Abstract
Pain-related coping, particularly catastrophizing, plays a significant role in shaping pain responses. One way catastrophizing is hypothesized to amplify pain and disability is via its effect on patients, social environments (e.g., communal coping model), though empirical support is limited. The present study tested whether the association between catastrophizing and deleterious pain-related outcomes was mediated by patients’ perceptions of significant others’ responses to their pain in a sample of 1,356 pain patients. Regression analyses showed that perceived significant other punishing responses partially mediated catastrophizing’s relationship with pain-related disability, and with depressive symptoms. Further, several variables moderated the association between catastrophizing and perceived social responses to pain. Catastrophizing was more strongly associated with greater perceived solicitous responses for patients of relatively short pain duration. Also, higher catastrophizing was more strongly associated with perceived punishing responses among patients perceiving lower social support. In addition, the mediational effects of perceived punishing responses on catastrophizing’s relationship with depressive symptoms, and with pain-related disability were only found in individuals reporting low levels of perceived social support. In sum, perceived social responses were found to play a small role in mediating the relationship between catastrophizing and pain-related outcomes, and these mediational effects may be strongest in particular patient subgroups. The present data suggest that interpersonal mechanisms may not constitute a primary route by which catastrophizing exerts its maladaptive effects on pain responses. The study and further understanding of what principal factors mediate catastrophizing’s deleterious effects on pain will be important in illuminating the biopsychosocial model of pain.
Keywords: Chronic Pain, Pain, Catastrophizing, Communal Coping Model, Solicitous Responses, Punishing Responses
1. Introduction
Catastrophizing, a negative cognitive-affective process that includes elements of magnification, helplessness, pessimism, and rumination, is a consistently important predictor of pain-related outcomes (Sullivan et al. 2001a). Cross-sectionally, more frequent catastrophizing is reliably associated with heightened pain experience and emotional distress across many chronically painful conditions (Sullivan et al. 2001a), although the potentially beneficial effects of catastrophizing early in the course of chronic pain have also been identified (Jensen et al. 2002). Moreover, recent prospective studies in healthy adults (Picavet et al. 2002), and patients with acute (Edwards et al. 2004),or chronic pain (Covic et al. 2003;Haythornthwaite et al. 2003) have revealed that catastrophizing is a risk factor for multiple deleterious pain outcomes. These findings have stimulated interest in understanding how catastrophizing exerts its effects.
One mechanism by which catastrophizing may enhance pain and disability is via its effects on the social environment. Within a communal coping model (CCM) framework, catastrophizing can be conceptualized as a coping strategy that activates the individual’s social environment, for instance by soliciting support or empathy. Within this framework, provision of desirable and/or reinforcing responses such as expressions of sympathy may be more important to patients than reductions in pain or disability (Keefe et al. 2000; Sullivan et al. 2000). Partially supporting this model, researchers have observed positive associations between catastrophizing and perceived solicitous responses (Giardino et al. 2003;Cano 2004), perceived instrumental support (Keefe et al. 2003), and perceived critical responses to pain (Boothby et al. 2004), suggesting that catastrophizing may elicit a broad variety of interpersonal responses. Collectively, however, the magnitude of associations between perceived social responses and catastrophizing has varied substantially across studies, and factors such as pain duration (Cano 2004) and the immediacy of social contacts (Giardino et al. 2003) may moderate these relationships. Generally, both perceived solicitous and punishing responses to pain are associated with higher pain intensity (Romano et al., 2000; Giardino et al., 2003) and elevated depressive symptoms (Boothby et al. 2004;Cano 2004), suggesting that these social inputs might form part of the mechanism by which catastrophizing exerts its detrimental effects on pain outcomes (Sullivan et al. 2001a).
While one specific interpretation of the CCM implies a mediational model for catastrophizing’s effects (i.e., the association between catastrophizing and deleterious pain outcomes is at least partially accounted for by perceived social responses), no existing research has directly evaluated this particular version of the CCM. We hypothesized that perceived solicitous and punishing responses to pain would at least partially mediate the relationship between catastrophizing and pain severity, pain interference, and depressive symptoms. Further, building upon previous findings, we explored the moderating roles of pain duration (Cano 2004) and social support (Giardino et al. 2003;Cano 2004), the only documented moderators of catastrophizing’s associations with the social environment. Given prior findings, we expected that catastrophizing would show the strongest associations with perceived solicitous responses in the context of shorter pain durations, and that catastrophizing and perceived punishing responses would show the largest relationship under conditions of low perceived social support.
