Abstract
Objective:
To establish the indications of the liver hanging maneuver for major hepatectomy.
Summary Background Data:
The liver hanging maneuver, which is a technique of passing a tape along the retrohepatic avascular space and suspending the liver during parenchymal transection, facilitates anterior approach of major hepatectomy. However, the feasibility and limits of this maneuver have never been established in patients with different clinical backgrounds.
Methods:
Medical records of 242 consecutive patients considered for major hepatectomy using the hanging maneuver were reviewed.
Results:
Among 242 patients, 14 patients (6%) were considered to have contraindication for this maneuver preoperatively because of tumor infiltration to anterior surface of retrohepatic inferior vena cava (IVC). It was successful in 201 patients with overall feasibility of 88%. The feasibility increased significantly in the recent years as compared with the initial years (94% in 2003–2005 vs. 76% in 2000–2002, P < 0.0001). Bleeding during the retrohepatic dissection occurred in 5 patients (2%), which was minor due to injury of hepatic capsule in 3 (1%) and major due to injury of short hepatic vein in 2 (1%). In all cases, bleeding stopped spontaneously. The maneuver was abandoned in 27 patients, including 15 related to severe adhesion between liver and IVC. Univariate analysis showed that adhesion between IVC and liver was the only significant negative predictor affecting the feasibility. Cirrhosis, large tumor, preoperative radiologic treatments did not influence on the feasibility.
Conclusions:
The liver hanging maneuver has 94% feasibility in recent years. Absolute contraindication is tumor infiltration to the retrohepatic avascular space. Adhesion between the IVC and liver has a negative impact of the feasibility. According to this indication, the hanging maneuver is easily achievable without risk of the major bleeding during the retrohepatic dissection.
The aim of this study is to investigate the feasibility of liver hanging maneuver in patients with different clinical backgrounds and clarify the limits of this technique, which has achieved a feasibility of 94% in recent years. Hanging maneuver is contraindicated in cases of tumor infiltration to the retrohepatic avascular space, and adhesion between the inferior vena cava and liver has a negative impact on the feasibility.
The liver hanging maneuver developed by our group is a technique of passing a tape between the anterior surface of the inferior vena cava (IVC) and the liver and suspending the liver during hepatic parenchymal transection.1 This technique facilitates major hepatectomy with “anterior approach,” which was established by Lai et al, reducing several risks caused by liver mobilization: 1) bleeding, 2) rupture of the tumor, 3) tumor cell dissemination, and 4) hemodynamic instability.2 Moreover, suspending the liver with a tape has several advantages: 1) it facilitates control of bleeding at the deeper parenchymal plane and 2) it guides the direction of anatomic parenchymal transection.1,3 This technique has been used in right hepatectomy,1,3–6 as well as in left-sided hepatectomy requiring exposure of anterior surface of the IVC,7 in donor operations for living donor liver transplantation, where a hepatic parenchymal transection should be performed before dividing the feeding vessels for the graft.3
The most important and technically difficult step of this maneuver, blind retrohepatic dissection, is proved to be safe based on the anatomic fact, shown by several morphologic studies, that there is an approximately 1 cm wide avascular space located at 10 to 11 o'clock position of the anterior surface of the retrohepatic IVC (Fig. 1). 8–14 Indeed, the reported incidence of bleeding from an injured short hepatic vein during the retrohepatic dissection was 0% to 4%.3–7 However, since hepatic parenchymal status, tumor characteristics, preoperative treatment, and surgical history are variable in each patient, some surgeons hesitate to try this maneuver for fear of possible massive bleeding during the retrohepatic dissection. The aim of this study is to investigate the feasibility of the hanging maneuver in patients with different clinical backgrounds and clarify the limits of this maneuver.
