Abstract
The development of second primary tumors has a negative impact on the prognosis of head and neck squamous cell carcinoma. Previously, we detected genetically altered and tumor-related mucosal lesions in the resection margins in 25% of unselected head and neck squamous cell carcinoma patients (Tabor MP, Brakenhoff RH, van Houten VMM, Kummer JA, Snel MHJ, Snijders PJF, Snow GB, Leemans CR, Braakhuis BJM: Persistence of genetically altered fields in head and neck cancer patients: biological and clinical implications. Clin Cancer Res 2001, 7: 1523–1532). The aim of this study was to determine whether first and second primary tumors are clonally related and originate from a single genetically altered field. From 10 patients we analyzed the first tumor of the oral cavity or oropharynx, the >3-cm remote second primary tumor, and the mucosa from the tumor-free margins from both resection specimens. We compared TP53 mutations and loss of heterozygosity profiles using 19 microsatellite markers at chromosomes 3p, 9p, 13q, and 17p. In all patients, genetically altered mucosal lesions were detected in at least one resection margin from both first and second primary tumor. Evidence for a common clonal origin of the first tumor, second primary tumor, and the intervening mucosa was found for at least 6 of 10 patients. Our results indicate that a proportion of multiple primary tumors have developed within a single preneoplastic field. Based on different etiology and clinical consequences, we propose that independent second primary tumors should be distinguished from second field tumors, that arise from the same genetically altered field the first tumor has developed from.
Head and neck squamous cell carcinoma (HNSCC) comprises ∼5% of all newly diagnosed cancer cases in the northern and western European countries and the United States. 1 Despite advances in therapy, long-term survival of HNSCC patients has only moderately improved during the last 20 years. 2 An important reason for this lack of progress is the development of second primary tumors in the upper aerodigestive tract. 3 The reported incidence of second primary tumors varies, but on average they develop at a constant rate of 2 to 3% new cases per year. 4 Patients at highest risk are those with early-stage disease, when control of the first (index) tumor, and therefore survival are greatest. 3 It is thus critical to learn more about the molecular mechanisms of developing second primary tumors to establish new strategies to identify patients at risk and to prevent second primary tumor development.
The development of HNSCC is a multistep process involving the accumulation of genetic and epigenetic alterations in key regulatory genes. 5 Deletion of somatic DNA at several tumor suppressor loci occurs early in HNSCC tumorigenesis and can be detected by microsatellite analysis. 5,6 Mutations in the TP53 tumor suppressor gene are present in the majority of the head and neck cancers, and seem to occur early in HNSCC carcinogenesis. 7-9
Originally, it was thought that all second primary tumors develop independently after widespread epithelial exposure to carcinogens. 10 By comparing TP53 mutations and microsatellite alterations in primary tumors and corresponding second primary tumors, indications have been found that supported this theory of independent origin. 11,12 In contrast, several other reports suggested that at least a proportion of second primary tumors in HNSCC patients have arisen from one clonal cell population. 13-17 Various mechanisms have been proposed to explain this proposed common clonal origin of second primary tumors such as shedding of (pre-)malignant cells into the saliva and implantation at other sites 14,16 or lateral migration of isolated (pre-)malignant cells. 13-17
We have recently found evidence for the existence of large genetically altered mucosal lesions (referred to as “fields”) in a significant proportion of patients with an oral or oropharyngeal tumor. 7 In 10 of 28 (36%) patients genetic alterations were detected in macroscopically normal mucosa surrounding the tumor, and in 7 of these 10 patients (25% of the total number) these mucosal lesions extended beyond the surgical resection margins. Genetic analysis strongly indicated a clonal relationship between tumor and accompanying genetically altered field. The picture emerges that these tumors have developed within a pre-existing preneoplastic field. In this model, a single genetically altered cell gives rise to a proliferating clone that develops into an expanding preneoplastic field and gradually replaces the normal mucosa. During progression within this genetically altered field various clones develop with additional genetic alterations. This is a continuous process of evolution and eventually multiple clones exist that are genetically different but share a common origin. One clone ultimately develops into a carcinoma. From the clinical point of view it is important to realize that after surgery of the first primary tumor, the nonresected field may progress further into a second primary tumor in adjacent areas. If this hypothesis is valid, the first and second primary tumors should have a common clonal origin and should share specific genetic alterations that are also present in the intervening genetically altered mucosa.
To test our hypothesis, we analyzed multiple primary oral and oropharyngeal tumors and their corresponding surgical resection margins from 10 patients. The clonal origin of the tumors was examined by studying patterns of allelic loss and TP53 mutations in the tumor samples and the intervening mucosa.
Materials and Methods
Patients and Tumor Specimens
Ten HNSCC patients who developed a second primary tumor in the period of 1995 to 2000 formed the basis of the present study. All patients fulfilled the following criteria: 1) all tumors must have been located in the oral cavity and/or in the oropharynx; 2) all tumors must have been of the squamous cell type; 3) all tumors must have been surgically resected to obtain mucosa of the routinely paraffin-embedded resection margins (used for histopathological assessment of complete tumor excision); 4) the first primary tumor must have been completely resected as assessed by conventional histopathological examination of the resection margins; 5) the second primary tumor and the first tumor must have been separated by at least 3 cm of nonneoplastic epithelium based on clinical and surgical findings (the distance between the tumors is an additional criterion to the ones proposed by Warren and Gates 18 and was larger than the 2 cm used by Hong and colleagues 19 ), and for the present study, it appeared that the first and second primary tumors were separated by a distance that varied between 3 and 6 cm; and 6) sufficient material should be available in the samples for DNA extraction and subsequent analysis. A total of 22 tumor samples were collected from these 10 patients. Seventeen tumor samples were obtained as archival paraffin-embedded tissue and five tumor samples as frozen material. The resection margins were obtained as archival paraffin-embedded tissue. From two patients (patients 4 and 7) with two synchronous HNSCCs an additional mucosal biopsy located between the two tumors was obtained during surgery. Patients’ characteristics are summarized in Table 1 ▶ . Tumor stages (pTN) were determined according to the International Union Against Cancer criteria. 20
Table 1.
