Abstract
Recurrent outbreaks of highly pathogenic avian influenza virus pose the threat of pandemic spread of lethal disease and make it a priority to develop safe and effective vaccines. Influenza virus-like particles (VLPs) have been suggested to be a promising vaccine approach. However, VLP-induced immune responses, and their roles in inducing memory immune responses and cross-protective immunity have not been investigated. In this study, we developed VLPs containing influenza virus A/PR8/34 (H1N1) hemagglutinin (HA) and matrix (M1) proteins and investigated their immunogenicity, long-term cross-protective efficacy, and effects on lung proinflammatory cytokines in mice. Intranasal immunization with VLPs containing HA induced high serum and mucosal antibody titers and neutralizing activity against PR8 and A/WSN/33 (H1N1) viruses. Mice immunized with VLPs containing HA showed little or no proinflammatory lung cytokines and were protected from a lethal challenge with mouse-adapted PR8 or WSN viruses even 5 months postimmunization. Influenza VLPs induced mucosal immunoglobulin G and cellular immune responses, which were reactivated rapidly upon virus challenge. Long-lived antibody-secreting cells were detected in the bone marrow of immunized mice. Immune sera administered intranasally were able to confer 100% protection from a lethal challenge with PR8 or WSN, which provides further evidence that anti-HA antibodies are primarily responsible for preventing infection. Taken together, these results indicate that nonreplicating influenza VLPs represent a promising strategy for the development of a safe and effective vaccine to control the spread of lethal influenza viruses.
Influenza virus is a segmented negative-sense RNA virus, belonging to the Orthomyxoviridae family. The virion is surrounded by a lipid membrane containing two major glycoproteins, the hemagglutinin (HA) and neuraminidase (NA). The HA protein is the most abundant viral surface glycoprotein and is responsible for the attachment of virus to terminal sialic acid residues on host cell receptors (4) and mediating fusion between viral and cellular membranes (6). There are 16 distinct antigenic subtypes of influenza A viruses that are recognized on the basis of antigenic properties of the HA protein (15). Influenza A virus causes a highly contagious and acute viral respiratory disease, which can pose serious public health problems resulting in significant morbidity and mortality worldwide each year (36, 40). A more serious concern is that avian influenza viruses are a source for a diverse mix of antigenic subtypes representing a large reservoir of novel viruses to which the human population is naïve (32, 37, 38, 41). Genetic reassortment of RNAs between avian and human influenza viruses or mutations affecting host range could enable avian viruses to transmit among the human population, which may lead to a global pandemic with high mortality.
Vaccination has been an effective way to reduce the disease resulting from an influenza virus infection. The major supply of influenza virus vaccine is currently produced using embryonated chicken eggs. However, manufacturing problems experienced in recent years illustrate that the current methods of production are fragile in ensuring an adequate and timely supply of influenza virus vaccine. More importantly, the egg-based technology may not be suitable to respond to a pandemic crisis. The H5 avian influenza virus strains responsible for recent epizoonotic outbreaks in Asia are lethal to chicken eggs (25, 29, 31). Also, due to the high pathogenicity of avian influenza virus strains, the conventional production of avian influenza virus vaccines would require biosafety level 3 containment facilities. In addition, vaccine development and production take several months following the identification of new potential strains and typically require reassortment with a high-yield strain. Therefore, a strategy that can rapidly produce new influenza virus vaccines is needed as a priority for pandemic preparedness.
Virus-like particles (VLPs) have been generated and tested as vaccine candidates for a variety of viruses (2, 11, 12, 19, 22). It was recently reported that immunization with influenza VLPs (H3N2 and H9N2) reduced challenge virus replication and conferred protection against an influenza virus challenge (8, 24). However, the immune responses induced by influenza VLPs are not well characterized, and the memory responses and cross-protective immunity are unknown for VLP immunization. In this study, we developed VLPs for influenza virus A/PR8 (H1N1), for which the challenge system and immune epitopes are well-defined in a mouse model. Intranasal immunization of mice with these influenza VLPs induced mucosal and systemic immune responses, including both humoral and cellular immune components. We observed that immune responses induced by the influenza VLPs conferred cross-protection against lethal challenge with homologous or heterologous strains. We further analyzed protective memory immune responses induced by VLP immunization.
MATERIALS AND METHODS
Virus and cells.
Spodoptera frugiperda Sf9 cells were maintained in suspension in serum-free SF900II medium (GIBCO-BRL) at 27°C in spinner flasks at a speed of 70 to 80 rpm. CV-1 and Madin-Darby canine kidney (MDCK) cells were grown and maintained in Dulbecco's modified Eagle's medium (DMEM). Mouse-adapted influenza A/PR8/34 (provided by Huan Nguyen, University of Alabama at Birmingham, Birmingham, AL) and A/WSN/33 (from Yumiko Matsuoka, CDC, Atlanta, GA) viruses were prepared as lung homogenates from intranasally infected mice.
Preparation of influenza VLPs.
A cDNA for influenza virus M1 (A/PR8) was obtained from Yumiko Matsuoka (CDC, Atlanta, GA). The M1 gene was PCR amplified with primers containing flanking restriction enzyme sites for cloning into the pSP72 plasmid expression vector under the T7 promoter (forward primer, 5′ TCC CCCGGG CCACC ATG AGC CTT CTG ACC GAG GTC 3′; reverse primer, 5′ TTA CT TCTAGA TTA CTT GAA CCG TTG CAT CTG 3′; SmaI and XbaI sites are underlined). The pSP72 clone containing the M1 gene was confirmed by DNA sequencing, and the expression of the M1 protein was confirmed by Western blot analysis of CV-1 cells transfected with pSP72 containing the M1 gene following infection with a recombinant vaccinia virus expressing T7 polymerase. The M1 gene was subcloned into the SmaI and XbaI site in the baculovirus transfer vector pc/pS1 containing a hybrid capsid-polyhedrin promoter. To produce a recombinant baculovirus (rBV) expressing M1, Sf9 insect cells were cotransfected with Baculogold DNA (BD/PharMingen) and the pc/pS1-M1 transfer vector by following the manufacturer's instructions. The supernatant was harvested 5 days after transfection, and recombinant plaques expressing M1 were selected by plaque assay and expanded. A rBV expressing influenza virus A/PR8 HA (H1N1) was previously described (10). For Western blot analysis to determine the expression of M1 and HA, transfected or infected cells were dissolved in sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE) sample buffer (50 mM Tris, 3% β-mercaptoethanol, 2% SDS, 10% glycerol), separated by SDS-PAGE, and then probed with mouse anti-M1 antibody (1:4,000; Serotec) and sera from PR8 virus-infected mice (1:1,000). The virus titer was determined with a Fast Plax titration kit according to the manufacturer's instructions (Novagen, Madison, WI).
To produce VLPs containing influenza virus M1 and HA, Sf9 cells were coinfected with rBVs expressing HA and M1 at multiplicities of infection of 4 and 2, respectively. Culture supernatants were harvested at 3 days postinfection, cleared by low-speed centrifugation (2,000 × g for 20 min at 4°C) to remove cells, and VLPs in the supernatants were pelleted by ultracentrifugation (100,000 × g for 60 min). The sedimented particles were resuspended in phosphate-buffered saline (PBS) at 4°C overnight and further purified through a 20%-30%-60% discontinuous sucrose gradient at 100,000 × g for 1 h at 4°C. The VLP bands were collected and analyzed by using Western blots probed with anti-M1 antibody and mouse anti-PR8 sera for detecting M1 and HA, respectively. The level of residual rBV in the purified VLPs was determined by plaque assay, and equivalent titers of HA-expressing rBVs were estimated to contribute less than 5% of HA in VLPs as determined by Western blotting (data not shown). The functionality of HA incorporated into VLPs was assessed by hemagglutination activity using chicken red blood cells as described previously (26). Also, cleavability of HA into HA1 and HA2 subunits was determined by using increasing concentrations of trypsin (treated with l-1-tosylamide-2-phenylethyl chloromethyl ketone [TPCK]; Sigma) as previously described (18).
Electron microscopy.
