Abstract
Most gastrointestinal stromal tumors (GISTs) harbor oncogenic mutations in the KIT gene, and the majority of these mutations affect the juxtamembrane domain of the kinase encoded by exon 11. Screening GISTs for KIT gene mutations is important for translational research studies and for providing prognostic information on the likelihood of tumor response to treatment with the kinase inhibitor imatinib mesylate (Gleevec). In a series of GISTs analyzed in our laboratory by a combination of denaturing HPLC and direct DNA sequencing, we identified 19 cases with KIT exon 11 deletions that included from 1 to 14 bp of intron 10 sequence and resulted in loss of the normal splice acceptor site at the beginning of exon 11. Predicted use of the next potential splice-acceptor site was confirmed by cDNA sequencing in 4 cases. Thus, the resulting mutant isoform, deletion KPMYEVQWK 550–558, was the same in all 19 cases. Only two other examples of deletions across the intron 10–exon 11 boundary have been reported, yet among 722 GISTs analyzed in our laboratories these deletions were not uncommon, accounting for 3.9% of exon 11 mutations and 2.6% of all tumors. Loss of KIT intron 10 sequences may be under-recognized if the forward primer is too close to exon 11, or if cases are examined exclusively at the cDNA level. Laboratories that offer clinical screening for KIT mutations in GI stromal tumors should be aware of this class of mutations.
Oncogenic activation of the receptor tyrosine kinase KIT plays a central role in the development of most gastrointestinal stromal tumors (GISTs). KIT expression is detectable by immunohistochemistry in approximately 95% of GISTs,1,2 and phosphorylation of the kinase is evident by immunoblotting in the great majority of tumors.3,4 A variety of mutations have been identified in KIT exons 9, 11, 13, and 17, including deletions, insertions, single nucleotide substitutions, and combinations thereof, that are invariably in-frame.2,5,6,7,8,9,10,11 The resulting mutant isoforms have constitutive kinase activity in vitro and support the development of tumors in nude mice.2,3 Several kindreds with germline KIT gene mutations have been identified in which affected individuals are at high risk for the development of multiple GISTs, providing additional evidence of an oncogenic role for KIT in these tumors.12,13,14,15,16,17 Interestingly, a minority of GISTs (5 to 7%) appear to develop through a parallel pathway involving activating mutation of the KIT-homologous receptor tyrosine kinase PDGFRA.18,19
The importance of KIT and PDGFRA in the biology of GISTs is underscored by the clinical response of many of these tumors to treatment with imatinib mesylate (Gleevec), an inhibitor that has activity against both of these kinases.20,21,22 Based on correlative studies of a recent phase II trial of imatinib for advanced GIST, there is a relationship between kinase mutation status and response to therapy.23 Patients whose tumor harbored a KIT exon 11 mutation had a higher response rate and better overall survival than those with KIT exon 9-mutant tumor and those with tumor lacking KIT or PDGFRA mutation. Similar observations have emerged from phase I and II trials conducted in Europe.24 Thus, mutation screening of GISTs is not only of research interest, but has prognostic value in evaluating tumors for which imatinib therapy may be considered. In addition, identification of KIT and PDGFRA mutations can be useful in confirming the diagnosis of GISTs that have unusual immunophenotypic features (eg, KIT-negative tumors).25,26
A number of methods have been applied in assessing GISTs for kinase gene mutations, including direct DNA sequencing, single-strand conformational polymorphism (SSCP) detection, and length analysis of PCR products (LAPP).5,6,8,11 We have found that a combination of denaturing HPLC (DHPLC) and DNA sequencing is highly sensitive for both deletion/insertion type mutations and point mutations.18,23,27 Among 722 GISTs analyzed in our laboratories by this approach, we identified 19 examples of unusual KIT exon 11 deletions that are the subject of this report.
