Abstract
Objective To determine whether low dose aspirin protects women aged 65 or more against cognitive decline.
Design Cohort study within both arms of the women's health study, a randomised, double blind, placebo controlled trial of low dose aspirin for the primary prevention of cardiovascular disease and cancer, 1992-5.
Setting Women's health study, 1998-2004.
Participants 6377 women aged 65 or more.
Interventions Low dose aspirin (100 mg on alternate days) or placebo for a mean of 9.6 years.
Main outcome measures Women had three cognitive assessments at two year intervals by telephone. The battery to assess cognition included five tests measuring general cognition, verbal memory, and category fluency. The primary prespecified outcome was a global score, averaging performance across all tests. The key secondary outcome was a verbal memory score, averaging performance on four measures of verbal memory.
Results At the initial assessment (mean 5.6 years after randomisation) cognitive performance in the aspirin group was similar to that of the placebo group (mean difference in global score −0.01, 95% confidence interval −0.04 to 0.02). Mean decline in the global score from the first to the final cognitive assessment was also similar in the aspirin compared with placebo groups (mean difference 0.01, −0.02 to 0.04). The risk of substantial decline (in the worst 10th centile of decline) was also comparable between the groups (relative risk 0.92, 0.77 to 1.10). Findings were similar for verbal memory; however, a 20% lower risk was observed for decline in category fluency with aspirin (relative risk 0.80, 0.67 to 0.97).
Conclusion Long term use of low dose aspirin does not provide overall benefits for cognition among generally healthy women aged 65 or more.
Introduction
Identifying ways to reduce the incidence of dementia is a public health priority. Because preventive measures may be most effective in the earliest stage of the disease, increasing research has focused on reducing the risk of early cognitive decline—a strong predictor of dementia.1 2
Aspirin and other anti-inflammatory drugs have been investigated in previous studies, with mixed findings. Randomised trials3 4 5 6 7 have generally found no cognitive benefits of these drugs for patients with Alzheimer's disease, although the trials were of short duration (<2 years) and the disease may have been too advanced to allow detection of benefits. Observational studies of cognitive function among healthy participants have been inconsistent and may be subject to biases from various sources. A recent meta-analysis8 of four cohort studies reported no relation between use of non-steroidal anti-inflammatory drugs and cognitive decline (summary relative risk 1.23, 95% confidence interval 0.70 to 2.31); thus, existing data on the relation between these drugs and dementia are inconclusive.
Another limitation of previous observational studies is that numerous anti-inflammatory agents and drug doses are often combined in analyses. Several anti-inflammatory drugs have been recently implicated in the development of cardiovascular disease9 and thus are unlikely to be viable candidates for neuroprotection. Low dose aspirin, however, has been shown to provide vascular benefits, particularly in those aged 65 or more.10 11
We tested the effect of long term use of low dose aspirin on overall cognitive decline over four years among a subset of 6377 women aged 65 or more participating in the women's health study.11
Methods
The women's health study was a randomised, double blind, placebo controlled 2×2 factorial trial of low dose aspirin (100 mg on alternate days; Bayer HealthCare) and vitamin E supplementation (600 IU on alternate days; Natural Source Vitamin E Association) in the prevention of cardiovascular disease and cancer among US women. Most participants are white (>95%). The study design has been described previously.12 Briefly, women were eligible if they were aged 45 or more; had no history of coronary heart disease, cerebrovascular disease, cancer (except for non-melanoma skin cancer), or other major chronic illnesses; and did not actively use or have a history of side effects from the study drugs.
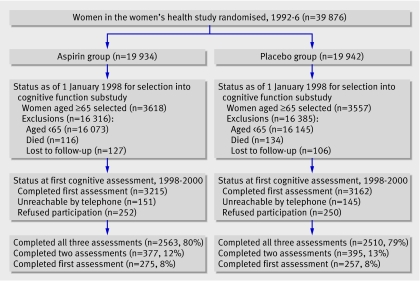
To identify women who were likely to be highly compliant, we enrolled eligible women in a three month run-in period of placebo administration. A total of 39 876 compliant women were randomised (19 934 to aspirin and 19 942 to placebo) from 1992 to 1995. Randomised assignments were computer generated in blocks of 16 within five year age strata by study programmers, masked to study investigators and enrolling staff. Participants provided written informed consent.
Every 12 months, based on their random assignments, participants were posted a year's supply of monthly calendar packs with identical white pills containing aspirin or placebo. Women were asked to complete annual postal questionnaires to update information on compliance, side effects, health and lifestyle characteristics, and the occurrence of clinical end points. They were instructed not to use vitamin E supplements and any prescribed or over the counter aspirin or aspirin containing drugs or any other non-steroidal anti-inflammatory drugs during the trial. The trial continued through to the scheduled end (31 March 2004), when overall follow-up on mortality exceeded 99%; the main results of the trial have been published and showed a benefit of aspirin in reducing the risk of stroke but no benefit in reducing the risk of myocardial infarction11 or cancer.13 Details of side effects are described elsewhere;11 briefly, the aspirin group had excesses of self reported gastrointestinal bleeding, peptic ulcer, haematuria, easy bruising, and epistaxis.