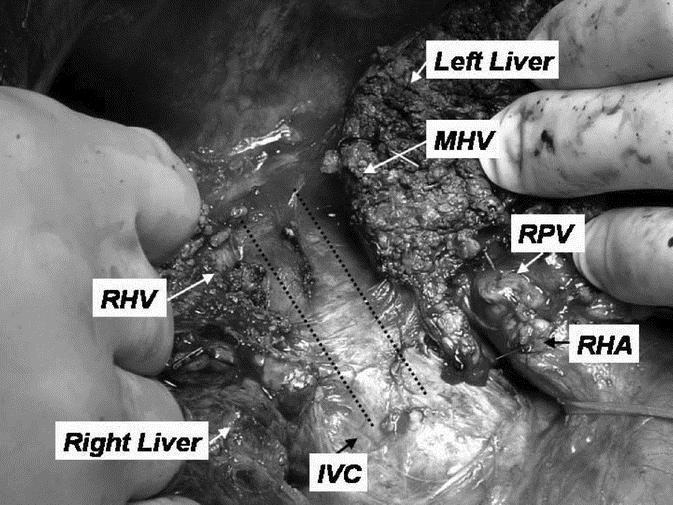
FIGURE 1. Intraoperative photograph immediately after completion of the liver parenchymal transection in right hepatectomy. The avascular space, located at 10 to 11 o'clock position of the anterior surface of retrohepatic IVC, is completely exposed (space between 2 broken lines). RHV, right hepatic vein; MHV, middle hepatic vein; RPV, right portal vein; RHA, right hepatic artery.
METHODS
Patients
Between June 2000 and July 2005, we reviewed the cohort of 242 consecutive patients with a median (range) age of 53 years (18–83 years) considered for major hepatic resection (resection of ≥4 Couinaud segments) using the hanging maneuver at the Department of Liver Surgery, Beaujon Hospital. All patients with histologically confirmed primary or metastatic malignancies with no clinical, radiographic, or intraoperative evidence of unresectable extrahepatic disease were eligible.
Preoperative Assessment
All patients were evaluated preoperatively with physical examination; serum laboratory tests including liver function tests and hepatitis B and C virus serology as appropriate.15 Status of the nontumorous liver parenchyma was defined according to the classification of Knodell et al by preoperative liver biopsy.16
Preoperative decision-making to consider the liver hanging maneuver was based on tumor location assessed by a triphasic computed tomography (CT). Special attention was given to assess the state of IVC from the level of hepato-caval confluence up to right renal vein. Hanging maneuver was considered to be indicated if tumors did not infiltrate the avascular space located at 10 to 11 o'clock position of the anterior surface of retrohepatic IVC (Fig. 2A, B). Direct invasion of tumors to distal major hepatic veins, diaphragm, retroperitoneum, or tumor contact with IVC except the avascular space were not considered as contraindication to perform the hanging maneuver. Even though initial assessment shows tumor infiltration to the anterior surface of IVC, tumor regression induced by systemic chemotherapy making the retrohepatic space free of tumor enables to consider the hanging maneuver (Fig. 2C).
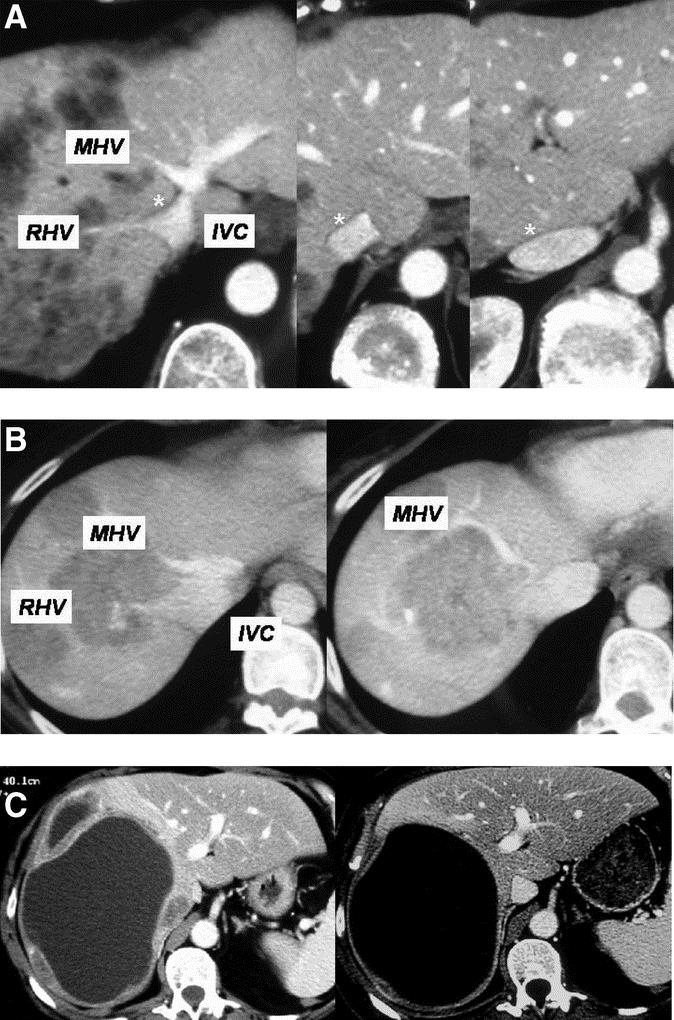
FIGURE 2. A, Indication for the liver hanging maneuver in a 46-year-old man with colorectal metastases. Preoperative CT scan reveals tumor-free space at 10 to 11 o'clock position of the anterior surface of retrohepatic IVC (*). This patient underwent right hepatectomy with the liver hanging maneuver. B, Contraindication for the liver hanging maneuver in a 40-year-old man with colorectal metastases. Preoperative CT scan after portal vein embolization reveals tumor infiltration between right hepatic vein and middle hepatic vein, as well as anterior surface of retrohepatic IVC. This patient underwent extended right hepatectomy without using the liver hanging maneuver. C, CT scan reveals tumor infiltration to the anterior surface of IVC in a 69-year-old woman with metastasis from epidermoid carcinoma of anal canal (left). Six-month systemic chemotherapy induced tumor regression, making the retrohepatic space free of tumor (right). This patient underwent right hepatectomy with the liver hanging maneuver.