To examine budding of VLPs, Sf9 cells infected with rBVs expressing M1 and HA were fixed with 0.25% glutaraldehyde and 1% osmium tetraoxide, dehydrated with ethanol, and then embedded in Epon resin. Thin sections were stained with lead citrate and uranyl acetate and observed by electron microscopy. For negative staining of VLPs, sucrose gradient-purified VLPs (1 to 5 μg) were applied to a carbon-coated Formvar grid for 30 seconds. Excess VLP suspension was removed by blotting with filter paper, and the grid was immediately stained with 1% phosphotungstic acid for 30 seconds. Excess stain was removed by filter paper, and the samples were examined using a transmission electron microscope.
Immunization and challenge.
Female inbred BALB/c mice (Charles River) aged 6 to 8 weeks were used. Mice (24 mice per group) were intranasally immunized with 40 μg of VLPs two times (weeks 0 and 3) and 10 μg of VLPs three times (weeks 0, 3, and 6) in 50 μl of PBS at 3-week intervals. To determine the effect of VLP integrity on its immunogenicity, VLPs were heat treated at 95°C for 5 min and used to immunize mice as a control group. For virus challenge, isoflurane-anesthetized mice were intranasally infected with 2,000 PFU of A/PR8 virus (10× the 50% lethal dose [LD50]) or 750 PFU WSN (10× LD50) in 50 μl of PBS per mouse 4 or 21 weeks after the final immunization. For measurement of immune response parameters, six mice from each group were sacrificed prior to challenge or on day 4 postchallenge. Mice were observed daily to monitor changes in body weight and to record death.
Sample collection.
Blood samples were collected by retro-orbital plexus puncture before immunization, at 2 weeks after boost immunization, and at different time points (weeks 4, 8, and 21) after the last immunization. After the blood samples were allowed to clot and centrifuged, serum samples were collected and stored at −20°C prior to antibody titration. Nasal and tracheal washes and lung samples were collected from individual mice at week 4.5 after the last immunization or on day 4 after a challenge infection (3, 33). The whole-lung extracts prepared as homogenates using frosted glass slides were centrifuged at 1,000 rpm for 10 min to collect supernatants. The lung supernatants were frozen and kept at −70°C until used for immunoglobulin and virus titers and cytokine assays. Cells from bone marrow were harvested from individual mice 21 weeks after the last immunization, prepared as previously described (14), and used for detection of influenza virus-specific immunoglobulin G (IgG) and IgA antibody-secreting plasma cells. Lymphocytes from spleen samples were collected from sacrificed mice and used for enzyme-linked immunospot (ELISPOT) analysis.
Evaluation of humoral immune responses.
Influenza virus-specific antibodies of different subtypes (IgG, IgG1, IgG2a, IgG2b, IgG3, and IgA) were determined in sera, wash samples of nose and trachea, and lung extracts by enzyme-linked immunosorbent assay (ELISA) as described previously (26). Briefly, 96-well microtiter plates (Nunc-Immuno Plate MaxiSorp; Nunc Life Technologies, Basel, Switzerland) were coated with 100 μl of inactivated PR8 (or WSN or heat-treated VLPs) at a concentration of 4 μg/ml in coating buffer (0.1 M sodium carbonate, pH 9.5) at 4°C overnight. The plates were then incubated with horseradish peroxidase-labeled goat anti-mouse IgG, IgG1, IgG2a, IgG2b, IgG3, or IgA (Southern Biotechnology) at 37°C for 1.5 h, and then, the substrate O-phenylenediamine (Zymed, San Francisco, Calif.) in citrate-phosphate buffer (pH 5.0) containing 0.03% H2O2 (Sigma) was used to develop color. The optical density at 450 nm was read using an ELISA reader (model 680; Bio-Rad).
Determination of influenza virus-specific antibody-secreting cells from bone marrow.
Inactivated PR8 viral antigen or anti-mouse IgA and IgG antibodies as capture antibodies were used to coat Multiscreen 96-well filtration plates (Millipore). Freshly isolated cells from bone marrow (1 × 106 cells) were added to each well and incubated for 48 h at 37°C with 5% CO2. Using horseradish peroxidase-conjugated anti-mouse immunoglobulin antibodies and the ELISPOT assay substrate diaminobenzidine (Research Genetics), color was developed following the manufacturer's instructions, and counting of ELISPOTs was performed as described previously (13).
Lung viral titers and virus neutralization assay.
Lung viral titers and neutralization assays were performed using MDCK cells as previously described (26). Briefly, serum samples were serially diluted in DMEM, and a final volume of 190 μl was mixed with 10 μl of diluted virus stock containing approximately 100 infectious particles. The virus-serum mixtures were incubated at 37°C for 1 h and then added to six-well plates containing confluent MDCK cell monolayers. The plates were incubated at 37°C for 1 h, overlay medium containing DEAE dextran, nonessential amino acids, glutamine, and trypsin was added, and incubated for 2 or 3 days. The cells were then fixed with 0.25% glutaraldehyde and stained with 1% crystal violet.
Cytokine assays.
All antibodies against mouse cytokines used in cytokine ELISPOT assays were purchased from BD/PharMingen (San Diego, Calif.). Anti-mouse gamma interferon (IFN-γ), interleukin-2 (IL-2), IL-4, and IL-5 antibodies (3 μg/ml in coating buffer) were used to coat Multiscreen 96-well filtration plates (Millipore). Freshly isolated splenocytes (1.5 × 106 cells) were added to each well and stimulated with a mixture of two major histocompatibility complex class I (MHC-I) peptides (IYSTVASSL and LYEKVKSQL) or a pool of five MHC-II peptides (SFERFEIFPKE, HNTNGVTAACSH, CPKYVRSAKLRM, KLKNSYVNKKGK, and NAYVSVVTSNYNRRF) at a concentration of 10 μg/ml (7, 23). The plates were incubated for 36 h at 37°C with 5% CO2. Development and counting of cytokine ELISPOTs were performed as described previously (13). Cytokine ELISA was performed as described previously (26). Ready-Set-Go IL-6 and IFN-γ kits (eBioscience, San Diego, CA) were used for detecting cytokine levels in lung extracts following the manufacturer's procedures.
Passive immunization.
Sera from influenza VLP-immunized mice or from naïve mice were heated for 30 min at 56°C to inactivate complement. Serum was administered intranasally (50 μl per mouse) to naïve mice. After 2 h, mice were challenged with a lethal dose of live influenza PR8 virus (2,000 PFU per mouse, 10× LD50), and morbidity and mortality were monitored daily.
Statistics.
All parameters were recorded for individual mice within all groups. Statistical comparisons of data were carried out using the analysis of variance and Npar1-way Kruskal-Wallis test of the PC-SAS system. A P value of <0.05 was considered significant.
RESULTS
Production of influenza VLPs.
The budding of VLPs was observed on the cell surfaces of Sf9 cells infected with rBV expressing M1 and HA (data not shown), and the size and morphology of budding particles were similar to those observed in MDCK cells infected with influenza virus (20). VLPs were found to be released into the culture supernatants (Fig. 1A), which is consistent with previous studies demonstrating that influenza virus matrix protein M1 possesses all the functions necessary for budding and release of VLPs (9, 17) and that HA-containing VLPs are produced and released in insect cells without neuraminidase coexpression (8).
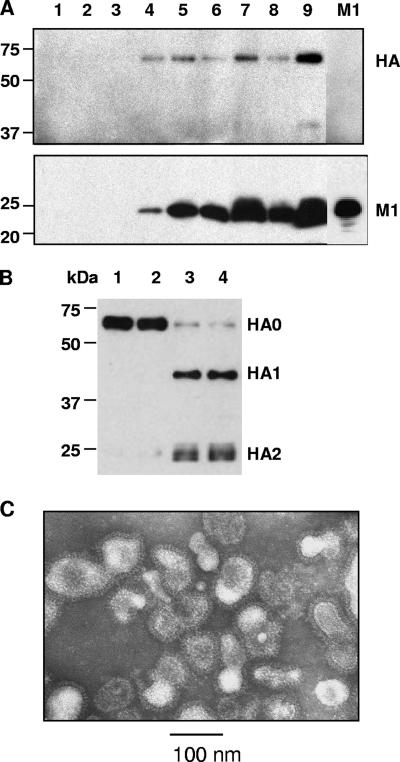
FIG. 1.
