Abstract
Enveloped viruses often require cleavage of a surface glycoprotein by a cellular endoprotease such as furin for infectivity and virulence. Previously, we showed that Ebola virus glycoprotein does not require the furin cleavage motif for virus replication in cell culture. Here, we show that there are no appreciable differences in disease progression, hematology, serum biochemistry, virus titers, or lethality in nonhuman primates infected with an Ebola virus lacking the furin recognition sequence compared to those infected with wild-type virus. We conclude that glycoprotein cleavage by subtilisin-like endoproteases is not critical for Ebola virus infectivity and virulence in nonhuman primates.
Ebola virus, a member of the family Filoviridae, causes hemorrhagic fever in human and nonhuman primates, with up to 90% lethality (2, 9). Although the molecular basis for the extreme virulence of Ebola virus remains largely unknown, many enveloped viruses require cleavage of their surface glycoprotein by cellular endoproteases for infectivity and virulence (3). This cleavage event produces two subunits and exposes a fusion peptide that inserts into the host cell membrane, thereby “fusing” the cellular and viral membranes. The glycoprotein (GP) of Zaire ebolavirus (ZEBOV) contains a highly conserved consensus sequence for the subtilisin-like endoprotease furin (10, 12). ZEBOV GP cleavage by this protease has been previously demonstrated (12). By contrast, the glycoprotein of Reston ebolavirus, the species least pathogenic for humans, lacks an optimal furin cleavage site (containing lysine, but not arginine, at position −4). Furin cleavage was therefore considered an important determinant of Ebola virus virulence (2). However, studies of pseudotyped viruses expressing Ebola GP with an altered furin recognition sequence demonstrated that GP cleavage by furin is dispensable for in vitro infectivity of the pseudotyped viruses (7, 14).
Using reverse genetics, which allows the artificial generation of Ebola virus from cloned cDNA (8, 13), we previously generated a ZEBOV mutant based on the Mayinga strain in which the multibasic sequence motif for furin cleavage (RRTRR at amino acids 497 to 501 of GP) was replaced with nonbasic amino acids (AGTAA) (8). This mutation prevented the generation of GP1 and GP2, the two cleavage products, and yet the mutant virus grew in cell culture to titers similar to those of wild-type virus, albeit with mildly attenuated growth early in infection (8). These findings indicated that furin-mediated cleavage of Ebola virus GP is not essential for virus replication in cell culture. However, does this finding also hold true in animals?
Nonhuman primates, including cynomolgus and rhesus macaques, develop disease with a pathology that resembles that observed in Ebola virus-infected humans. Because these animals display similar symptoms and disease progression and succumb to infection with wild-type ZEBOV without prior adaptation, they are considered the “gold standard” animal model for Ebola virus infection.
Here, we assessed our recombinant Ebola virus that lacks the conserved furin recognition sequence (ZEBOVΔCleav) in rhesus macaques. Two healthy, filovirus-seronegative, adult rhesus macaques were inoculated in the right caudal thigh with 103 PFU of recombinant ZEBOVΔCleav virus. Two additional animals were inoculated with the same dose of wild-type ZEBOV generated by reverse genetics. Animals were observed twice daily for signs of illness, including cutaneous rashes, hemorrhage, and reduced activity. Blood samples for virus titration, hematology, and serum biochemistry were collected prior to infection and on days 3, 4, 6, and 7 postinfection. Animals that showed severe signs of disease were euthanized in compliance with approved protocols. Animal studies were performed under biosafety level 4 biocontainment conditions at the U.S. Medical Research Institute of Infectious Diseases and approved by the U.S. Medical Research Institute of Infectious Diseases Laboratory Animal Care and Use Committee. Animal research was conducted in compliance with the Federal statues and regulations relating to animals and experiments involving animals, adhering to the principles in the Guide for the Care and Use of Laboratory Animals (7a). The facility used is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
All infected animals were asymptomatic until day 4 postinfection, when all four animals became febrile (temperature > 39.7°C). By day 5, all four had developed characteristic macular cutaneous rashes (Fig. 1A). On day 7, one animal infected with ZEBOVΔCleav expired, while the remaining three monkeys became terminally ill and were euthanized. These findings demonstrate that wild-type ZEBOV generated by reverse genetics is as virulent as the original ZEBOV (4) and that Ebola virus lacking the consensus furin recognition motif in GP is as capable as wild-type virus of causing fatal disease in nonhuman primates.