Patient Characteristics and Clonal Relationship of Primary Tumor and Second Primary Tumor
| Patient | Sex | Lesion | Date | Site* | pTN | Clonality† |
|---|---|---|---|---|---|---|
| 1 | F | t1 | 7/97 | R retromolar trigone | T2N2b | Clonal |
| t2 | 12/97 | Anterior floor of mouth | T1N0 | |||
| 2 | M | t1 | 2/97 | L retromolar trigone | T2N0 | Not clonal |
| t2 | 2/97 | R mobile tongue | T2N0 | |||
| t3 | 4/98 | Uvula | T1N0 | |||
| 3 | M | t1 | 7/94 | L-lateral border of tongue | T2N0 | Clonal |
| t2 | 3/99 | L retromolar trigone | T1N0 | |||
| 4 | F | t1 | 5/99 | L base of tongue | T2N1 | Not clonal |
| t2 | 5/99 | R anterior tonsillar pillar | T1N0 | |||
| 5 | M | t1 | 11/92 | R lower alveolus | T4N1 | Clonal |
| t2 | 12/98 | R upper alveolus | T2N0 | |||
| 6 | M | t1 | 3/93 | R lower alveolus | T3N2b | Not clonal |
| t2 | 5/98 | R retromolar trigone | T2N0 | |||
| 7 | M | t1 | 11/00 | L retromolar trigone | T2N0 | Clonal |
| t2 | 11/00 | Anterior floor of mouth | T2N1 | |||
| 8 | M | t1 | 10/91 | L-lateral border of tongue | T1N0 | Clonal |
| t2 | 9/95 | Anterior floor of mouth | T1N0 | |||
| 9 | F | t1 | 3/95 | R buccal mucosa | T2N0 | Clonal |
| t2 | 4/96 | Soft palate | T2N0 | |||
| 10 | M | t1 | 2/88 | Anterior floor of mouth | T3N1 | Not clonal |
| t2 | 8/95 | L retromolar trigone | T4N0 | |||
| t3 | 8/95 | Uvula | T1N0 |
*L, left; R, right.
†Clonal relationship of the primary tumor and second primary tumor revealed by molecular analysis. All tumors that were clonally related originated from a single precursor lesion.
Microdissection of Tumor and Mucosa Samples
Freshly frozen tumor samples were cut on a cryomicrotome, and tissue sections (10 μm) were mounted on microscopic glass slides. From the paraffin-embedded tumor samples 10-μm sections were obtained, placed on microscopic glass slides, and subsequently deparaffinized in xylene. For all cases the first and last tissue sections were stained with hematoxylin and eosin (H&E) for histological analysis and to guide microdissection. The other tissue sections were stained with 1% toluidine blue and 0.2% methylene blue and manually microdissected under a stereomicroscope. All microdissected samples contained >80% of tumor cells.
From every tumor at least two paraffin-embedded margins were microdissected. We selected margins that were localized opposite the other tumor and were nearest to the virtual line that connects the tumors. When one of these two margins showed genetic alterations, we did not study any other margin. When both margins did not show genetic alterations, all other margins were studied as well. Histopathology and TP53 immunostaining were used to guide microdissection (see below). First, all H&E slides of the resection margins were examined and histopathologically abnormal mucosa was microdissected. Second, mucosa that showed clear suprabasal staining for TP53 was microdissected separately. When no histopathologically abnormal or TP53-positive stained mucosa was present, a part of the normal mucosa was selected at random and microdissected. All mucosal areas selected for microdissection were continuous in a given sample and encompassed at least 25% of the total mucosa of the resection margin.
Selection of Chromosomal Loci for Microsatellite Analysis
To assess genetic relationships between first tumor, second primary tumor, and both accompanying fields, we investigated loss of heterozygosity (LOH) by using 19 microsatellite markers located at chromosomes 3p, 9p, 17p, and 13q. These markers were selected because they frequently demonstrate LOH in HNSCCs and precursor lesions. 5,6,21 The following markers were used: D3S1284 (3p12), D3S1274 (3p12), D3S1217 (3p13), D3S1766 (3p14), D3S1029 (3p21), D3S1293 (3p24), D9S171 (9p21), D9S1748 (9p21), D9S1751 (9p21), IFNA (9p21), D9S162 (9p22), D9S157 (9p22), CHRNB1 (17p11-12), TP53 (17p13.1), D17S1866 (17p13.3), D13S294 (13q14.3), D13S168 (13q14.3), D13S170 (13q31), and D13S158 (13q32). Primer sequences were obtained from the Genome Database for all of these markers (http://gdbwww.gdb.org/).
DNA Extraction and Microsatellite Analysis
Dissected tissues were treated with 1 mg/ml of proteinase K for 24 hours at 52°C in a 100-μl buffer containing 100 mmol/L Tris-HCL (pH 9.0), 10 mmol/L NaCl, 1% sodium dodecyl sulfate, and 5 mmol/L ethylenediaminetetraacetic acid. The DNA was purified by phenol-chloroform extraction and collected by ethanol precipitation using 2 μg of glycogen as carrier. The DNA was redissolved in LoTE-buffer (3 mmol/L Tris, 0.2 mmol/L ethylenediaminetetraacetic acid, pH 7.5). Normal DNA was isolated from blood samples obtained at the time of surgery, from connective tissue or from muscle microdissected from the sections. The DNA concentration was measured by microfluorometry with the Hoefer Dynaquant (Amersham/Pharmacia Benelux NV, Roosendaal, The Netherlands).