Surgical Techniques
The liver is exposed through an abdominal incision using either a bilateral subcostal or a J-shaped incision. Intraoperative ultrasound is performed with special attention to confirm the absence of tumor infiltration and abnormal short hepatic veins at 10 to 11 o'clock position of the anterior surface of retrohepatic IVC. The technique of retrohepatic dissection for the hanging maneuver was described previously.1 In brief, the upper surface of the liver is exposed up to the anterior surface of the suprahepatic IVC. The space between the right hepatic vein (RHV) and the middle hepatic vein (MHV) is dissected with the punch-burn-cut method and subsequently 3 to 4 cm downwards with a right angled dissector and vascular clamp. For caudal retrohepatic dissection, the caudal edge of the caudate lobe is lifted from the IVC, and small short hepatic veins are divided and ligated up to the level of inferior right hepatic vein. A long light curved aortic clamp is inserted behind the caudate lobe just to the left side of right inferior hepatic vein and passed cranially along the anterior surface of IVC between 10 and 11 o'clock position, identifying the position of the clamp tip assisted by ultrasonography, by successively opening and closing the clamp, toward the previously dissected space between the RHV and MHV until the clamp tip reaches suprahepatically. Normally, the retrohepatic dissection can be performed without encountering any resistance. When adhesion between the IVC and liver is severe due to previous surgery or inflammation in caudal part of the retrohepatic IVC causing resistance to the dissection, the retrohepatic dissection is discontinued. A 10-mm-wide soft, silicon multitubular drain is seized with the clamp and pulled down through the retrohepatic space. As described previously, when the right hepatectomy with the MHV, the tape is switched from the right to the left side of the MHV.17 This allows safer dissection of the MHV near the vena cava confluence.
Parenchymal transection is performed by either clamp-crush technique or with an ultrasound aspiration dissector (Dissectron, Satelec Medical, Merignac-France) under intermittent clamping of the hepatic pedicle.18 The liver is suspended with the tape during the transection. During deeper parenchymal transection, continuous traction is applied on the tape by holding both ends of the tape together. This maneuver helps to reduce venous back flow bleeding facilitating bloodless transection. Biliostasis and hemostasis of vessels smaller than 3 mm were performed using irrigated bipolar coagulation. Larger vessels were ligated with clips or sutures.
Statistical Analysis
Statistical analysis was performed using Medcalc version 7.3 (Frank Schoonjans, Broekstraat, Belgium). The Fisher exact test or χ2 test was used for qualitative variables. P < 0.05 was considered significant.
RESULTS
Among 242 patients, 14 patients (5.8%) were considered to have contraindication to perform the hanging maneuver preoperatively because of tumor infiltration to anterior surface of retrohepatic IVC (Table 1). These patients underwent curative hepatectomy without using the hanging maneuver.