2. Method
2.1. Participants
Participants were 1,365 pain patients referred to three different multidisciplinary pain treatment programs, all of which were tertiary care facilities located within university hospitals. Each treatment program was comprised of a multidisciplinary treatment team (e.g., psychologists, physical therapists, physicians, nurses); patients were typically referred to the programs by healthcare professionals in the surrounding community. Generally, the patients referred to these programs had experienced pain for a number of years, and had not received adequate long-term benefit from multiple other treatment approaches. Consistent with epidemiological data, the majority of pain patients in the study were women (i.e., approximately 57%). Ages of participants ranged from 18 to 95 with a mean age of 45.8 (SD = 13.9). The racial breakdown of the sample was approximately 79% Caucasian, 13% African-American, and 5% Hispanic with relatively small percentages of patients representing other racial groups. The average duration of pain was 4.8 years (SD = 6.8; ranging from 3 months to 47.32 years). The majority of patients in the sample were married (68%), and 53% reported a 12th grade education or higher. A plurality of patients reported low back pain (37%), with 24% referred for lower limb pain, and 18% referred for upper limb pain. The characteristics of these patients are relatively typical for this type of tertiary-care pain treatment setting (i.e., a variety of different etiologies and locations of pain, lengthy durations of pain complaints, etc.). Unfortunately, given the size of the samples involved and the likely variability among treating physicians in diagnosing pain conditions, we were unable to obtain more specific diagnostic information than the primary location of pain reported by the patients.
2.2. Measures
2.2.1. Demographics
Demographic information was collected from all participants for descriptive purposes. Specifically, information was gathered about gender, age, ethnicity, marital status, pain duration, pain location, and level of education.
2.2.2. The Beck Depression Inventory (BDI)
The BDI is one of the most commonly-used measures of depressive symptomatology; it assesses the frequency and severity of a variety of cognitive, affective, physiological, and motivational symptoms of depression (Beck et al. 1961). Each item is scored on a four-point scale (0–3) with higher scores reflecting more severe symptoms. The BDI has well-established psychometric properties (Beck et al. 1988).
2.2.3. The Coping Strategies Questionnaire (CSQ)
The CSQ is a 50-item self-administered questionnaire designed to measure the frequency with which patients report the use of a variety of pain coping strategies (Rosenstiel and Keefe 1983). The CSQ is comprised of seven subscales that assess particular cognitive and behavioral coping strategies. Subjects use a seven-point Likert scale that ranges from 0 (never) to 6 (always) to indicate how often they use each strategy when they experience pain. The catastrophizing subscale is a well-validated, six-item scale, which is the most frequently-used measure of catastrophizing (Sullivan et al. 2001a).
2.2.4. The Multidimensional Pain Inventory (MPI)
The MPI is a 52-item self-administered questionnaire that assesses a range of psychosocial variables associated with the experience of chronic pain (Kerns et al. 1985). Items query respondents about pain severity and the impact of pain on the patient’s life (Section I), perceived responses of the social environment to the patient’s pain (Section II), and the daily activity level of the patient (Section III). These three sections include 12 subscales in which the four subscales from section III can be combined to create a General Activity factor score. Five of the MPI subscales were used in the present study: Pain severity (3 items, e.g., On average, how severe has your pain been during the past week?), Interference (9 items, e.g., In general, how much does your pain interfere with your day-to-day activities?), Support (3 items, e.g., How supportive or helpful is your spouse (significant other) to you in relation to your pain?), Punishing responses (4 items; e.g., “Your spouse expresses irritation at you when you are in pain”), and Solicitous responses (6 items; e.g., “Your spouse gets you something to eat or drink when you are in pain”). All items on the MPI are rated on a scale of 0–6. All MPI subscales have adequate construct and discriminant validity, internal consistency, and test-retest reliability (Kerns et al. 1985;Kerns and Jacob 1992).
2.3. Procedure
Research participants were recruited from patients referred to multidisciplinary pain treatment facilities in three university hospital clinics. During their initial clinic visit, patients completed the aforementioned questionnaires assessing pain and psychosocial adjustment, and these questionnaires were kept on file. A de-identified data set was created and used in these analyses; the relevant Institutional Review Boards approved all study procedures.
2.4. Data Analyses
Pearson Product-Moment correlations were conducted to examine the bivariate relationships between patients’ level of catastrophizing, pain severity, pain interference, depressive symptoms and perceived significant other responses to pain (see Table 1). Correlation analyses were also performed prior to hierarchical analyses in order to identify potential covariates. Variables were selected for inclusion as a covariate if they were significantly related to the dependent variable used in the analysis at P < 0.05. The following variables were assessed as potential covariates: age, pain duration, sex, education, marital status, and race. Further, outcome variables were included as covariates when not being treated as a dependent variable (DV).
Table 1.