Cognitive cohort
Although the original purpose of the trial was to evaluate cardiovascular and cancer outcomes, this large scale, long term trial provided an opportunity to incorporate cognitive outcomes to study the potential effect of aspirin on delaying cognitive decline. In 1998 we started a study of cognitive function among women aged 65 or more. Eligible women were aged 65 or more and were still active participants of the women's health study (n=7175). Most of the ineligibility (98.5%) was due to the age restriction in the cognitive study protocol; only 1.5% of deaths or losses to follow-up had occurred by the start of the cognitive study, and these women were distributed equally between the aspirin and placebo groups (figure).
Flow chart of participation in cognitive cohort of women's health study
Of the 7175 women selected for the substudy of cognitive function, 296 (4.1%) were unreachable by telephone and 502 (6.9%) did not participate; thus 6377 (88.9%) women completed the initial cognitive assessment by telephone (figure). The initial assessments were carried out an average of 5.6 years after randomisation. The participation rates in the initial interview were virtually identical in the two groups. In addition, no significant differences were found in important baseline characteristics by treatment assignment.
After the initial cognitive assessment, participants underwent two follow-up assessments, at about two year intervals. High follow-up was maintained (figure): 5845 (91.7%) of those who completed the initial assessment also completed at least one follow-up assessment, and 5073 women (79.5%) completed all cognitive assessments. Among the 8% of participants who did not complete any follow-up assessments, 2% died, 1% was unreachable, and 5% refused. Follow-up rates were nearly identical in the two groups.
Although the sample size of the women's health study was not designed for the cognitive outcome, the 6377 women in this substudy provided sufficient power to detect modest differences in cognitive decline between the aspirin and placebo groups (3215 receiving aspirin and 3162 receiving placebo). For example, for the categorical outcome of substantial cognitive decline we had at least 80% power to detect a modest relative risk of 0.76 in the aspirin group compared with the placebo group; moreover, power was considerably greater for continuous analyses of mean cognitive decline in the two groups.
We have previously published results of the vitamin E treatment14; we found no relation between vitamin E and cognitive function.
Cognitive function assessment
The telephone cognitive battery was administered by trained nurses masked to participants' treatment group. The assessment included five tests measuring general cognition, verbal memory, and category fluency. To assess general cognition we administered the telephone interview of cognitive status,15 an adaptation of the mini-mental state examination for use by telephone. To test verbal memory we administered the immediate and delayed recalls of the east Boston memory test,16 in which a short paragraph is read and 12 key elements must be repeated immediately and again at 15 minutes. To further evaluate delayed verbal memory we administered a delayed recall of the telephone interview of cognitive status 10 word list. Finally, to assess category fluency,17 women were asked to name as many animals as possible in one minute.
Our primary, prespecified outcome was a global composite score averaging performance across all five cognitive tests, using z scores. Because verbal memory is among the strongest predictors of eventual risk of Alzheimer's disease,1 our key, secondary outcome was a composite score of verbal memory, averaging performance on four tests (the immediate and delayed recalls of both the east Boston memory test and the 10 word list).
In a test-retest study of the telephone interview of cognitive status among 35 high functioning, educated older women, we found a correlation of 0.7 (P<0.001) between two assessments administered 31 days apart. In a validation study of our telephone instrument, among 61 high functioning, educated older women, the correlation was 0.81 comparing overall performance on our telephone administered interview and overall performance on an extensive in-person interview, showing high validity. Cognitive impairment determined from our telephone assessment strongly predicted later dementia in educated women; among 88 older women followed over three years, lower scores on both the telephone interview of cognitive status and verbal memory were associated with significant eightfold and 12-fold increased risks of dementia.
Statistical analysis
We first examined mean performance at each cognitive assessment using repeated measures analysis of means (which permits examination of each time point, taking into account correlation between assessments). Secondly, we examined mean change in cognitive function over the three cognitive assessments. We treated scores and change in scores at each assessment as repeated continuous outcomes and we modelled the treatment effect by a time by treatment interaction. Because the trends for test scores over time were non-linear, in all analyses we used general linear models of response profiles, modelling time nominally rather than linearly.18 This approach imposes minimal structure on outcome trends and permits valid estimation of effects in non-linear data. We fitted all models by maximum likelihood, incorporating the longitudinal correlation within participants, using unstructured covariance structures; for statistical testing, we used Wald tests.18 All linear models were fitted using Proc Mixed in SAS (version 9).
In secondary analyses we examined effect modification by key risk factors for cognitive decline (most measured at baseline): age, baseline score, perceived change in memory, education, cigarette smoking, alcohol consumption, body mass index, physical activity, hormone replacement therapy use, history of diabetes, hypertension, hyperlipidaemia, depression (at four years after randomisation), and cardiovascular disease (all incident occurrences from randomisation to the end of the study). Cardiovascular disease included all medical record confirmed non-fatal myocardial infarction, non-fatal stroke, cardiovascular related deaths, or vascular disease as evidenced by either a coronary artery bypass graft or percutaneous transluminal coronary angioplasty or stenting.11 We carried out all tests of effect modification by evaluating the interaction terms in the models of mean change.
