided only 25% protection (two of eight mice), and Salmonella expressing PA domain 4 or a Salmonella-only control afforded no measurable protection. However, a purified recombinant fusion protein of domains 1 and 4 provided 100% protection, and purified recombinant 4 provided protection in three of eight immunized mice. Thus, we demonstrate for the first time the efficacy of an oral S. enterica-based vaccine against aerosolized B. anthracis spores.
Bacillus anthracis is the causative agent of anthrax, a disease that affects wildlife, livestock, and humans. The ability of B. anthracis to cause disease is dependent on the production of a polyglutamic acid capsule, which provides resistance to phagocytosis and to the production of anthrax toxins. The toxins consist of three proteins—protective antigen (PA), edema factor (EF), and lethal factor (LF)—which act in binary combinations (20). PA and EF together produce the edema toxin, whereas PA and LF together produce the lethal toxin. Protection against anthrax is considered to be due mainly to the immune response to PA. Specifically, research into mechanisms associated with the efficacy of current anthrax vaccines has led to the conclusion that PA is essential and a dominant component of the vaccines since the protein can elicit effective protective immunity in the absence of LF and EF (19, 26).
The current licensed United Kingdom and U.S. anthrax vaccines for human use consist of cell-free filtrates of a nonencapsulated but toxigenic B. anthracis derivative, adsorbed to alum (U.S. vaccine) or aluminum hydroxide (United Kingdom vaccine). Although effective in animal studies, these vaccines must be administered by needle in multiple doses over several months, with annual boosters to maintain continuous protection (1). In addition to occasional cases of adverse local reactions, the vaccines are expensive to produce, have a limited shelf life as a consequence of their formulation, and are currently only available to military personnel. There is a need to develop vaccines capable of protecting both military and civilian populations, which poses challenges in terms of the general health of these populations, compliance, and the ability to mass vaccinate in the event of an attack. Therefore, improvements to increase the efficacy, longevity, and safety of the anthrax vaccine are warranted. A subunit vaccine consisting of purified recombinant PA protein adsorbed to aluminum hydroxide has been proposed (24) but will suffer from the drawbacks of limited ambient stability and the need to be administered by needle.
One approach to the development of an improved next-generation anthrax vaccine involves the use of live attenuated Salmonella vaccines to deliver PA. This approach offers a number of advantages (12). First, live Salmonella vaccines can be given orally (the natural route of infection), enabling a noninvasive route of vaccine administration. Second, both mucosal and systemic immune responses can be elicited, which may be important for protection against airborne infection. In addition, live attenuated Salmonella vaccines are able to simulate both humoral and cellular immune responses that may be important for protection against disease. Since the live attenuated Salmonella vaccine strain Ty21a (14) is licensed for human use and other next-generation attenuated Salmonella strains are in clinical trials (12), it should also be possible to develop safe recombinant Salmonella vaccines for licensure. Finally, since Salmonella is genetically tractable, recombinant Salmonella vaccines are relatively easy to develop and are also relatively cost-effective to produce.
Preliminary studies evaluating the use of attenuated Salmonella for delivery of PA have been reported (4, 13). Initially, PA was expressed in Salmonella from a high-copy-number plasmid, leading to high-levels of PA in vitro but plasmid instability in vivo and low colonization of the host tissues by the bacteria (4). More recently, a lower-copy-number plasmid was used to express PA as a fusion to the Escherichia coli hemolysin (Hly) export system in order to enable export of the expressed PA protein from the Salmonella (13). This plasmid was also found to be unstable, perhaps as a consequence of the high metabolic load placed upon the bacteria in continuously producing both the Hly export proteins and PA. However, when the Hly-PA fusion was integrated into the Salmonella chromosome, the resulting recombinant was able to provide protection against an injected anthrax spore challenge if administered via the intravenous route and not by the oral route.
We considered a number of approaches that would allow us to realize our goal of devising an orally delivered Salmonella vaccine which would provide protection against airborne B. anthracis. The use of an inducible promoter to selectively express PA in vivo coupled with a stabilized plasmid-based expression system would promote an enhanced immune response. In addition, we considered that expression only of the domains of PA which are associated with protective immunity (6) could allow the generation of a more stable recombinant. Recently, Galen et al. described the use of the S. enterica serovar Typhi cytolysin A (ClyA) export system for delivery of a domain of PA in Salmonella, improving the immunogenicity of PA compared to cytoplasmic expression (11). This ClyA export apparatus requires only the fusion of proteins to the 34-kDa ClyA protein, making it attractive and simple to use for the secretion of proteins from Salmonella.
In the present study, attenuated Salmonella strains expressing PA, domain 4 of PA, or a fusion protein of domains 1 and 4 of PA were produced and compared for immunogenicity and protective efficacy against aerosolized B. anthracis spores.
MATERIALS AND METHODS
Bacterial strains, plasmids, and growth conditions.
S. enterica serovar Typhimurium SL3261 (aroA mutant), an attenuated amino acid-dependent strain, and S. enterica serovar Typhimurium LB5010, used for methylation of E. coli-derived plasmids prior to transformation of strain SL3261, were taken from laboratory stocks (Dstl Porton Down, United Kingdom). E. coli TOP10F′ or E. coli DH5α cells (Invitrogen) were used for plasmid maintenance and E. coli BL21(DE3)/pLYsS cells were used for protein expression. Plasmid pVDL9.3PA83ec encoding an E. coli codon-optimized PA gene of B. anthracis (13) was used as a template DNA for PCR. The pCR2.1-TOPO plasmid vector (Invitrogen, United Kingdom) was used to clone PCR products. Plasmid pGEX-6-P3 (Amersham-Pharmacia) was used to express proteins as fusions to N-terminal glutathione S-transferase (GST). Bacterial strains were cultured aerobically on Luria agar or in Luria broth supplemented with ampicillin (100 μg/ml), kanamycin (10 μg/ml), or chloramphenicol (25 μg/ml), as appropriate, at 37°C and with agitation at 180 to 200 rpm or statically. Similarly, strain SL3261 was routinely supplemented with 1% (vol/vol) “aromix” comprising 4 mg of phenylalanine/ml, 4 mg of tryptophan/ml, 1 mg of para-aminobenzoic acid (PABA)/ml and 1 mg of dihydroxybenzoic acid/ml (adapted from Chatfield et al. [3]).