Correlations between catastrophizing, partner response variables, and outcome measures
| M | SD | Catastrophizing | Punish Response | Solicit Response | Support | BDI | Pain Severity | Pain Interfere | Pain Duration | |
|---|---|---|---|---|---|---|---|---|---|---|
| Catastrophizing | 2.6 | 1.6 | 1.00 | |||||||
| Punishing Responses | 1.9 | 1.6 | 0.30** | 1.00 | ||||||
| Solicitous Responses | 3.7 | 1.6 | 0.15** | −0.23** | 1.00 | |||||
| Support | 4.8 | 1.4 | 0.06* | −0.34** | 0.62** | 1.00 | ||||
| BDI | 14.8 | 10.0 | 0.61** | 0.34** | 0.05 | −0.02 | 1.00 | |||
| Pain Severity | 4.6 | 1.0 | 0.43** | 0.14** | 0.25** | 0.20** | 0.31** | 1.00 | ||
| Pain Interference | 4.6 | 1.1 | 0.47** | 0.23** | 0.24** | 0.19** | 0.46** | 0.57** | 1.00 | |
| (Yrs) Pain Duration | 4.8 | 6.8 | 0.03 | 0.02 | −0.08** | −0.08** | 0.08** | 0.04 | 0.01 | 1.00 |
P < .01
P < 0.05
Regression analyses were used to test mediational models of pain-related catastrophizing, perceived social responses (punishing/solicitous responses), and outcomes (pain severity/pain interference/depressive symptoms) using the criteria outlined by (Baron and Kenny 1986): (1) the IV (catastrophizing) must be significantly associated with the DV (pain severity/pain interference/depressive symptoms); (2) the IV (catastrophizing) must be significantly associated with the mediator (perceived punishing/solicitous responses); (3) the mediator (perceived punishing/solicitous responses) must be significantly associated with the DV (pain severity/pain interference/depressive symptoms) after controlling for the IV (catastrophizing); and (4) the strength of the relationship between the IV (catastrophizing) and the DV (pain severity/pain interference/depressive symptoms) must be significantly reduced after controlling for the mediator (perceived punishing/solicitous responses). Covariates were entered in the first step of the regression analyses and these four conditions were tested with a set of three regression equations similar to the following:
| Eq1 |
| Eq2 |
| Eq3 |
where b01, b02, and b03 represent intercepts in the equation and b1, b2, b3, and b4 represent unstandardized regression coefficients. The four conditions necessary to demonstrate a mediational model are (1) b1 in Eq1 must be significant; (2) b2 in Eq2 must be significant; (3) b4 in Eq3 must be significant; and (4) b3 in Eq3 must be significantly smaller than b1 in Eq1.
Regression analyses were also used to test the moderating effects of pain duration and of social support on the relationship between catastrophizing and perceived significant other responses (i.e., punishing/solicitous responses). Based on prior findings (Giardino et al. 2003;Cano 2004), we expected that the relationship between catastrophizing and perceived significant other responses would be different at different levels of pain duration and of social support. Therefore, regression analyses tested main effects and their interaction following the recommendations of (Cohen 1988) and (Holmbeck 2002), which included centering catastrophizing, pain duration, and social support prior to analysis and using these centered scores to compute interaction terms. Post hoc probing of significant interactions provided the simple slopes of catastrophizing and the moderators. For example, separate regression lines were generated for the sample’s mean pain duration, as well as ± one standard deviation (Holmbeck 2002). Lastly, moderated mediation was investigated by repeating the mediational analyses at both high and low levels of social support (i.e., ± 1 SD from the mean), which allowed us to determine whether the mediational effects of perceived social responses to pain differed as a function of the moderating variable social support. Given that one standard deviation above the mean yielded a value exceeding the maximum score for social support, the mediation analyses were conducted in the portion of the subject sample with a maximum score on the MPI social support subscale.
3. Results
3.1. Simple Correlations
In the present study, as expected, pain catastrophizing was moderately positively correlated with depressive symptoms, pain severity, and pain interference (see Table 1). Catastrophizing was also modestly and positively related to both perceived solicitous and punishing responses. Perceived punishing and solicitous responses were negatively correlated with one another and both were positively related to pain severity and pain interference, while only perceived punishing responses were associated with depressive symptoms.
3.2. Mediation of catastrophizing-outcome relationships by perceived punishing responses
Regression analyses indicated that perceived punishing responses were not significantly related to pain severity after controlling for catastrophizing (i.e., condition 3 was not met). The non-significant relationship precluded further testing of the hypothesis that perceived punishing responses mediated the relationship between catastrophizing and pain severity. In testing the mediation of the catastrophizing-pain interference association by perceived punishing responses, regression analyses revealed that catastrophizing was significantly related to pain interference (condition 1) and perceived punishing responses (condition 2), and perceived punishing responses were significantly related to pain interference after controlling for catastrophizing (condition 3). Condition 4 was also met, as the relationship between catastrophizing and pain interference was significantly (though slightly) reduced (from β = 0.12 to 0.11; z = 2.02, P < 0.05) when perceived punishing responses were included in the regression equation. This effect represents partial mediation, as the relationship between catastrophizing and pain interference remains significant (t(1358) = 4.07, P < 0.001) even when perceived punishing responses are included in the regression equation (see Table 2).
Table 2.