Purification of influenza VLPs and electron microscopy examination. (A) Western blot analysis of fractions from sucrose density gradient centrifugation. Blots for HA (top) and M1 (bottom) were probed using mouse anti-PR8 sera and purified mouse anti-M1 IgG antibody, respectively. Lanes: 1 to 3, top fractions without sucrose; 4 and 5, fractions with above 20% sucrose; 6 and 7, fractions between 20 and 30% sucrose; 8 and 9, fractions between 30 and 60% sucrose. Lane M1 contains HA-negative M1 VLPs. The positions of influenza virus HA and M1 proteins are indicated to the right of the blots. The positions of molecular mass markers (in kilodaltons) are shown to the left of the blots. (B) Cleavage of HA in VLPs. VLPs containing HA were incubated for 5 min with different concentrations of TPCK-treated trypsin, resolved by SDS-PAGE, and probed by Western blotting. Lanes 1 to 4 contain 0, 0.125, 1.0, and 2.5 μg/ml trypsin concentrations, respectively. (C) Negative staining electron microscopy of influenza VLPs containing HA and M1.
VLPs were harvested from the culture supernatants of Sf9 cells coinfected with two individual rBVs that express either HA or M1. To purify influenza VLPs containing HA, the harvested VLPs were applied onto a sucrose gradient and Western blotting was performed to determine the distribution of HA and M1 proteins (Fig. 1A). Two major visible bands present between 30% and 60% of sucrose density were found to contain both M1 and HA by Western blotting as shown in lanes 7 and 9 in Fig. 1A. When each band of HA and M1 was scanned by densitometry, the VLP band (lane 9 in Fig. 1A) positioned near the 60% sucrose layer represented 55% of total HA and contained a higher ratio of HA to M1 compared to that near the 30% sucrose (lane 7 in Fig. 1A) which represented 20% of HA. These results suggest that a high level of HA incorporated into M1 VLPs may produce influenza virus-like particles of higher density. The HA titer of VLPs was 128 per μg of VLPs containing HA, which was approximately three- to fourfold lower than that of influenza virions. On the basis of HA content in influenza virions (34), VLPs were estimated to contain 0.5 to 0.7 μg HA per 10 μg VLPs. HA on the VLPs was found mostly in a form of the uncleaved precursor and thus would not be fusogenic, because proteolytic cleavage is required for the membrane fusion activity (28). As an indication of correct folding of HA, we found that HA incorporated into VLPs could be cleaved into HA1 and HA2 subunits in a trypsin dose-dependent manner (Fig. 1B). These results indicate that HA incorporated into VLPs retains hemagglutination activity and maintains a proper conformation. The size and morphology of influenza VLPs were examined by electron microscopy (Fig. 1C). The morphology of VLPs resembles the morphology of influenza virus particles with spikes on their surfaces, characteristic of influenza virus HA proteins on virions. The particle sizes ranged from approximately 80 to 120 nm. Taken together, these results show that Sf9 cells infected with rBVs expressing HA and M1 generated particles resembling influenza virions in morphology and size.
Influenza HA VLPs elicit humoral immune responses.
To determine whether influenza VLPs induce immune responses specific to influenza virus HA, groups of mice were intranasally immunized with 40 μg or 10 μg of influenza VLPs containing both M1 and HA (VLPs), HA-negative VLPs containing M1 alone (M1 VLPs), or human immunodeficiency virus (HIV) VLPs at 3-week intervals. In addition, VLPs were heat treated and used for immunization (10 μg per mouse) to determine the requirements for VLP integrity and HA activity for induction of immune responses. Heat treatment of VLPs resulted in loss of hemagglutination activity (data not shown).
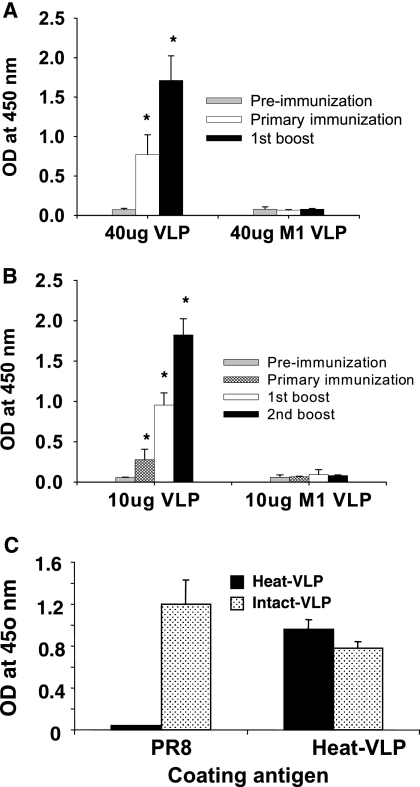
The levels of PR8-specific IgG were found to be significantly increased after the primary immunization in both groups of mice that received 40 μg or 10 μg of VLPs (P < 0.0001), although higher levels of total IgG were observed in the group given 40 μg (Fig. 2A). The first boost significantly enhanced the levels of PR8-specific antibodies (P < 0.0001) with the higher dose inducing higher levels of antibodies (Fig. 2). Three immunizations with a low dose (10 μg VLPs [Fig. 2B]) resulted in levels of antibodies similar to those observed after two immunizations with 40 μg of VLPs. We also observed that the magnitude of humoral immune responses induced by VLPs was comparable to those induced by sublethal live virus infection (data not shown). No significant levels of antibodies specific to PR8 virus were detected in groups of mice immunized with HA-negative M1 VLPs (Fig. 2A and B) or heat-treated VLPs (Fig. 2C), whereas heat-treated VLPs induced antibody binding to heat-treated VLPs (Fig. 2C).
FIG. 2.
Influenza virus-specific total serum IgG antibody responses. Groups of mice were immunized twice with 40 μg VLPs (A) or three times with 10 μg VLPs (B). Mice (24 BALB/c mice per group) were intranasally immunized with influenza HA VLPs or M1 VLPs at 3-week intervals. Blood samples were collected individually at 2 weeks after each immunization. Sera diluted 100-fold were used to determine PR8-specific total IgG by ELISAs. Optical densities (OD) were read at 450 nm, and results are expressed as the arithmetic means plus standard deviations (error bars). Immunization groups: 40 μg VLP, 40 μg influenza VLPs containing HA and M1 at weeks 0 and 3; 40 μg M1 VLP, 40 μg HA-negative M1 VLPs (M1 VLPs) at weeks 0 and 3; 10 μg VLP, 10 μg influenza VLPs containing HA and M1 at weeks 0, 3, and 6; 10 μg M1 VLP, 10 μg M1 VLPs at weeks 0, 3, and 6. Statistical significance is indicated for the difference between mice immunized with influenza HA VLPs and M1 VLPs (*, P < 0.005). (C) Comparison of immune sera from mice immunized with heat-treated VLPs and intact VLPs. Groups of mice (12 mice per group) were immunized with 10 μg of VLPs (heat treated or intact) containing PR8 HA at weeks 0, 2, and 4. The abilities of serum samples (sera diluted 200-fold) after the last immunization to bind to antibodies against inactivated A/PR8 (PR8), heat-treated VLPs (Heat-VLP), and intact VLPs (Intact-VLP) used as an ELISA coating antigen were compared.
To further characterize the kinetics of antibody production, the titers of serum IgG subtypes IgG1, IgG2a, IgG2b, and IgG3 were determined before and after the final immunization at weeks 0, 2, 5, 8, and 27 (Table 1). All antibody isotypes showed significantly increased titers in groups of mice that received 10 μg of VLPs compared to the preimmune levels (P < 0.001) or the M1 VLP group (data not shown). IgG1 and IgG2a levels were found to be the highest among other subtypes, indicating that T helper types 1 (Th1) and T helper type 2 (Th2) immune responses were induced by intranasal immunization with influenza VLPs. Interestingly, a higher level of IgG2b was observed in the group given 10 μg of VLPs, whereas IgG3 was higher in the group given 40 μg of VLPs (data not shown). Notably, antibody titers were twofold higher at 5 months than those at 2 weeks after the final (second boost) immunization (Table 1). These results indicate that influenza VLPs are immunogenic and capable of inducing long-lived antibody responses against influenza virus.