Materials and Methods
GI Stromal Tumors
Paraffin-embedded samples of formalin-fixed GISTs were obtained from the archives of the Departments of Pathology at OHSU Hospital, the Portland VA Medical Center, Kaiser Northwest Laboratories, and the Brigham & Women’s Hospital. In accordance with Institutional Review Board (IRB) requirements at all four institutions, each sample was assigned a unique number and all information was stored in a password-protected database. In addition, samples were included from recent clinical trials in which patients were consented for research use of their tumor tissue. A total of 722 GISTs from these various sources have been analyzed in our laboratories for KIT gene mutations. Data from subsets of these cases have been previously reported.18,23,27
Preparation of Genomic DNA
Genomic DNA was extracted as previously described. Briefly, a hematoxylin and eosin (H&E)-stained section of the embedded tumor was reviewed by standard light microscopy to determine which areas were suitable for analysis (>80% tumor cells). These areas were then removed from the paraffin block or scraped from matched, unstained slides using a sterile scalpel blade. Following deparaffinization in xylenes and graded ethanols, DNA was extracted from the rehydrated tissue using the QIAamp mini kit (Qiagen, Valencia, CA).
PCR Amplification and Analysis of KIT Exon 11
Amplification of KIT gene exon 11 was performed using our previously published protocol.27 The forward primer used was CCAGAGTGCTCTAATGACTG, and the reverse primer used was ACCCAAAAAGGTGACATGGA. Amplicons were screened both for length alterations (deletions and/or insertions) and single nucleotide polymorphisms by DHPLC (WAVE system, Transgenomic, Inc., Omaha, NE), as detailed in a previous report.27 Specimens with aberrant HPLC profiles were sequenced bidirectionally using the ABI Prism Big Dye terminator kit (Applied Biosystems, Foster City, CA) and analyzed on an ABI 310 sequencer (Applied Biosystems).
Preparation and Analysis of cDNA
Formalin-fixed, paraffin-embedded samples of tumor tissue were identified, collected, and deparaffinized as described above. The tissue was rehydrated in 10 mmol/L Tris-HCl, 0.1 mmol/L EDTA, 2% EDTA and digested with 500 μg/ml proteinase K (Qiagen) at 60°C for at least 4 hours (longer if the tissue was not fully lysed). Total RNA was purified using the StrataPrep Total RNA microprep kit (Stratagene, La Jolla, CA) according to the manufacturer’s instructions. RNA (1 μg) was converted to cDNA using 1 unit of SuperScript RNase H reverse transcriptase (Gibco Biologicals, Carlsbad, CA) and 0.2 μg random primers (Gibco) in a 30-μl volume incubated at 37°C for 60 minutes. KIT cDNA sequences from exons 10 and 11 were amplified by PCR using a reverse primer (GAGTCGGACAAAGACCCTTT) matched with one of two forward primers: AAATCCATCCCCACACCC (247-bp product) or CCTTTGCTGATTGGTTTCGT (201-bp product). The PCR conditions were as follows: 1 minute at 95°C, 45 cycles of 1 minute at 94°C/1 minute at 56°C/1 minute at 72°C, and then 7 minutes at 72°C. Samples yielding proper-sized amplicons, as confirmed by DHPLC, were sequenced as described above. In one of the four cases analyzed, direct DNA sequencing yielded satisfactory results in only one direction. Therefore, the amplicon was TOPO cloned as previously described, and a subclone was sequenced bidirectionally to confirm the initial sequence result.18
Results and Discussion
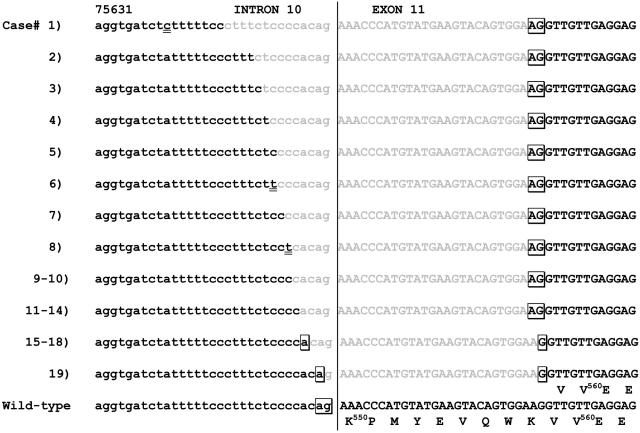