Microsatellite analysis was performed on an automated ABI PRISM sequencer (310 Genetic Analyzer; Applied Biosystems, Nieuwerkerk a/d IJssel, The Netherlands). One primer (Isogen Bioscience, Maarssen, The Netherlands) of each marker was end-labeled with one of the fluorescent dyes FAM, HEX, or NED (Applied Biosystems). DNA (10 ng) was amplified by multiplex polymerase chain reaction (PCR) (involving two or three markers) in a total volume of 10 μl containing 2 pmol of each labeled and unlabeled primer. Details of the multiplex PCR are available on request. The PCR buffer included 10 mmol/L Tris-HCl (pH 8.3), 50 mmol/L KCl, 1.5 mmol/L MgCl2, 0.2 mmol/L deoxynucleotide triphosphate, and 0.5 U of Taq DNA polymerase (AmpliTaq; Perkin Elmer, Gouda, The Netherlands). PCR amplifications for each primer set were performed for 35 cycles consisting of denaturation at 94°C for 1 minute, annealing at a temperature between 55°C and 65°C (depending on the primer set) for 1 minute, and extension at 72°C for 2 minutes. The amplified product was diluted in sterilized water, usually fivefold. For analysis, 12 μl of deionized formamide were combined with 0.5 μl of Genescan-350 (ROX) size standard (Applied Biosystems) and 1 μl of diluted PCR product in a tube. The samples were loaded on the automated sequencer and run following the supplier’s protocol. The data were analyzed with GeneScan Analysis software (version 1.2, Applied Biosystems). LOH was scored if one allele was decreased by greater than 50% in the tumor sample when compared with the same allele in normal control DNA, when necessary after stutter correction as described previously. 22
Immunohistochemistry with Anti-TP53 Antibodies
Immunohistochemical staining was performed on the primary tumor samples and on the accompanying paraffin-embedded resection margins. The method used for TP53 staining was essentially as described by Cruz and colleagues. 23 Briefly, 5-μm sections were deparaffinized, placed in 0.3% methanolic peroxide (30 minutes) to block endogenous peroxidase activity, rinsed in phosphate-buffered saline, and subsequently subjected to antigen retrieval in 0.01 mol/L of sodium citrate buffer (pH 6.0) in a microwave oven (600 W at 100°C for 10 minutes). Preincubation with normal rabbit serum (1:50; DAKO, Copenhagen, Denmark) was followed by overnight incubation at 4°C with anti-TP53 monoclonal antibody DO7 (1:500, DAKO). Consecutive sections were incubated with mouse myeloma IgG monoclonal antibody (1:500; Zymed, San Francisco, CA) as a negative control. After incubation, slides were thoroughly washed and sections sequentially incubated with biotinylated rabbit anti-mouse antibody (1:500, DAKO) for 1 hour. Diaminobenzidine in H2O2 was used as chromogen (stained for 5 minutes). Sections were counterstained with hematoxylin, dehydrated, and mounted with xylene substitute mountant. The staining pattern of the tumor samples was assessed and was classified positive if more than 50% of the tumor cell nuclei were stained. The mucosa of the resection margins was scored positively when there was a clear suprabasal staining.
TP53 Sequencing
All tumors of the 10 HNSCC patients were sequenced for exons 5 to 9 of the TP53 gene. Sequencing was performed as described by Sidransky and colleagues 24 In short, a 1.8-kb fragment of the TP53 gene, encompassing exons 5 to 9, was amplified from DNA of microdissected frozen tumor specimens. For paraffin-embedded material the exons were amplified separately. Purified PCR products were directly sequenced by exon-specific primers using the radioactive dideoxynucleotide method (Applied Biosystems). 24 Primer sequences and reaction conditions are available on request. When no mutation was found in exons 5 to 9 of the TP53 gene, exon 4 was sequenced in addition. When a TP53 mutation was detected in DNA of the primary tumors, DNA isolated from the mucosa of the accompanying resection margins was subsequently sequenced for mutations in that particular exon.
Histopathological Classification
All H&E-stained slides were examined by an experienced pathologist (JEvdW) and scored according to the standard criteria of the World Health Organization international histological classification of tumors. 25 Lesions were classified as: 1) normal mucosa, 2) mild dysplasia, 3) moderate dysplasia, 4) severe dysplasia or carcinoma in situ, and 5) squamous cell carcinoma. The pathologist had no information on molecular data during histopathological classification.
Methodological Analysis
We tested the hypothesis that one genetically aberrant cell has evolved into a large field consisting of various subclones with related genetic patterns. Within this field two subclones developed into two carcinomas. As a consequence, all cells in the field and the tumors share one or more genetic aberration(s) characteristic for the primordial clone. To be considered “field” two criteria were applied: the dissected mucosal lesion should not be malignant according to routine histopathological criteria and LOH should be present in at least one marker. The likelihood that the various lesions (first tumor, field of first tumor, field of second primary tumor, and second primary tumor) are genetically related, and thus have a common clonal origin, was based on the comparison of TP53 mutations and LOH patterns. When the TP53 mutation was identical in primary tumor, field of primary tumor, field of second primary tumor, and second primary tumor, the clonal relationship was considered proven. As for the LOH pattern, the probability that this similarity arose by chance was calculated. The chromosomal locus 9p21 (markers D9S171, D9S1748, D9S1751, and IFNA) and/or the chromosomal arm of 17p (markers CHRNB1, TP53, and D17S1866) were selected because these loci particularly demonstrated LOH in genetically altered and tumor-related fields as has been shown previously. 5,7,26,27 When LOH patterns at 9p21 and/or 17p appeared to be similar then the most telomeric informative marker of either of these chromosomal loci was selected for probability calculation based on the LOH frequencies reported for these loci. Based on previous work, frequencies of LOH in HNSCCs at 9p21 and 17p were estimated as 0.93 and 0.70, respectively. 7,9 The probability that the same (paternal or maternal) allele was lost is therefore 0.5 × 0.93 = 0.465 and 0.5 × 0.70 = 0.35 for both markers. Genetic alterations at either chromosomal locus 9p21 or 17p were considered to be independent, allowing the multiplication of the probabilities when both loci were involved. The probabilities that a similar LOH pattern arose by chance in the four lesions investigated are calculated will be either (0.465)3 = 0.10 (only 9p21 involved), (0.35)3 = 0.04 (only 17p involved), or (0.465)3 × (0.35)3 = 0.004 (both 9p21 and 17p involved).