TABLE 1.
Antibody isotype titers specific to influenza virus A/PR8 at different time pointsa
| Time (immune sera) | Antibody isotype titer (103)
|
|||
|---|---|---|---|---|
| IgG1 | IgG2a | IgG2b | IgG3 | |
| 0 wk (preimmune) | 0.5 ± 0.1 | 0.05 ± 0.1 | 0.05 ± 0.02 | 0.05 ± 0.01 |
| 2 wk (primary) | 2 ± 0.5 | 2 ± 0.5 | 1 ± 0.3 | 0.05 ± 0.01 |
| 5 wk (first boost) | 16 ± 2.4 | 16 ± 1.8 | 2 ± 0.5 | 0.5 ± 0.01 |
| 8 wk (second boost) | 32 ± 2.5 | 32 ± 2.2 | 32 ± 3.6 | 1 ± 0.1 |
| 5 mo postimmunization | 64 ± 4.2 | 64 ± 3.4 | 32 ± 3.2 | 1 ± 0.1 |
IgG subclass serum antibodies specific to influenza virus PR8 were determined at week 0, 2, 5, 8, and 5 month postimmunization (at week 27) in the group of mice that were intranasally immunized with 10 μg of HA VLPs. Titers are expressed as the highest dilution of serum having a mean optical density at 450 nm greater than the mean plus 2 standard deviations of similarly diluted naïve serum samples.
Induction of neutralization activity.
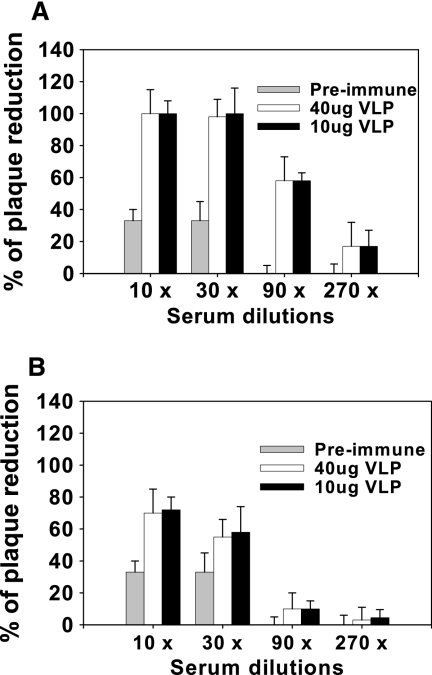
Since neutralizing activities against influenza virus are an indicator of induction of functional antibodies most likely conferring protective immunity, we performed neutralization assays. As shown in Fig. 3, preimmunization and immune sera from M1 VLPs (data not shown) showed only background levels or no neutralizing activity. Immune sera collected 4 weeks after the last immunization with 40 μg or 10 μg of HA VLPs showed a neutralizing titer of 90 (50% neutralization activity titer) against PR8. A neutralizing titer of 30 and hemagglutination inhibition titer of 40 (data not shown), although lower than those against PR8, were observed against A/WSN (Fig. 3B). Meanwhile, similar levels of antibodies binding to inactivated A/WSN were induced in the groups given 10 and 40 μg of VLPs, which was comparable to binding antibody to inactivated A/PR8 (data not shown). These results suggest that immunization with VLPs can induce cross-neutralizing antibodies against influenza viruses and that antibodies recognizing HA contribute to the neutralizing activity.
FIG. 3.
Neutralization activity. Neutralizing antibodies against A/PR8 (A) or A/WSN (B). Viral neutralizing antibody activities were determined using plaque assays for sera collected 4 weeks after the final immunization from mice immunized with 40 μg or 10 μg VLPs (12 mice per group analyzed). Serial dilutions of sera from individual mice were incubated with approximately 100 PFU of PR8 virus for 1 h at 37°C, and a standard plaque reduction assay was performed using MDCK cells. 40 μg VLP, 40 μg influenza VLPs containing HA and M1 at weeks 0 and 3; 10 μg VLP, 10 μg influenza VLPs containing HA and M1 at weeks 0, 3, and 6.
Immunization with HA VLPs confers protection from challenge with homologous and heterologous strains.
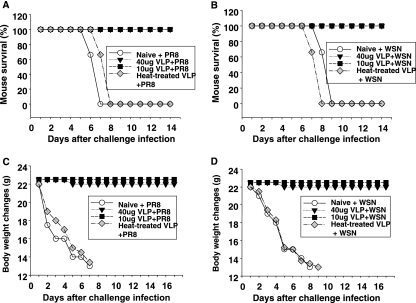
To investigate whether vaccinated mice are cross-protected against a lethal challenge and whether VLP-induced immune responses can lower viral load in vivo, VLP-vaccinated mice were challenged with homologous (PR8) or heterologous (WSN) strains (Fig. 4). All mice immunized with VLPs survived a lethal virus challenge with PR8 and WSN (Fig. 4A and B). In contrast, the naïve group showed a significant and progressive loss in body weight and shivering with challenge infection, indicating that these mice suffered severe illness due to PR8 or WSN viral infection. By days 7 to 9 postchallenge with PR8 or WSN strain, all mice in the naïve group lost over 35% of body weight and died (Fig. 4C and D). In contrast, no loss in body weight was observed postchallenge in groups of mice immunized with 40 μg or 10 μg of VLPs. Also, all mice immunized with heat-treated VLPs (Fig. 4) or HIV VLPs (data not shown) died between days 7 and 9 postchallenge following severe signs of illness and body weight loss. Interestingly, although most M1 VLP-vaccinated mice suffered severe illness and body weight loss and then died, a low level (less than 20%) of mice survived the lethal virus challenge (data not shown), implying a protective role for M1.
FIG. 4.
Protection of mice from lethal PR8 and WSN challenge. At week 4 after the final immunization, naïve and immunized mice were intranasally infected with a lethal dose of mouse-adapted PR8 or WSN virus (10× LD50) (six mice per group). Mice were monitored daily for 15 days. (A and B) Percent survival after PR8 challenge (A) or WSN challenge (B); (C and D) body weight changes (in grams [G]) after PR8 challenge (C) or WSN challenge (D). Immunization groups are described in the legend to Fig. 2, and PR8 and WSN denote a challenge infection with PR8 and WSN, respectively.
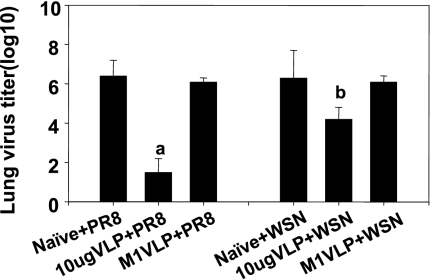
Viral titers in lungs were analyzed to determine the replication of challenge virus at day 4 postchallenge (Fig. 5). The naïve mouse group that received PR8 or WSN challenge virus showed high viral titers reaching 3 × 106 PFU, while lower virus titers were detected in the VLP-immunized groups. Also, high titers of challenge virus replication were observed in the mice that received M1 VLPs; these titers were similar to those in the naïve challenge group. However, significantly decreased virus titers in lungs were found in VLP-immunized mice after PR8 (P < 0.01) or WSN challenge (P < 0.05), although viral titers were higher after WSN challenge (2 × 104 PFU) than after PR8 challenge (5 × 101 PFU). These results indicate that influenza VLPs can induce protective immune responses against both PR8 and WSN lethal challenges.
FIG. 5.
Virus titers in lungs. Lung samples from individual mice in each group (six mice per group) were collected on day 4 postchallenge with a lethal dose of PR8 or WSN, and each sample was diluted in 1 ml DMEM. The titers are presented as log10 PFU per ml, and immunization groups of mice are described in the legend to Fig. 2. PR8 and WSN denote a challenge infection with PR8 and WSN, respectively. Statistical significance is indicated between groups of mice immunized with VLPs and HA-negative M1 VLPs (a, P < 0.01; b, P < 0.05).
