Abstract
Burkholderia cepacia, a species found infrequently in cystic fibrosis (CF), was isolated from 85% of patients infected with bacteria of the B. cepacia complex that visited the major Portuguese CF center, in Lisbon, during 2003 to 2005. A detailed molecular analysis revealed that this was mainly due to two B. cepacia clones. These clones were indistinguishable from two strains isolated from intrinsically contaminated nonsterile saline solutions for nasal application, detected during routine market surveillance by the Portuguese Medicines and Health Products Authority.
Burkholderia cepacia complex (BCC) bacteria are opportunistic pathogens that may colonize and/or infect patients with cystic fibrosis (CF), an inherited disorder that, among other clinical manifestations, predisposes individuals to recurrent respiratory infections and lung damage (15). Epidemiological surveys carried out in several countries indicated that all nine BCC species can be recovered from respiratory secretions of CF patients, but Burkholderia cenocepacia and Burkholderia multivorans are predominant (17). A remarkable exception to this observation is the epidemiological analysis carried out by our laboratory at the major Portuguese CF center (6). Although the prevalence of B. cenocepacia (52%) was confirmed, a significant percentage (36%) of the patients at the CF center of Hospital de Santa Maria (HSM) during 1995 to 2002 were colonized or infected with B. cepacia (6). This contrasts with previous studies performed in Canada, the United States, Italy, and France, where B. cepacia incidence ranged from 0.2% to 7.7% (1, 3, 4, 13, 21, 23). The reason for the unexpectedly high representation of B. cepacia during this surveillance period could not be determined. By the end of 2003, a routine market surveillance analysis performed by Infarmed, the Portuguese Medicines and Health Products Authority, revealed that several batches of nonsterile saline solutions from two local manufacturers greatly exceeded the microbiological quality limits (≤102 CFU/ml) established by European Pharmacopoeia VII (7). Preliminary identification by gas chromatography analysis of the fatty acid methyl esters (MIDI; Sherlock, Newark, DE) suggested that the isolated bacteria belong to the species B. cepacia. Following the confirmation of the identification by molecular methods described below, the contaminated batches were immediately withdrawn from the market. New contaminated batches were detected later, in March 2006. Since saline is used in inhalant therapy by CF patients, a correlation between this contamination and the unusually high representation of B. cepacia registered at the CF center under surveillance (6) was considered. To test this hypothesis, molecular analysis of 95 BCC isolates recovered from sputum samples from 13 CF patients on selective B. cepacia solid medium (Selectatab; Mast Diagnostics, Merseyside, United Kingdom) from November 2002 to March 2006 was carried out, and their genetic relatedness to the saline isolates was assessed. In general, sputum samples from CF patients were obtained every 2 to 3 months during periodic consultation to monitor their clinical status. Samples were cultured more often for patients showing clinical deterioration. All serial isolates obtained from chronically infected patients (80% of patients examined) were included in the study. A patient was considered chronically infected when three positive cultures of BCC strains were isolated within an 8-month period.
Distribution of isolates from CF patients and saline among BCC species.
During the 3.5-year surveillance period in this study, 85% of BCC-positive CF patients under surveillance at the HSM CF center harbored strains of the species B. cepacia (recA HaeIII restriction fragment length polymorphism [RFLP] type D, E, K, Z, or AG). This conclusion was based on polymorphisms of the recA gene with HaeIII and species-specific recA-directed PCR, performed as described before (16). B. cenocepacia (recA HaeIII RFLP type G, AN, or AU) was present in 23% of the CF patients examined, 15% of them also being colonized or infected with B. cepacia (Table 1). While B. cenocepacia infections predominated until 2001 (6), B. cepacia became the most represented species after November 2002, its incidence peaking in 2004 (Table 1). The analysis of saline isolates indicated that they belonged to recA HaeIII RFLP type D or E (Table 2).
TABLE 1.