To assess the effect of aspirin treatment on the risk of “substantial cognitive decline,” we used logistic regression models in which substantial cognitive decline was defined as the worst 10% of the distribution of decline from the initial to the final cognitive assessment of the whole cohort. In all models we adjusted for the time between the first and third assessments.
Results
Characteristics at randomisation were similar among women assigned to aspirin and those assigned to placebo (table 1). At the first cognitive assessment the average duration of aspirin or placebo treatment was 5.6 years (range 4.4-6.8) and the mean time between the first and the last assessment was 4.0 years (range 2.6-5.7); thus the average total follow-up from randomisation to final evaluation was 9.6 years (range 8.2-11.3). Compliance was identical between the groups: at the final assessment, 70.0% of women in both treatment groups reported taking at least two thirds of the assigned pills.
Table 1.
Characteristics of participants in women's health study cognitive cohort at randomisation. Values are numbers (percentages) unless stated otherwise
| Characteristics | Aspirin group (n=3215) | Placebo group (n=3162) | P value |
|---|---|---|---|
| Mean (SD) age (years) at randomisation | 66.2 (4.1) | 66.3 (4.1) | 0.21 |
| Mean (SD) age (years) at initial cognitive assessment | 71.8 (4.1) | 71.9 (4.1) | 0.19 |
| Self reported perceived change in memory in past year*: | |||
| None or improved | 83.0 | 82.8 | 0.84 |
| Memory worse | 17.0 | 17.2 | |
| Highest attained education: | |||
| LPVN, associates degree, registered nurse | 66.6 | 67.7 | 0.37 |
| Bachelors degree, masters degree, doctorate | 33.4 | 32.3 | |
| Cigarette smoking: | |||
| Never | 53.3 (1712) | 51.6 (1629) | 0.30 |
| Former | 37.1 (1192) | 38.0 (1203) | |
| Current | 9.6 (307) | 10.4 (328) | |
| Alcohol consumption: | |||
| Less than weekly | 59.4 (1909) | 59.3 (1874) | 0.95 |
| Weekly | 28.5 (916) | 28.4 (896) | |
| Daily | 12.1 (389) | 12.3 (389) | |
| Body mass index: | |||
| <25 | 49.4 (1549) | 50.9 (1574) | 0.49 |
| 25-9 | 35.1 (1100) | 34.2 (1058) | |
| ≥30 | 15.5 (486) | 14.9 (460) | |
| Physical exercise: | |||
| Less than once weekly | 59.7 (1919) | 59.3 (1873) | 0.70 |
| Once or more weekly | 40.3 (1293) | 40.7 (1287) | |
| Hormone replacement therapy use: | |||
| Never | 40.0 (1285) | 40.0 (1261) | 0.67 |
| Past | 19.1 (613) | 19.9 (628) | |
| Current | 40.9 (1314) | 40.1 (1266) | |
| Medical history: | |||
| Diabetes mellitus | 3.4 (110) | 3.5 (111) | 0.85 |
| Hypertension | 40.9 (1315) | 39.2 (1240) | 0.18 |
| Hyperlipidaemia | 42.5 (1365) | 43.5 (1374) | 0.42 |
| Depression‡ | 6.0 (191) | 5.8 (181) | 0.69 |
LPVN=licensed practical or vocational nurse.
*At run-in period.
‡Assessed four years after randomisation.
At the first assessment cognitive performance did not differ by assigned group (table 2). When performance was examined at each follow-up assessment, no mean differences were observed between the groups for global score (table 3). For example, the mean difference between aspirin and placebo groups at the final assessment, after a mean 9.6 years of treatment, was 0.00 (95% confidence interval −0.04 to 0.04). Similarly, for verbal memory no differences were observed between the groups at any of the three assessments. For example, at the final assessment the mean difference for the aspirin group compared with placebo group was −0.02 (−0.06 to 0.02). The aspirin group also did not show better performance in the telephone interview of cognitive status. The aspirin group performed better for category fluency than the placebo group at all three assessments, and this difference was statistically significant at the final assessment (mean difference 0.37 points, 95% confidence interval 0.10 to 0.65). To help interpret this mean difference, the effects of aspirin were compared with the effects of age in this cohort; for each year of age a mean difference in score on category fluency of 0.14 points was observed, thus the effects of aspirin on category fluency seemed equivalent to being 2.6 years younger.
Table 2.
Cognitive test scores at initial assessment.* Values are means (ranges) unless stated otherwise
| Cognitive tests | Aspirin group (n=3215) | Placebo group (n=3162) | P value |
|---|---|---|---|
| Telephone interview of cognitive status | 34.2 (4-41) | 34.3 (15-41) | 0.44 |
| East Boston memory test: | |||
| Immediate recall | 9.6 (0-12) | 9.6 (0-12) | 0.50 |
| Delayed recall | 9.3 (0-12) | 9.3 (0-12) | 0.30 |
| Delayed recall of 10 word list | 3.0 (0-10) | 3.0 (0-10) | 0.68 |
| Category fluency | 17.6 (0-36) | 17.5 (0-43) | 0.31 |
*Initial testing carried out a mean 5.6 years after randomisation.
†Adjusted means.
Table 3.