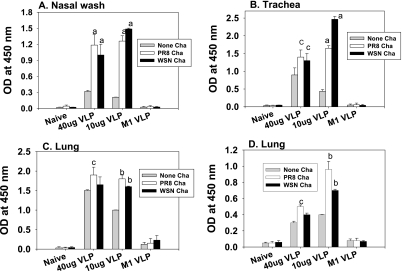
VLP immunization induces mucosal immune responses that reactivate rapidly following challenge.
Since the respiratory mucosal surfaces (nose, trachea, and lung) are the natural route of entry and the primary replication site of influenza virus, it is important to determine mucosal immune responses. Mucosal samples from the nose, trachea, and lung were collected from mice 4.5 weeks after the final immunization and used to determine virus (PR8)-specific antibodies (Fig. 6). We observed high levels of mucosal IgG and IgA antibodies specific to PR8 in all mucosal samples obtained from mice intranasally immunized with 40 μg or 10 μg of influenza HA VLPs (Fig. 6), although levels of IgA were lower than those of IgG (data not shown). Mucosal samples from naïve or HA-negative M1 VLP-immunized mice did not show PR8-specific antibodies.
FIG. 6.
Mucosal antibody responses following challenge infection. (A) IgG in nasal washes, (B) IgG in trachea, (C) IgG in lung extracts, and (D) IgA in lung extracts. Nasal, trachea, and lung samples were collected 4.5 weeks after the final immunization and on day 4 after challenge infections. ELISAs were used to determine respiratory IgG and IgA antibody levels. Optical density at 450 nm (OD 450) values were obtained from 10-fold-diluted mucosal samples, and results are represented as the arithmetic means plus standard deviations (error bars). Each bar represents the arithmetic mean from six mice per group at each time point. Naïve denotes unimmunized mice, and the other groups are as described in the legend to Fig. 2. M1 VLP represent mice immunized with 40 μg M1 VLPs. PR8 and WSN denote a challenge infection with PR8 and WSN, respectively. None denotes the group of mice without a virus challenge infection. Statistical significance (a, P < 0.01; b, P < 0.05; c, P < 0.05) between the values before and after challenge of VLP-immunized mice is indicated.
To investigate the induction of mucosal antibodies after challenge infection, we collected nasal, tracheal, and lung samples 4 days after the challenge infections. We found significant increases in virus-specific IgG antibody levels in all mucosal samples from mice immunized with 40 μg or 10 μg of VLPs following challenge infection with either PR8 or WSN compared to those before challenge. In contrast, virus-specific antibodies were not observed in naïve or M1 VLP-immunized mice even after challenge infection (Fig. 6). Interestingly, higher levels of tracheal IgG and lung IgA were observed in the group immunized with 10 μg VLPs after WSN challenge than those in the group given 40 μg VLPs (Fig. 6B and D). We also found significant increases in lung IgA antibodies in the 10 μg VLP-immunized group after PR8 or WSN challenge (Fig. 6D, P < 0.05 for the group given 40 μg VLPs and P < 0.01 for the group given 10 μg VLPs comparing the groups before and after challenge). Overall, these results suggest that mucosal immunization with influenza VLPs can induce good memory immune responses.
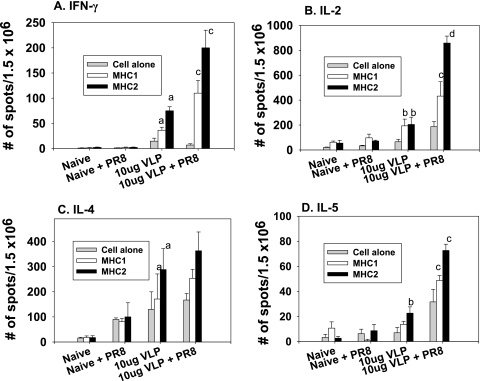
VLP immunization enhances CD4 and CD8 T-cell responses.
Next we determined the magnitude of virus-specific CD4 and CD8 T-cell responses induced by influenza VLPs using ELISPOT assays. Briefly, splenocytes from mice immunized with VLPs 4.5 weeks after the final immunization were stimulated with HA-specific MHC-I- or MHC-II-restricted peptides to quantify HA-specific CD4 and CD8 cells secreting Th1-type (IFN-γ and IL-2) and Th2-type (IL-4 and IL-5) cytokines (Fig. 7). Significant levels of IFN-γ in responses to MHC-I or MHC-II peptide stimulation were detected in mice immunized with VLPs but not in naïve mice (Fig. 7A, P < 0.01 comparing immunized and naïve mice groups), indicating induction of CD4 and CD8 cells secreting IFN-γ. Similarly, upon stimulation with HA-specific peptides, we observed significant increases in both CD4 and CD8 T cells secreting IL-2 compared to the naïve control (Fig. 7B, P < 0.05). Regarding IL-4 and IL-5 cytokines, higher levels of CD4 cells were found to secrete the cytokines than CD8 cells, although both T-cell types were activated to secrete cytokines upon HA peptide stimulation (Fig. 7C and D, P < 0.05).
FIG. 7.
Cytokine-secreting splenocytes following challenge infection. IFN-γ (A), IL-2 (B), IL-4 (C), and IL-5 (D) ELISPOT assays. Splenocytes were isolated from immunized mice 4.5 weeks after the final immunization and on day 4 postchallenge, and cytokine-secreting cells were determined by ELISPOT assays after stimulation with HA-specific MHC class I or II peptides. Naive + PR8 indicates naïve mice that received a PR8 challenge, and 10 μg VLP + PR8 indicates influenza VLP-immunized mice that received a PR8 challenge. The spots for cytokine-producing cells from the spleen were counted and expressed based on 1.5 × 106 cells per well. Each column represents the arithmetic mean from six mice per group at each time point. Statistical significance between the values for naïve and VLP-immunized mice (a, P < 0.01; b, P < 0.05) and the values before and after challenge of VLP-immunized mice (c, P < 0.05; d, P < 0.01) is indicated.
Upon virus infection, the rapid induction of cellular immune responses is also important to control viral replication. Splenocytes were harvested on day 4 after the challenge infection, and cytokine-secreting cells were determined following stimulation with immunodominant MHC class I and II HA peptides (Fig. 7). Mice immunized with VLPs rapidly induced significantly high levels of lymphocytes secreting IFN-γ and IL-2-secreting CD4 and CD8 cells as indicated by stimulation with MHC-II and -I peptides, respectively, and these levels were much higher than those observed prior to challenge (P < 0.05 between the VLP-immunized groups before and after challenge). We also observed significant enhancement of IL-5-secreting lymphocytes at day 4 postchallenge infection in mice immunized with VLPs (Fig. 7D, P < 0.05 compared to the group before challenge). In contrast, naïve mice that received challenge infection were not able to induce cytokine-producing lymphocytes specific to HA peptides (Fig. 7). These results suggest that influenza VLPs induce both Th1- and Th2-type cellular immune responses, which can expand rapidly in response to influenza virus infection.
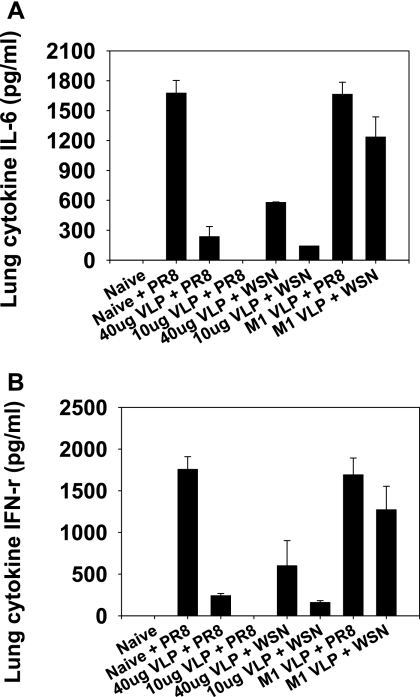
VLP immunization reduces inflammatory cytokines following challenge infection.