The growth rates of the recombinant Salmonella strains were determined by culturing the bacteria for 24 h in Luria broth containing antibiotic selection and enumerating them on Luria agar containing antibiotics. To establish the stability of the strains in vitro, the recombinant bacteria were cultured over 72 h, with passage every 24 h, in the absence of antibiotic (equivalent to culturing the bacteria for approximately 44 generations), and the stability of the plasmids within the Salmonella was calculated by enumeration of bacteria on Luria agar with or without antibiotic selection. Inocula were produced by culturing the recombinant Salmonella strains statically overnight at 37°C, harvesting the bacteria by centrifugation (7,000 × g for 20 min at 4°C), and then washing and resuspending the bacteria in sterile phosphate-buffered saline (PBS). The inoculum dose was verified by plating serial dilutions of each culture on Luria agar supplemented with antibiotic, where appropriate.
Mice.
Female A/Jola (A/J) mice (supplied and used at 8 to 12 weeks of age; Harlan UK, Ltd.) were used for all studies since these mice provide a consistent mouse model for infection with a toxigenic nonencapsulated (Tox+ Cap−) strain of B. anthracis (32). All animal procedures strictly adhered to the Animals (Scientific Procedures) Act of 1986.
Construction of recombinant Salmonella strains expressing PA domains.
All methods for DNA manipulation were carried out according to the method of Sambrook et al. (29) unless otherwise stated. Taq DNA polymerase (Invitrogen) or Vent DNA polymerase (New England Biolabs) were used in the PCRs.
(i) Construction of expression plasmid pSEC10.
A new expression plasmid was derived by using the origin of replication from pSC101 (2), which normally exists at five copies per chromosomal equivalent. The primers used are listed in Table 1, and the essential plasmids created from these primers are listed in Table 2. First, an ori101 replication cassette was synthesized by PCR using primers 1 and 2 with pSC101 as a template, generating a 1,949-bp BamHI-AvrII fragment. This fragment was inserted into the pBR322-derivative pGEN2, cleaved with BglII-AvrII to create pGEN4. The authenticity of this PCR product was confirmed by nucleotide sequencing the cloned DNA. Construction of pGEN132 was accomplished by removal of the ori101 cassette from pGEN4 as a 2,638-bp BamHI fragment and insertion into pJN5 digested with BglII and BamHI, thereby regenerating the gfpuv gene encoding the green fluorescent protein allele GFPuv (BD Biosciences/Clontech) under an osmotically controlled PompC promoter. Final assemblage of a pSC101-derived expression plasmid containing a complete plasmid maintenance system (9) was achieved by introduction of parA from pJN8. A 4,469-bp BamHI-SpeI cassette from pJN8 containing bla, hok-sok, and parA was ligated to the 2,649-bp BamHI-SpeI ori101 cassette from pGEN132 to regenerate gfpuv and create pGEN206. The β-lactamase cassette of pGEN206 was replaced by partial cleavage with SpeI, complete digestion with XbaI, and replacement of the resulting 1,181-bp bla gene with a previously described 1,046-bp NheI fragment encoding resistance to kanamycin (11), creating pEXO5. Finally, the clyA cassette was cleaved from pSEC91 (11) as an XhoI-AvrII fragment and ligated into pEXO5 digested with XhoI-AvrII to generate pSEC10.
TABLE 1.
Primers used in this study
| Primer | Oligonucleotide sequencea | Template |
|---|---|---|
| 1 | 5′-GTCTGCCGGATTGCTTATCCTGGCGGATCCGGTTGACAGTAAGACGGGTAAGCCTGTTGAT-3′ | pSC101 |
| 2 | 5′-CCTAGGTTTCACCTGTTCTATTAGGTGTTACATGCTGTTCATCTGTTACATTGTCGATCTG-3′ | pSC101 |
| PA83/F1 | 5′-CACGCTAGCGAAGTAAAGCAAGAGAACCGTCTGC-3′ | pVDL9.3PA83ec |
| PA83/R1 | 5′-CACGCTAGCACCGATCTCGTAACCTTTCTTGGAG-3′ | pVDL9.3PA83ec |
| DOM4/F2 | 5′-CACGCTAGCTTCCACTACGATCGTAATAACATCGC-3′ | pVDL9.3PA83ec |
| DOM1/R2 | 5′-CACGCTAGCCGCAGCAACCAGTGGATGGCGTG-3′ | pVDL9.3PA83ec |
| LINK/F1 | 5′-TTCCACTACGATCGTAATAACATCGC-3′ | pVDL9.3PA83ec |
| LINK/R1 | 5′-GATGTTATTACGATCGTAGTGGAAGGCAGCTGGACCTGGACCCGCAGCAACCAGTGGATGGCGTGCTT-3′ | pVDL9.3PA83ec |
| PA83/F4 | 5′-GTGTTGGGATCCGAAGTAAAGCAAGAGAACCGTCTG-3′ | pVDL9.3PA83ec |
| PA83/R4 | 5′-GTGTTGCTCGAGTTATTAACCGATCTCGTAACCTTTCTTGGA-3′ | pVDL9.3PA83ec |
Boldface type denotes a linker sequence(s). Underlining denotes a region cleaved by restriction endonucleases.
TABLE 2.
Selected plasmids used in this study
| Plasmid | Size (kb) | Relevant genotype | Source or reference |
|---|---|---|---|
| pJN5 | 3.1 | oriE1 gfpuv bla | 8 |
| pJN8 | 5.4 | oriE1 gfpuv bla hok-sok parA | 8 |
| pGEN2 | 4.2 | oriE1 gfpuv tetA hok-sok | 8 |
| pSC101 | 9.3 | ori101 tetA par | 1 |
| pGEN4 | 5.6 | ori101 gfpuv tetA hok-sok | This study |
| pGEN132 | 4.8 | ori101 gfpuv bla par | This study |
| pGEN206 | 7.1 | ori101 gfpuv bla par hok-sok parA | This study |
| pEXO5 | 7.0 | ori101 gfpuv aph par hok-sok parA | This study |
| pSEC91 | 7.6 | ori15A clay tetA aph hok-sok par parA | 9 |
| pSEC10 | 7.2 | ori101 clyA aph hok-sok par parA | This study |
(ii) Cloning of PA domains into pSEC10.