Results of molecular analysis of BCC isolates from CF patients under surveillance at HSM from November 2002 to March 2006a
| Patient reference | Isolate | Date of isolation | Organism | recA RFLP profile | Ribotype | PFGE profile |
|---|---|---|---|---|---|---|
| O | IST4135 | November 2002 | B. cepacia | AG | 12 | — |
| IST4137 | January 2003 | B. cepacia | AG | 12 | — | |
| IST4139 | April 2003 | B. cepacia | AG | 12 | — | |
| IST4142 | June 2003 | B. cepacia | AG | 12 | — | |
| IST4146 | August 2003 | B. cepacia | AG | 12 | — | |
| IST4150 | September 2003 | B. cepacia | AG | 12 | — | |
| IST4157 | January 2004 | B. cepacia | AG | 12 | — | |
| IST4165 | March 2004 | B. cepacia | AG | 12 | — | |
| IST4167 | May 2004 | B. cepacia | AG | 12 | — | |
| IST4240 | September 2004 | B. cepacia | AG | 12 | — | |
| IST4177 | November 2004 | B. cepacia | AG | 12 | — | |
| IST4180 | January 2005 | B. cepacia | AG | 12 | — | |
| IST4183 | March 2005 | B. cepacia | AG | 12 | — | |
| IST4189 | May 2005 | B. cepacia | AG | 12 | — | |
| IST4204 | July 2005 | B. cepacia | AG | 12 | — | |
| IST4209 | October 2005 | B. cepacia | AG | 12 | — | |
| IST4216 | November 2005 | B. cepacia | AG | 12 | — | |
| IST4227 | January 2006 | B. cepacia | AG | 12 | — | |
| IST4230 | February 2006 | B. cepacia | AG | 12 | — | |
| R | IST4144 | July 2003 | B. cenocepacia B | AN | 15 | — |
| IST4149 | September 2003 | B. cenocepacia B | AN | 15 | — | |
| IST4155 | November 2003 | B. cenocepacia B | AN | 15 | — | |
| IST4164 | March 2004 | B. cenocepacia B | AN | 15 | — | |
| IST4178 | November 2004 | B. cenocepacia B | AN | 15 | — | |
| IST4203 | July 2005 | B. cenocepacia B | AN | 15 | — | |
| IST4205 | August 2005 | B. cenocepacia B | AN | 15 | — | |
| IST4210 | September 2005 | B. cenocepacia B | AN | 15 | — | |
| IST4219 | November 2005 | B. cenocepacia B | AN | 15 | — | |
| IST4228 | January 2006 | B. cenocepacia B | AN | 15 | — | |
| IST4231 | February 2006 | B. cenocepacia B | AN | 15 | — | |
| IST4232 | February 2006 | B. cenocepacia B | AN | 15 | — | |
| IST4235 | March 2006 | B. cenocepacia B | AN | 15 | — | |
| V | IST4148 | September 2003 | B. cepacia | E | 17 | I |
| IST4241 | June 2004 | B. cepacia | E | 17 | I | |
| IST4169 | June 2004 | B. cepacia | E | 17 | I | |
| IST4200 | July 2005 | B. cepacia | E | 17 | I | |
| IST4224 | December 2005 | B. cepacia | E | 17 | I | |
| AB | IST4136 | January 2003 | B. cenocepacia A | G | 7 | — |
| IST4140 | May 2003 | B. cenocepacia A | G | 7 | — | |
| IST4141 | May 2003 | B. cenocepacia A | G | 7 | — | |
| IST4151 | October 2003 | B. cenocepacia A | G | 7 | — | |
| IST4153 | November 2003 | B. cenocepacia A | G | 7 | — | |
| IST4154 | November 2003 | B. cenocepacia A | G | 7 | — | |
| IST4166 | April 2004 | B. cenocepacia A | G | 7 | — | |
| IST4170 | June 2004 | B. cenocepacia A | G | 7 | — | |
| IST4173 | August 2004 | B. cepacia | D | 19 | II | |
| IST4179 | January 2005 | B. cenocepacia A | G | 7 | — | |
| IST4182 | March 2005 | B. cenocepacia A | G | 7 | — | |
| IST4191 | June 2005 | B. cenocepacia A | G | 7 | — | |
| IST4187 | April 2005 | B. cenocepacia A | G | 7 | — | |
| IST4202 | July 2005 | B. cenocepacia A | G | 7 | — | |