Analysis of GIST samples from 722 patients in our laboratories yielded 578 cases (80.0%) in which a mutation in exon 9, 11, 13, or 17 of the KIT gene was identified. The great majority of these mutations affected the juxtamembrane region of KIT encoded by exon 11 (67.7% of all GISTs). Among these exon 11 mutations were 19 examples in which there was a deletion that spanned the intron 10–exon 11 boundary. As illustrated in Figure 1, these deletions included from 1 to 14 bp of the 3′ end of intron 10 and resulted in loss of the splice acceptor site for exon 11. In each case, a new potential splice acceptor AG was created, based on either the last two nucleotides of codon K558 (cases 1 to 14) or juxtaposition of an intron 10 adenosine with the terminal guanine of this codon (cases 15 to 19). The deletion resulting from use of this splice acceptor was predicted as KPMYEVQWK550–558. In 14 of the 19 cases, there was a C immediately 5′ to the splice acceptor AG, consistent with the preference for a CAG sequence at the splice acceptor site. Based on DHPLC profiles, 6 of the 19 cases appeared to be hemizygous or homozygous for the detected deletion.
Figure 1.
Genomic deletions that include the intron 10–exon 11 boundary. Sequence from the end of intron 10, beginning at nucleotide 75631, and the beginning of exon 11 is shown, with the deletions of all 19 cases indicated in gray. Predicted splice acceptor sites are boxed. Wild-type sequence and amino acid codons are shown at the bottom of the figure for comparison. Note that in cases 6 and 8 the deletion was accompanied by a single nucleotide substitution at the 5′ end (underlined). A separate single nucleotide polymorphism is underlined in the intron 10 sequence of case 1.
To prove that the new splice acceptor site was, in fact, used we prepared cDNA from the paraffin-embedded tumor of four of the cases (no frozen material was available). Using two different forward primers, amplicons of either 201 or 247 bp were successfully generated from the exon 10−11 boundary. Sequencing of these amplicons confirmed loss of codons 550–558 in all four samples (Figure 2). Interestingly, the cDNA products of all four cases were uniformly mutant even though three of the cases appeared heterozygous at the genomic level. One explanation for this apparent discrepancy is that wild-type genomic DNA contributed by non-tumor cells masked hemi/homozygosity of the tumor for the mutant allele. Alternatively, there may be selective transcription of the mutant allele in tumors that are truly heterozygous. For comparison, cDNA analyses were also performed on four exon 11-mutant tumors that did not include intron 10 sequences; three of these showed heterozygous allelic expression as expected, while the fourth appeared to express only the mutant allele, despite apparent genomic heterozygosity. Thus, this phenomenon is not unique to tumors with mutations that begin in intron 10 and may be worthy of further study.
Figure 2.
cDNA sequences. The cDNA sequences from cases 1, 5, 11, and 15 all showed the identical deletion, as predicted from the genomic analyses.
Deletion of KPMYEVQWK550–558 in KIT exon 11 was one of the five mutations identified by Hirota and colleagues2 in their original report of oncogenic KIT mutations in GI stromal tumors. However, that study was based on cDNA analysis, precluding identification of a possible intronic component of the deletion. Emile and colleagues6 reported a GIST with a genomic deletion that extended 7 bp into intron 10 (identical to our case 5), and deduced that use of the next possible splice acceptor site would result in the deletion KPMYEVQWK550–558. Our results, confirmed at the cDNA level, demonstrate that this phenomenon is not uncommon. Indeed, it is possible that the KPMYEVQWK550–558 deletions reported by Taniguchi et al (two cases),11 Miettinen et al,28 and Antonescu et al,5 also included intron 10 sequences, but this issue was not addressed in these studies.