Results of regression analyses testing the role of perceived punishing responses in mediating the effects of catastrophizing on pain interference
| Step Variable | Unstandardized β | Standard Error | Standardized β | t |
|---|---|---|---|---|
| Eq. (1): DV = Pain Interference | ||||
| 1. Age | −0.00 | 0.00 | −0.03 | −1.21 |
| Education | −0.01 | 0.05 | −0.00 | −0.16 |
| Pain Severity | 0.47 | 0.03 | 0.44 | 18.79** |
| Depressive Sx | 0.03 | 0.00 | 0.25 | 9.67** |
| 2. Catastrophize | 0.09 | 0.02 | 0.12 | 4.38** |
| Eq. (2): DV = Punishing Responses | ||||
| 1. Education | −0.06 | 0.08 | −0.02 | −0.73 |
| Gender | −0.33 | 0.08 | −0.10 | −4.02** |
| Pain Severity | −0.05 | 0.05 | −0.04 | −1.09 |
| Interference | 0.10 | 0.05 | 0.07 | 2.08* |
| Depressive Sx | 0.04 | 0.01 | 0.24 | 7.14** |
| 2. Catastrophize | 0.14 | 0.04 | 0.14 | 4.01** |
| Eq. (3): DV = Pain Interference | ||||
| 1. Age | −0.00 | 0.00 | −0.03 | −1.22 |
| Education | −0.01 | 0.05 | −0.00 | −0.11 |
| Pain Severity | 0.47 | 0.03 | 0.44 | 18.84** |
| Depressive Sx | 0.03 | 0.00 | 0.24 | 9.02** |
| 2. Catastrophize | 0.08 | 0.02 | 0.11 | 4.07** |
| Punishing Resp | 0.04 | 0.02 | 0.05 | 2.27* |
P < 0.05
P < 0.01
Table 3 summarizes the results of the regression equations that support a role for partial mediation of perceived punishing responses in the relationship between catastrophizing and depressive symptoms. Specifically, catastrophizing was significantly related to depressive symptoms (condition 1) and perceived punishing responses (condition 2), and perceived punishing responses were significantly related to depressive symptoms after controlling for catastrophizing (condition 3). Condition 4 was also met, as the relationship between catastrophizing and depressive symptoms was significantly reduced (from β = 0.50 to 0.46; z = 3.47, P < 0.001) when perceived punishing responses were included in the regression equation. This effect represents partial mediation, as the relationship between catastrophizing and depressive symptoms remains significant (t(1356) = 18.98, P < 0.001) even when perceived punishing responses are included in the regression equation.
Table 3.
Results of regression analyses testing the role of perceived punishing responses in mediating the effects of catastrophizing on depressive symptoms
| Step Variable | Unstandardized β | Standard Error | Standardized β | t |
|---|---|---|---|---|
| Eq. (1): DV = Depressive Symptoms | ||||
| 1. Age | −0.05 | 0.02 | −0.07 | −3.35** |
| Education | −0.40 | 0.42 | −0.02 | −0.95 |
| Pain Duration | 0.01 | 0.00 | 0.08 | 3.96** |
| Marital Status | 0.86 | 0.45 | 0.04 | 1.93 |
| Pain Severity | −0.61 | 0.25 | −0.06 | −2.44* |
| Interference | 2.30 | 0.24 | 0.26 | 9.78** |
| 2. Catastrophize | 3.19 | 0.15 | 0.50 | 20.74** |
| Eq. (2): DV = Punishing Responses | ||||
| 1. Education | −0.06 | 0.08 | −0.02 | −0.73 |
| Gender | −0.33 | 0.08 | −0.10 | −4.02** |
| Pain Severity | −0.05 | 0.05 | −0.04 | −1.09 |
| Interference | 0.10 | 0.05 | 0.07 | 2.08* |
| Depressive Sx | 0.04 | 0.01 | 0.24 | 7.14** |
| 2. Catastrophize | 0.14 | 0.04 | 0.14 | 4.01** |
| Eq. (3): DV = Depressive Symptoms | ||||
| 1. Age | −0.05 | 0.02 | −0.07 | −3.34** |
| Education | −0.32 | 0.41 | −0.02 | −0.78 |
| Pain Duration | 0.01 | 0.00 | 0.08 | 3.91** |
| Marital Status | 0.86 | 0.44 | 0.04 | 1.97 |
| Pain Severity | −0.53 | 0.25 | −0.06 | −2.16* |
| Interference | 2.13 | 0.23 | 0.24 | 9.14** |
| 2. Catastrophize | 2.95 | 0.16 | 0.46 | 18.98** |
| Punishing Resp | 0.90 | 0.13 | 0.15 | 6.78** |
P < 0.05
P < 0.01
3.5. Mediation by perceived solicitous responses
Similar regression equations were used to examine whether perceived solicitous responses mediated the effect of catastrophizing on pain severity, pain interference, and depressive symptoms. In all three cases, condition 2 was not satisfied (catastrophizing was not significantly related to perceived solicitous responses in the regression equations), so no further tests of the mediational role of perceived solicitous responses were conducted. That is, after controlling for relevant covariates (i.e., pain duration, race, marital status, education, pain interference, and pain severity), the small positive association between catastrophizing and perceived solicitous responses was rendered non-significant.
3.6. Moderation of associations between catastrophizing and perceived social responses by pain duration
The interaction between catastrophizing and pain duration was significant for perceived solicitous responses but not for perceived punishing responses to the patient’s pain (see Table 4). The simple slopes provided from post hoc probing are displayed in Figure 1. Pain catastrophizing was positively and significantly related to perceived solicitous responses to pain, with this association being stronger among patients with shorter (−1 SD) pain durations (β= 0.23; SE = 0.04; Beta = 0.23; t = 6.17, P < 0.001), relative to longer (+ 1 SD) pain durations (β= 0.08; SE = 0.04; Beta = 0.08; t = 2.3, P = 0.02).
Table 4.
