Abstract
Daniel K Sokol argues that on rare occasions benignly deceiving patients can be morally acceptable, and he has devised a decision checklist to help doctors facing such a dilemma
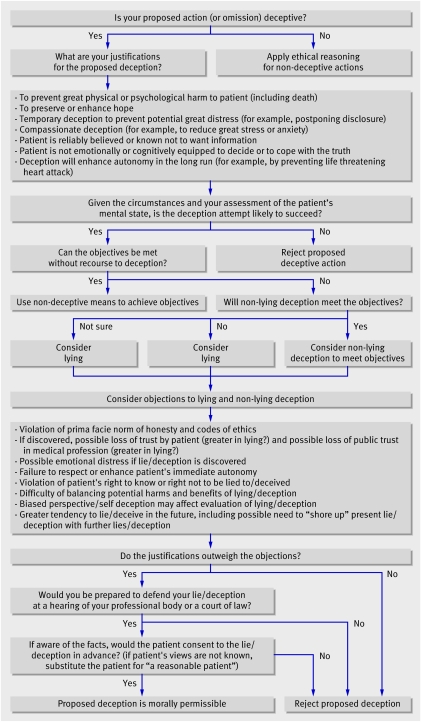
Nearly all doctors, at some time, will question the wisdom of telling a grim truth to a patient. To help doctors resolve such dilemmas, I have developed a “deception flowchart.” By providing a sequence of questions and a checklist of relevant moral considerations, the flowchart might help the ethically sensitive doctor make a more informed decision about when to over-ride the duty to be honest. It might also be useful to teachers of medical ethics, who can use it to illustrate the complexity of this puzzling area of medicine.
The ongoing deception debate
It is a truth universally acknowledged that ethical doctors will not intentionally deceive their patients. The American Medical Association states: “A physician shall . . . be honest in all professional interactions, and strive to report physicians . . . engaging in fraud or deception, to appropriate entities.”1
Similar injunctions are offered by the World Medical Association and the United Kingdom's General Medical Council.2 3 The situation at the bedside may well be different, however.4 5 6 7 8 When it comes to disclosing a grim prognosis, doctors may control information by using euphemisms, ambiguities, evasions, and other strategies.5 7 9 In some countries, doctors commonly withhold an adverse diagnosis and prognosis from patients.10 11
I have argued elsewhere that benignly intended deception by doctors may, in some cases, be morally acceptable.9 12 Although deception in medicine is generally wrong, as it tends to undermine patients' autonomy and erode the trust between doctor and patient, the ethical duty to be honest is not absolute. Some moral goods, such as the avoidance of severe physical or emotional suffering and the preservation of life or long term autonomy, may over-ride the prima facie duty not to deceive. When a distressed mother asks if her beloved daughter suffered in her dying moments, or when on the operating table a patient with a ruptured abdominal aneurysm asks the unhopeful anaesthetist whether he will be all right (see box), the usually strict need for honesty gives way to compassion and humanity. I acknowledge, however, that many readers will believe that doctors' truthfulness, as a cornerstone of trust and respect, is an absolute requirement that allows for no exceptions.
Case study: the unhopeful anaesthetist
A patient with a ruptured aortic aneurysm is rushed to the operating theatre. The anaesthetist knows the patient's chances of survival are poor. Just as preoxygenation is about to begin, the distressed patient asks “I am going to be all right, aren't I, doctor?” Can the unhopeful anaesthetist justifiably deceive the patient?
Brief flowchart analysis
The strongest reasons for deception here are to prevent great psychological harm and compassionate (humane) deception. As the patient will be conscious for only a short time, the deception is likely to succeed. A truthful alternative needs quick thinking and careful phrasing and therefore runs a higher risk of distressing the patient. As non-lying forms of deception (such as the evasive “we'll do our very best”) might arouse suspicion, and as the likelihood of eventual discovery is minimal, lying is preferable for reducing such harm.
The main objections to deception are violation of the duty to be truthful, respect for patient autonomy, and the “right to know.” Given the anticipated intensity of the distress, however short lived; the lack of realistic alternative clinical options; the negative impact of delay on an already poor prognosis; and the improbability in the remaining seconds of the patient coming to terms with the grim truth, the balance might justifiably be judged to fall on the side of deception. In light of the reasoning above, I would be willing to justify my decision to colleagues and the General Medical Council and believe many reasonable people might want to be deceived in such circumstances. I conclude that the proposed deception is morally acceptable.