It should be noted that deletion KPMYEVQWK550–558 can also result from an in-frame deletion that begins precisely at the first coding nucleotide of exon 11 (codon 550). We have observed five such deletions in our series (data not shown). Of course, at the protein level the final mutant isoform is the same as in tumors that have deleted part of intron 10 and use the alternative splice acceptor. It is not surprising, then, that the clinicopathologic features of the intron 10-deleted tumors are not substantively different from those with more typical exon 11 deletions. All 19 tumors were positive for KIT (CD117) by immunohistochemistry and had a spindle or mixed spindle/epithelioid morphology. All of the tumors with an assigned site of origin derived from the stomach. Available information on the age (median 57 years, n = 10) and sex (male:female, 1.25:1, n = 9) of the patients does not appear to differ from other published series of GISTs (information on cases from ongoing clinical trials is not available). Sixteen of the 19 tumors were malignant, but this very likely reflects the bias of our series for clinical trial patients. On the other hand, three tumors were classified as very low-risk by the criteria of Fletcher et al,1 so deletions crossing into intron 10 are not necessarily inherently aggressive. Most significantly, among six patients treated with imatinib for advanced disease, five had a partial remission and one had disease stabilization. These results are entirely consistent with the responses of exon 11-mutant GISTs in general.23,24
To our knowledge, the only other documented example of a genomic deletion across the KIT intron 10–exon 11 boundary was described by Lee et al.9 Case 4 in their report was interpreted as a deletion/substitution KPMYEV550–555I, but it appears from the published sequence that loss of the splice acceptor site was not appreciated. It is likely that the AG of codon Q556 served as an alternative splice acceptor in that tumor, such that the resulting deletion was KPMYEVQ550–556. Interestingly, a KPMYEV550–555I deletion/substitution was also listed in the original report by Hirota and colleagues.2 In that case, the isoleucine substitution was documented at the cDNA level and, therefore, the underlying genomic mutation must have differed from case 4 of Lee et al.9 Another example of a KPMYEV550–555I deletion/substitution was reported by Taniguchi et al,11 but their report did not include the supporting sequence and it is unclear whether intronic sequences were part of that deletion, Our series has yielded two cases with the deletion/substitution KPMYEV550–555I and one case with deletion KPMYEVQ550–556, but none of these included intron 10 sequences.
The juxtamembrane (JM) domain of KIT exerts an autoinhibitory effect on kinase activity through interaction with the N-terminal kinase domain.29,30 Length alterations or point substitutions in the JM domain disrupt this interaction and result in kinase activation. As autoinhibition of kinase activity by the JM domain is a property of other members of the receptor tyrosine kinase family, it is possible that length-altering mutations that involve the intron/exon boundary of JM domains will be found in other kinase genes. PDGFRA is of particular interest in this regard. Many of the reported intra-chromosomal deletions that lead to fusion of the FIP1L1 and PDGFRA genes in patients with hypereosinophilic syndrome result in loss of the splice acceptor site for exon 12, which encodes the PDGFRA JM domain.31 An alternate AG splice acceptor within the sequence of exon 12 serves to maintain the reading frame in these cases.
In summary, our findings and other published reports indicate that deletions across the intron 10–exon 11 boundary of KIT can result in two mutant isoforms, deletion KPMYEVQ550–556 and deletion KPMYEVQWK550–558. Of these two isoforms, the latter is not uncommon, accounting for 3.9% of all exon 11 mutations in our series. The choice of the forward primer for exon 11 amplification is important in the identification of these partially intronic deletions. Indeed, it remains possible that even larger deletions would be found if other primers were used. It is also conceivable that mutations involving the splice donor site at the exon 10–intron 10 boundary could affect the JM domain of KIT, although we have not yet observed any in separate analyses of exon 10 (data not shown). Laboratories engaged in mutation screening of GISTs for research or clinical purposes should be aware of the existence of deletions involving the intron 10–exon 11 boundary, because identification of exon 11-mutant GISTs has prognostic significance in regard to imatinib response.
Footnotes
Supported in part by a Merit Review Research Grant from the Department of Veterans Affairs (M.C.H).