Results
Detection of Genetically Altered Fields in Resection Margins
In all 10 patients, genetically altered fields were detected in at least one resection margin from both first tumor and second primary tumor (Figure 1) ▶ . In nine patients, genetic alterations were detected in the one or two margins facing the other tumor. Only in patient 4, the two margins facing the other tumor did not show genetic alterations. However, in other margins of both tumors of this patient genetic alterations were detected. The genetic alterations were detected in mucosal lesions that encompassed at least 25% of the total epithelial layer of a surgical margin and were at least 4 mm in length. In most cases, the genetically altered mucosa showed similar genetic alterations when compared to the corresponding tumor, suggesting a clonal relationship. In a few cases the tumor and the corresponding resection margins, had no genetic alterations in common (eg, first tumor of patient 4 and corresponding margin Ct1 and patient 10 and margin At1).
Figure 1.
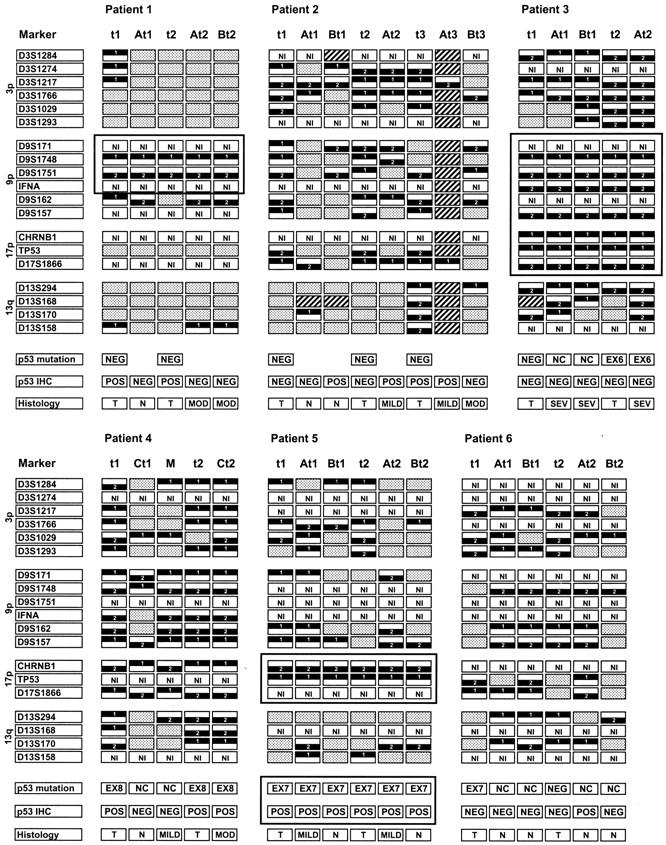

Results of the genetic analysis of the multiple primary tumors from 10 patients. t1, t2, and t3, represent the first tumor, second primary tumor, and third tumor, respectively. At1 and Bt1 represent the resection margins of the first primary tumor that were localized in the opposite direction to the second primary tumor and were nearest to the virtual line that connects both tumors. At2 and Bt2 represent the resection margins of the second primary tumor that were localized in the opposite direction to the first primary tumor. Only the margins that showed genetic alterations are presented. When no genetic alterations were detected in the two margins facing the other tumor, all other margins (with prefix Ct) were studied as well. Only in patient 4 were genetic alterations detected in other margins than the two margins facing the other tumor. M represents a mucosal biopsy that was located between the two synchronous tumors of patients 4 and 7. The TP53 mutations are indicated as NEG (negative) and EX4-9 when a mutation was detected in that particular exon. The codon and type of mutation are listed in Table 2 ▶ . NC indicates that TP53 mutation of the tumor could not be confirmed in the corresponding resection margins. The immunohistochemical staining for the TP53 protein (p53 IHC) was indicated as NEG (negative) and POS (positive). The samples were histopathologically classified as normal mucosa (N), mild dysplasia (MILD), moderate dysplasia (MOD), severe dysplasia (SEV), and squamous cell carcinoma (T). Genetic alterations that were present in the first and second primary tumor and both resection margins are placed in a framed box. In all these cases, the margins with genetic alterations were facing the other tumor, suggesting that these margins are part of a single preneoplastic field.
TP53 Mutation Analysis of the First Tumor, Second Primary Tumor, and Corresponding Resection Margins
Ten primary tumors and 12 second primary tumors from 10 patients were sequenced for TP53 mutations in exons 5 to 9. In nine tumors a single TP53 mutation was detected in exons 5 to 9, and in one tumor (patient 10, t2) two mutations were detected (Table 2) ▶ . In 12 tumors no mutation was found in exons 5 to 9 of the TP53 gene, and by additional sequencing of exon 4 an extra mutation could be identified in 1 of these 12 tumors (patient 7, Table 2 ▶ ).
Table 2.