Cognitive function at each cognitive assessment
| Cognitive test (assessment) | Aspirin group | Placebo group | Mean difference* (95% CI) | |||
|---|---|---|---|---|---|---|
| No of participants | Adjusted mean (SE) | No of participants | Adjusted mean (SE) | |||
| Global score†: | ||||||
| First | 3215 | −0.01 (0.01) | 3162 | 0.00 (0.01) | −0.01 (−0.04 to 0.02) | |
| Second | 2873 | 0.07 (0.01) | 2819 | 0.06 (0.01) | 0.01 (−0.03 to 0.04) | |
| Third | 2630 | 0.02 (0.01) | 2596 | 0.02 (0.01) | 0.00 (−0.04 to 0.04) | |
| Verbal memory score‡: | ||||||
| First | 3215 | −0.01 (0.01) | 3162 | 0.01 (0.01) | −0.02 (−0.05 to 0.02) | |
| Second | 2873 | 0.13 (0.01) | 2819 | 0.13 (0.01) | 0.00 (−0.04 to 0.04) | |
| Third | 2630 | 0.09 (0.02) | 2596 | 0.11 (0.02) | −0.02 (−0.06 to 0.02) | |
| TICS test: | ||||||
| First | 3208 | 34.18 (0.05) | 3154 | 34.26 (0.05) | −0.08 (−0.22 to 0.05) | |
| Second | 2871 | 34.07 (0.05) | 2817 | 34.12 (0.05) | −0.05 (−0.20 to 0.10) | |
| Third | 2630 | 34.09 (0.06) | 2596 | 34.11 (0.06) | −0.02 (−0.19 to 0.14) | |
| Category fluency test: | ||||||
| First | 3202 | 17.58 (0.09) | 3151 | 17.46 (0.09) | 0.12 (−0.13 to 0.36) | |
| Second | 2871 | 18.13 (0.10) | 2817 | 18.02 (0.10) | 0.12 (−0.15 to 0.39) | |
| Third | 2629 | 17.76 (0.10) | 2596 | 17.38 (0.10) | 0.37 (0.10 to 0.65) | |
TICS=telephone interview of cognitive status.
*From longitudinal linear models by treatment assignment of mean cognitive performance.
†Composite of five tests: TICS, immediate and delayed recalls of east Boston memory test, delayed recall of 10 word list, and category fluency.
‡Composite of four tests: immediate and delayed recalls of both 10 word list and east Boston memory test.
No differences were observed in mean change in cognitive performance by treatment assignment for any of the cognitive outcomes (table 4). The mean change over time between the aspirin and placebo groups was 0.01 (95% confidence interval −0.02 to 0.04) for global score, 0.01 (−0.03 to 0.04) for verbal memory score, 0.02 (−0.11 to 0.16) for the telephone interview of cognitive status, and 0.11 (−0.12 to 0.34) for category fluency.
Table 4.
Mean difference in cognitive decline between aspirin and placebo groups during follow-up, from initial assessment
| Cognitive test | Mean difference (95% CI) | P value |
|---|---|---|
| Global score*: | ||
| From first to second assessment | 0.01 (−0.02 to 0.05) | 0.45 |
| From first to third assessment | 0.01 (−0.03 to 0.04) | 0.70 |
| Average over follow-up | 0.01 (−0.02 to 0.04) | 0.50 |
| Verbal memory score†: | ||
| From first to second assessment | 0.02 (−0.02 to 0.06) | 0.38 |
| From first to third assessment | −0.01 (−0.05 to 0.03) | 0.73 |
| Average over follow-up | 0.01 (−0.03 to 0.04) | 0.71 |
| TICS test: | ||
| From first to second assessment | 0.01 (−0.13 to 0.16) | 0.87 |
| From first to third assessment | 0.04 (−0.12 to 0.20) | 0.61 |
| Average over follow-up | 0.02 (−0.11 to 0.16) | 0.71 |
| Category fluency: | ||
| From first to second assessment | −0.01 (−0.28 to 0.25) | 0.91 |
| From first to third assessment | 0.25 (−0.02 to 0.52) | 0.07 |
| Average over follow-up | 0.11 (−0.12 to 0.34) | 0.34 |
TICS=telephone interview of cognitive status.
*Composite of five tests: TICS test, immediate and delayed recalls of east Boston memory test, delayed recall of 10 word list, and category fluency.
†Composite of four tests: immediate and delayed recalls of both 10 word list and east Boston memory test.
The risk of substantial decline on the global score from the first to final assessments for women in the aspirin group was not lower than women in the placebo group; compared with women in the placebo group the relative risk of substantial decline was 0.92 (0.77 to 1.10) for women assigned to aspirin. Only for the test of category fluency did women assigned to aspirin have a statistically significant 20% lower risk of substantial decline than women assigned to placebo (relative risk 0.80, 0.67 to 0.97; table 5).
Table 5.
Relative risk of substantial cognitive decline*
| Cognitive test | No of women | Relative risk of substantial decline (95% CI) | P value |
|---|---|---|---|
| Global score†: | |||
| Placebo | 270 | 1.00 | |
| Aspirin | 253 | 0.92 (0.77 to 1.10) | 0.36 |
| Verbal memory score‡: | |||
| Placebo | 260 | 1.00 | |
| Aspirin | 263 | 1.00 (0.83 to 1.20) | 0.99 |
| TICS test: | |||
| Placebo | 297 | 1.00 | |
| Aspirin | 294 | 0.98 (0.82 to 1.16) | 0.79 |
| Category fluency: | |||
| Placebo | 268 | 1.00 | |
| Aspirin | 222 | 0.80 (0.67 to 0.97) | 0.02 |
TICS=telephone interview of cognitive status.