References
- Fletcher C, Berman J, Corless C, Gorstein F, Lasota J, Longley J, Miettinen M, O’Leary T, Remotti HE, Rubin BP, Shmookler BM, Sobin L, Weiss SW. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002;33:459–465. doi: 10.1053/hupa.2002.123545. [DOI] [PubMed] [Google Scholar]
- Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M, Muhammad Tunio G, Matsuzawa Y, Kanakura Y, Shinomura Y, Kitamura Y. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–580. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- Heinrich MC, Rubin BP, Longley BJ, Fletcher JA. Biology and genetic aspects of gastrointestinal stromal tumors: kIT activation and cytogenetic alterations. Hum Pathol. 2002;33:484–495. doi: 10.1053/hupa.2002.124124. [DOI] [PubMed] [Google Scholar]
- Rubin BP, Singer S, Tsao C, Duensing A, Lux ML, Ruiz R, Hibbard MK, Chen CJ, Xiao S, Tuveson DA, Demetri GD, Fletcher CDM, Fletcher JA. KIT activation is a ubiquitous feature of gastrointestinal stromal tumors. Cancer Res. 2001;61:8118–8121. [PubMed] [Google Scholar]
- Antonescu CR, Sommer G, Sarran L, Tschernyavsky SJ, Riedel E, Woodruff JM, Robson M, Maki R, Brennan MF, Ladanyi M, DeMatteo RP, Besmer P. Association of KIT exon 9 mutations with nongastric primary site and aggressive behavior: KIT mutation analysis and clinical correlates of 120 gastrointestinal stromal tumors. Clin Cancer Res. 2003;9:3329–3337. [PubMed] [Google Scholar]
- Emile JF, Lemoine A, Bienfait N, Terrier P, Azoulay D, Debuire B. Length analysis of polymerase chain reaction products: a sensitive and reliable technique for the detection of mutations in KIT exon 11 in gastrointestinal stromal tumors. Diagn Mol Pathol. 2002;11:107–112. doi: 10.1097/00019606-200206000-00007. [DOI] [PubMed] [Google Scholar]
- Hirota S, Nishida T, Isozaki K, Taniguchi M, Nakamura J, Okazaki T, Kitamura Y. Gain-of-function mutation at the extracellular domain of KIT in gastrointestinal stromal tumours. J Pathol. 2001;193:505–510. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH818>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Lasota J, Wozniak A, Sarlomo-Rikala M, Rys J, Kordek R, Nassar A, Sobin LH, Miettinen M. Mutations in exons 9 and 13 of KIT gene are rare events in gastrointestinal stromal tumors: a study of 200 cases. Am J Pathol. 2000;157:1091–1095. doi: 10.1016/S0002-9440(10)64623-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JR, Joshi V, Griffin JW, Jr, Lasota J, Miettinen M. Gastrointestinal autonomic nerve tumor: immunohistochemical and molecular identity with gastrointestinal stromal tumor. Am J Surg Pathol. 2001;25:979–987. doi: 10.1097/00000478-200108000-00001. [DOI] [PubMed] [Google Scholar]
- Lux ML, Rubin BP, Biase TL, Chen CJ, Maclure T, Demetri G, Xiao S, Singer S, Fletcher CDM, Fletcher JA. KIT extracellular and kinase domain mutations in gastrointestinal stromal tumors. Am J Pathol. 2000;156:791–795. doi: 10.1016/S0002-9440(10)64946-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taniguchi M, Nishida T, Hirota S, Isozaki K, Ito T, Nomura T, Matsuda H, Kitamura Y. Effect of c-kit mutation on prognosis of gastrointestinal stromal tumors. Cancer Res. 1999;59:4297–4300. [PubMed] [Google Scholar]