Results of regression analyses testing the role of pain duration in moderating the effects of catastrophizing on perceived solicitous and punishing responses
| Step Variable | β | SE | Beta | R2 | ΔR2 |
|---|---|---|---|---|---|
| DV = Solicitous Responses | |||||
| 1. Catastrophizing | 0.16 | 0.03 | 0.16** | ||
| Pain Duration | −0.00 | 0.00 | −0.08** | 0.03 | 0.03** |
| 2. Catastrophizing × Pain Duration | −0.001 | 0.000 | −0.08** | 0.04 | 0.01** |
| DV = Punishing Responses | |||||
| 1. Catastrophizing | 0.31 | 0.03 | 0.30** | ||
| Pain Duration | 0.00 | 0.00 | 0.01 | 0.09 | 0.09** |
| 2. Catastrophizing × Pain Duration | 0.00 | 0.00 | 0.00 | 0.09 | 0.00 |
P < 0.01
Figure 1.
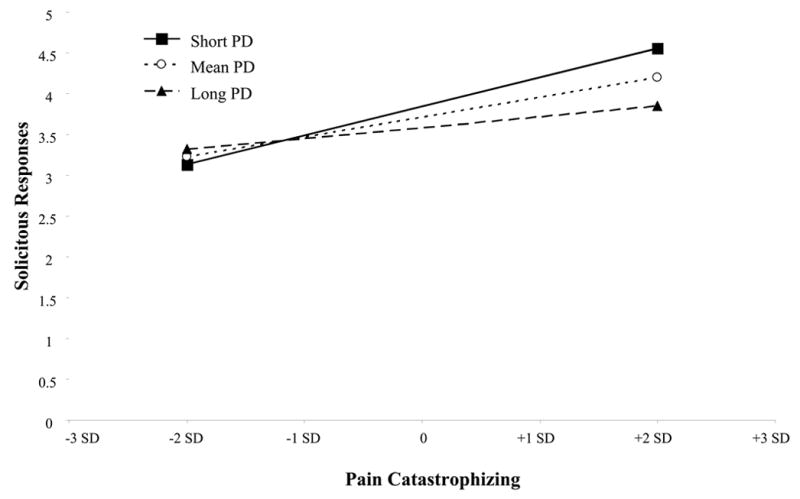
Interaction of Pain Duration with Pain Catastrophizing on Perceived Solicitous
Responses
PD = Pain Duration; SD = Standard Deviation
3.7. Moderation of associations between catastrophizing and perceived social responses by perceived social support
The interaction between catastrophizing and perceived social support was significant for perceived punishing responses but not for perceived solicitous responses to the patient’s pain (see Table 5). Figure 2 shows the simple slopes provided from post hoc comparisons. As depicted in figure 2, the positive association between catastrophizing and perceived punishing responses was strongest at lower levels of perceived social support. Pain catastrophizing was positively and significantly related to perceived punishing responses to pain among patients with lower levels (−1 SD) of perceived social support (β= 0.44; SE = 0.03; Beta = 0.43; t = 13.19, P < 0.001), with a less strong (though still significant) association observed at higher levels (+ 1 SD) of perceived social support (β= 0.23; SE = 0.04; Beta = 0.22; t = 6.47, P < 0.001).
Table 5.
Results of regression analyses testing the role of social support in moderating the effects of catastrophizing on perceived punishing and solicitous responses
| Step Variable | β | SE | Beta | R2 | ΔR2 |
|---|---|---|---|---|---|
| DV = Solicitous Responses | |||||
| 1. Catastrophizing | 0.11 | 0.02 | 0.11** | ||
| Social Support | 0.69 | 0.02 | 0.61** | 0.40 | 0.40** |
| 2. Catastrophizing × Social Support | −0.01 | 0.02 | −0.01 | 0.40 | 0.00 |
| DV = Punishing Responses | |||||
| 1. Catastrophizing | 0.33 | 0.03 | 0.32** | ||
| Social Support | −0.40 | 0.03 | −0.35** | 0.22 | 0.22** |
| 2. Catastrophizing × Social Support | −0.08 | 0.02 | −0.11** | 0.24 | 0.02** |
P < 0.01
Figure 2.