An adaptation of a fusion PCR protocol (18) was used to create a 1,212-bp fusion of DNA encoding PA domain 1 (PA1) and PA domain 4 (PA4). First, the PA1 and PA4 domains were amplified separately in 50-μl reactions using primers (PA83/F1 and LINK/R1 for PA1 and LINK/F1 and PA83/R1 for PA4; Table 1) designed to create a linker (GGC AGC TGG ACC TGG ACC) between the individual domains with NheI restriction digestion sites at the 5′ end of PA1 and the 3′ end of PA4. Plasmid pVDL9.3PA83ec (13) was used as the DNA template. Subsequently, a 50-μl “fusion” PCR was prepared incorporating 1 μl each of the PA1 and PA4 PCR products and using the flanking primers PA83/F1 and PA83/R1 containing NheI sites (Table 1). In addition, DNA encoding either PA4 and the full-length PA gene (PA1-4) was PCR amplified using appropriate primers (DOM4/F2 and PA83/R1 for PA4 and PA83/F1 and PA83/R1 for PA1-4; Table 1) containing NheI sites. The resulting PCR products were cloned into the pCR2.1-TOPO vector. Subsequently, the PA insert cassettes were cleaved from the TOPO vectors as NheI subcloned into the NheI site of pSEC10, generating ClyA-PA domain fusions downstream of the PompC promoter. The authenticity of all of the PCR products detailed above was confirmed by nucleotide sequencing of the appropriate cloned DNA.
(iii) Transformation of Salmonella.
The pSEC10 derivatives were transformed into E. coli, and individual transformants were screened for expression of the ClyA-PA proteins by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and Western blotting of colony lysates (see below) and one positive clone for each plasmid construct was electroporated into S. enterica serovar Typhimurium SL3261 via passage through S. enterica serovar Typhimurium LB5010, an intermediate host strain required for methylation of the plasmid DNA. In addition, plasmid pVDL9.3PA83ec, encoding full-length PA fused to the Hly export system and conferring resistance to chloramphenicol (13), was transformed into SL3261 for comparison.
Detection of PA expression.
Recombinant Salmonella was cultured in L broth supplemented with antibiotic selection for 24 h with agitation. Samples (1 ml) were centrifuged at 13,000 × g for 10 min, and the resulting cell pellets or supernatants were diluted 1:1 in 2× Laemmli buffer then boiled for 5 min. The samples were normalized to 3 × 108 CFU/ml for comparison. To evaluate PA expression, SDS-PAGE on 12.5% (wt/vol) polyacrylamide gels (PhastSystem; Amersham Pharmacia Biotech, Ltd.) and Western blotting on Immobilon-P nitrocellulose membrane (Millipore) was performed. After transfer of proteins from SDS-PAGE gels, membranes were blocked with PBS containing 2% (wt/vol) bovine serum albumin (PBS-BSA), and then probed by using mouse anti-PA4 antibody, 2D4J (produced at DSTL), and a rabbit anti-mouse horseradish peroxidase-conjugated secondary antibody (Sigma-Aldrich). Antibodies were used at 1:2,000 dilutions in PBS-BSA, and membranes were washed using PBS containing 0.05% (vol/vol) Tween 20. Proteins were visualized by using Sigma-Fast 3,3′-diaminobenzidine tablets (DAB peroxidase substrate; Sigma-Aldrich).
Determination of plasmid stability in vivo.
Groups of eight female A/J mice were inoculated with approximately 1 × 109 to 3.8 × 109 CFU of SL3261 or SL3261 recombinants orally by intragastric gavage. On day 8 postinoculation, mice were culled by cervical dislocation and spleens and Peyer's patches (six/mouse) were harvested. The tissues were homogenized in 1 ml of sterile PBS using 50-μm-pore-size cell strainers (Becton Dickinson Labware) and subsequently inoculated onto agar plates with or without antibiotic selection to determine counts of recombinants or total bacteria, respectively, in order to calculate the stability of the plasmids in the Salmonella strains.
Production of PA1+4 protein.
DNA encoding the PA1+4 fusion was PCR amplified from the recombinant the pCR2.1-TOPO vector using primers PA83/F4 and PA83/R4, containing XhoI and BamHI restriction sites (Table 1) and then cloned into the XhoI/BamHI sites of the expression vector pGEX-6-P3 (GE Healthcare) downstream and in frame of the lac promoter, as a fusion to GST. To produce purified recombinant GST-PA1+4 protein, the recombinant plasmid was transformed into E. coli BL21(DES)/pLysS, and transformants were cultured in Luria broth containing 50 μg of ampicillin/ml, 30 μg of chloramphenicol/ml, and 1% (wt/vol) glucose, followed by shaking at 37°C, to an A600 of 0.4 prior to induction with 1 mM IPTG (isopropyl-β-d-thiogalactopyranoside). Cultures were then incubated for a further 4 h, followed by harvesting by centrifugation at 10,000 rpm for 15 min. Cell pellets were resuspended in PBS and sonicated four times for 20 s each time in an ice water bath, and the suspension was centrifuged at 15,000 × g for 30 min. Subsequently, cell supernatants were loaded onto a 5-ml GSTrap 4B column (GE Healthcare) previously equilibrated with PBS. The column was washed with PBS, and the fusion protein was eluted with 20 mM reduced glutathione-50 mM Tris (pH 8). After analysis by SDS-PAGE, fractions containing PA1+4 were pooled and dialyzed into cleavage buffer (50 mM Tris, 150 mM NaCl, 1 mM EDTA, 1 mM dithiothreitol; pH 7). PreScission protease was added at a ratio of 2 U per 100 μg of fusion protein, followed by incubation overnight at room temperature. Cleaved PA1+4 protein was separated from the GST by reapplying to a 5-ml GSTrap 4B column pre-equilibrated with PBS. Unbound fractions containing protein were analyzed by SDS-PAGE, pooled, and dialyzed against PBS. The PA1+4 protein concentration was determined by using a BCA assay (Pierce). Purified recombinant (r) PA1, PA4, and PA1-4 were all produced using the same protocol as described previously (6). Purified proteins were visualized by SDS-PAGE alongside appropriate Bio-Rad molecular weight markers.
Immune response analysis.
Groups of five to eight mice were inoculated orally by intragastric gavage with between 1 × 108 and 5 × 109 CFU of S. enterica serovar Typhimurium SL3261 or SL3261 recombinants on days 0, 14, and 28. Bacteria were centrifuged and resuspended in PBS before dosing. Alternatively, mice were injected via the intramuscular route with 10 μg of purified rPA proteins absorbed to a 20% (vol/vol) solution of 1.3% Alhydrogel (Superfos Biosector a/s, Vedback, Denmark). Subsequently, serum samples were evaluated for immune response analyses.
(i) ELISA.