High levels of proinflammatory cytokines are involved in causing tissue damage, which may lead to death. After challenge infection, cytokines in lung extracts from naïve and VLP-vaccinated mice were determined using a cytokine ELISA (Fig. 8). We detected the proinflammatory cytokine IL-6 at significantly high levels in naïve or HA-negative M1 VLP-immunized mice upon challenge infection with PR8 or WSN (Fig. 8A). In contrast, little or no IL-6 was observed in the groups of mice immunized with influenza HA VLPs after challenge infection (Fig. 8A). Similarly, IFN-γ was produced at high levels in the lungs of naïve or HA-negative M1 VLP-immunized mice, whereas no or low levels of lung IFN-γ were detected in mice that received influenza HA VLP immunization (Fig. 8B). The same pattern of IFN-γ production was observed upon WSN challenge (data not shown). Therefore, these results indicate that highly increased levels of IL-6 and IFN-γ cytokines induced in naïve mice after an influenza virus infection may be involved in lung inflammation and that influenza HA VLP immunization can avoid or lessen proinflammatory cytokine production in lungs upon viral infection.
FIG. 8.
Proinflammatory cytokines IL-6 (A) and IFN-γ (B) in the lungs after virus challenge. Lung extracts were prepared on day 4 postchallenge. Naïve mouse samples were used as controls. Cytokines in lung extracts were determined by ELISAs, and results shown are geometric mean values obtained from six mice at each time point. Immunization groups (40 μg VLP, 10 μg VLP, and M1 VLP) are described in the legend to Fig. 2, and PR8 and WSN denote a challenge infection with PR8 and WSN, respectively.
VLP immunization maintains long-lasting protective immune responses.
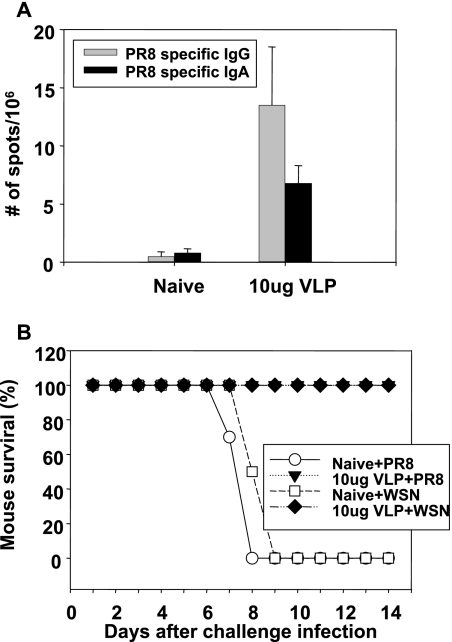
During the differentiation and development of B-cell memory, a fraction of germinal center B cells migrate to the bone marrow where they develop into antibody-secreting plasma cells. To investigate long-lived plasma cells in the bone marrow, we collected bone marrow cells from mice immunized with VLPs 5 months after the last immunization and determined antibody-secreting cells specific for PR8 antigen. We observed 10- and 7-fold increases in PR8-specific IgG and IgA antibody-secreting cells in VLP-immunized mice, respectively, compared to those in naïve mice (Fig. 9A), whereas a threefold increase was observed in total IgA but not in IgG-secreting cells (data not shown).
FIG. 9.
Detection of antibody-secreting cells in the bone marrow and protection from lethal challenge 5 months postimmunization. (A) PR8-specific antibody-producing cells. Bone marrow cells were collected from naïve and influenza HA VLP-immunized mice. The spots for antibody-producing cells from the bone marrow were counted and expressed based on 1 × 106 total bone marrow cells per well. (B) Survival rates after challenge infection. Groups of mice immunized with 10 μg of VLPs (six mice per group) were challenged with lethal doses of influenza virus (10× LD50) 5 months postimmunization and monitored daily for morbidity and mortality.
To determine whether the VLP immune sera collected 5 months after the final immunization have a protective role, naïve mice were administered immune or normal sera intranasally and then challenged with a lethal dose of PR8 or WSN virus (Table 2). Naïve mice that received influenza HA VLP immune sera were protected against a lethal virus challenge of both strains, but mice that received normal sera (Table 2) or HA-negative M1 VLP immune sera were not protected (data not shown). Also, naïve mice infected with a lethal dose of virus first and then administered VLP immune sera 2 h postinfection were protected, indicating the therapeutic value of the immune sera (data not shown).
TABLE 2.
Protective role of immune seraa
| Group | Clinical sign(s) | Protection (%) |
|---|---|---|
| Naïve + PR8 | Sick, loss of wt, dead | 0 |
| Normal sera + PR8 | Sick, loss of wt, dead | 0 |
| Immune sera + PR8 | Healthy | 100 |
| Naïve + WSN | Sick, loss of wt, dead | 0 |
| Normal sera + WSN | Sick, loss of wt, dead | 0 |
| Immune sera + WSN | Healthy | 100 |
Naïve mice were intranasally administered pooled sera from mice immunized with influenza HA VLPs (immune sera) or naïve mouse serum (normal sera). Then, mice were challenge infected with a lethal dose (10× LD50) of live PR8 or WSN after 2 h. The mouse survival and body weight changes were recorded daily.
The induction of long-lasting protective immunity is a critical requirement for an effective vaccine. To determine whether the influenza HA VLP-immunized mice maintain protective immunity after 5 months, we challenged these mice with a lethal dose of virus (Fig. 9B). All VLP-immunized mice survived the lethal challenge, and we did not observe body weight changes or any sign of illness (Fig. 9B). These results demonstrate that VLP immunization can induce long-lived antibody-secreting plasma cells and protective immunity even 5 months postimmunization.
DISCUSSION
We have investigated detailed immune responses induced by influenza VLPs, including antibody isotypes, neutralizing activity, cellular immune responses, and induction of memory responses, which have not been investigated previously. In addition, our findings provide evidence that influenza VLPs containing HA, but not HA-negative M1 VLPs, can induce protective immunity against a lethal virus challenge with homologous as well as heterologous virus strains.
Immunization with recombinant influenza virus HA proteins was previously demonstrated to afford protection in chickens against challenge infection (5). However, preparing HA proteins with high purity as a vaccine candidate on a large scale may require a high-cost manufacturing process. In this regard, the production and purification processes of influenza VLPs in insect cells can be relatively simple and easily scalable. Insect cells do not add sialic acids to the N-glycans during posttranslational modifications (16), which explains why VLPs with HA are effectively released from the insect cell surfaces in this and other studies (8). Nonetheless, it will be interesting to determine the effect of neuraminidase coexpression on VLP budding and yield in the insect cells. In addition, incorporating an additional component, neuraminidase, into VLPs would be an advantage for an influenza virus vaccine, although VLPs containing influenza virus HA and M were found to be effective in inducing protective immune responses in the absence of adjuvants.
Maintaining the VLP structure and functionality of HA are expected to be important for inducing protective immunity. It is likely that the HA molecules on the surfaces of the VLPs maintain the native-like conformation as evidenced by hemagglutination activity and cleavability of HA in VLPs. Disrupting the intact VLP structure and inactivating the hemagglutination activity of HA abrogated the humoral immune responses against A/PR8 virus and did not induce protective immunity. Therefore, the particulate nature and intactness of VLPs are critically important in inducing protective immunity and may be necessary in facilitating interaction with antigen-presenting cells leading to strong immune responses. In support of this notion, HIV VLPs were found to preferentially interact with CD11b+ monocyte/macrophage and B220+ B-cell populations in vitro (present study).