| IST4213 | October 2005 | B. cenocepacia A | G | 7 | — | |
| IST4234 | February 2006 | B. cenocepacia A | G | 7 | — | |
| AF | IST4193 | December 2004 | B. cepacia | K | 2 | — |
| IST4186 | April 2005 | B. cepacia | K | 2 | — | |
| IST4188 | May 2005 | B. cepacia | K | 2 | — | |
| IST4192 | June 2005 | B. cepacia | K | 2 | — | |
| IST4194 | October 2005 | B. cepacia | K | 2 | — | |
| IST4206 | October 2005 | B. cepacia | K | 2 | — | |
| IST4207 | October 2005 | B. cenocepacia B | AN | 15 | — | |
| IST4221 | November 2005 | B. cepacia | E | 17 | I | |
| IST4238 | March 2006 | B. cepacia | K | 2 | — | |
| IST4237 | March 2006 | B. cepacia | K | 2 | — | |
| AG | IST4171 | July 2004 | B. cepacia | D | 19 | II |
| IST4176 | October 2004 | B. cepacia | D | 19 | — | |
| IST4181 | February 2005 | B. cepacia | D | 19 | — | |
| AJ | IST4162 | March 2004 | B. cepacia | D | 19 | II |
| AL | IST4152 | October 2003 | B. cepacia | D | 19 | II |
| IST4158 | February 2004 | B. cepacia | D | 19 | — | |
| IST4159 | February 2004 | B. cepacia | D | 19 | — | |
| IST4160 | February 2004 | B. cepacia | D | 19 | — | |
| IST4168 | May 2004 | B. cepacia | D | 19 | — | |
| IST4175 | October 2004 | B. cepacia | D | 19 | — | |
| IST4184 | March 2005 | B. cepacia | D | 19 | — | |
| IST4220 | November 2005 | B. cepacia | D | 19 | — | |
| IST4222 | December 2005 | B. cepacia | D | 19 | — | |
| IST4226 | January 2006 | B. cepacia | D | 19 | — | |
| AM | IST4156 | November 2003 | B. cepacia | D | 19 | II |
| IST4161 | February 2004 | B. cepacia | D | 19 | — | |
| AN | IST4190 | January 2005 | B. cenocepacia A | AU | 21 | — |
| IST4197 | May 2005 | B. cenocepacia A | AU | 21 | — | |
| IST4201 | July 2005 | B. cenocepacia A | AU | 21 | — | |
| IST4211 | September 2005 | B. cenocepacia A | AU | 21 | — | |
| IST4215 | October 2005 | B. cenocepacia A | AU | 21 | — | |
| IST4223 | December 2005 | B. cenocepacia A | AU | 21 | — | |
| AO | IST4212 | October 2005 | B. cepacia | D | 19 | II |
| IST4217 | November 2005 | B. cepacia | D | 19 | — | |
| AP | IST4199 | July 2005 | B. cepacia | D | 19 | II |
| IST4218 | November 2005 | B. cepacia | D | 19 | — | |
| IST4236 | March 2006 | B. cepacia | D | 19 | — | |
| AQ | IST4198 | July 2005 | B. cepacia | Z | 24 | — |
| IST4214 | October 2005 | B. cepacia | Z | 24 | — | |
| IST4225 | December 2005 | B. cepacia | Z | 24 | — | |
| IST4229 | January 2006 | B. cepacia | Z | 24 | — | |
| IST4233 | February 2006 | B. cepacia | Z | 24 | — |
Sequential isolates from chronically infected patients represent 80% of the 95 isolates examined. —, not determined.
TABLE 2.
Results of the molecular analysis of B. cepacia isolates recovered from contaminated saline solutions by Infarmed at the end of 2003 and in March 2006
| Manufacturer (brand) | Date of isolation | No of isolates | recA HaeIII profile | Ribotype | PFGE profilea |
|---|---|---|---|---|---|
| A (K) | December 2003 | 3 | E | 17 | I |
| A (K) | November-December 2003 | 5 | E | 18 | — |
| A (K) | November 2003 | 2 | E | 20 | — |
| B (X) | November-December 2003 | 8 | D | 19 | II |
| B (X) | March 2006 | 6 | D | 19 | II |
| B (Y) | March 2006 | 5 | D | 19 | II |
| B (Z) | March 2006 | 4 | D | 19 | II |
—, not determined.