Results of TP53-Immunostaining and TP53 Mutation Analysis in Primary Tumor and Second Primary Tumor
| Patient | Lesion* | TP53-immunostaining | Change† | Exon | Codon | Amino acid-change | Resection margins‡ |
|---|---|---|---|---|---|---|---|
| 1 | t1 | + | Wt | ||||
| t2 | + | Wt | |||||
| 2 | t1 | − | Wt | ||||
| t2 | − | Wt | |||||
| t3 | + | Wt | |||||
| 3 | t1 | − | Wt | ||||
| t2 | − | G → A | 6 | Intron | Splice site | Id. (At2) | |
| 4 | t1 | + | G → A | 8 | 273 | Arg → His | Neg. (Ct1, M) |
| t2 | + | G → A | 8 | 273 | Arg → His | Id. (Ct2) | |
| 5 | t1 | + | G → A | 7 | 244 | Gly → Asp | Id. (At1, Bt1) |
| t2 | + | G → A | 7 | 244 | Gly → Asp | Id. (At2, Bt2) | |
| 6 | t1 | − | G → A | 7 | Intron | Splice site | Neg. (At1, Bt1) |
| t2 | − | Wt | |||||
| 7 | t1 | + | 1 bp ins | 4 | 109 | Frameshift | Neg. (At1, M) |
| t2 | − | C → T | 6 | 196 | Arg → Stop | Neg. (At2, Bt2) | |
| 8 | t1 | + | Wt | ||||
| t2 | + | Wt | |||||
| 9 | t1 | + | A → T | 8 | 280 | Arg → Stop | Id. (At1, Bt1) |
| t2 | + | A → T | 8 | 280 | Arg → Stop | Id. (At2, Bt2) | |
| 10 | t1 | + | Wt | ||||
| t2 | + | G → A | 5 | 175 | Arg → His | ND | |
| A → T | 9 | Intron | Splice site | ND | |||
| t3 | + | Wt |
*t1 and t2 represent the first tumor and second primary tumor.
†wt, wild type; ins, insertion.
‡Id. means that the TP53 mutation of the tumor was identical to the mutation of the corresponding resection margins listed in parentheses. Neg. means that the mutation of the tumor was not confirmed in the samples of the corresponding margins listed in parentheses. ND means not determined, since the corresponding resection margins showed loss of the opposite allele at the TP53 locus (Figure 1) ▶ when compared to the primary tumor. For the codes of the samples listed in parentheses see Figure 1 ▶ .
From the 11 tumors in which a TP53 mutation was detected, we also tried to confirm the presence of the mutation in the mucosa of the corresponding resection margins (Table 2) ▶ . In six comparisons, the TP53 mutation of the tumor could also be detected in one or more resection margin(s). Three patients showed the same TP53 mutations in both first primary tumor and second primary tumor. In two of these three patients (patients 5 and 9), the same TP53 mutation could be detected in the mucosa of the resection margins of both the first and second primary tumor (Table 2 ▶ , Figure 1 ▶ ). To exclude the possibility that these concordant TP53 mutations were germ-line mutations, DNA of connective tissue and muscle from both patients was sequenced in addition. In both cases, the DNA of connective tissue and muscle showed wild-type TP53. In the third patient (patient 4), the TP53 mutation could only be detected in the mucosa of the resection margin of the second primary tumor and not in the resection margins of the first tumor. Furthermore, a mucosal biopsy of this patient (located between the primary tumor and second primary tumor) also lacked the TP53 mutation.
LOH Analysis of First Tumor, Second Primary Tumor, and Corresponding Resection Margins
From all 10 patients the first tumor, the second primary tumor, and mucosa of the corresponding resection margins of both tumors were analyzed for LOH. The results of the LOH analysis are summarized in Figure 1 ▶ . All tumors analyzed showed LOH at two or more chromosomal loci.
For none of the 10 patients was the LOH pattern of the first tumor completely identical to the LOH pattern of the corresponding second primary tumor, and it differed at least at five microsatellite markers. Five of 10 patients showed concordant LOH at one or more chromosomal loci in the first tumor, second primary tumor, and the corresponding margins of both tumors (Figure 1) ▶ . Patient 1 showed loss of the same alleles at 9p21 in the first tumor, its resection margin A, the second primary tumor, and its resection margins A and B (Figure 1) ▶ . Patients 3 and 8 showed loss of the same allele at 9p21, 9p22, and 17p in the first tumor, second primary tumor, and the resection margins of both tumors. Patient 7 showed the same LOH pattern at chromosome 17p in the first tumor, resection margin A of the primary tumor, mucosal biopsy M (located between the primary tumor and second primary tumor), resection margins A and B of the second primary tumor, and the second primary tumor. Finally, patient 5 showed the same LOH pattern at chromosomal loci 17p in the first tumor, the resection margins A and B of the first tumor, resection margin A and B of second primary tumor, and the second primary tumor (also the same TP53 mutation was detected in all samples of this patient, see above).
Interpretation of the Results and Molecular Assessment of Clonality
The hypothesis that the first tumor and second primary tumor have a common clonal origin and thus have developed from a large common premalignant field was considered to be confirmed in patients 5 and 9. Both tumors and accompanying resection margins of these patients showed the same TP53 mutation.
In contrast to TP53 mutations, LOH patterns are less specific and are much more likely to be identical by chance. For four cases (patients 1, 3, 7, and 8) concordant LOH at 9p21 and/or 17p13 was observed between the first tumor, the second primary tumor, and the intervening mucosa. The probability that this concordant LOH pattern arose by chance was calculated. As an example in patient 7 the resection margins closest to the virtual line between the tumors were At1 and At2. The mucosa of these margins was assigned as field-based on the presence of LOH. The first tumor, margin At1, margin At2, and second primary tumor showed loss of the same alleles at 17p. Microsatellite marker TP53 was used for calculation using LOH in the primary tumor as proband, and the probability that the pattern arose by chance was calculated as 1 × 0.35 × 0.35 × 0.35 = 0.043 or 4.3% (see Materials and Methods). The probabilities that the LOH patterns arose by chance were 0.43% for patient 3, 10% for patient 1, and 0.43% for patient 8. In this study we performed calculations based on the presence of a common LOH. The absence of LOH, however, was found at the chromosomal loci 3p14-3p24, 17p, and 13q14 for patient 1 and at chromosomal loci 13q14-13q32 for patient 9. If we had used this information in our calculations as well, then the probabilities that the similarity of LOH patterns arose by chance would have been lower for these two patients. We judged that sufficient evidence is provided that for 6 of 10 patients the first tumor and second primary tumor are clonally related and arose from a single primordial field. The molecular diagnosis of clonality is summarized in Table 1 ▶ .