TABLE 1. Feasibility of Hanging Maneuver According to Diagnosis
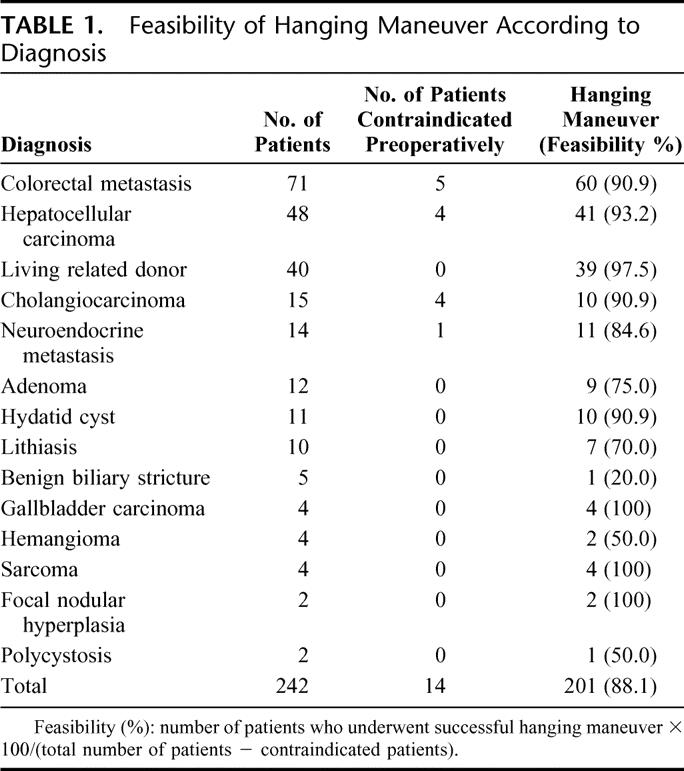
Among the 228 patients on whom the hanging maneuver was attempted, it was successful in 201 patients with overall feasibility of 88.1%. Using the liver hanging maneuver, right hepatectomy without the MHV (n = 159), right hepatectomy with the MHV (n = 28), left hepatectomy with caudate lobe (n = 9), and extended left hepatectomy (resection of segment 1, 2, 3, 4, 5, and 8) (n = 5) were performed. The median operative time was 420 minutes (range, 180–760 minutes). The median operative blood loss was 700 mL (range, 100–3600 mL). In living donation, patients with hepatocellular carcinoma, colorectal metastasis, and cholangiocarcinoma, the feasibility of the hanging maneuver was >90%. The feasibility was ≤50% in patients with benign biliary stricture, polycystosis, and hemangioma (Table 1). Among 8 patients with colorectal metastasis in whom the hanging maneuver was considered contraindicated due to tumor infiltration to the anterior surface of IVC, tumor regression after systemic chemotherapy was encountered in 3 patients (37.5%) and enabled the hanging maneuver to be performed successfully without any technical difficulty (Fig. 2C).
The hanging maneuver was abandoned in 27 patients for one or more of the following reasons: severe adhesion between IVC and liver (n = 15; 5.3%), voluminous tumor (n = 5; 2.2%), tumor bleeding (n = 3; 1.3%), severe liver atrophy (n = 3; 1.3%), bleeding during the retrohepatic dissection (n = 2; 0.9%), and not specified (n = 5; 2.2%). These 27 patients underwent conventional hepatectomy with liver mobilization or with anterior approach without the hanging maneuver. Bleeding during the retrohepatic dissection was encountered in 5 patients (2.2%). The bleeding was minor (estimated blood loss, <50 mL) in 3 patients (1.3%) and was major (estimated blood loss, 100–200 mL) in 2 patients (0.9%). The minor bleeding was caused by wrong plane of dissection under hepatic capsule in all 3 patients. The major bleeding was observed in 1 patient caused by inserting the clamp in wrong direction to the left anterior surface of the IVC. The other was caused by injury of abnormal short hepatic vein on caudal half of retrohepatic IVC, although the dissection was on the proper plane, in patients with complete obstruction of right hepatic vein with tumor thrombosis. In all cases, either minor or major, the bleeding stopped spontaneously. The hanging maneuver was reattempted and was successful after hemostasis in 3 patients with minor bleeding. No other complication related to retrohepatic dissection was encountered.
As shown in Figure 3, the feasibility of the hanging maneuver clearly demonstrated a learning curve. The feasibility was significantly higher in the recent years than that in the initial years (143 of 152, 94.1% in 2003–2005 vs. 58 of 76, 76.3% in 2000–2002, P < 0.0001). The patients in whom the hanging maneuver failed because of bleeding during the retrohepatic dissection, severe liver atrophy, and tumor bleeding were experienced during the initial 3 years due to paucity of experience.