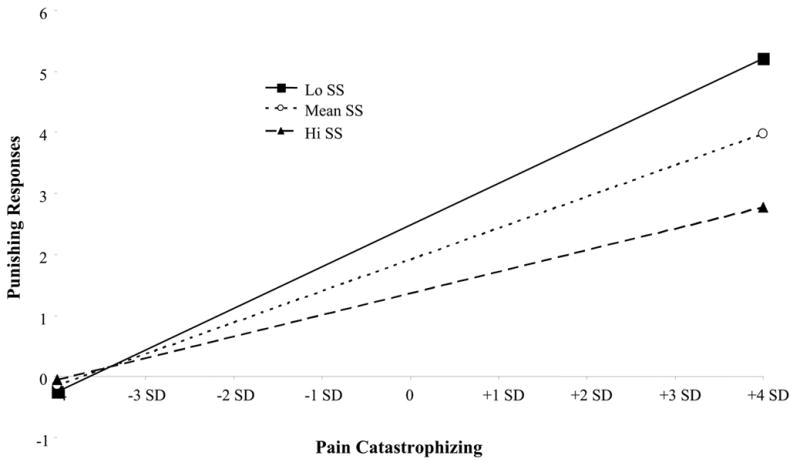
Interaction of Perceived Global Social Support with Pain Catastrophizing on Perceived
Punishing Responses
SS = Social Support; SD = Standard Deviation
3.8. Perceived social support moderating the mediational effects of perceived punishing responses
Given that perceived social support acted as a moderator of the catastrophizing-perceived punishing responses relationship, and not of the catastrophizing-perceived solicitous responses relationship, we only examined whether perceived punishing responses were a stronger mediator of catastrophizing’s effects on pain outcomes at low levels of perceived social support. The results support a role for partial mediation of perceived punishing responses in the relationship between catastrophizing and depressive symptoms for patients with a low (−1 SD) MPI social support score (i.e., ≤ 3.42) but not for patients with a high (+1 SD) MPI social support score (i.e., =6). At lower levels of perceived social support, catastrophizing was significantly related to depressive symptoms (condition 1) and perceived punishing responses (condition 2), and perceived punishing responses were significantly related to depressive symptoms after controlling for catastrophizing (condition 3). Condition 4 was also met, as the relationship between catastrophizing and depressive symptoms was significantly reduced (from β= 0.40 to 0.32; z = 2.34, P = 0.02) when perceived punishing responses were included in the regression equation. This effect represents partial mediation, as the relationship between catastrophizing and depressive symptoms remains significant (t(215) = 4.80, P < 0.001) even when perceived punishing responses are included in the regression equation. In contrast, for patients high in perceived social support, perceived punishing responses were not significantly related to pain interference after controlling for catastrophizing (i.e., condition 3 was not met).
Similarly, when examining pain interference as a DV, the results supported a mediational role for perceived punishing responses in the relationship between catastrophizing and pain interference for patients low in perceived social support score (i.e., MPI Social Support < 3.42), but not for patients high in perceived social support. At lower levels of perceived social support, catastrophizing was significantly related to pain interference (condition 1) and perceived punishing responses (condition 2), and perceived punishing responses were significantly related to pain interference after controlling for catastrophizing (condition 3). Condition 4 was also met, as the relationship between catastrophizing and pain interference was significantly reduced (from β= 0.18 to 0.12; z = 2.33, P = 0.02) when perceived punishing responses were included in the regression equation. This effect represents full mediation, as the relationship between catastrophizing and pain interference ceased to be significant (t(215) = 1.90, P = 0.06) when perceived punishing responses are included in the regression equation. In contrast to these findings at low levels of perceived social support, catastrophizing was not significantly related to perceived punishing responses at high levels of perceived social support (i.e., condition 3 was not met), indicating no mediational effects.
4. Discussion
In light of prior studies investigating catastrophizing’s activation of the social environment, it is believed that the social environment may exert a mediational effect on catastrophizing’s association with deleterious pain-related outcomes. Thus, the objective of the present study was to investigate the relationship between catastrophizing and pain-related outcomes in a way that incorporated perceived significant other solicitous and punishing responses as mediators and pain duration and perceived social support as moderators of those relationships. The results of the present study indicate that pain patients’ perception of their significant other’s punishing responses to their pain partially mediates the association between catastrophizing and depressive symptoms and between catastrophizing and pain interference. In analyses of perceived punishing responses, social support moderated the relationship between catastrophizing and perceived punishing responses whereas pain duration did not. Thus, catastrophizing was related to a perception of increased punishing responses when pain patients had a perception of low social support and to a perception of fewer punishing responses when pain patients perceived higher levels of social support. Among patients reporting lower social support, perceived punishing responses partially mediated the relationship between catastrophizing and depressive symptoms and fully mediated the relationship between catastrophizing and pain interference; these mediating effects were not observed among patients reporting higher social support. Although solicitous responses did not mediate the relationship between catastrophizing and pain outcomes, pain duration was found to moderate the relationship between catastrophizing and perceived solicitous responses. That is, catastrophizing was related to a perception of greater perceived solicitous responses at shorter pain durations, and a perception of fewer solicitous responses at longer pain durations. Perceived social support did not moderate the relationship between catastrophizing and perceived solicitous responses.
In general, in the present sample, catastrophizing was more strongly associated with perceived punishing responses than with perceived solicitous responses (e.g., solicitous responses did not mediate or partially mediate catastrophizing’s relationships with pain severity, pain interference, or depressive symptoms), though patients with a shorter duration of pain tended to show a stronger association between catastrophizing and solicitous responses. This is consistent with prior studies of chronic pain patients, which have also shown stronger relationships between catastrophizing and punishing responses than between catastrophizing and solicitous responses (Boothby et al. 2004), and have reported similar moderating effects of pain duration on the association between catastrophizing and solicitous responses (Cano 2004).