*Worst 10% of distribution of decline from first to third assessment (global score −0.8 points, verbal memory score −0.9 points, TICS −4 points, category fluency −7 points).
†Composite of five tests: TICS, immediate and delayed recalls of east Boston memory test, delayed recall of 10 word list, and category fluency.
‡Composite of four tests: immediate and delayed recalls of both 10 word list and east Boston memory test.
Secondary analyses
Few interactions were found between aspirin use and cognitive risk factors (table 6). A significant interaction (P for interaction 0.03) was found between cigarette smoking and aspirin use. Among current smokers, the aspirin group experienced significantly less cognitive decline than the placebo group: the difference in mean decline over time between the aspirin and placebo groups was 0.13 (95% confidence interval 0.03 to 0.22). In contrast, little difference was found in mean change between the treatment groups among never smokers or former smokers. Significant differences were also observed in effects of aspirin in relation to cholesterol levels, with aspirin providing cognitive benefits among women with hyperlipidaemia (difference in mean decline 0.05, 95% confidence interval 0.01 to 0.09) but not among those without (−0.02, −0.06 to 0.02).
Table 6.
Mean difference in cognitive decline in global score between aspirin compared with placebo groups: effect modification by major risk factors for cognitive decline*
| Characteristics | Mean difference (95% CI) | P for interaction |
|---|---|---|
| Age (years) at first cognitive assessment: | ||
| <75 | 0.00 (−0.03 to 0.03) | 0.16 |
| ≥75 | 0.06 (−0.02 to 0.13) | |
| Cognitive performance at first assessment: | ||
| Below median | 0.02 (−0.02 to 0.07) | 0.49 |
| Above median | 0.00 (−0.03 to 0.04) | |
| Self reported perceived change in memory†: | ||
| None or improved | 0.00 (−0.03 to 0.03) | 0.21 |
| Worse | 0.05 (−0.02 to 0.12) | |
| Highest attained education: | ||
| LPVN, associates degree, or registered nurse | 0.02 (−0.02 to 0.05) | 0.56 |
| Bachelors degree, masters degree, or doctorate | 0.00 (−0.05 to 0.05) | |
| Cigarette smoking: | ||
| Never | −0.01 (−0.05 to 0.03) | 0.03 |
| Former | 0.01 (−0.03 to 0.06) | |
| Current | 0.13 (0.03 to 0.22) | |
| Alcohol consumption: | ||
| Less than weekly | 0.01 (−0.02 to 0.05) | 0.94 |
| Weekly | 0.01 (−0.05 to 0.06) | |
| Daily | 0.00 (−0.08 to 0.08) | |
| Body mass index: | ||
| <30 | 0.01 (−0.02 to 0.04) | 0.96 |
| ≥30 | 0.01 (−0.06 to 0.08) | |
| Physical exercise: | ||
| Less than once weekly | 0.03 (−0.01 to 0.07) | 0.14 |
| Once or more weekly | −0.02 (−0.06 to 0.03) | |
| Hormone replacement therapy use: | ||
| Never | 0.00 (−0.04 to 0.05) | 0.69 |
| Ever (former plus current) | 0.01 (−0.02 to 0.05) | |
| Diabetes: | ||
| Yes | 0.13 (−0.03 to 0.29) | 0.15 |
| No | 0.01 (−0.02 to 0.04) | |
| Hypertension: | ||
| Yes | −0.02 (−0.06 to 0.03) | 0.17 |
| No | 0.03 (−0.01 to 0.06) | |
| Raised cholesterol level: | ||
| Yes | 0.05 (0.01 to 0.09) | 0.02 |
| No | −0.02 (−0.06 to 0.02) | |
| Depression‡: | ||
| Yes | 0.09 (−0.04 to 0.21) | 0.20 |
| No | 0.00 (−0.03 to 0.03) | |
| Cardiovascular disease during follow-up§: | ||
| Yes | 0.08 (−0.04 to 0.20) | 0.24 |
| No | 0.00 (−0.03 to 0.03) |
LPVN=licensed practical or vocational nurse.
*Characteristics at randomisation, unless stated otherwise.
†Assessed at run-in phase.
‡Assessed four years after randomisation.
§Includes non-fatal myocardial infarction, non-fatal stroke, revascularisation surgery, or cardiovascular death.
Cognitive benefits with aspirin did not differ substantially between women who developed cardiovascular disease (7.4% of participants; mean difference in change in global score 0.08, −0.04 to 0.20) and those who did not (92.6%; 0.00, −0.03 to 0.03). Relatively few women developed cardiovascular disease and the interaction was not statistically significant (P for interaction 0.24).
To evaluate the sensitivity of the results for those at the worst end of the spectrum of cognitive function, those who performed in the worst 10% of the distribution of cognitive function were excluded. No substantial differences were found from the primary findings.