Serum samples were tested for specific antibody responses by enzyme-linked immunosorbent assay (ELISA) using standard procedures. Blood samples were collected from the tail veins of all immunized and control mice on days 13, 15, 46, and 73 after inoculations on days 0, 14, and 28 and serum was assayed for PA-specific immunoglobulin G (IgG) antibody responses. Ninety-six-well microtiter plates were coated with 5 μg of recombinant PA/ml (produced at Dstl [25]) overnight at 4°C and then washed. All washing steps were carried out with PBS containing 0.02% (vol/vol) Tween 20. Plates were then blocked with 2% (wt/vol) skimmed milk in PBS for 1 h, and each serum sample was serially diluted 1:2 in blocking solution across the plate, followed by a 1-h incubation. Bound antibody was detected by using horseradish peroxidase-conjugated polyclonal goat anti-mouse IgG (Harlan Sera-lab) diluted 1:2,000 in blocking buffer and incubated for 1 h. Plates were developed with 100 μl of ABTS [2,2′ azinobis(3-ethylbenzthiazolinesulfonic acid)]; Sigma-Aldridge) substrate, and the A414 of the plates were measured. All samples were assayed in duplicate. Endpoint antibody titers were expressed as the maximum dilution of sample giving an absorbance or more than 0.1 A414 units, after subtraction of the absorbance due to nonspecific binding detected in control sera from mice immunized with the parent S. enterica serovar Typhimurium SL3261 strain. The results are presented as the reciprocal of the dilution, and the mean represented the average of duplicate values for each samples.
(ii) TNA.
The titer of toxin-neutralizing antibody (TNA) in immune sera was determined based on the ability of the serum to inhibit the cytotoxicity of the combination of PA with LF as described previously (28). Briefly, J774A.1 murine macrophage cells (American Tissue Culture Collection) were harvested and plated out at approximately 3.5 × 104 cells/well in a 96-well microtiter plate, and 40 to 60% confluent layers were allowed to form over a 17- to 19-h period at 37°C in 5% (vol/vol) CO2 as viewed by microscopy. Antisera was prepared in a separate 96-well plates and serially diluted down the plate. A positive control reference sera with a known 50% effective dose was also included, and a nonspecific mouse antisera was used as a negative control. Then, 100 μl of anthrax lethal toxin was added (50 ng of PA/ml and 40 ng of LF/ml) per well, and the plates were incubated for 30 min. Medium was then removed from the J774A.1 cells, and the antiserum-toxin mix was added to the plates (100 μl/well). These were subsequently incubated for 4 h at 37°C in 5% (vol/vol) CO2. Cell viability was determined by the addition of 25 μl of 5 mg of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (Sigma)/ml dissolved in PBS (Gibco). Throughout the assay, wells containing positive and negative controls were randomly checked via microscopy to check cell viability visually; negative control wells contained small, rounded, dead cells, and positive control wells contained living, healthy cells, as expected. The incubation was continued for a further 2 h under the same conditions, and then the reaction was stopped by the addition of a 20% (wt/vol) SDS (Becton-Dickinson) dissolved in 50% (vol/vol) DMF (Becton-Dickinson) in water (Gibco). Plates were then incubated for 16 to 20 h at 37°C in 5% (vol/vol) CO2. The optical density readings of the plates were taken by using MultisKan Ascent microplate photometer (Thermo Labsystems) at 570 and 690 nm as a reference filter. Endpoints were calculated by using SAS software (version 8.2), running an endpoint calculation algorithm developed by the Centers for Disease Control and Prevention. The TNA endpoint is defined as the reciprocal of the serum dilution that gives 50% neutralization of the anthrax lethal toxin, corresponding to the inflection point of a four-parameter logistic-log fit of the neutralization curve. All antisera were tested at least twice by two separate analysts; the results shown are the averages of each individual 50% effective dose from each separate assay performed by each analyst.
B. anthracis spore preparation.
B. anthracis STI (Tox+ Cap−) was cultured on the surface of Roux bottles containing New Sporulation medium (3.0 g of Difco Trypton, 6.0 g of Oxoid bacteriological peptone, 3.0 g Oxoid yeast extract, 1.5 g of Oxoid Lab Lemco, 1 ml of 0.1% MnCl2·4H2O, and 25 g of Difco Bacto agar in 1 liter of distilled H2O) at 37°C until the cultures contained more than 95% phase bright spores, measured by phase-contrast microscopy; typically, incubation of between 7 to 10 days resulted in >95% phase bright spores. Spores were harvested by centrifugation at 10,000 × g for 10 min and then washed 10 times with ice-cold distilled water to remove any vegetative cells and cell debris. The spore preparation was heated at 70°C for 1 h to kill any remaining vegetative cells, and the final spore concentration was determined by serial dilution. Spore preparations were stored at −20°C until required.
Challenge with aerosolized B. anthracis spores.
Aerosol exposure was carried out by using a Henderson-type apparatus (17) and Collison spray (22). Briefly, 10-ml aliquots of STI spores were suspended in sterile distilled water at a concentration of up to 109 CFU/ml, and 3 drops of Antifoam 289 (Sigma) was added just before each preparation was placed in the Collison spray. Groups of mice (heads only) were exposed for 10 min to an air stream containing an aerosol of STI spores generated by the Collison spray and conditioned by the Henderson-type apparatus. The concentration of STI spores in the aerosol was determined by taking samples from the exposure chamber with an all-glass impinger (23) containing sterile distilled water and then plating diluted impinger samples onto nutrient agar to determine the number of spores per liter. The respiratory volume of the animals was calculated by the method of Guyton (15) and the actual dose inhaled and retained in the lungs was calculated by the method of Harper and Morton (16).
Initially, to identify a challenge dose with which to evaluate the Salmonella vaccine candidates, a small dose-finding study was carried out. Briefly, groups of four to five mice were exposed to B. anthracis STI, giving calculated retained doses of approximately 66 CFU, 4.7 × 102 CFU, 5.3 × 103, or 6.3 × 104 CFU. Subsequently, at 9 weeks after the final immunizing dose with Salmonella mice were challenged with B. anthracis STI spores via the aerosol route with a calculated retained dose of approximately 105 CFU for all groups (ranging between 8.5 × 104 and 1.4 × 105 CFU). This is equivalent to approximately 200 median lethal doses by this route (6). The challenge experiment was carried out blinded. Animals were closely observed for 14 days after challenge to determine their protected status. Humane endpoints were strictly observed so that any animal that displayed a collection of clinical signs that indicated a lethal infection (piloerection, posture [hunching], and mobility problems) was culled.
Statistical analysis.