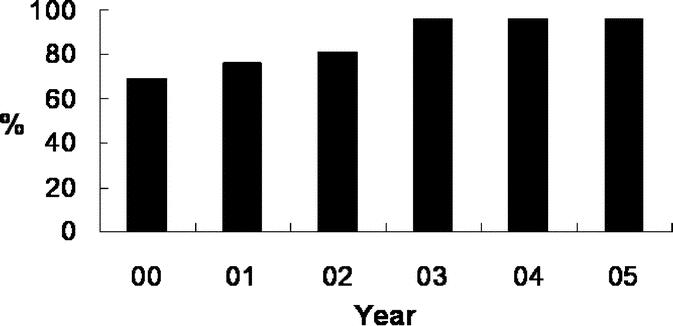
FIGURE 3. The feasibility of the hanging maneuver (2000–2005). The feasibility of the hanging maneuver clearly demonstrated leaning curve. The feasibility was significantly higher in the recent years than that in the initial years (143 of 152 [94.1%] in 2003–2005 vs. 58 of 76 [76.3%] in 2000–2002, P < 0.0001).
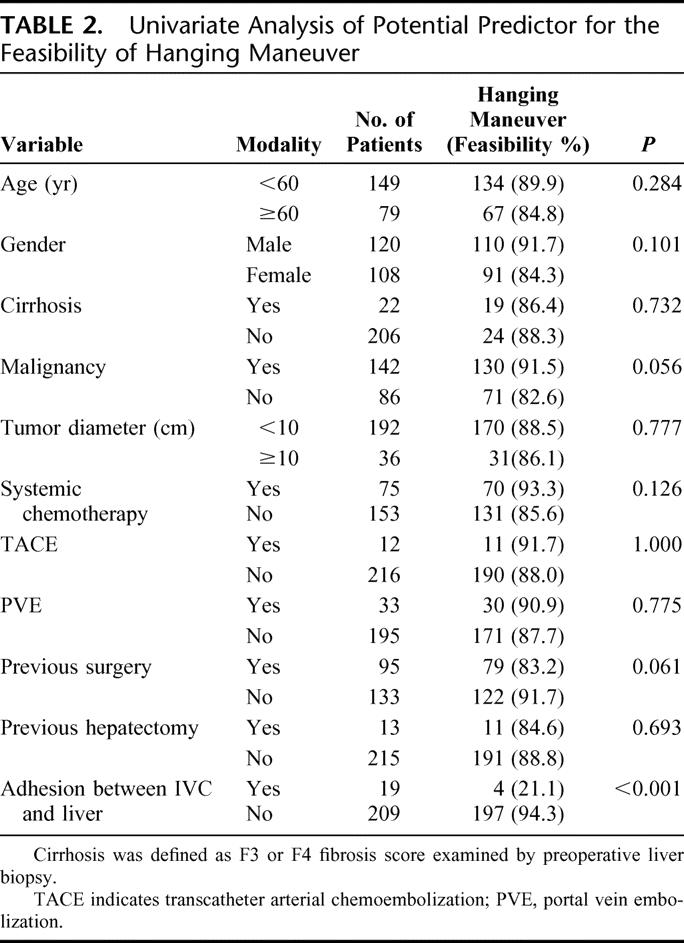
Among the 228 patients on whom the hanging maneuver was attempted, 11 independent clinical variables were analyzed as potential predictors for the feasibility of the hanging maneuver. On univariate analysis, only one of 11 variables, adhesion between IVC and liver, proved to be significant (Table 2). Among the 19 patients with adhesion between IVC and liver, 15 patients had undergone previous surgery in hilar plate or liver resection in right liver and the other 4 patients had inflammation in benign cyst or tumor. Among the 13 post hepatectomy patients, the hanging maneuver was feasible in the 10 patients after limited hepatectomy in the left liver, including the 8 patients with two-step hepatectomy.19 Cirrhosis, large tumor, preoperative transcatheter arterial chemoembolization, and/or portal vein embolization and systemic chemotherapy did not affect on the feasibility of the hanging maneuver.
TABLE 2. Univariate Analysis of Potential Predictor for the Feasibility of Hanging Maneuver
DISCUSSION
The most important and technically difficult step of the liver hanging maneuver is the dissection of the anterior plane of the IVC.1 This is considered as unsafe by some surgeons because of the false notion that the distribution of short hepatic veins is diffuse along the anterior surface of the IVC. However, lessons learned during the total hepatectomy for the recipient of orthotopic liver transplantation have shown that there is a space with no short hepatic veins along the right part of the anterior surface of IVC. Furthermore, several morphologic studies have demonstrated there is an approximately 1-cm-wide avascular space between the 10 and 11 o'clock position, especially in the cranial half of retrohepatic IVC (Fig. 1).8–14 Based on this evidence, we considered the blind retrohepatic dissection safe in the absence of tumor infiltration to this avascular space. Combination of preoperative CT scan as well as intraoperative ultrasound could accurately assess tumor infiltration to the avascular space, avoiding accidental injury during the retrohepatic dissection.20 Excluding these patients who were considered as absolute contraindication, we achieved a success rate of 88% for this maneuver.