FIG. 1.
Comparison of monkeys infected with ZEBOV (left panels) or ZEBOVΔCleav (right panels). (A) Macular cutaneous rashes on day 6 postinfection. (B) Phosphotungstic acid hematoxylin-positive fibrin in spleen. Staining was carried out as described in reference 5. Note that there is no apparent difference in the amount or distribution of polymerized fibrin (see arrows that point to fibrin-stained regions). Original magnification, ×40. (C) Immunostaining of inguinal lymph nodes. Staining was carried out as described in reference 4. Note that positive immunostaining of monocytes-macrophages for Ebola virus (red) is evident in both animals. Also, lymphoid depletion and lymphocytolysis are prominent in both animals. Original magnification, ×20.
No appreciable differences in hematology and serum biochemistry (measured as described previously; see reference 4) were detected between monkeys infected with ZEBOV virus and those infected with ZEBOVΔCleav virus. In similarity to results previously obtained for Ebola virus infections in cynomolgus macaques (4, 6), all animals developed lymphopenia and thrombocytopenia with elevated liver enzyme levels during late infection. The most pronounced increases were in alanine aminotransferase and aspartate aminotransferase levels on days 6 and 7 postinfection, indicative of liver failure. In addition, monkeys infected with ZEBOV or ZEBOVΔCleav virus revealed similar levels of fibrin deposits (Fig. 1B) and similar numbers of infected monocytes-macrophages (Fig. 1C).
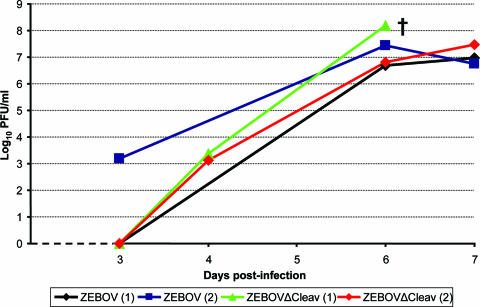
The clinical signs and blood biochemistry of rhesus macaques infected with ZEBOVΔCleav virus suggested replication of the virus in monkeys; this growth may, however, have been attenuated due to the lack of the consensus furin recognition motif in GP. We, therefore, determined virus titers in serum and organs. When plaque assays were performed, virus titers in serum were undetectable or low on day 3 postinfection but reached high levels on days 6 and 7 postinfection (6.7 to 7.5 log10 PFU/ml) (Fig. 2) for ZEBOV-infected animals. The two animals infected with ZEBOVΔCleav reached similar titers (6.8 to 8.2 log10 PFU/ml) on day 6 and 7 postinfection, respectively. Note that one animal infected with ZEBOVΔCleav expired on day 7 prior to blood sampling. We also conducted quantitative real-time reverse transcription-PCR and found low numbers of genomic copies on day 3 postinfection for animals infected with ZEBOV and no viral genomic copies in animals infected with ZEBOVΔCleav (note that the detection limit of the assay is 140 genomic copies), suggesting mild attenuation of the mutant virus. Quantitative reverse transcription-PCR analysis on day 6 postinfection revealed no differences in the numbers of genomic copies between the two groups.
FIG. 2.
Viremia in rhesus macaques infected with wild-type Ebola virus (ZEBOV) generated by reverse genetics and in a mutant lacking the conserved recognition sequence for furin (ZEBOVΔCleav). Note that one animal infected with ZEBOVΔCleav expired on day 7 postinfection (†); therefore, no fresh serum sample for that animal could be obtained for virus titration.