One-way analysis of variance with Tukey's multiple comparison postanalysis test and statistical analysis of survival using the GraphPad Prism version 3.02 for Windows (GraphPad Software, San Diego, CA) were performed.
RESULTS
Construction of Salmonella expressing ClyA-PA fusion proteins.
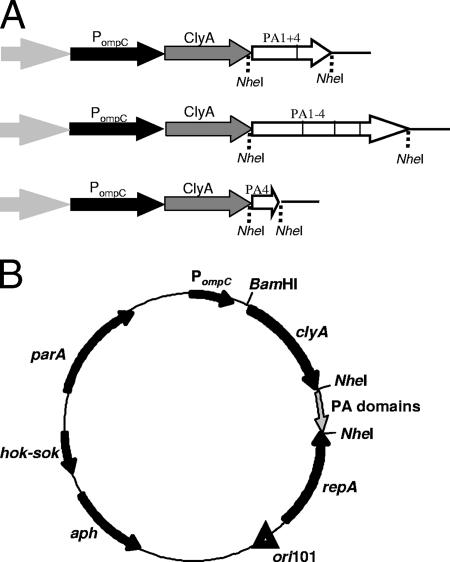
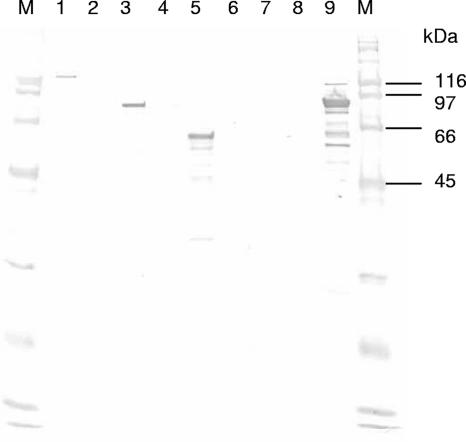
Proteins fused to the carboxyl terminus of the S. enterica serovar Typhi ClyA export apparatus can be expressed at a high level in Salmonella and could be transported out of the bacterial cell without causing lysis (10). Thus, in the present study we chose to evaluate ClyA as an export mechanism for known protective domains of PA expressed in Salmonella. Initially, a plasmid expression vector, pSEC10, was constructed that contained the gene encoding ClyA downstream of the PompC promoter. This plasmid is similar to those previously described by Galen et al. (11) and also included the hok-sok postsegregational killing locus and the parA gene encoding an active partitioning system. A fusion PCR protocol was followed to create a fusion between domain 1 of PA (PA1) and domain 4 of PA (PA4) and the resulting PA1+4 fusion was cloned into the expression plasmid pSEC10 as a fusion to ClyA, resulting in plasmid pSECPA1+4 (Fig. 1). Similar constructs producing ClyA fused to PA4 and full-length PA were also produced and termed pSECPA4 and pSECPA1-4, respectively. The recombinant plasmids containing the ClyA-PA fusions were subsequently transformed into S. enterica serovar Typhimurium SL3261 by electroporation (resulting in strains SL3261/pSECPA1+4, SL3261/pSECPA4, and SL3261/pSECPA1-4). In vitro expression of the ClyA-PA fusion proteins from the strains was detected by SDS-PAGE and Western blotting in whole-cell lysates with a PA4-specific antibody (Fig. 2). However, the ClyA-PA fusion proteins could not be detected in the culture supernatants using this method.
FIG. 1.
PA expression plasmids. (A) Cloning of PA fragments into NheI sites of pSEC10 as fusions to the ClyA gene. (B) General structure of pSEC10-based plasmids encoding PA gene fragments: SL3261/PSECPA1-4 encoding domains 1 to 4 of PA, SL3261/pSECPA1+4 encoding domain 1 and domain 4 of PA, and SL3261/pSECPA4 encoding domain 4 of PA.
FIG. 2.
Expression of PA as ClyA fusions from Salmonella. Normalized cell lysates (3 × 108 CFU/ml) and culture supernatants (either neat or diluted 1:10 as indicated) from S. enterica serovar Typhimurium SL3261 recombinants were subjected to SDS-PAGE and Western blotting with PA4-specific monoclonal antibody. Lane M, Bio-Rad broad-range biotinylated SDS marker; lane 1, SL3261/pSECPA1-4 1:10 cell pellet; lane 2, SL3261/pSECPA1-4 neat supernatant; lane 3, SL3261/pSECPA1+4 1:10 cell pellet; lane 4, SL3261/pSECPA1+4 neat supernatant; lane 5, SL3261/pSECPA4 1:10 cell pellet; lane 6, SL3261/pSECPA4 neat supernatant; lane 7, SL3261/pSEC10 1:10 cell pellet; lane 8, SL3261/pSEC10 neat supernatant; lane 9, 0.1 mg of rPA/ml.
Growth and stability of recombinant Salmonella strains.
The S. enterica serovar Typhimurium SL3261 recombinants containing pSEC10 and pSEC10 derivatives were found to grow similarly to the parental SL3261 strain when cultured in Luria broth over 24 h (data not shown). Furthermore, in vitro, the plasmids were stably maintained (80 to 100% plasmid retention) over 72 h in the absence of antibiotic selection. The in vivo stability of the SL3261 recombinants was assessed by determining the level of colonization of murine tissues. Eight days after intragastric dosing of A/J mice with approximately 109 CFU of the SL3261 recombinants, the spleens and Peyer's patches were removed, and the level of colonization and stability of the bacteria in the tissues was assessed by plating homogenized tissues onto selective or nonselective agar. Similar levels of colonization of spleens by the SL3261 recombinants were found (data not shown), and the plasmids were stably maintained in all of the bacteria isolated from splenic tissues. At the time point tested, the colonization of the Peyer's patches was low although, where there was colonization, the SL3261 recombinants were generally stable. This indicated that the infection had progressed to the deeper tissues such as the spleen.
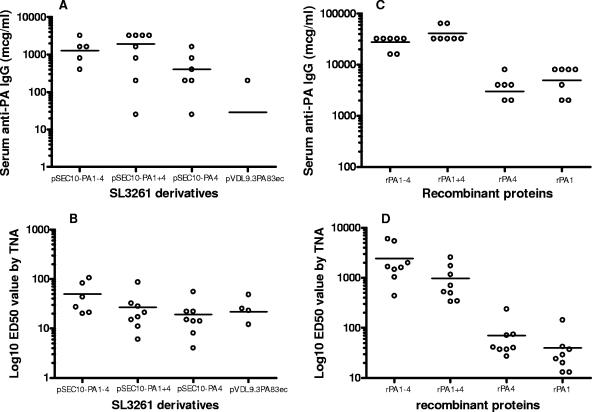
Immunogenicity of Salmonella strains expressing PA.