Finally, to assess whether compliance may have influenced the results, the primary analyses were repeated after excluding participants who reported taking less than two thirds of their assigned treatment by the third assessment (30% of participants). The results were robust: the difference in mean change in global score between the aspirin and placebo groups was −0.01 (95% confidence interval−0.05 to 0.02).
Discussion
In a randomised, placebo controlled trial with nearly 10 years of treatment among over 6000 women, this study of women aged 65 or more showed that those assigned to low dose aspirin had similar overall cognitive performance to those receiving placebo. Compared with women receiving placebo, women who took low dose aspirin did not differ in overall performance at any of the three assessments of cognition, ranging from the first assessment after 5.6 years of treatment to the final assessment after a mean 9.6 years of treatment, and also did not differ in their average cognitive decline during 3-6 years of follow-up.
There was some suggestion that women in the aspirin group performed better in the category fluency test than women in the placebo group, particularly at the final assessment; women assigned to aspirin were 20% less likely to develop substantial decline in performance on category fluency. A specific association with category fluency has also been reported in one small trial of low dose aspirin over five years,19 as well as in a large observational study of long term aspirin use.20 Because the category fluency test partially assesses executive function—a cognitive system that is influenced by vascular disease21—it is biologically plausible that low dose aspirin may specifically help preserve executive function. However, because category fluency was the only test in our battery that measured executive function, and because this was not a primary outcome of our trial, this result should be interpreted with caution and confirmed by future studies.
We observed apparent effect modification by high cholesterol level and by smoking status. Among the subset of women with a high cholesterol level, aspirin treatment protected against cognitive decline; this is consistent with the results from the primary trial of cardiovascular events, where aspirin seemed more protective against major cardiovascular events among women with hyperlipidaemia (relative risk 0.80, 95% confidence interval 0.66 to 0.97) than those with normal blood lipid levels (0.98, 0.84 to 1.16).11 Also, women who were current smokers and assigned to aspirin experienced less cognitive decline over time than smokers who were taking placebo; in contrast, aspirin had no effect on cognition among women who never smoked or had quit smoking. These results were the opposite of those found in the primary trial of cardiovascular events,11 where aspirin seemed protective against major cardiovascular events only among women who never smoked or had quit smoking. Given the numerous subgroup analyses carried out, chance cannot be ruled out as an explanation for these findings.
Limitations of the study
A limitation of our trial is that the study population consisted of mainly healthy white “young-old” (mean age 72) women; thus, whether the results are generalisable to women of older ages or other races is unknown. The age of the study population may have contributed to the lack of major decline in cognitive function over the follow-up period of 3-6 years, although we have detected other risk factors for cognitive decline in these women over a similar period.22 23 In addition, we started cognitive testing a mean 5.6 years after randomisation, thus we were unable to measure change in cognitive performance from randomisation. However, at randomisation numerous risk factors for cognitive impairment were similarly distributed across treatment groups, and it is highly likely in this large trial that cognitive function was also comparable between the groups at randomisation. Thus the lack of a true baseline cognitive assessment should not have a major influence on our ability to detect effects of long term aspirin use on cognitive decline. Although it is possible that there may have been some transient, short term benefits of aspirin on cognition just during the first 5.6 years, this possibility seems biologically implausible given that cognitive changes develop progressively over long periods. Finally, loss to follow-up did not differ by treatment group; however, greater losses to follow-up occurred among those who developed cardiovascular disease (15%) compared with the entire cohort (8%). Thus there may have been some bias towards the null; however, such bias would be minimal as the proportion of women with cardiovascular events was low.
Although many observational studies have investigated the use of non-steroidal anti-inflammatory drugs in relation to cognitive decline,8 few studies20 24 25 26 have specifically examined aspirin use. These studies have generally shown inconsistent associations between aspirin and cognitive decline, largely supporting our null results. For example, one small study26 of 612 participants aged 62-85 followed for three years reported significant inverse associations between continued low dose aspirin use and cognitive decline. Yet in a study among 2087 people aged 65 or more followed for three years, little association was found for low or medium dose aspirin (relative risk 0.90, 95% confidence interval 0.48 to 1.69);24 similarly, a study25 of 2556 participants aged 65 or more found that aspirin use was related to a small, non-significant decrease in cognitive decline over six years: for intermittent use of aspirin (<1 aspirin daily) the relative risk for cognitive decline was 0.84 (0.66 to 1.06), and for 1-2 aspirins daily the relative risk was 0.91 (0.68 to 1.22). The largest observational study,20 including 13 255 women aged at least 70, found that long term use of low dose aspirin for 15 years or more had little association with substantial decline in cognition over two years (relative risk 0.91, 95% confidence interval 0.70 to 1.19). This present study contributes to the existing literature in that biases related to the indication for aspirin treatment are minimised owing to randomisation and the length of aspirin treatment (almost 10 years), allowing for strong conclusions about the specificity of the role of aspirin in cognitive changes.
Biologically our null results should be interpreted in light of the treatment dose and the drug selected. Although the low prophylactic aspirin dose used in this trial (100 mg on alternate days) has shown antiplatelet activity, it confers limited anti-inflammatory effects.27 In addition, unlike some non-steroidal anti-inflammatory drugs such as ibuprofen,28 aspirin lacks the ability in vitro to modulate the processing of the amyloid precursor protein, believed to be critical in the pathogenesis of Alzheimer's disease, the most common cause of dementia.