Based on previous accounts of the communal coping model (CCM) of catastrophizing and on the particular interpretation that social responses play a mediational role between catastrophizing and deleterious pain-related outcomes, it was expected that perceived significant other responses would play a substantial mediational role in the relationship between catastrophizing and negative pain-related outcomes. However, catastrophizing’s association with pain severity was not mediated to any degree by perceived solicitous or punishing responses, and catastrophizing’s associations with pain-related interference and with depressive symptoms were only slightly attenuated after controlling for perceived punishing responses, except in particular subgroups (i.e., those who were low in perceived social support). Collectively, the rather small magnitude of these effects suggests that perceived social responses may not be the most important mediator of catastrophizing’s effects on negative pain-related outcomes. The CCM of catastrophizing posits that catastrophizing is a coping strategy designed to elicit empathy, sympathy, or social support from others, which may actually be more important than whether the empathy or support reduce pain or pain-related disability. In this regard, it is interesting to note that perceived punishing and solicitous responses were significantly inversely related to each other while both were positively and significantly related to catastrophizing. Catastrophizing, therefore, appears to evoke not just sympathetic and supportive responses, but also critical and frustrated responses, which may in fact be more influential in contributing to pain-relevant outcomes.
Collectively, the CCM is more of a theoretical framework for predicting catastrophizing’s effects than a specific model with operationalized variables. For example, the particular interpretation of the CCM that we are testing (i.e., the mediational role of social responses) does not specify which aspects of the social environment are affected by expressions of pain-related catastrophizing, and similarly does not indicate exactly which pain-related parameters are subsequently modified by the social environment, and in what manner. Thus, while the CCM has been of substantial heuristic value in shaping research on one possible/potential pathway (i.e., the elicitation of interpersonal responses) by which catastrophizing may operate, future studies would certainly benefit from testing more concrete pathways (Thorn et al. 2004). That is, a patient’s expressions of catastrophizing might independently affect the patient’s perception of a spouse’s typical behavioral responses to expressions of pain (i.e., ignoring the patient, providing instrumental support, calling a doctor, etc.), a spouse’s verbal communications directed towards the patient (which might include empathy, criticism, encouragement, frustration, worry, solicitousness, anger, etc.), others’ willingness to spend time with the patient, a spouse’s facial expressions during the patient’s verbalizations, etc. In the current catastrophizing literature, a patient’s verbal and behavioral expressions of catastrophizing are rarely, if ever, measured (i.e., generally, self-report of catastrophizing on a written questionnaire is assessed), and the responses of others are also rarely measured, either by their self-report, psychophysiological recording, behavioral observation, etc. Such multi-person, multi-modal evaluation of interpersonal transactions in the context of pain would likely help to substantially clarify the potentially important impact of catastrophizing on the social and interpersonal environments of patients in pain. Furthermore, given the potential moderating effects of variables such as pain duration, these studies will benefit from being performed in specific subgroups of patients in order to isolate catastrophizing’s effects.
It is important to note several limitations of the present study. First, though support for a mediating role of perceived social responses was found, the magnitude of the coefficients was small. It should also be noted that the social responses measured in the present study comprise only a subset of the social responses that may be affected by catastrophizing. Additional research will be needed to replicate these findings as well as investigate other potential mediating factors. Second, given the cross-sectional design of this study, causal associations cannot be determined. Third, patient diagnoses were not available, thus precluding the investigation of diagnostic specificity as a potentially important moderator of the association between catastrophizing and pain-related outcomes. Fourth, a unidimensional measure of catastrophizing was used; in future studies, the use of a multi-component measure such as the Pain Catastrophizing Scale (PCS) (Sullivan et al. 1995) may yield richer information. Fifth, there were no data available regarding patients who were approached but chose not participate in the study, possibly introducing selection bias into the sample. Another limitation is that 32% of the study sample was not married, and while they followed the standard MPI instructions and it is assumed that they answered the questions with a significant other in mind, this cannot be independently verified. Lastly, further studies using longitudinal data collection strategies (e.g., diary studies) and more directly assessing social interactions (e.g., as opposed to measuring perceived social responses as was done in this study) will be important in elucidating catastrophizing’s effects on the social environments of patients in pain. In sum, in spite of its limitations, the present study provides some support for a partial mediational model in which the association between catastrophizing and pain related outcomes is partially accounted for by pain patients’ perceptions of their significant others’ punishing responses to their expressions of pain. The findings suggest that future research into the role of factors that mediate the association between catastrophizing and pain-related outcomes may be fruitful in assisting to better understand the process of catastrophizing, and in designing interventions that can ameliorate its effects.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This work was supported in part by NIH grants F32DE017282(LFB), K23AR051315(RRE), and K24NS002225(JAH).