The deception flowchart
The deception flowchart (figure) can help doctors who are non-absolutist decide when deception is appropriate. The flowchart combines a series of questions with a list of justifications and objections to deception. Additional principles act as moral “safety checks.”
Deception flowchart
SUMMARY POINTS
Although deceiving patients is generally wrong, benignly intended deception may be morally acceptable in certain circumstances
No detailed guidance is available on when clinicians' deception is morally acceptable
The proposed deception flowchart might help clinicians make better informed decisions regarding deception
The deception flowchart might be useful when teaching medical students and clinicians
Navigating the flowchart
People define deception in different ways. For some doctors, withholding dismal facts about a terminal prognosis is not deception but being “economical with the truth” to maintain a patient's morale. Others will disagree and call this omission or optimistic disclosure deceptive. As the term deception is laden with negative value, people's attitudes towards a proposed action (or omission) may influence their evaluation of that act as deception. Thus, the answer to the first question “Is your proposed action deceptive?” should be answered “yes” even if the doctor doubts that the act constitutes deception.13 This uncharitable approach should reduce the distorting influence of bias.
The second question requires the doctor to justify the deception and lists possible reasons derived from both a comprehensive review of the philosophical and medical literature and qualitative interviews and surveys with patients, doctors, and members of the public in the UK.9 These reasons include the prevention of great physical or psychological harm (including death), the exercise of kindness or compassion, the emotional or cognitive incapacity of the patient, and the reliable belief that the patient wishes to be deceived.
Once the justifications have been clarified, the next questions examine practical issues. Like any medical procedure, deception can be used inappropriately. It may be too ambitious, risky, or simply ineffective. Doctors must ask themselves: am I satisfied with my assessment of the patient? Is the act likely to deceive the patient? If it does succeed, will it achieve the intended aims?
If the answers to these questions are “yes” (or “probably”), the next step is to consider alternatives to deception. Is there an alternative that does not involve deception? If deception is necessary, can lying be avoided in favour of less direct forms of deception, such as using ambiguous or obscure language or evading the question? Although philosophers disagree over whether lying is always morally worse than other forms of deception, many people consider lying to be worse, so non-lying deception is preferable if both types are equally effective.14 15 16 17 If the deception is discovered, a lie may cause greater damage to the doctor-patient relationship than a non-lying deception.
The next step is to identify possible objections to deception. These include violation of the patient's autonomy (as an autonomous decision needs accurate and adequate information), the risk of damaging trust in the relationship and in the medical profession as a whole, the risk of self deception, and an increased probability of deceiving again in the future.
Once the objections have been identified, the reasons for and against deception need to be balanced. No algorithm exists to help doctors in this task. They will have to exercise careful judgment to establish the relative moral weight of those reasons.
Moral safety checks
Two safety checks remain to ensure the permissibility of the proposed deception. The first is for the doctor to consider how he or she would articulate and defend their views and reasoning before a body of reasonable people, such as a professional association or a court of law.18 19 The purpose of this test is to encourage doctors to reassess the strengths and weaknesses of their justifications, to reduce the risk of personal bias and self deception in their judgments,20 21 and to remind them that deceiving patients is no trivial matter.
The final test requires the doctor to consider whether the patient, if aware of all the facts, would probably have consented to the deception (“yes, if that situation arises, please deceive me”). Confidentiality permitting, it might be best to seek the views of the patient's relatives to obtain a clearer idea of the patient's probable preferences. If the answer to this final question is “yes” the proposed deception is morally permissible and possibly even morally required.
The flowchart presents a demanding set of criteria for doctors who contemplate deception. Only a small proportion of proposed deceptions will be morally permissible. This is to be expected. Deception, as a violation of a doctor's duty to be honest to patients, is rarely justified. The demanding nature of the flowchart reflects the stringency of the duty not to deceive.
Value of the flowchart
The flowchart does not obviate the need for judgment. Doctors who use it will need, initially, to decide whether the proposed action constitutes deception. In answer to the question, “given the circumstances and your assessment of the patient's mental state, is the deception attempt likely to succeed?” they should determine at what level of certainty they can justifiably move on to the next stage of the chart. If the patient's mental state is in doubt, the doctor may request a formal psychological assessment. Later, the doctor will need to balance the likely harms and benefits of deception. The moral weight of these harms and benefits cannot be specified in advance, but will depend on the specific situation, including the social and cultural background. Answers to many of the questions will rarely be a clear cut yes or no. The decision to follow a particular branch will usually be the result of a balance of probabilities.