Genetic relatedness of clinical and saline isolates of B. cepacia.
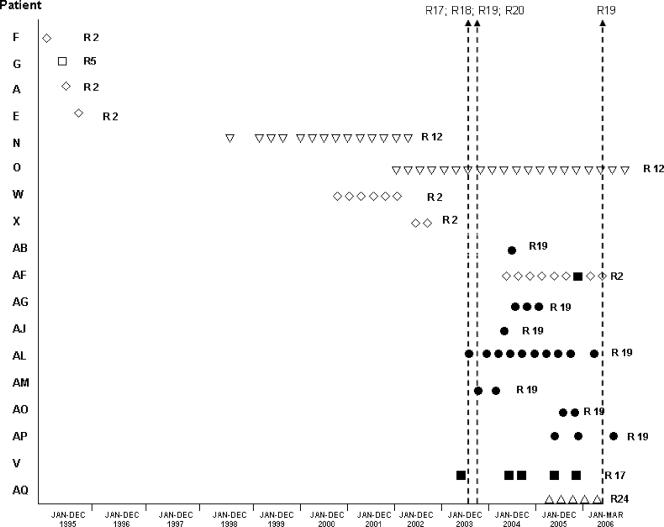
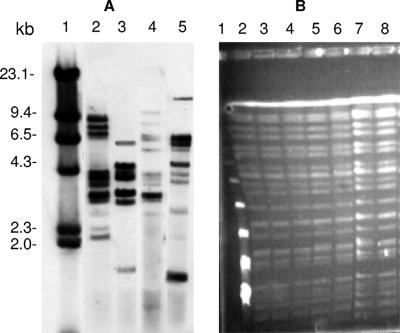
The 60 clinical isolates of B. cepacia tested generated five ribopatterns, designated 2, 12, 17, 19, and 24 (Fig. 1; Table 1), while the 35 B. cenocepacia isolates generated three ribopatterns, designated 7, 15, and 21 (Table 1). Ribotyping was performed as described by Cunha et al. (6), using as a probe fluorescein-labeled 16S and 23S rDNA from B. cenocepacia J2315 chromosomal DNA, amplified with the primers 16SF (5′-GATTGAACGCTGGCGGCATG-3′), 16SR (5′-GAGGTGATCCAGCCGCACCT-3′), 23SF (5′-AAGCGATCAAGTGCATGTGGTG-3′), and 23SR (5′-GATCAAGCCTTACGGGCAATTA-3′). The 33 B. cepacia isolates recovered by Infarmed in December 2003 and March 2006 from nine contaminated lots of saline generated four different ribopatterns (Fig. 2A; Table 2). Isolates with ribopattern 19 were recovered on both occasions from the saline produced by manufacturer B. Remarkably, ribopatterns 17 and 19, generated by 23 B. cepacia saline isolates, were also generated by 28 B. cepacia isolates obtained from 9 CF patients receiving care at HSM from September 2003 to March 2006 (Table 1). RFLP-pulsed-field gel electrophoresis (PFGE) analysis, carried out according to standard protocols (22), confirmed the clonality of clinical and saline B. cepacia isolates with ribopattern 19 or 17, since all the isolates with the same ribotype gave rise to identical RFLP-PFGE patterns (Fig. 2B). This result indicates that the majority of the respiratory infections with B. cepacia registered in 2003 to 2005 were due to two strains, with ribopatterns 17 and 19 and RFLP-PFGE profiles I and II, respectively, that were indistinguishable by ribotyping and RFLP-PFGE profiling from the two B. cepacia clones isolated in 2003 and 2006 from the intrinsically contaminated saline solutions. Moreover, prior to the date of the detection of the first lots of contaminated saline solutions (the end of 2003), no B. cepacia isolate with ribopattern 17 or 19 had been recovered from CF patients (Fig. 1) (6). Furthermore, patients with ribopattern 17 or 19 isolates had never been colonized/infected with BCC bacteria (Fig. 1). Indeed, the very strong increase in the incidence of B. cepacia in the CF center under surveillance, registered during 2003 and 2004, coincided with the detection in the market of contaminated saline solutions. Three B. cepacia strains different from those present in the contaminated saline also colonized and/or infected the CF patients receiving care at HSM from 2003 through 2006 (Table 1). These strains also contributed to the unusually high representation of B. cepacia species in this CF center during the surveillance period, but the source of infection remains unclear.