- Beghini A, Tibiletti MG, Roversi G, Chiaravalli AM, Serio G, Capella C, Larizza L. Germline mutation in the juxtamembrane domain of the kit gene in a family with gastrointestinal stromal tumors and urticaria pigmentosa. Cancer. 2001;92:657–662. doi: 10.1002/1097-0142(20010801)92:3<657::aid-cncr1367>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Hirota S, Okazaki T, Kitamura Y, O’Brien P, Kapusta L, Dardick I. Cause of familial and multiple gastrointestinal autonomic nerve tumors with hyperplasia of interstitial cells of Cajal is germline mutation of the c-kit gene. Am J Surg Pathol. 2000;24:326–327. doi: 10.1097/00000478-200002000-00045. [DOI] [PubMed] [Google Scholar]
- Hirota S, Nishida T, Isozaki K, Taniguchi M, Nishikawa K, Ohashi A, Takabayashi A, Obayashi T, Okuno T, Kinoshita K, Chen H, Shinomura Y, Kitamura Y. Familial gastrointestinal stromal tumors associated with dysphagia and novel type germline mutation of KIT gene. Gastroenterology. 2002;122:1493–1499. doi: 10.1053/gast.2002.33024. [DOI] [PubMed] [Google Scholar]
- Isozaki K, Terris B, Belghiti J, Schiffman S, Hirota S, Vanderwinden J-M. Germline-activating mutation in the kinase domain of KIT gene in familial gastrointestinal stromal tumors. Am J Pathol. 2000;157:1581–1585. doi: 10.1016/S0002-9440(10)64795-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeyama H, Hidaka E, Ota H, Minami S, Kajiyama M, Kuraishi A, Mori H, Matsuda Y, Wada S, Sodeyama H, Nakata S, Kawamura N, Hata S, Watanabe M, Iijima Y, Katsuyama T. Familial gastrointestinal stromal tumor with hyperpigmentation: association with a germline mutation of the c-kit gene. Gastroenterology. 2001;120:210–215. doi: 10.1053/gast.2001.20880. [DOI] [PubMed] [Google Scholar]
- Nishida T, Hirota S, Taniguchi M, Hashimoto K, Isozaki K, Nakamura H, Kanakura Y, Tanaka T, Takabayashi A, Matsuda H, Kitamura Y. Familial gastrointestinal stromal tumours with germline mutation of the KIT gene. Nat Genet. 1998;19:323–324. doi: 10.1038/1209. [DOI] [PubMed] [Google Scholar]
- Heinrich MC, Corless CL, Duensing A, McGreevey L, Chen CJ, Joseph N, Singer S, Griffith DJ, Haley A, Town A, Demetri GD, Fletcher CD, Fletcher JA. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299:708–710. doi: 10.1126/science.1079666. [DOI] [PubMed] [Google Scholar]
- Hirota S, Ohashi A, Nishida T, Isozaki K, Kinoshita K, Shinomura Y, Kitamura Y. Gain-of-function mutations of platelet-derived growth factor receptor alpha gene in gastrointestinal stromal tumors. Gastroenterology. 2003;125:660–667. doi: 10.1016/s0016-5085(03)01046-1. [DOI] [PubMed] [Google Scholar]
- Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S, Janicek M, Fletcher JA, Silverman SG, Silberman SL, Capdeville R, Kiese B, Peng B, Dimitrijevic S, Druker BJ, Corless C, Fletcher CD, Joensuu H. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347:472–480. doi: 10.1056/NEJMoa020461. [DOI] [PubMed] [Google Scholar]
- Joensuu H, Roberts PJ, Sarlomo-Rikala M, Andersson LC, Tervahartiala P, Tuveson D, Silberman SL, Capdeville R, Dimitrijevic S, Druker BJ, Demetri GD. Effect of the tyrosine kinase inhibitor STI571 in a patient with a metastatic gastrointestinal stromal tumor. N Engl J Med. 2001;1052:1052–1056. doi: 10.1056/NEJM200104053441404. [DOI] [PubMed] [Google Scholar]