The most likely mechanism by which low dose aspirin might influence cognitive decline is that aspirin reduces platelet aggregation, improves cerebral blood flow, and prevents cardiovascular disease; although, overall, aspirin did not reduce major cardiovascular events in the primary trial of the women's health study,11 among the subset of women aged 65 or more, treatment conferred a modest protective effect against major cardiovascular events (relative risk 0.74, 95% confidence interval 0.59 to 0.92). Although we found no cognitive benefits of aspirin in this trial, it remains possible that any benefits require many years to noticeably affect cognitive decline; indeed it is widely believed that brain ageing takes decades to develop.29 Several recent studies30 31 32 33 34 have reported adverse relations between vascular risk factors in middle age and development of cognitive impairment later in life, implying that for prevention, early modification of cardiovascular risk may be most important.
In conclusion, in this study within a large, randomised, placebo controlled trial among over 6000 healthy women aged 65 or more, we observed no apparent benefit of low dose aspirin in slowing cognitive decline over four years. Other methods for preserving cognitive function in older people need to be investigated.
What is already known on this topic
Laboratory and epidemiological evidence suggests that aspirin and other anti-inflammatory drugs may be protective against dementia
Data from randomised studies to date have been inconclusive
What this study adds
Low dose aspirin did not provide overall cognitive benefits in generally healthy ageing women participating in a large, long term randomised trial
We thank the participants, staff, and investigators of the women's health study.
Contributors: All authors conceived and designed the study. JHK and FG carried out the study. JHK and NC analysed the data. JHK drafted the manuscript and is guarantor. All authors critically reviewed the paper and approved the final draft for publication.
Funding: The study was supported by grant AG15933 from the National Institute of Aging, HL-43851 from the National Heart, Lung, and Blood Institute, and CA-47988 from the National Cancer Institute. Aspirin and placebo were provided by Bayer HealthCare.
Competing interests: None declared.
Ethical approval: The trial was approved by the institutional review board of Brigham and Women's Hospital.
References
- 1.Small BJ, Fratiglioni L, Viitanen M, Winblad B, Backman L. The course of cognitive impairment in preclinical Alzheimer disease: three- and 6-year follow-up of a population based sample. Arch Neurol 2000;57:839-44. [DOI] [PubMed] [Google Scholar]
- 2.Amieva H, Jacqmin-Gadda H, Orgogozo J-M, Le Carret N, Helmer C, Letenneur L, et al. The 9 year cognitive decline before dementia of the Alzheimer type: a prospective population-based study. Brain 2005;128:1093-101. [DOI] [PubMed] [Google Scholar]
- 3.Rogers J, Kirby LC, Hempelman SR, Berry DL, McGeer PL, Kaszniak AW, et al. Clinical trial of indomethacin in Alzheimer's disease. Neurology 1993;43:1609-11. [DOI] [PubMed] [Google Scholar]
- 4.Scharf S, Mander A, Ugoni A, Vajda F, Christophidis N. A double-blind, placebo-controlled trial of diclofenac/misoprostol in Alzheimer's disease. Neurology 1999;53:197-201. [DOI] [PubMed] [Google Scholar]
- 5.Aisen PS, Davis KL, Berg JD, Schafer K, Campbell K, Thomas RG, et al. A randomized controlled trial of prednisone in Alzheimer's disease. Alzheimer's disease cooperative study. Neurology 2000;54:588-93. [DOI] [PubMed] [Google Scholar]
- 6.Van Gool WA, Weinstein HC, Scheltens P, Walstra GJ. Effect of hydroxychloroquine on progression of dementia in early Alzheimer's disease: an 18-month randomised, double-blind, placebo-controlled study. Lancet 2001;358:455-60. [DOI] [PubMed] [Google Scholar]
- 7.Aisen PS, Schafer KA, Grundman M, Pfeiffer E, Sano M, Davis KL, et al. Effects of rofecoxib or naproxen vs placebo on Alzheimer disease progression: a randomized controlled trial. JAMA 2003;289:2819-26. [DOI] [PubMed] [Google Scholar]
- 8.De Craen AJ, Gussekloo J, Vrijsen B, Westendorp RG. Meta-analysis of nonsteroidal antiinflammatory drug use and risk of dementia. Am J Epidemiol 2005;161:114-20. [DOI] [PubMed] [Google Scholar]
- 9.Couzin J. Halt of Celebrex study threatens drug's future, other trials. Science 2004;306:2170. [DOI] [PubMed] [Google Scholar]
- 10.Steering Committee of the Physician's Health Study Research Group. Final report on the aspirin component of the ongoing physician's health study. N Engl J Med 1989;321:129-35. [DOI] [PubMed] [Google Scholar]
- 11.Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005;352:1293-304. [DOI] [PubMed] [Google Scholar]
- 12.Buring JE, Hennekens CH. The women's health study: summary of the design. J Myocardial Ischemia 1992;4:27-9. [Google Scholar]
- 13.Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, et al. Low-dose aspirin in the primary prevention of cancer: the women's health study: a randomized controlled trial. JAMA 2005;294:47-55. [DOI] [PubMed] [Google Scholar]
- 14.Kang JH, Cook NR, Manson JE, Buring JE, Grodstein F. A randomized trial of vitamin E and cognitive function in women. Arch Intern Med 2006;166:2462-8. [DOI] [PubMed] [Google Scholar]
- 15.Brandt J, Folstein MF. Telephone interview for cognitive status: professional manual Lutz, FL: Psychological Assessment Resources, 2003
- 16.Scherr PA, Albert MS, Funkenstein HH, Cook NR, Hennekens CH, Branch LG, et al. Correlates of cognitive function in an elderly community population. Am J Epidemiol 1988;128:1084-101. [DOI] [PubMed] [Google Scholar]
- 17.Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology 1989;39:1159-65. [DOI] [PubMed] [Google Scholar]
- 18.Fitzmaurice GM, Laird NM, Ware JH. Modelling the mean: analyzing response profiles. Applied longitudinal analysis Hoboken, NJ: John Wiley, 2004:103-39.