FIG. 1.
Ribopatterns (⋄, R2; □, R5; ▿, R12; ▪, R17; •, R19; ▵, R24) of the B. cepacia isolates obtained from CF patients visiting the HSM CF center between January 1995 and March 2006. Clinical B. cepacia strains identical to strains isolated from the contaminated saline solutions, with ribopatterns 17 and 19, are represented by solid symbols. The arrows indicate the date of detection of contaminated saline solutions. Patients G, O, AB, and AF also harbored B. cenocepacia isolates. This representation is based on results in Table 1 and on previous results (6).
FIG. 2.
(A) Ribopatterns generated by B. cepacia isolates from contaminated saline solutions or from CF patients. Lanes: 1, λ/HindIII molecular size standard; 2, ribotype 17; 3, ribotype 20; 4, ribotype 18; 5, ribotype 19. Ribotypes 19 and 17 are common to isolates from saline solutions and CF patients. (B) RFLP-PFGE profile II, generated by seven B. cepacia isolates that gave rise to ribopattern 19, isolated from contaminated saline solutions or from CF patients. Lanes: 1, bacteriophage lambda concatemer molecular size standards; 2, saline solution isolate; 3, IST4173 (CF); 4, IST4162 (CF); 5, IST4152 (CF); 6, IST4171 (CF); 7, IST4199 (CF); 8, IST4202 (CF).
Clinical outcome of CF patients infected with B. cepacia or B. cenocepacia.
During the surveillance period in this study, no death was registered among the CF patients harboring BCC bacteria. In general, the CF patients chronically infected with B. cenocepacia or B. cepacia strains remained clinically stable, in particular those harboring strains indistinguishable from the saline clones. The only exception was patient AF, who had already presented with moderate lung disease before testing positive for B. cepacia but whose clinical condition suffered a rapid deterioration (as indicated by lung function and number of hospitalizations) following colonization for almost 18 months with a B. cepacia strain of ribopattern 2. Although this clinical strain was unrelated to the saline clones, a B. cepacia strain with ribopattern 17 was sporadically isolated from this patient, as well as a B. cenocepacia strain (Table 1).
Concluding remarks.
Bacteria of the BCC are resistant to multiple antimicrobials and to diverse growth inhibitors, which they can even use as carbon sources (5). These bacteria also have minimal nutritional requirements, which enables them to grow in aqueous products, including disinfectants (10, 19). Contamination of albuterol and sulbutamol nebulization solutions (2, 9), nebulizers (11), mouthwash (18), nasal sprays (8), and ultrasound gel (12) has resulted in outbreaks of nosocomially acquired infection by BCC bacteria. Although results from this study appear to suggest an epidemiological relationship between the intrinsically contaminated saline solutions and CF patients colonized/infected with the less commonly isolated species B. cepacia, it was not possible to establish a definitive link between the use of contaminated saline solutions and patient contamination. Furthermore, other B. cepacia strains with no direct relation to the clones detected in the contaminated saline solutions also contributed to the unusually high representation of B. cepacia registered in this CF center during the period under analysis, suggesting other sources of infection. A significant proportion of the CF patients that were not colonized with the two clones under discussion harbored unique strains of B. cepacia or B. cenocepacia. This observation indicates that although transmission of these bacteria is significant in the colonization of CF patients, in a CF center that follows the recommended control measures, as is the case at the Lisbon CF center, other primary sources of infection must account for many of the cases. It is likely that the environment may act as reservoir for novel BCC infections (14, 20, 24). This study supports the recommendation for the exclusive use of sterile saline solutions by CF patients. It also highlights the importance of the continuous monitoring of medications for microbial contamination and the surveillance of unexplained outbreaks involving less common pathogens. In particular, attention should be given to the usually poorly represented species, like B. cepacia, especially when patients with underlying lung disease and increased risk, such as CF patients, are involved.