Histology and Immunohistochemistry
All tumor samples and corresponding resection margins were reviewed and histopathologically classified and compared with the genetic analyses. A total of 37 paraffin-embedded surgical margins showing genetic alterations were histopathologically classified as: 13 as normal mucosa, 12 as mild dysplasia, 6 as moderate dysplasia, and 6 as severe dysplasia (see Figure 1 ▶ ). The two freshly frozen mucosal biopsies (located between the primary tumor and second primary tumor) that both showed LOH were classified as normal mucosa (patient 7) and mild dysplasia (patient 4).
All tumor samples and corresponding resection margins were analyzed by immunohistochemistry for overexpression of the TP53 protein. Fifteen of the 22 analyzed tumors showed intense TP53 staining of most tumor nuclei (Figure 1 ▶ , Table 2 ▶ ). In 8 of the 15 positively stained tumors, a TP53 mutation was identified (Table 2) ▶ . Twenty-three of the 37 surgical margins that showed genetic alterations demonstrated a clear suprabasal staining for the TP53 protein (Figure 1) ▶ .
Discussion
Second primary tumors are a major problem in head and neck oncology. Their development has a profound impact on long-term survival, particularly for patients with early-stage disease. Current understanding of the origin of these second tumors is limited. In the present study molecular techniques have been used to better understand the pathobiology of these lesions.
An important finding of this study was that the frequency of genetically altered field is very high in the total patient group. In all ten cases proof for field was detected, surrounding both first tumor and SPT. This prevalence of a genetically altered field is much higher than the 25% we have observed for a group of 28 unselected patients with a single oral or oropharyngeal tumor. 7 It should be noted, that although we have evaluated the same chromosomal loci, we used more markers in the current study; when the analysis is limited to the markers of the previous study one of the patients (number 1) would have been judged to be without a field. The overall results of the present study suggest that the presence of large genetically altered fields in one or more resection margin(s) is a risk factor for the development of SPT. Therefore, analyzing margins for the presence of genetically altered mucosa might identify the subgroup of patients at high risk for developing SPT. Whether (and which type of) an unresected genetically altered field eventually will develop into SPT, is not clear at this time and should be determined in a carefully designed study with larger patient groups. Other parameters should be taken into account as well, such as follow-up time, 26,28 smoking behavior 29,30 and specific genetic alterations. 28 If such a high-risk patient group can be identified chemoprevention or gene therapy are potential approaches to prevent the development of SPT.
Evidence was provided that genetically altered fields could be large. For six of the ten patients two primary tumors have developed in a contiguous geneticallly altered field. In all these six patients the first and second primary tumor were separated by 3 to 6 cm, indicating the large extension of these fields. Taking also the surface of the tumors into account, fields can have a diameter of over 7 cm.
On the basis of the results of the present and the previous study, 7 we propose a revised model for head and neck carcinogenesis. Large areas of normal mucosa are replaced by a population of genetically altered cells of monoclonal origin (referred to as an expanding field). Within such a field additional genetic hits may lead to the emergence of multiple genetically related subclones, and one eventually develops into cancer. In case of a very large field (> 3 cm diameter) SPT can develop. The mode by which these genetically altered cells replace the normal mucosa is unclear, but this expanding population of cells probably has a growth advantage as compared with the normal epithelial stem cells, and therefore overgrow the normal stem cells by a higher proliferation rate. Indeed, we have recently obtained proof that lesions with genetically altered cells have a higher proliferation rate than normal epithelial cells. 31 The presence of a large preneoplastic field to explain the mechanism of a common origin of first and second primary tumor make the other proposed mechanisms unlikely. 13-17
For four of the ten patients, no or in our opinion too little evidence of a single precursor lesion was found suggesting that these SPT were of independent origin. However, it should be emphasized that this may be an over-estimation and the possibility of a common initiating genetic alteration can not be completely excluded, as only a limited number of genetic markers were analyzed. To stress this point, patient 9 showed only an identical TP53 mutation in both tumors and their corresponding margins, whereas the LOH-patterns would never have been considered convincing evidence for a common clonal origin. As discussed above, all the four patients with seemingly unrelated tumors had genetically altered fields in margins of the first and second tumor. Some of these fields did not have a single genetic alteration similar to the tumor, suggesting an independent origin of tumor and field. Such independent fields have been reported before. 7
We have detected concordant TP53 mutations in the first tumor and second primary tumor in three cases. This is in contrast to other authors who failed to show similar TP53 mutations in the first tumor and second primary tumor. 11,12 In two cases (patients 5 and 9) the TP53 mutation was also present in the intervening mucosa of both tumors. Thus, for two cases convincing evidence was found that the first tumor and second primary tumor had the same clonal origin and that they had developed within a single preneoplastic lesion. In the third case (patient 4) an identical TP53 mutation was detected in both primary tumors, but this mutation could not be detected in any of the resection margins of the first tumor. Thus, the criterion for establishing the common origin of both tumors and the field in between was not fulfilled. Of notice, this TP53 mutation resulted in strong positive immunohistochemical staining of the tumors. The mucosa of the margins from the first tumor, however, did not show TP53 immunopositivity, which in our view is indicative for the absence of the common genetically altered field. It should be realized that this TP53 mutation was located at a hot spot (codon 273) in one of the most conserved areas of the TP53 gene. Mutations at this hot spot are detected at a percentage of 6 to 9% in primary tumors (our own unpublished data and Walker and colleagues 32 ). We therefore decided that these tumors do not have a common clonal origin, and do not share a common field. In support of this statement is that the LOH analysis revealed that the tumors had lost the opposite allele at the TP53 locus. There are, however, mechanisms, such as gene conversion and crossing over, which might explain the LOH of the opposite allele at the TP53 locus. So, it cannot be excluded completely that the tumors are genetically related, apparently without a common field.
The results of the present study suggest that inactivation of the tumor suppressor genes p14ARF, p16 (both at 9p21), and TP53 (located at 17p13) play a key role in the early malignant progression of a cell and are the initiating events in the mechanism of clonal expansion of a field. All three of these tumor suppressor genes play a crucial role in cell cycle regulation and/or apoptosis and are interacting at various levels. These tumor suppressor genes seem therefore to be the most promising molecular targets for prevention strategies.