The immunogenicity of the SL3261 recombinants was assessed after intragastric dosing of A/J mice three times at 2-week intervals with approximately 109 CFU of the bacteria. Serum samples were taken on day 13, 27, 45, or 73 and analyzed by ELISA for PA-specific IgG responses. A progressive increase in PA-specific IgG responses was detected over time in immunized mice (data not shown). After only one or two doses of the SL3261 recombinants, PA-specific IgG antibody responses were generally low. However, on day 73, and prior to challenge with B. anthracis spores, all of the mice immunized with Salmonella expressing PA or fragments of PA had developed PA-specific IgG responses (Fig. 3A). Furthermore, analysis of the sera by TNA demonstrated that antibodies capable of neutralizing anthrax toxin were present in the sera from mice immunized with the recombinant Salmonella (Fig. 3B). Differences in the magnitude of the anti-PA responses were observed in individual mice within the groups, and some individual mice failed to show measurable PA-specific responses. However, in mice showing responses, all groups showed statistically similar toxin-neutralizing activity.
FIG. 3.
Serum immune responses to PA. Serum samples were taken from A/J mice orally immunized three times at 2-week intervals with 1 × 108 to 5 × 109 CFU of S. enterica serovar Typhimurium SL3261 or SL3261 recombinants (A and B) or intramuscularly immunized with 10 μg of PA protein adsorbed to a 20% (vol/vol) solution of Alhydrogel (C and D). Sera were used to determine the IgG (A or C) or TNA (B or D) responses to PA.
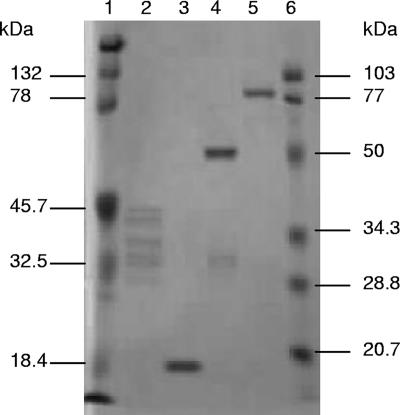
Immunogenicity of rPA proteins.
An expression vector was produced to allow the purification of the PA1+4 fusion protein, and the protein was subsequently purified (Fig. 4) and used, along with rPA1-4, rPA4, and rPA1 (6), for immunization of A/J mice as a comparison to the Salmonella vaccine candidates. Specifically, 10 μg of each recombinant protein was administered along with the adjuvant Alhydrogel three times at 2-week intervals, and serum samples were taken on days 13, 27, 45, and 73 for analysis of the PA-specific IgG responses by ELISA. Similarly to the responses observed with the Salmonella, at days 13, 27, and 45, progressive increases in PA-specific IgG induced by the proteins could be detected (data not shown). On day 73, ELISA of the sera from individual mice showed that all of the recombinant proteins were able to induce PA-specific IgG responses (Fig. 3C). The responses to rPA1-4 and rPA1+4 were approximately 1 log greater than those to rPA4 and rPA1 which, in turn, were greater than the responses to the SL3261 derivatives. Analysis of the sera by TNA demonstrated that the anthrax toxin-neutralizing activity stimulated by the rPA1-4 and rPA1+4 proteins was also greater than that induced by the Salmonella (Fig. 3D).
FIG. 4.
SDS-PAGE analysis of purified recombinant PA proteins. Purified PA proteins (2 μg per 10-μl sample loaded) were subjected to SDS-PAGE. Lane 1, Bio-Rad Kaleidoscope-prestained standards; lane 2, rPA1; lane 3, rPA4; lane 4, rPA1+4; lane 5, rPA1-4; lane 6, Bio-Rad low-range prestained standards.
Protection of mice against an aerosolized B. anthracis challenge.
Initially, an experiment was carried out to determine the concentration of B. anthracis STI spores for use as a lethal challenge to naive mice. Groups of four to five naive A/J mice were exposed to retained doses of between 66 and 6.3 × 104 CFU of aerosolized B. anthracis spores and then monitored for survival. Only the mice given the highest inoculum of 6.3 × 104 CFU completely succumbed to the challenge (data not shown). Thus, this dose was considered the minimum challenge requirement for the subsequent protection experiment.
Mice inoculated with the SL3261 recombinants or the purified recombinant proteins were challenged with approximately 105 CFU (equivalent to approximately 200 mean lethal doses) of aerosolized B. anthracis STI spores and monitored for survival. Naive mice and those given the SL3261 parental control strain succumbed to infection within 6 days, and all mice receiving SL3261/pSEC10, SL3261/pSECPA4, or SL3261/pVDL9.3PA83ec died by day 7 postchallenge (Table 3). However, two of eight mice immunized with SL3261/pSECPA1+4 were protected against the challenge, and five of six mice inoculated with SL3261/pSECPA1-4 also survived. Thus, SL3261/pSECPA1-4 expressing the full-length PA protein as a fusion with ClyA afforded significant protection against aerosolized B. anthracis spore challenge (P < 0.01 compared to SL3261/pSEC10). Mice immunized with rPA1-4, rPA1+4, or rPA4 were solidly protected against challenge, and immunization of mice with rPA1 protected two of six mice from challenge with B. anthracis STI (Table 3).
TABLE 3.
Survival of vaccinated mice challenged with aerosolized B. anthracis STI sporesa
| Inoculum | No. of survivors/total no. |
|---|---|
| SL3261 | 0/8 |
| SL3261/pSEC10 | 0/8 |
| SL3261/PSECPA1-4 | 5/6 |
| SL3261/pSECPA1+4 | 2/8 |
| SL3261/pSECPA4 | 0/8 |
| SL3261/pVDL9.3PA83ec | 0/6 |
| rPA1-4 | 8/8 |
| rPA1+4 | 7/7 |
| rPA4 | 8/8 |
| rPA1 | 3/8 |
| None | 0/7 |
A/J mice were inoculated three times at 2-week intervals with 1 × 108 to 5 × 109 CFU of S. enterica serovar Typhimurium SL3261 or SL3261 recombinants delivered orally by intragastric gavage or 10 μg of protein adsorbed to a 20% (vol/vol) solution of Alhydrogel delivered by intramuscular injection. The mice were subsequently challenged 9 weeks after the final dose via the intranasal route with approximately 105 CFU of aerosolized B. anthracis STI spores and monitored for survival until 14 days postexposure.