ZEBOV and ZEBOVΔCleav also replicated to comparable titers in various organs (Table 1), although viral titers were low in the spleen and undetectable in the pancreas of the animal infected with ZEBOVΔCleav that died on day 7. Virus titers in the pancreas and brain of one ZEBOV-infected monkey were also low, suggesting normal variability among these infected animals. Our findings establish that Ebola virus replication in nonhuman primates is not significantly attenuated by the loss of the furin recognition motif in GP.
TABLE 1.
Virus titers in various organs of rhesus macaques infected with wild-type Ebola virus (ZEBOV) or with an Ebola virus lacking the consensus furin recognition motif in GP (ZEBOVΔCleav)
| Virus strain (animal no.) | Virus titer (log10 of PFU/gram tissue on day 7 postinfection)a
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Liver | Spleen | Kidney | Lungs | Pancreas | Brain | Heart | Bone marrow | Testis | Adrenal glands | Axillary lymph nodes | Inguinal lymph nodes | Mesenteric lymph nodes | Mandibular lymph nodes | |
| ZEBOV (1) | 6.93 | 7.41 | 5.51 | 5.50 | 2.40 | 3.98 | 4.93 | 6.15 | 5.81 | 6.01 | 6.20 | 7.12 | 6.68 | 6.01 |
| ZEBOV (2) | 6.95 | 7.40 | 6.70 | 6.10 | 6.51 | 5.01 | 5.31 | 6.08 | 6.75 | 7.07 | 6.79 | 6.47 | 7.86 | 6.90 |
| ZEBOV ΔCleav (1) | 5.54 | 2.87 | 6.10 | 6.74 | 0 | 6.22 | 5.97 | 5.90 | 6.22 | 5.65 | 6.37 | 6.26 | 5.89 | 6.30 |
| ZEBOV ΔCleav (2) | 7.80 | 7.70 | 5.87 | 4.23 | 5.65 | 5.31 | 5.83 | 6.90 | 6.60 | 7.33 | 6.76 | 6.59 | 7.44 | 7.05 |
Animals were inoculated in the caudal thigh with 103 PFU of virus.
To confirm that the amino acid changes introduced into the furin recognition motif of ZEBOVΔCleav were retained during replication, we sequenced the GP genes of viruses from plasma and spleen samples of ZEBOVΔCleav-infected animals on day 6 and day 7 postinfection, respectively. For all samples, the introduced mutations were retained. Moreover, no other nucleotide replacements were found in the GP gene.
GP cleavage by host cell proteases is critical for the virulence of many viruses, and the conservation of the furin cleavage motif among Ebola virus GP sequences suggested a similar role in Ebola virus replication. Our previous and present findings, however, establish that the furin recognition sequence in Ebola virus GP is dispensable in cell culture (8) and in nonhuman primates (this study), indicating that GP cleavage is dispensable for Ebola virus replication in these systems. However, GP cleavage by furin or a furin-like endoprotease may be required for Ebola virus replication in its natural host. GP1 degradation by endosomal cathepsins is important for the initiation of Ebola virus uncoating (1, 11). Our findings indicate that GP cleavage by furin into GP1 and GP2 is not a prerequisite for cathepsin digestion. Whether proteolytic processing by other proteases in endosomes is required prior to cathepsin digestion remains unknown.
Acknowledgments
We thank Susan Watson for editing the manuscript, Denise Braun for technical assistance with animal studies, Tom Larsen for pathology support, and Elizabeth Fritz and Leslie Wachter for assistance with the quantitative PCR assays. We also thank Lisa Hensley for helpful discussions.
This work was sponsored in part by Public Health Service research grants from the National Institute of Allergy and Infectious Diseases and by the National Institutes of Health-National Institute of Allergy and Infectious Diseases Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research Program. We acknowledge membership within and support from the Region V “Great Lakes” Regional Center of Excellence (National Institutes of Health award 1-U54-AI-057153). This study was also supported in part by financial support from the Public Health Agency of Canada and a grant from the Canadian Institute of Health Research (MOP-43921) and the Medical Chemical/Biological Defense Research Program and Military Infectious Diseases Research Program, U.S. Army Medical Research and Material Command (project number 02-4-4J-081).
Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
Footnotes
Published ahead of print on 17 January 2007.
REFERENCES
- 1.Chandran, K., N. J. Sullivan, U. Felbor, S. P. Whelan, and J. M. Cunningham. 2005. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 308:1643-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feldmann, H., and H. D. Klenk. 2005. Filoviruses, p. 1085-1101. In B. W. J. Mahy and V. TerMeulen (ed.), Topley & Wilson's microbiology & microbial infections, virology. Hodder Arnold, London, United Kingdom.
- 3.Garten, W., and H. D. Klenk. 1999. Understanding influenza virus pathogenicity. Trends Microbiol. 7:99-100. [DOI] [PubMed] [Google Scholar]
- 4.Geisbert, T. W., L. E. Hensley, T. Larsen, H. A. Young, D. S. Reed, J. B. Geisbert, D. P. Scott, E. Kagan, P. B. Jahrling, and K. J. Davis. 2003. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am. J. Pathol. 163:2347-2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geisbert, T. W., H. A. Young, P. B. Jahrling, K. J. Davis, E. Kagan, and L. E. Hensley. 2003. Mechanisms underlying coagulation abnormalities in Ebola hemorrhagic fever: overexpression of tissue factor in primate monocytes/macrophages is a key event. J. Infect. Dis. 188:1618-1629. [DOI] [PubMed] [Google Scholar]
- 6.Geisbert, T. W., H. A. Young, P. B. Jahrling, K. J. Davis, T. Larsen, E. Kagan, and L. E. Hensley. 2003. Pathogenesis of Ebola hemorrhagic fever in primate models: evidence that hemorrhage is not a direct effect of virus-induced cytolysis of endothelial cells. Am. J. Pathol. 163:2371-2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ito, H., S. Watanabe, A. Takada, and Y. Kawaoka. 2001. Ebola virus glycoprotein: proteolytic processing, acylation, cell tropism, and detection of neutralizing antibodies. J. Virol. 75:1576-1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7a.National Research Council. 1996. Guide for the care and use of animals. National Academy Press, Washington, DC.
- 8.Neumann, G., H. Feldmann, S. Watanabe, I. Lukashevich, and Y. Kawaoka. 2002. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J. Virol. 76:406-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanchez, A., A. S. Khan, S. R. Zaki, G. J. Nabel, T. G. Ksiazek, and C. J. Peters. 2001. Filoviridae: marburg and ebola viruses, p. 1279-1304. In D. M. Knipe, P. M. Howley, D. E. Griffin, M. A. Martin, R. A. Lamb, B. Roizman, and S. E. Straus (ed.), Fields virology, vol. 1. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 10.Sanchez, A., Z. Y. Yang, L. Xu, G. J. Nabel, T. Crews, and C. J. Peters. 1998. Biochemical analysis of the secreted and virion glycoproteins of Ebola virus. J. Virol. 72:6442-6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schornberg, K., S. Matsuyama, K. Kabsch, S. Delos, A. Bouton, and J. White. 2006. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J. Virol. 80:4174-4178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volchkov, V. E., H. Feldmann, V. A. Volchkova, and H. D. Klenk. 1998. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc. Natl. Acad. Sci. USA 95:5762-5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volchkov, V. E., V. A. Volchkova, E. Muhlberger, L. V. Kolesnikova, M. Weik, O. Dolnik, and H. D. Klenk. 2001. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science 291:1965-1969. [DOI] [PubMed] [Google Scholar]
- 14.Wool-Lewis, R. J., and P. Bates. 1999. Endoproteolytic processing of the Ebola virus envelope glycoprotein: cleavage is not required for function. J. Virol. 73:1419-1426. [DOI] [PMC free article] [PubMed] [Google Scholar]