The current, parenterally administered influenza virus vaccine is considered to provide protective immunity against circulating viruses by inducing neutralizing antibodies directed against HA, although it is relatively less effective against antigenic variants within a subtype (1). Serum antibodies induced by intranasal immunization with VLPs were found to have the capability to neutralize virus infectivity in vitro. We demonstrated that intranasal immunization with PR8 VLPs can confer 100% protection against PR8 as well as WSN strains using a 10× LD50 dose without any clinical symptoms, and VLP-immunized mice also survived a lethal dose of both strains as high as 200× LD50 with some weight loss (data not shown). The PR8 HA has approximately 91% amino acid homology with WSN HA on the basis of sequence analysis (GenBank accession numbers NC_004521 and ABF47955 for PR8 HA and WSN HA, respectively). Reflecting serological differences between A/PR8 and A/WSN, in addition to differences in lung viral titers, hemagglutination inhibition titers and neutralizing activity of PR8 VLP immune sera against A/WSN were two- to threefold less than those against A/PR8. Also, sera of mice infected with sublethal doses of WSN showed four- to eightfold differences in binding antibody titers against PR8 compared to those of the homologous antigen WSN, and this serologic difference was similarly observed when sera of mice infected with sublethal doses of PR8 were tested (data not shown). Nonetheless, we observed cross-reactive binding antibodies against A/WSN in VLP immune sera, and humoral and cellular immune responses were rapidly expanded upon lethal virus challenge with PR8 or WSN. Therefore, our studies demonstrate that influenza VLPs can be developed as a candidate vaccine. It will be of interest to determine whether the immune responses induced by influenza VLPs are cross-reactive with more distantly related strains within the same subtype. Influenza M1 VLPs can incorporate different subtype HAs, resulting in mixed influenza VLPs, and experiments to determine whether such phenotypically mixed VLPs can provide protection against influenza viruses of different subtypes are in progress.
An important goal of vaccination is to induce memory immune responses, which can provide long-term protective immunity. The cells responsible for memory response are T and B lymphocytes that can persist for long periods of time and can quickly be reactivated following infection. Induction of memory cells has been mostly investigated following live virus infection (30, 39), but not much is known about memory responses after immunization with nonreplicating VLP vaccines. A fraction of memory B lymphocytes developed in the secondary lymphoid organs is routed to the bone marrow, resides there as long-lived plasma cells, and secretes antibodies, maintaining long-term serum antibody levels. We observed the presence of influenza virus-specific antibody-secreting plasma cells in the bone marrow of the VLP-immunized mice and found that VLP-immunized mice were protected equally well 4 weeks or 5 months after the final immunization. In addition, naïve mice that received intranasal administration of heat-treated immune sera collected 5 months postvaccination were completely protected from lethal virus challenge with either homologous or heterologous strains (Table 2), demonstrating the protective role of antibodies induced by VLPs. Taken together, these results suggest that influenza VLPs can induce the differentiation of B cells to long-lived plasma cells secreting antibodies, which may play a role in maintaining long-term protective immunity.
Lung cytokine-mediated immunoinflammatory reactions as well as infiltration of activated lymphocytes may be a cause of the morbidity and mortality associated with influenza virus infections (21, 27, 35). We observed that high levels of IL-6 and IFN-γ were detected in naïve or HA-negative M1 VLP-immunized mouse lungs after challenge, whereas little or no proinflammatory cytokines were present in the lungs of the influenza HA VLP-immunized mice. Also, there seems to be a correlation between lung viral titers and the levels of inflammatory cytokines. This is consistent with a previous study demonstrating that high levels of lung viral titers and proinflammatory cytokines (IFN-α and IL-6) were found in the lungs of pigs with swine influenza virus infection (35). Also, lymphocytes expressing CD69, an activation marker, were lower in influenza HA VLP-immunized mice than in naïve mice after challenge (data not shown). Thus, influenza VLP immunization can prevent immunopathologic lung inflammation upon influenza virus infection.
In summary, our results demonstrate that influenza VLPs can induce neutralizing antibodies and cellular immune responses, which can confer protection against lethal virus infection by homologous or heterologous strains within the same subtype. In addition, mucosal antibody and cellular immune responses induced by influenza VLPs were rapidly expanded upon challenge virus infection, inhibiting viral replication and lung inflammatory cytokine production. These results provide insight for developing effective prophylactic vaccines based on VLPs to fight pathogenic influenza viruses that pose a pandemic threat.
Acknowledgments
This work was supported by NIH/NIAID grant AI0680003.
We thank Huan Nguyen for the mouse-adapted influenza virus A/PR8/34 strain, Yumiko Matsuoka for the influenza virus A/WSN/33 strain, Hong Yi for assistance with electron microscopy, Joshy Jacob for critical reading of the manuscript, and Tanya Cassingham for assistance in preparing the manuscript.
Footnotes
Published ahead of print on 24 January 2007.
REFERENCES
- 1.Ada, G. L., and P. D. Jones. 1986. The immune response to influenza infection. Curr. Top. Microbiol. Immunol. 128:1-54. [DOI] [PubMed] [Google Scholar]
- 2.Antonis, A. F., C. J. Bruschke, P. Rueda, L. Maranga, J. I. Casal, C. Vela, L. A. Hilgers, P. B. Belt, K. Weerdmeester, M. J. Carrondo, and J. P. Langeveld. 2006. A novel recombinant virus-like particle vaccine for prevention of porcine parvovirus-induced reproductive failure. Vaccine 24:5481-5490. [DOI] [PubMed] [Google Scholar]
- 3.Asahi-Ozaki, Y., T. Yoshikawa, Y. Iwakura, Y. Suzuki, S. Tamura, T. Kurata, and T. Sata. 2004. Secretory IgA antibodies provide cross-protection against infection with different strains of influenza B virus. J. Med. Virol. 74:328-335. [DOI] [PubMed] [Google Scholar]
- 4.Carroll, S. M., and J. C. Paulson. 1985. Differential infection of receptor-modified host cells by receptor-specific influenza viruses. Virus Res. 3:165-179. [DOI] [PubMed] [Google Scholar]
- 5.Crawford, J., B. Wilkinson, A. Vosnesensky, G. Smith, M. Garcia, H. Stone, and M. L. Perdue. 1999. Baculovirus-derived hemagglutinin vaccines protect against lethal influenza infections by avian H5 and H7 subtypes. Vaccine 17:2265-2274. [DOI] [PubMed] [Google Scholar]
- 6.Daniels, P. S., S. Jeffries, P. Yates, G. C. Schild, G. N. Rogers, J. C. Paulson, S. A. Wharton, A. R. Douglas, J. J. Skehel, and D. C. Wiley. 1987. The receptor-binding and membrane-fusion properties of influenza virus variants selected using anti-haemagglutinin monoclonal antibodies. EMBO J. 6:1459-1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deng, Y., J. W. Yewdell, L. C. Eisenlohr, and J. R. Bennink. 1997. MHC affinity, peptide liberation, T-cell repertoire, and immunodominance all contribute to the paucity of MHC class I-restricted peptides recognized by antiviral CTL. J. Immunol. 158:1507-1515. [PubMed] [Google Scholar]
- 8.Galarza, J. M., T. Latham, and A. Cupo. 2005. Virus-like particle (VLP) vaccine conferred complete protection against a lethal influenza virus challenge. Viral Immunol. 18:244-251. [DOI] [PubMed] [Google Scholar]
- 9.Gomez-Puertas, P., C. Albo, E. Perez-Pastrana, A. Vivo, and A. Portela. 2000. Influenza virus matrix protein is the major driving force in virus budding. J. Virol. 74:11538-11547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo, L., X. Lu, S. M. Kang, C. Chen, R. W. Compans, and Q. Yao. 2003. Enhancement of mucosal immune responses by chimeric influenza HA/SHIV virus-like particles. Virology 313:502-513. [DOI] [PubMed] [Google Scholar]