DISCUSSION
In order to develop an oral vaccine for anthrax using Salmonella as a vehicle to deliver PA, a sufficiently stable, immunogenic vaccine candidate is required. We have constructed and evaluated a recombinant Salmonella which contains a multicopy plasmid encoding codon-optimized PA in order to increase the number of gene copies from which the PA protein may be expressed. We have also incorporated the ClyA export system for the direct export of PA. This approach has previously been used by Galen et al. (11) to export PA4 and requires only the coexpression of the 34-kDa ClyA protein. The pSEC10 plasmid allowed the expression of PA under the control of the PompC promoter, in order to target expression to the intracellular location. Since PA domains 1 and 4 are known to possess protective epitopes, SL3261 derivatives expressing full-length PA, a PA1+4 fusion protein, or PA4 only were produced.
Although studies by Wai et al. (31) indicated that the ClyA protein accumulates in the periplasm and is subsequently exported from the bacterial cell via the release of outer membrane vesicles from the cell surface, we were unable to show that the ClyA-PA protein fusions were exported into the culture supernatants. However, PA expression was detected and the SL3261 recombinants containing pSEC10-based plasmids were found to be at least 80% stable in vitro and in vivo. The pVDL9.3PA83ec plasmid, previously shown to be unstable in S. enterica serovar Typhimurium strain Zoosaloral H (13), was stably maintained in SL3261. This finding perhaps reflects, generally, the relative stabilities of plasmids in different strains of Salmonella.
Mice orally inoculated with SL3261 recombinants expressing full-length PA, domain 4 only, or a fusion protein consisting of domains 1 and 4 generated anthrax toxin-neutralizing antibodies. The Western blot of the SL3261 recombinants probed with anti-PA was prepared using standardized CFU/ml samples (Fig. 2) indicated that full-length PA was not expressed at a higher level in Salmonella than PA1+4 or PA4. Thus, it is likely that the enhanced protective response induced after immunization with full-length PA is a result of the presence of domains 2 and 3. This is consistent with the previous finding that domain 2 is able to improve protection afforded by domain 1 (6). This could be due to the presence of additional protective epitopes or the role played by domains 2 and 3 in tertiary conformation or protein export (30).
Mice orally immunized with SL3261 expressing the full-length PA were protected (five of six mice) against a lethal exposure to aerosolized B. anthracis spores. In comparison, only two of eight mice given SL3261 expressing PA1+4 survived the exposure, whereas all of the mice given SL3261 expressing PA4 succumbed to infection. We believe that this is the first report of the protection of aerosolized anthrax after oral immunization with a Salmonella-based vaccine.
In the present study, we have also evaluated the ability of purified PA protein, the individual domains PA1 or PA4, or the PA1+4 fusion protein to protect mice against aerosolized B. anthracis spores. When administered with Alhydrogel, all of the proteins stimulated strong antigen-specific antibody responses. Although rPA4, rPA1+4, and rPA1-4 conferred complete protection, rPA1 was only able to protect three of eight animals. These data correspond with the finding that rPA1 provided a lower level of protection than rPA4 when challenged with B. anthracis by injection (6). It was not possible to determine whether the purified recombinant fusion protein, rPA1+4, offered a greater level of protection against anthrax than rPA4 only. A higher challenge level may have allowed this to be determined. However, the comparison of the Salmonella recombinants indicated that PA1+4 is more protective than PA1, supporting the evaluation of the fusion protein. Overall, the results from the in vitro and in vivo protection studies indicate that the optimum protective effect is obtained when the full-length PA protein is used to develop the Salmonella-based vaccine.
An important finding from the work reported here is the poor correlation of serum antibody levels to PA with the degree of protection against B. anthracis challenge. However, when sera was tested in a toxin-neutralizing assay, a good correlation was observed. Clearly, these findings suggest that only a proportion of the antibody generated after immunization is able to neutralize anthrax toxin, and immunogens that are able to induce high levels of antibody will not necessarily provide high levels of protection. Similar findings have recently been reported by Duc et al. (5).
The aim of this research is ultimately to develop an orally delivered vaccine for anthrax. In the present study, we have shown for the first time that orally administered Salmonella expressing PA is able to protect mice against infection caused by airborne B. anthracis. However, the development of a vaccine suitable for use in humans would be dependent on the expression of PA in S. enterica serovar Typhi. Depending on the immunogenicity of this recombinant, it may be more appropriate to use this vaccine to boost existing responses that have been primed at an earlier date. Such an orally delivered booster vaccine would be valuable when it is necessary to ensure that large populations rapidly develop protective immunity. Work to construct S. enterica serovar Typhi expressing PA, using the systems we have reported here, is currently under way.
Acknowledgments
This study was supported by NIH grant 5-U19-AI-56578-03.
We gratefully acknowledge the technical assistance provided by Helen Flick-Smith and the animal technicians at DSTL.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 4 December 2006.
REFERENCES
- 1.Baillie, L. 2001. The development of new vaccines against Bacillus anthracis. J. Appl. Microbiol. 91:609-613. [DOI] [PubMed] [Google Scholar]
- 2.Bernardi, A., and F. Bernardi. 1984. Complete sequence of pSC101. Nucleic Acids Res. 12:9415-9426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chatfield, S. N., K. Strahan, D. Pickard, I. G. Charles, C. E. Hormaeche, and G. Dougan. 1992. Evaluation of Salmonella typhimurium strains harbouring defined mutations in htrA and aroA in the murine salmonellosis model. Microb. Pathog. 12:145-151. [DOI] [PubMed] [Google Scholar]
- 4.Coulson, N. M., M. Fulop, and R. W. Titball. 1994. Bacillus anthracis protective antigen, expressed in Salmonella typhimurium SL3261, affords protection against anthrax spore challenge. Vaccine 12:1395-1401. [DOI] [PubMed] [Google Scholar]
- 5.Duc, L. H., H. A. Hong, H. S. Atkins, H. C. Flick-Smith, Z. Durrani, S. Rijpkema, R. W. Titball, and S. M. Cutting. 2007. Immunization against anthrax using Bacillus subtilis spores expressing the anthrax protective antigen. Vaccine 25:346-355. [DOI] [PubMed]
- 6.Flick-Smith, H. C., N. J. Walker, P. Gibson, H. L. Bullifent, S. Hayward, J. Miller, R. W. Titball, and E. D. Williamson. 2002. A recombinant carboxy-terminal domain of the protective antigen of Bacillus anthracis protects mice against anthrax infection. Infect. Immun. 70:1653-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reference deleted.