Acknowledgments
The contributions of L. Lito (HSM) and M. Miranda, A. Galvão, and E. Bértolo (Infarmed) to this study are gratefully acknowledged.
M. V. Cunha is the recipient of a fellowship (SFRH/BPD/14911/2004) from Fundação para a Ciência e a Tecnologia (FCT).
Footnotes
Published ahead of print on 14 March 2007.
REFERENCES
- 1.Agodi, A., E. Mahenthiralingam, M. Barchitta, V. Giannino, A. Sciacca, and S. Stefani. 2001. Burkholderia cepacia complex infection in Italian patients with cystic fibrosis: prevalence, epidemiology, and genomovar status. J. Clin. Microbiol. 39:2891-2896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balkhy, H. H., G. Cunningham, C. Francis, M. A. Almuneef, G. Stevens, N. Akkad, A. Elgammal, A. Alassiri, E. Furukawa, F. K. Chew, M. Sobh, D. Daniel, G. Poff, and Z. A. Memish. 2005. A National Guard outbreak of Burkholderia cepacia infection and colonization secondary to intrinsic contamination of albuterol nebulization solution. Am. J. Infect. Control 33:182-188. [DOI] [PubMed] [Google Scholar]
- 3.Brisse, S., C. Cordevant, P. Vandamme, P. Bidet, C. Loukil, G. Chabanon, M. Lange, and E. Bingen. 2004. Species distribution and ribotype diversity of Burkholderia cepacia complex isolates from French patients with cystic fibrosis. J. Clin. Microbiol. 42:4824-4827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campana, S., G. Taccetti, N. Ravenni, F. Favari, L. Cariani, A. Sciacca, D. Savoia, A. Collura, E. Fiscarelli, G. De Intinis, M. Busetti, A. Cipolloni, A. d'Aprile, E. Provenzano, I. Collebrusco, P. Frontini, G. Stassi, M. Trancassini, D. Tovagliari, A. Lavitola, C. J. Doherty, T. Coenye, J. R. W. Govan, and P. Vandamme. 2005. Transmission of Burkholderia cepacia complex: evidence for new epidemic clones infecting cystic fibrosis patients in Italy. J. Clin. Microbiol. 43:5136-5142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coenye, T., and P. Vandamme. 2003. Diversity and significance of Burkholderia cepacia occupying diverse ecological niches. Environ. Microbiol. 5:719-729. [DOI] [PubMed] [Google Scholar]
- 6.Cunha, M. V., J. H. Leitão, E. Mahenthiralingam, P. Vandamme, L. Lito, C. Barreto, M. J. Salgado, and I. Sá-Correia. 2003. Molecular analysis of Burkholderia cepacia complex isolates from a Portuguese cystic fibrosis center: a seven-year study. J. Clin. Microbiol. 41:4113-4120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Directorate for the Quality of Medicines of the Council of Europe. European Pharmacopoeia, 4th ed. Council of Europe, Strasbourg, France.