References
- Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward E, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- Boothby JL, Thorn BE, Overduin LY, Charles WL. Catastrophizing and perceived partner responses to pain. Pain. 2004;109:500–506. doi: 10.1016/j.pain.2004.02.030. [DOI] [PubMed] [Google Scholar]
- Cano A. Pain catastrophizing and social support in married individuals with chronic pain: the moderating role of pain duration. Pain. 2004;110:656–664. doi: 10.1016/j.pain.2004.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Covic T, Adamson B, Spencer D, Howe G. A biopsychosocial model of pain and depression in rheumatoid arthritis: a 12-month longitudinal study. Rheumatology (Oxford) 2003 doi: 10.1093/rheumatology/keg369. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Fillingim RB, Maixner W, Sigurdsson A, Haythornthwaite J. Catastrophizing predicts changes in thermal pain responses after resolution of acute dental pain. J Pain. 2004;5:164–170. doi: 10.1016/j.jpain.2004.02.226. [DOI] [PubMed] [Google Scholar]
- Engel JM, Schwartz L, Jensen MP, Johnson DR. Pain in cerebral palsy: the relation of coping strategies to adjustment. Pain. 2000;88:225–230. doi: 10.1016/S0304-3959(00)00330-4. [DOI] [PubMed] [Google Scholar]
- Flor H, Breitenstein C, Birbaumer N, F++rst M. A psychophysiological analysis of spouse solicitousness towards pain behaviors, spouse interaction, and pain perception. Behav Ther. 1995;26:255–272. [Google Scholar]
- Flor H, Kerns RD, Turk DC. The role of spouse reinforcement, perceived pain, and activity levels of chronic pain patients. J Psychosom Res. 1987;31:251–259. doi: 10.1016/0022-3999(87)90082-1. [DOI] [PubMed] [Google Scholar]
- Giardino ND, Jensen MP, Turner JA, Ehde DM, Cardenas DD. Social environment moderates the association between catastrophizing and pain among persons with a spinal cord injury. Pain. 2003;106:19–25. doi: 10.1016/s0304-3959(03)00226-4. [DOI] [PubMed] [Google Scholar]
- Haythornthwaite JA, Clark MR, Pappagallo M, Raja SN. Pain coping strategies play a role in the persistence of pain in post-herpetic neuralgia. Pain. 2003;106:453–460. doi: 10.1016/j.pain.2003.09.009. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. J Pediatr Psychol. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Ehde DM, Hoffman AJ, Patterson DR, Czerniecki JM, Robinson LR. Cognitions, coping and social environment predict adjustment to phantom limb pain. Pain. 2002;95:133–142. doi: 10.1016/s0304-3959(01)00390-6. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM, Karoly P. Coping with chronic pain: A critical review of the literature. Pain. 1991;47:249–283. doi: 10.1016/0304-3959(91)90216-K. [DOI] [PubMed] [Google Scholar]
- Keefe F, Brown G, Wallston K, Caldwell D. Coping with rheumatoid arthritis pain: Catastrophizing as a maladaptive strategy. Pain. 1989;37:51–56. doi: 10.1016/0304-3959(89)90152-8. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain. 2000;87:325–334. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Lipkus I, Lefebvre JC, Hurwitz H, Clipp E, Smith J, Porter L. The social context of gastrointestinal cancer pain: a preliminary study examining the relation of patient pain catastrophizing to patient perceptions of social support and caregiver stress and negative responses. Pain. 2003;103:151–156. doi: 10.1016/s0304-3959(02)00447-5. [DOI] [PubMed] [Google Scholar]
- Kerns R, Turk D, Rudy T. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Jacob MC. Assessment of the Psychosocial Context of the Experience of Chronic Pain. In: Turk DMR, editor. Handbook of Pain Assessment. New York: The Guilford Press; 1992. pp. 235–253. [Google Scholar]
- Martin MY, Bradley LA, Alexander RW, Alarcon GS, Triana-Alexander M, Aaron LA, Alberts Kr. Coping strategies predict disbilities in patients with primary fibromyalgia. Pain. 1996;68:45–53. doi: 10.1016/S0304-3959(96)03179-X. [DOI] [PubMed] [Google Scholar]
- Picavet HS, Vlaeyen JW, Schouten JS. Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am J Epidemiol. 2002;156:1028–1034. doi: 10.1093/aje/kwf136. [DOI] [PubMed] [Google Scholar]
- Romano JM, Jensen MP, Turner JA, Good AB, Hops H. Chronic pain patient-partner interactions: Further support for a behavioral model of chronic pain. Behav Ther. 2000;31:415–440. [Google Scholar]
- Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and Validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- Sullivan MJ, Stanish W, Waite H, Sullivan M, Tripp DA. Catastrophizing, pain, and disability in patients with soft-tissue injuries. Pain. 1998;77:253–260. doi: 10.1016/S0304-3959(98)00097-9. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001a;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, D’Eon JL. Relation between catstrophizing and depression in chronic pain patients. J Abnorm Psychol. 1990;99:260–263. doi: 10.1037//0021-843x.99.3.260. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Rodgers WM, Kirsch I. Catastrophizing, depression and expectancies for pain and emotional distress. Pain. 2001b;91:147–154. doi: 10.1016/s0304-3959(00)00430-9. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Tripp DA, Santor D. Gender differences in pain and pain behavior: The role of catastrophizing. Cognit Ther Res. 2000;24:121–134. [Google Scholar]
- Thorn BE, Keefe FJ, Anderson T. The communal coping model and interpersonal context: problems or process? Pain. 2004;110:505–507. doi: 10.1016/j.pain.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Turk DC, Rudy TE. Cognitive factors and persistent pain: A glimpse into Pandora’s box. Cognit Ther Res. 1992;16:99–122. [Google Scholar]