- Van Oosterom AT, Judson I, Verweij J, Stroobants S, Donato DP, Dimitrijevic S, Martens M, Webb A, Sciot R, van Glabbeke M, Silberman S, Nielsen OS. Safety and efficacy of imatinib (STI571) in metastatic gastrointestinal stromal tumours: a phase I study. Lancet. 2001;358:1421–1423. doi: 10.1016/s0140-6736(01)06535-7. [DOI] [PubMed] [Google Scholar]
- Heinrich MC, Corless CL, Demetri GD, Blanke CD, von Mehren M, Joensuu H, McGreevey LS, Chen CJ, Van den Abbeele AD, Druker BJ, Kiese B, Eisenberg B, Roberts PJ, Singer S, Fletcher CD, Silberman S, Dimitrijevic S, Fletcher JA. Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol. 2003;21:4342–4349. doi: 10.1200/JCO.2003.04.190. [DOI] [PubMed] [Google Scholar]
- Debiec-Rychter M, Dumez H, Judson I, Wasag B, Verweij J, Brown M, Dimitrijevic S, Sciot R, Stul M, Vranck H, Scurr M, Hagemeijer A, van Glabbeke M, Van Oosterom AT. Use of c-KIT/PDGFRA mutational analysis to predict the clinical response to imatinib in patients with advanced gastrointestinal stromal tumours entered on phase I and II studies of the EORTC Soft Tissue and Bone Sarcoma Group. Eur J Cancer. 2004;40:689–695. doi: 10.1016/j.ejca.2003.11.025. [DOI] [PubMed] [Google Scholar]
- Debiec-Rychter M, Wasag B, Stul M, De Wever I, Van Oosterom A, Hagemeijer A, Sciot R. Gastrointestinal stromal tumours (GISTs) negative for KIT (CD117 antigen) immunoreactivity. J Pathol. 2004;202:430–438. doi: 10.1002/path.1546. [DOI] [PubMed] [Google Scholar]
- Medeiros F, Corless CL, Duensing A, Hornick JL, Oliveira AM, Heinrich MC, Fletcher JA, Fletcher CDM. KIT-negative gastrointestinal stromal tumors: proof of concept and therapeutic implications. Am J Surg Pathol. 2004;28:889–894. doi: 10.1097/00000478-200407000-00007. [DOI] [PubMed] [Google Scholar]
- Corless CL, McGreevey L, Haley A, Town A, Heinrich MC. KIT mutations are common in incidental gastrointestinal stromal tumors one centimeter or less in size. Am J Pathol. 2002;160:1567–1572. doi: 10.1016/S0002-9440(10)61103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miettinen M, Sarlomo-Rikala M, Sobin LH, Lasota J. Esophageal stromal tumors: a clinicopathologic, immunohistochemical, and molecular genetic study of 17 cases and comparison with esophageal leiomyomas and leiomyosarcomas. Am J Surg Pathol. 2000;24:211–222. doi: 10.1097/00000478-200002000-00007. [DOI] [PubMed] [Google Scholar]
- Chan PM, Ilangumaran S, La Rose J, Chakrabartty A, Rottapel R. Autoinhibition of the Kit receptor tyrosine kinase by the cytosolic juxtamembrane region. Mol Cell Biol. 2003;23:3067–3078. doi: 10.1128/MCB.23.9.3067-3078.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y, Cunningham ME, Wang X, Ghosh I, Regan L, Longley BJ. Inhibition of spontaneous receptor phosphorylation by residues in a putative alpha-helix in the KIT intracellular juxtamembrane region. J Biol Chem. 1999;274:13399–13402. doi: 10.1074/jbc.274.19.13399. [DOI] [PubMed] [Google Scholar]
- Cools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J, Kutok J, Clark J, Galinsky I, Griffin JD, Cross NC, Tefferi A, Malone J, Alam R, Schrier SL, Schmid J, Rose M, Vandenberghe P, Verhoef G, Boogaerts M, Wlodarska I, Kantarjian H, Marynen P, Coutre SE, Stone R, Gilliland DG. A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med. 2003;348:1201–1214. doi: 10.1056/NEJMoa025217. [DOI] [PubMed] [Google Scholar]