Sources and selection criteria
The flowchart was derived from a comprehensive review of the philosophical and medical literature and qualitative interviews and surveys with patients, doctors, and members of the public in the United Kingdom
Because of its multiple phases, the flowchart may be of limited use to the doctor faced with an immediate decision. The flowchart may be more useful for retrospective analysis—even shortly after a deceptive response has been given—and for doctors who are contemplating deceiving a patient in the future. Finally, it might be useful in teaching to analyse real or hypothetical cases of benignly intended deception and when discussing themes such as honesty, trust, the doctor-patient relationship, and the role of the doctor in the 21st century.
Thanks to Raanan Gillon, who suggested the idea of a flowchart; Azeem Majeed, Helen Morant, Søren Holm, John Saunders, Paul Booton, Andrew Hartle, and Andrew Macleod for their insightful comments on earlier drafts.
Contributors: DKS conducted his PhD on the ethics of truth telling and deception in the doctor-patient relationship and has published widely on clinical ethics. The idea for this article arose from discussions with his PhD supervisor, Raanan Gillon. DKS is the director of the UK's first professional course in applied clinical ethics. He is guarantor of the study.
Funding: Funded by the Wellcome Trust.
Competing interests: None declared.
Provenance and peer review: Not commissioned; peer reviewed.
References
- 1.American Medical Association. Principles of medical ethics. 2001. www.ama-assn.org/ama/pub/category/2512.html.
- 2.General Medical Council. Duties of a doctor registered with the GMC www.gmc-uk.org/guidance/archive/library/duties_of_a_doctor.asp. [PubMed]
- 3.World Medical Association. International code of medical ethics 1983. www.wma.net/e/policy/c8.htm.
- 4.Hagerty R, Butow P, Ellis P, Dimitry S, Tattersall M. Communicating prognosis in cancer care: a systematic review of the literature. Ann Oncol 2005;16:1005-53. [DOI] [PubMed] [Google Scholar]
- 5.Miyaji N. The power of compassion: truth-telling among American doctors in the care of dying patients. Social Sci Med 1993;36:249-94. [DOI] [PubMed] [Google Scholar]
- 6.Brewin T. Telling the truth. Lancet 1994;343:1512. [DOI] [PubMed] [Google Scholar]
- 7.Christakis N. Death foretold; prophecy and prognosis in medical care Chicago: University of Chicago Press, 2001
- 8.Burton M, Parker R. Psychological aspects of cancer surgery: surgeons' attitudes and opinions. Psychooncology 1997;6:47-64. [DOI] [PubMed] [Google Scholar]
- 9.Sokol D. Truth-telling and benignly intended deception in contemporary medicine: an empirical and philosophical analysis [PhD dissertation]. London: Imperial College, 2006
- 10.Seo M, Tamura K, Morioka E, Ikegame C, Hirasako K. Telling the diagnosis to cancer patients in Japan: attitude and perception of patients, physicians and nurses. Palliat Med 2000;14:105-10. [DOI] [PubMed] [Google Scholar]
- 11.Hamadeh G, Adib S. Cancer truth disclosure by Lebanese doctors. Social Sci Med 1998;47:1289-94. [DOI] [PubMed] [Google Scholar]
- 12.Sokol D. Truth-telling in the doctor-patient relationship: a case analysis. Clin Ethics 2006;1:130-4. [Google Scholar]
- 13.Sokol D. Dissecting deception. Cambridge Quarterly of Healthcare Ethics 2006;15:457-64. [PubMed] [Google Scholar]
- 14.Bakhurst D. On lying and deceiving. J Med Ethics 1992;18:63-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson J. On the morality of deception—does method matter? A reply to David Bakhurst. J Med Ethics 1993;19:183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gillon R. Is there an important moral distinction for medical ethics between lying and other forms of deception? J Med Ethics 1993;19:131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benn P. Medicine, lies and deception. J Med Ethics 2001;27:130-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bok S. Lying: moral choice in public and private life New York: Pantheon House, 1978
- 19.Gert B. Morality; its nature and justification New York: Oxford University Press, 1998
- 20.Redelmeier D. The cognitive psychology of missed diagnoses. Ann Intern Med 2005;142:115-20. [DOI] [PubMed] [Google Scholar]
- 21.Giannetti E. Lies we live by; the art of self-deception London: Bloomsbury, 2000