- 8.Galen, J. E., O. G. Gomez-Duarte, G. A. Losonsky, J. L. Halpern, C. S. Lauderbaugh, S. Kaintuck, M. K. Reymann, and M. M. Levine. 1997. A murine model of intranasal immunization to assess the immunogenicity of attenuated Salmonella typhi live vector vaccines in stimulating serum antibody responses to expressed foreign antigens. Vaccine 15:700-708. [DOI] [PubMed] [Google Scholar]
- 9.Galen, J. E., and M. M. Levine. 2001. Can a “flawless” live vector vaccine strain be engineered? Trends Microbiol. 9:372-376. [DOI] [PubMed] [Google Scholar]
- 10.Galen, J. E., J. Nair, J. Y. Wang, S. S. Wasserman, M. K. Tanner, M. B. Sztein, and M. M. Levine. 1999. Optimization of plasmid maintenance in the attenuated live vector vaccine strain Salmonella typhi CVD 908-htrA. Infect. Immun. 67:6424-6433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galen, J. E., L. Zhao, M. Chinchilla, J. Y. Wang, M. F. Pasetti, J. Green, and M. M. Levine. 2004. Adaptation of the endogenous Salmonella enterica serovar Typhi clyA-encoded hemolysin for antigen export enhances the immunogenicity of anthrax protective antigen domain 4 expressed by the attenuated live-vector vaccine strain CVD 908-htrA. Infect. Immun. 72:7096-7106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garmory, H. S., K. A. Brown, and R. W. Titball. 2002. Salmonella vaccines for use in humans: present and future perspectives. FEMS Microbiol. Rev. 26:339-353. [DOI] [PubMed] [Google Scholar]
- 13.Garmory, H. S., R. W. Titball, K. F. Griffin, U. Hahn, R. Böhm, and W. Beyer. 2003. Salmonella enterica serovar Typhimurium expressing a chromosomally integrated copy of the Bacillus anthracis protective antigen gene protects mice against an anthrax spore challenge. Infect. Immun. 71:3831-3836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Germanier, R., and E. Fuer. 1975. Isolation and characterization of Gal E mutant Ty21a of Salmonella typhi: a candidate strain for a live, oral typhoid vaccine. J. Infect. Dis. 131:553-558. [DOI] [PubMed] [Google Scholar]
- 15.Guyton, A. C. 1947. Measurement of the respiratory volumes of laboratory animals. Am. J. Physiol. 150:70-77. [DOI] [PubMed] [Google Scholar]
- 16.Harper, G. J., and J. D. Morton. 1953. The respiratory retention of bacterial aerosols: experiments with radioactive spores. J. Hyg. 51:372-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henderson, D. W. 1952. An apparatus for the study of airborne infection. J. Hyg. Camb. 50:53-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hobert, O. 2002. PCR fusion-based approach to create reporter gene constructs for expression analysis in transgenic Caenorhabditis elegans. Bio Techniques 32:728-730. [DOI] [PubMed] [Google Scholar]
- 19.Ivins, B. E., and S. L. Welkos. 1988. Recent advances in the development of an improved human anthrax vaccine. Eur. J. Epidemiol. 4:12-19. [DOI] [PubMed] [Google Scholar]
- 20.Leppla, S. H. 1995. Anthrax toxins, p. 543-572. In J. Moss, B. Iglewski, M. Vaughan, and A. Tu (ed.), Bacterial toxins and virulence factors in disease. Marcel Dekker, Inc., New York, NY.
- 21.Reference deleted.
- 22.May, K. R. 1973. The collision nebulizer: description, performance, and application. J. Aero. Sci. 4:235-243. [Google Scholar]
- 23.May, K. R., and G. H. Harper. 1957. The efficacy of various liquid impinger samplers in bacterial aerosols. Br. Ind. Med. 14:287-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McBride, B. W., A. Mogg, J. L. Telfer, M. S. Lever, J. Miller, P. C. B. Turnbull, and L. Baillie. 1998. Protective efficacy of a recombinant protective antigen against Bacillus anthracis challenge and assessment of immunological markers. Vaccine 16:810-817. [DOI] [PubMed] [Google Scholar]
- 25.Miller, J., B. W. McBride, R. J. Manchee, P. Moore, and L. W. J. Baillie. 1998. Production and purification of recombinant protective antigen and protective efficacy against Bacillus anthracis. Lett. Appl. Microbiol. 26:56-60. [DOI] [PubMed] [Google Scholar]
- 26.Pezard, C., M. Weber, J.-C. Sirard, P. Berche, and M. Mock. 1995. Protective immunity induced by Bacillus anthracis toxin-deficient strains. Infect. Immun. 1369-1372. [DOI] [PMC free article] [PubMed]
- 27.Reference deleted.
- 28.Quinn, C. P., P. M. Dull, V. Semenova, H. Li, S. Crotty, T. H. Taylor, E. Steward-Clark, K. L. Stamey, D. S. Schmidt, K. Wallace Stinson, A. E. Freeman, C. M. Elie, S. K. Martin, C. Greene, R. D. Aubert, J. Glidewell, B. A. Perkins, R. Ahmed, and D. S. Stephens. 2004. Immune responses to Bacillus anthracis protective antigen in individuals with bioterrorism-associated cutaneous and inhalational anthrax. J. Infect. Dis. 190:1228-1236. [DOI] [PubMed] [Google Scholar]
- 29.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY.
- 30.Thwaite, J. E., L. W. J. Baillie, N. M. Carter, K. Stephenson, M. Rees, C. R. Harwood, and P. T. Emmerson. 2002. Optimization of the cell wall microenvironment allows increased production of recombinant Bacillus anthracis protective antigen (rPA) from Bacillus anthracis. Appl. Environ. Microbiol. 68:227-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wai, S. N., B Lindmark, T. Soderblom, A. Takade, M. Westermark, J. Oscarsson, J. Jass, A. Richter-Dahlfors, Y. Mizunoe, and B. E. Uhlin. 2003. Vesicle-mediated export and assembly of pore-forming oligomers of the enterobacterial ClyA cytotoxin. Cell 115:25-35. [DOI] [PubMed] [Google Scholar]
- 32.Welkos, S. L., T. J. Keener, and P. H. Gibbs. 1986. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 51:795-800. [DOI] [PMC free article] [PubMed] [Google Scholar]