- 11.Harro, C. D., Y. Y. Pang, R. B. Roden, A. Hildesheim, Z. Wang, M. J. Reynolds, T. C. Mast, R. Robinson, B. R. Murphy, R. A. Karron, J. Dillner, J. T. Schiller, and D. R. Lowy. 2001. Safety and immunogenicity trial in adult volunteers of a human papillomavirus 16 L1 virus-like particle vaccine. J. Natl. Cancer Inst. 93:284-292. [DOI] [PubMed] [Google Scholar]
- 12.Jeong, S. H., M. Qiao, M. Nascimbeni, Z. Hu, B. Rehermann, K. Murthy, and T. J. Liang. 2004. Immunization with hepatitis C virus-like particles induces humoral and cellular immune responses in nonhuman primates. J. Virol. 78:6995-7003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang, S. M., L. Guo, Q. Yao, I. Skountzou, and R. W. Compans. 2004. Intranasal immunization with inactivated influenza virus enhances immune responses to coadministered simian-human immunodeficiency virus-like particle antigens. J. Virol. 78:9624-9632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang, S. M., M. G. Narducci, C. Lazzeri, A. M. Mongiovi, E. Caprini, A. Bresin, F. Martelli, J. Rothstein, C. M. Croce, M. D. Cooper, and G. Russo. 2005. Impaired T- and B-cell development in Tcl1-deficient mice. Blood 105:1288-1294. [DOI] [PubMed] [Google Scholar]
- 15.Kawaoka, Y., S. Yamnikova, T. M. Chambers, D. K. Lvov, and R. G. Webster. 1990. Molecular characterization of a new hemagglutinin, subtype H14, of influenza A virus. Virology 179:759-767. [DOI] [PubMed] [Google Scholar]
- 16.Lanford, R. E., V. Luckow, R. C. Kennedy, G. R. Dreesman, L. Notvall, and M. D. Summers. 1989. Expression and characterization of hepatitis B virus surface antigen polypeptides in insect cells with a baculovirus expression system. J. Virol. 63:1549-1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Latham, T., and J. M. Galarza. 2001. Formation of wild-type and chimeric influenza virus-like particles following simultaneous expression of only four structural proteins. J. Virol. 75:6154-6165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li, Z. N., S. N. Mueller, L. Ye, Z. Bu, C. Yang, R. Ahmed, and D. A. Steinhauer. 2005. Chimeric influenza virus hemagglutinin proteins containing large domains of the Bacillus anthracis protective antigen: protein characterization, incorporation into infectious influenza viruses, and antigenicity. J. Virol. 79:10003-10012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.LoBue, A. D., L. Lindesmith, B. Yount, P. R. Harrington, J. M. Thompson, R. E. Johnston, C. L. Moe, and R. S. Baric. 2006. Multivalent norovirus vaccines induce strong mucosal and systemic blocking antibodies against multiple strains. Vaccine 24:5220-5234. [DOI] [PubMed] [Google Scholar]
- 20.Nayak, D. P., E. K. Hui, and S. Barman. 2004. Assembly and budding of influenza virus. Virus Res. 106:147-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oda, T., T. Akaike, T. Hamamoto, F. Suzuki, T. Hirano, and H. Maeda. 1989. Oxygen radicals in influenza-induced pathogenesis and treatment with pyran polymer-conjugated SOD. Science 244:974-976. [DOI] [PubMed] [Google Scholar]
- 22.O'Neal, C. M., J. D. Clements, M. K. Estes, and M. E. Conner. 1998. Rotavirus 2/6 viruslike particles administered intranasally with cholera toxin, Escherichia coli heat-labile toxin (LT), and LT-R192G induce protection from rotavirus challenge. J. Virol. 72:3390-3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oran, A. E., and H. L. Robinson. 2003. DNA vaccines, combining form of antigen and method of delivery to raise a spectrum of IFN-gamma and IL-4-producing CD4+ and CD8+ T cells. J. Immunol. 171:1999-2005. [DOI] [PubMed] [Google Scholar]
- 24.Pushko, P., T. M. Tumpey, F. Bu, J. Knell, R. Robinson, and G. Smith. 2005. Influenza virus-like particles comprised of the HA, NA, and M1 proteins of H9N2 influenza virus induce protective immune responses in BALB/c mice. Vaccine 23:5751-5759. [DOI] [PubMed] [Google Scholar]
- 25.Qiao, C. L., K. Z. Yu, Y. P. Jiang, Y. Q. Jia, G. B. Tian, M. Liu, G. H. Deng, X. R. Wang, Q. W. Meng, and X. Y. Tang. 2003. Protection of chickens against highly lethal H5N1 and H7N1 avian influenza viruses with a recombinant fowlpox virus co-expressing H5 haemagglutinin and N1 neuraminidase genes. Avian Pathol. 32:25-32. [DOI] [PubMed] [Google Scholar]
- 26.Quan, F. S., R. W. Compans, Y. K. Cho, and S. M. Kang. 2007. Ginseng and salviae herbs play a role as immune activators and modulate immune responses during influenza virus infection. Vaccine 25:272-282. [DOI] [PubMed] [Google Scholar]
- 27.Rainsford, K. D. 2006. Influenza (“bird flu”), inflammation and anti-inflammatory/analgesic drugs. Inflammopharmacology 14:2-9. [DOI] [PubMed] [Google Scholar]
- 28.Scholtissek, C. 1991. Synthesis and function of influenza A virus glycoproteins. Behring Inst. Mitt. 1991:46-53. [PubMed] [Google Scholar]
- 29.Shortridge, K. F., N. N. Zhou, Y. Guan, P. Gao, T. Ito, Y. Kawaoka, S. Kodihalli, S. Krauss, D. Markwell, K. G. Murti, M. Norwood, D. Senne, L. Sims, A. Takada, and R. G. Webster. 1998. Characterization of avian H5N1 influenza viruses from poultry in Hong Kong. Virology 252:331-342. [DOI] [PubMed] [Google Scholar]
- 30.Slifka, M. K., and R. Ahmed. 1996. Limiting dilution analysis of virus-specific memory B cells by an ELISPOT assay. J. Immunol. Methods 199:37-46. [DOI] [PubMed] [Google Scholar]
- 31.Steinhauer, D. A. 1999. Role of hemagglutinin cleavage for the pathogenicity of influenza virus. Virology 258:1-20. [DOI] [PubMed] [Google Scholar]
- 32.Stephenson, I., K. G. Nicholson, J. M. Wood, M. C. Zambon, and J. M. Katz. 2004. Confronting the avian influenza threat: vaccine development for a potential pandemic. Lancet Infect. Dis. 4:499-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tamura, S., Y. Samegai, H. Kurata, T. Nagamine, C. Aizawa, and T. Kurata. 1988. Protection against influenza virus infection by vaccine inoculated intranasally with cholera toxin B subunit. Vaccine 6:409-413. [DOI] [PubMed] [Google Scholar]
- 34.Tumpey, T. M., M. Renshaw, J. D. Clements, and J. M. Katz. 2001. Mucosal delivery of inactivated influenza vaccine induces B-cell-dependent heterosubtypic cross-protection against lethal influenza A H5N1 virus infection. J. Virol. 75:5141-5150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Reeth, K., S. Van Gucht, and M. Pensaert. 2002. Correlations between lung proinflammatory cytokine levels, virus replication, and disease after swine influenza virus challenge of vaccination-immune pigs. Viral Immunol. 15:583-594. [DOI] [PubMed] [Google Scholar]
- 36.Webby, R. J., D. R. Perez, J. S. Coleman, Y. Guan, J. H. Knight, E. A. Govorkova, L. R. McClain-Moss, J. S. Peiris, J. E. Rehg, E. I. Tuomanen, and R. G. Webster. 2004. Responsiveness to a pandemic alert: use of reverse genetics for rapid development of influenza vaccines. Lancet 363:1099-1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Webster, R. G., W. J. Bean, O. T. Gorman, T. M. Chambers, and Y. Kawaoka. 1992. Evolution and ecology of influenza A viruses. Microbiol. Rev. 56:152-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wood, J. M., and J. S. Robertson. 2004. From lethal virus to life-saving vaccine: developing inactivated vaccines for pandemic influenza. Nat. Rev. Microbiol. 2:842-847. [DOI] [PubMed] [Google Scholar]
- 39.Woodland, D. L., R. J. Hogan, and W. Zhong. 2001. Cellular immunity and memory to respiratory virus infections. Immunol. Res. 24:53-67. [DOI] [PubMed] [Google Scholar]
- 40.Wright, P., and R. Webster. 2001. Orthomyxoviruses, p. 1533-1579. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 4th ed., vol. 2. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 41.Zhou, L. J., and T. F. Tedder. 1996. CD14+ blood monocytes can differentiate into functionally mature CD83+ dendritic cells. Proc. Natl. Acad. Sci. USA 93:2588-2592. [DOI] [PMC free article] [PubMed] [Google Scholar]