The present results give further insight into the molecular mechanisms of second primary tumor development. Thus far, and also in the present study, the definition of second primary tumor is based on clinical parameters. Intriguingly, it is at this moment possible to discriminate between different ways of development of second primary tumor and the question arises whether every second tumor should be called a second primary tumor. In a recent article 33 we proposed a new classification of second tumors in adjacent sites for HNSCC, based on the genetic profile of the tumors and the intervening mucosal field. We propose to allocate the term “second primary tumor” for the second tumor that has developed independently from the first tumor. This type of cancer comes closest to the original clinical concept of second primary cancer. When a second tumor arises from the same field as the first tumor has developed, we propose to designate it as a “second field tumor.” It is more than a question of semantics; based on the different etiology, we believe it is important to make this discrimination. Moreover, there may be clinical consequences, eg, additional field tumors may require other screening and therapeutic approaches than real second primary tumors.
In conclusion, our study provides evidence that in a proportion of patients the primary tumor and second primary tumor develop from a single contiguous genetically altered field and thus have a common clonal origin. In other patients the first and second primary tumors develop independently from genetically unrelated fields. The picture emerges that in the second primary tumor patients large areas of the normal mucosa have been replaced by one or more monoclonal cell populations. Adequately identifying the presence of genetically altered fields and their risk for progression may have profound implications for the effective prevention of second primary tumor.
Footnotes
Address reprint requests to Dr. B. J. M. Braakhuis, Section Tumor Biology, Department of Otolaryngology/Head and Neck Surgery, VU University Medical Center, P.O. Box 7057, 1007 MB Amsterdam, The Netherlands. E-mail: bjm.braakhuis@vumc.nl.
Supported by a grant from the Dutch Cancer Society (VU 1998-1674).
References
- 1.Muir C, Weiland L: Upper aerodigestive tract cancers. Cancer 1995, 75:147-153 [DOI] [PubMed] [Google Scholar]
- 2.Vokes EE, Weichselbaum RR, Lippman SM, Hong WK: Head and neck cancer. N Engl J Med 1993, 328:184-194 [DOI] [PubMed] [Google Scholar]
- 3.Lippman SM, Hong WK: Second malignant tumors in head and neck squamous cell carcinoma: the overshadowing threat for patients with early-stage disease. Int J Radiat Oncol Biol Phys 1989, 17:691-694 [DOI] [PubMed] [Google Scholar]
- 4.Licciardello JT, Spitz MR, Hong WK: Multiple primary cancer in patients with cancer of the head and neck: second cancer of the head and neck, esophagus, and lung. Int J Radiat Oncol Biol Phys 1989, 17:467-476 [DOI] [PubMed] [Google Scholar]
- 5.Califano J, van der Riet P, Westra W, Nawroz H, Clayman G, Piantadosi S, Corio R, Lee D, Greenberg B, Koch W, Sidransky D: Genetic progression model for head and neck cancer: implications for field cancerization. Cancer Res 1996, 56:2488-2492 [PubMed] [Google Scholar]
- 6.Partridge M, Emilion G, Pateromichelakis S, Phillips E, Langdon J: Location of candidate tumour suppressor gene loci at chromosomes 3p, 8p and 9p for oral squamous cell carcinomas. Int J Cancer 1999, 83:318-325 [DOI] [PubMed] [Google Scholar]
- 7.Tabor MP, Brakenhoff RH, van Houten VMM, Kummer JA, Snel MHJ, Snijders PJF, Snow GB, Leemans CR, Braakhuis BJM: Persistence of genetically altered fields in head and neck cancer patients: biological and clinical implications. Clin Cancer Res 2001, 7:1523-1532 [PubMed] [Google Scholar]
- 8.Waridel F, Estreicher A, Bron L, Flaman JM, Fontolliet C, Monnier P, Frebourg T, Iggo R: Field cancerisation and polyclonal p53 mutation in the upper aerodigestive tract. Oncogene 1997, 14:163-169 [DOI] [PubMed] [Google Scholar]
- 9.Tabor MP, van Houten VMM, Kummer JA, Vosjan MJWD, Vlasblom R, Snow GB, Leemans CR, Braakhuis BJM, Brakenhoff RH: Discordance of genetic alterations between primary head and neck tumors and corresponding metastases is associated with mutational status of the TP53 gene. Genes Chromosom Cancer 2002, 33:168-177 [DOI] [PubMed] [Google Scholar]
- 10.Slaughter DP, Southwick HW, Smejkal W: “Field cancerization” in oral stratified squamous epithelium. Cancer 1953, 6:963-968 [DOI] [PubMed] [Google Scholar]
- 11.Chung KY, Mukhopadhyay T, Kim J, Casson A, Ro JY, Goepfert H, Hong WK, Roth JA: Discordant p53 gene mutations in primary head and neck cancers and corresponding second primary cancers of the upper aerodigestive tract. Cancer Res 1993, 53:1676-1683 [PubMed] [Google Scholar]
- 12.van Oijen MGCT, van der Straat FGJL, Tilanus MGJ, Slootweg PJ: The origins of multiple squamous cell carcinomas in the aerodigestive tract. Cancer 2000, 88:884-893 [DOI] [PubMed] [Google Scholar]