- 19.Richards M, Meade TW, Peart S, Brennan PJ, Mann AH. Is there any evidence for a protective effect of antithrombotic medication on cognitive function in men at risk of cardiovascular disease? Some preliminary findings. J Neurol Neurosurg Psychiatry 1997;62:269-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kang JH, Grodstein F. Regular use of non-steroidal anti-inflammatory drugs and cognitive function in aging women. Neurology 2003;60:1591-7. [DOI] [PubMed] [Google Scholar]
- 21.Roman GC, Royall DR. Executive control function: a rational basis for the diagnosis of vascular dementia. Alzheimer Dis Assoc Disord 1999;13(Suppl 3):S69-80. [DOI] [PubMed] [Google Scholar]
- 22.Devore E, Buring JE, Grodstein F. Plasma cholesterol levels and cognitive function in older women [abstract]. Neurobiol Aging 2004;25(Suppl 2):S52 [Google Scholar]
- 23.Lee S, Buring JE, Cook NR, Grodstein F. The relation of education and income to cognitive function among professional women. Neuroepidemiology 2006;26:93-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saag KG, Rubenstein LM, Chrischilles EA, Wallace RB. Nonsteroidal antiinflammatory drugs and cognitive decline in the elderly. J Rheumatol 1995;22:2142-7. [PubMed] [Google Scholar]
- 25.Sturmer T, Glynn RJ, Field TS, Taylor JO, Hennekens CH. Aspirin use and cognitive function in the elderly. Am J Epidemiol 1996;143:683-91. [DOI] [PubMed] [Google Scholar]
- 26.Jonker C, Comijs HC, Smit JH. Does aspirin or other NSAIDs reduce the risk of cognitive decline in elderly persons? Results from a population-based study. Neurobiol Aging 2003;24:583-8. [DOI] [PubMed] [Google Scholar]
- 27.Ridker PM, Hennekens CH, Tofler GH, Lipinska I, Buring JE. Anti-platelet effects of 100 mg alternate day oral aspirin: a randomized, double-blind, placebo-controlled trial of regular and enteric coated formulations in men and women. J Cardiovasc Risk 1996;3:209-12. [PubMed] [Google Scholar]
- 28.Weggen S, Eriksen JL, Das P, Sagi SA, Wang R, Pietrzik CU, et al. A subset of NSAIDs lower amyloidogenic Ab42 independently of cyclooxygenase activity. Nature 2001;414:212-6. [DOI] [PubMed] [Google Scholar]
- 29.Braak E, Griffing K, Arai K, Bohl J, Bratzke H, Braak H. Neuropathology of Alzheimer's disease: what is new since A. Alzheimer? Eur Arch Psychiatry Clin Neurosci 1999;249(Suppl 3):14-22. [DOI] [PubMed] [Google Scholar]
- 30.Swan GE, DeCarli C, Miller BL, Reed T, Wolf PA, Jack LM, et al. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology 1998;51:986-93. [DOI] [PubMed] [Google Scholar]
- 31.Launer LJ, Masaki K, Petrovitch H, Foley D, Havlik RJ. The association between midlife blood pressure levels and late-life cognitive function. The Honolulu-Asia aging study. JAMA 1995;274:1846-51. [PubMed] [Google Scholar]
- 32.Elias PK, Elias MF, D'Agostino RB, Cupples LA, Wilson PW, Silbershatz H, et al. NIDDM and blood pressure as risk factors for poor cognitive performance. The Framingham study. Diabetes Care 1997;20:1388-95. [DOI] [PubMed] [Google Scholar]
- 33.Carmelli D, Swan GE, Reed T, Miller B, Wolf PA, Jarvik GP, et al. Midlife cardiovascular risk factors, ApoE, and cognitive decline in elderly persons. JAMA 1998;50:1580-5. [DOI] [PubMed] [Google Scholar]
- 34.Kivipelto M, Helkala EL, Laakso MP, Hanninen T, Hallikainen M, Alhainen K, et al. Midlife vascular risk factors and Alzheimer's disease in later life: longitudinal, population based study. BMJ 2002;322:1447-51. [DOI] [PMC free article] [PubMed] [Google Scholar]