- 8.Dolan, S., E. Dowell, S. Valdez, J. J. LiPuma, and J. James. 2005. An outbreak of Burkholderia cepacia complex associated with an intrinsically contaminated nasal spray product. Am. J. Infect. Control 33:e110-e111. [DOI] [PubMed] [Google Scholar]
- 9.Ghazal, S. S., K. Al-Mudaimeegh, and E. M. A. Fakihi. 2006. Outbreak of Burkholderia cepacia bacteremia in immunocompetent children caused by contaminated nebulized sulbutamol in Saudi Arabia. Am. J. Infect. Control 34:394-398. [DOI] [PubMed] [Google Scholar]
- 10.Holmes, B. 1986. The identification of Pseudomonas cepacia and its occurrence in clinical material. J. Appl. Bacteriol. 61:299-314. [DOI] [PubMed] [Google Scholar]
- 11.Hutchinson, G. R., S. Parker, J. A. Pryor, F. Duncan-Skingle, P. N. Hoffman, M. E. Hodson, M. E. Kaufmann, and T. L. Pitt. 1996. Home-use nebulizers: a potential source of Burkholderia cepacia and other colistin-resistant, gram-negative bacteria in patients with cystic fibrosis. J. Clin. Microbiol. 34:584-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobson, M., R. Wray, D. Kovach, D. Henry, D. Speert, and A. Matlow. 2006. Sustained endemicity of Burkholderia cepacia complex in a pediatric institution, associated with contaminated ultrasound gel. Infect. Control Hosp. Epidemiol. 27:362-366. [DOI] [PubMed] [Google Scholar]
- 13.LiPuma, J. J., T. Spilker, L. H. Gill, P. W. Campbell III, L. Liu, and E. Mahenthiralingam. 2001. Disproportionate distribution of Burkholderia cepacia complex species and transmissibility markers in cystic fibrosis. Am. J. Respir. Crit. Care Med. 164:92-96. [DOI] [PubMed] [Google Scholar]
- 14.LiPuma, J. J., T. Spilker, T. Coenye, and C. F. Gonzalez. 2002. An epidemic Burkholderia cepacia complex strain identified in soil. Lancet 359:2002-2003. [DOI] [PubMed] [Google Scholar]
- 15.Lyczak, J. B., C. L. Cannon, and G. B. Pier. 2002. Lung infections associated with cystic fibrosis. Clin. Microbiol. Rev. 15:194-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahenthiralingam, E., J. Bischof, S. K. Byrne, C. Radomski, J. E. Davies, Y. Av-Gay, and P. Vandamme. 2000. DNA-based diagnostic approaches for identification of Burkholderia cepacia complex, Burkholderia vietnamiensis, Burkholderia multivorans, Burkholderia stabilis, and Burkholderia cepacia genomovars I and III. J. Clin. Microbiol. 38:3165-3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahenthiralingam, E., T. A. Urban, and J. B. Goldberg. 2005. The multifarious, multireplicon Burkholderia cepacia complex. Nat. Rev. Microbiol. 3:144-156. [DOI] [PubMed] [Google Scholar]
- 18.Matrician, L., G. Ange, S. Burns, W. L. Fanning, C. Kioski, G. C. Cage, and K. K. Komatsu. 2000. Outbreak of nosocomial Burkholderia cepacia infection and colonization associated with intrinsically contaminated mouthwash. Infect. Control Hosp. Epidemiol. 21:739-741. [DOI] [PubMed] [Google Scholar]
- 19.Oie, S., and A. Kamiya. 1996. Microbial contamination of antiseptics and disinfectants. Am. J. Infect. Control. 24:389-395. [DOI] [PubMed] [Google Scholar]
- 20.Pallud, C., V. Viallard, J. Balandreau, P. Normand, and G. Grundmann. 2001. Combined use of a specific probe and PCAT medium to study Burkholderia in soil. J. Microbiol. Methods 47:25-34. [DOI] [PubMed] [Google Scholar]
- 21.Reik, R., T. Spilker, and J. J. LiPuma. 2005. Distribution of Burkholderia cepacia complex species among isolates recovered from persons with or without cystic fibrosis. J. Clin. Microbiol. 43:2926-2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Richau, J. A., J. H. Leitão, M. Correia, L. Lito, M. J. Salgado, C. Barreto, P. Cescutti, and I. Sá-Correia. 2000. Molecular typing and exopolysaccharide biosynthesis of Burkholderia cepacia isolates from a Portuguese cystic fibrosis center. J. Clin. Microbiol. 38:1651-1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Speert, D. P., D. Henry, P. Vandamme, M. Corey, and E. Mahenthiralingam. 2002. Epidemiology of Burkholderia cepacia complex in patients with cystic fibrosis in Canada: geographical distribution and clustering of strains. Emerg. Infect. Dis. 8:181-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vanlaere, E., T. Coenye, E. Samyn, C. Van den Plas, J. Govan, F. De Baets, K. De Boeck, C. Knoop, and P. Vandamme. 2005. A novel strategy for the isolation and identification of environmental Burkholderia cepacia complex bacteria. FEMS Microbiol. Lett. 249:303-307. [DOI] [PubMed] [Google Scholar]