- 13.Worsham MJ, Wolman SR, Carey TE, Zarbo RJ, Benninger MS, Vandyke D: Common clonal origin of synchronous primary head and neck squamous cell carcinomas: analysis by tumor karyotypes and fluorescence in situ hybridization. Hum Pathol 1995, 26:251-261 [DOI] [PubMed] [Google Scholar]
- 14.Bedi GC, Westra WH, Gabrielson E, Koch W, Sidransky D: Multiple head and neck tumors: evidence for a common clonal origin. Cancer Res 1996, 56:2484-2487 [PubMed] [Google Scholar]
- 15.Scholes AGM, Woolgar JA, Boyle MA, Brown JS, Vaughan ED, Hart CA, Jones AS, Field JK: Synchronous oral carcinomas: independent or common clonal origin? Cancer Res 1998, 58:2003-2006 [PubMed] [Google Scholar]
- 16.Califano J, Leong PL, Koch WM, Eisenberger CF, Sidransky D, Westra WH: Second esophageal tumors in patients with head and neck squamous cell carcinoma: an assessment of clonal relationships. Clin Cancer Res 1999, 5:1862-1867 [PubMed] [Google Scholar]
- 17.Jang SJ, Chiba I, Hirai A, Hong WK, Mao L: Multiple oral squamous epithelial lesions: are they genetically related? Oncogene 2001, 20:2235-2242 [DOI] [PubMed] [Google Scholar]
- 18.Warren S, Gates O: Multiple primary malignant tumors. A survey of the literature and a statistical study. Am J Cancer 1932, 16:358-1414 [Google Scholar]
- 19.Hong WK, Lippman SM, Itri LM, Karp DD, Lee JS, Byers RM, Schantz SP, Kramer AM, Lotan R, Peters LJ, Dimery IW, Brown BW, Goepfert H: Prevention of second primary tumors with isotretinoin in squamous-cell carcinoma of the head and neck. N Engl J Med 1990, 323:795-801 [DOI] [PubMed] [Google Scholar]
- 20.Sobin LH, Wittekind C: Sobin LH Wittekind C eds. TNM Classification of Malignant Tumors, ed 5 1997. Wiley-Liss, New York
- 21.Gupta VK, Schmidt AP, Pashia ME, Sunwoo JB, Scholnick SB: Multiple regions of deletion on chromosome arm 13q in head-and-neck squamous-cell carcinoma. Int J Cancer 1999, 84:453-457 [DOI] [PubMed] [Google Scholar]
- 22.van Houten VMM, Tabor MP, van den Brekel MWM, Denkers F, Wishaupt RGA, Kummer JA, Snow GB, Brakenhoff RH: Molecular assays for the diagnosis of minimal residual head-and-neck cancer: methods, reliability, pitfalls, and solutions. Clin Cancer Res 2000, 6:803-816 [PubMed] [Google Scholar]
- 23.Cruz IB, Snijders PJ, Meijer CJ, Braakhuis BJ, Snow GB, Walboomers JM, van der Waal I: p53 expression above the basal cell layer in oral mucosa is an early event of malignant transformation and has predictive value for developing oral squamous cell carcinoma. J Pathol 1998, 184:360-368 [DOI] [PubMed] [Google Scholar]
- 24.Sidransky D, Von Eschenbach A, Tsai YC, Jones P, Summerhayes I, Marshall F, Paul M, Green P, Hamilton SR, Frost P, Vogelstein B: Identification of p53 gene mutations in bladder cancers and urine samples. Science 1991, 252:706-709 [DOI] [PubMed] [Google Scholar]
- 25.Shanmugaratnam K: Shanmugaratnam K eds. Histological Typing of Tumours of the Upper Respiratory Tract and Ear, ed 2 1993. Springer-Verlag, Berlin
- 26.Mao L, Lee JS, Fan YH, Ro JY, Batsakis JG, Lippman S, Hittelman W, Hong WK: Frequent microsatellite alterations at chromosomes 9p21 and 3p14 in oral premalignant lesions and their value in cancer risk assessment. Nat Med 1996, 2:682-685 [DOI] [PubMed] [Google Scholar]
- 27.Lydiatt WM, Anderson PE, Bazzana T, Casale M, Hughes CJ, Huvos AG, Lydiatt DD, Schantz SP: Molecular support for field cancerization in the head and neck. Cancer 1998, 82:1376-1380 [PubMed] [Google Scholar]
- 28.Rosin MP, Cheng X, Poh C, Lam WL, Huang YQ, Lovas J, Berean K, Epstein JB, Priddy R, Le ND, Zhang LW: Use of allelic loss to predict malignant risk for low-grade oral epithelial dysplasia. Clin Cancer Res 2000, 6:357-362 [PubMed] [Google Scholar]
- 29.Khuri FR, Kim ES, Lee JJ, Winn RJ, Benner SE, Lippman SM, Fu KK, Cooper JS, Vokes EE, Chamberlain RM, Williams B, Pajak TF, Goepfert H, Hong WK: The impact of smoking status, disease stage, and index tumor site on second primary tumor incidence and tumor recurrence in the head and neck retinoid chemoprevention trial. Cancer Epidemiol Biomarkers Prev 2001, 10:823-829 [PubMed] [Google Scholar]
- 30.Cloos J, Leemans CR, van der Sterre ML, Kuik DJ, Snow GB, Braakhuis BJM: Mutagen sensitivity as a biomarker for second primary tumors after head and neck squamous cell carcinoma. Cancer Epidemiol Biomarkers Prev 2000, 9:713-717 [PubMed] [Google Scholar]
- 31.Tabor MP, Braakhuis BJM, van der Wal JE, van Diest PJ, Leemans CR, Brakenhoff RH, Kummer JA: Comparative molecular and histological grading of epithelial dysplasia of the oral cavity and the oropharynx. J Pathol, in press [DOI] [PubMed]
- 32.Walker DR, Bond JP, Tarone RE, Harris CC, Makalowski W, Boguski MS, Greenblatt MS: Evolutionary conservation and somatic mutation hotspot maps of p53: correlation with p53 protein structural and functional features. Oncogene 1999, 18:211-218 [DOI] [PubMed] [Google Scholar]
- 33.Braakhuis BJM, Tabor MP, Leemans CR, van der Waal I, Snow GB, Brakenhoff RH: Second primary tumors and field cancerization in oral and oropharyngeal cancer: molecular techniques provide new insights and definitions. Head Neck 2002, 24:198-206 [DOI] [PubMed] [Google Scholar]