Major bleeding during the retrohepatic dissection, which was encountered in the first year, occurred in 2 patients (0.9%) in our experience. Despite being along proper plane during retrohepatic dissection, injury of short hepatic veins occurred in 1 patient with complete right hepatic venous obstruction by tumor thrombosis. The abnormal short hepatic veins on the proper plane on retrohepatic IVC had probably increased in size and/or developed as collaterals like in Budd-Chiari syndrome. Since then, intraoperative ultrasonography before the hanging maneuver has been performed routinely with special attention to identify abnormal short hepatic veins on the retrohepatic avascular space.20 The other was caused by inserting the clamp in wrong direction. After this accidental venous injury, ultrasonography has been used routinely to identify the position of the clamp tip during the retrohepatic dissection. The assistance of ultrasonography could overcome the pitfall of blind dissection with possible hepatic venous injury caused by inserting the clamp in wrong direction.
Our results showed a significant learning curve in the feasibility of the hanging maneuver. The feasibility of this maneuver became 94% in the recent 3 years with no incidence of major bleeding during the retrohepatic dissection. The following technical modifications in the retrohepatic dissection have significantly contributed to improvement of our results in the recent years: 1) cranial dissection between the RHV and MHV for 3 to 4 cm downwards with a right angled vascular clamp, 2) caudal ligation of short hepatic veins up to the level of inferior right hepatic vein, and 3) inserting operator's left index finger into the previously dissected cranial space to control the direction of blind dissection with a light curved aortic clamp. These technical modifications have reduced the length of the blind dissection to approximately 2 cm in contrast to the previous technique where the dissection was 4 to 6 cm long.1 These technical improvements could be easily assimilated, not only by the senior liver surgeons but also by the residents. This successful experience has helped to avoid hesitation and fear to perform this maneuver even by inexperienced junior surgeons.
Colorectal liver metastasis located in the paracaval portion of the caudate lobe could be difficult to treat surgically because such tumor often invades the hepatic veins and/or IVC.21 Our results showed that tumor regression induced by preoperative systemic chemotherapy allowed us to perform safely the hanging maneuver in 38% of patients initially considered as contraindication. Although preoperative chemotherapy has offered a possibility of cure to previously unresectable patients with the liver surgery after tumor downstaging,22 our experience suggests a new indication of preoperative chemotherapy for patients with tumor close to major vessels to facilitate technical procedure in hepatectomy.
Univariate analysis for potential predictors of the feasibility of the hanging maneuver showed adhesion between IVC and liver was the only significant factor negatively affecting the feasibility. As previously thought, cirrhosis or large tumor, which were considered as relative contraindications, were not significant factors affecting the success rate of the hanging maneuver. Based on this result, we consider adhesion between IVC and liver caused by previous surgery or severe tumor inflammation as relative contraindication for the hanging maneuver.
CONCLUSION
The liver hanging maneuver has 94% feasibility in recent years. Use of ultrasonographic assistance and technical modification shortening the length of blind dissection avoid accidental injury of short hepatic vein during retrohepatic dissection. The absolute contraindication for the hanging maneuver is tumor infiltration to the retrohepatic avascular space. Adhesion between the IVC and liver has a negative impact on the feasibility of this technique. According to this indication, the hanging maneuver using advanced technique is easily achievable without risk of the major bleeding during the retrohepatic dissection.
Footnotes
Reprints: Jacques Belghiti, MD, Department of Surgery, Hospital Beaujon, 100 Boulevard du Général Leclerc, 92118 Clichy Cedex, France. E-mail: jacques.belghiti@bjn.aphp.fr.
REFERENCES
- 1.Belghiti J, Guevara OA, Noun R, et al. Liver hanging maneuver: a safe approach to right hepatectomy without liver mobilization. J Am Coll Surg. 2001;193:109–111. [DOI] [PubMed] [Google Scholar]
- 2.Lai EC, Fan ST, Lo CM, et al. Anterior approach for difficult major right hepatectomy. World J Surg. 1996;20:314–317. [DOI] [PubMed] [Google Scholar]
- 3.Kokudo N, Sugawara Y, Imamura H, et al. Sling suspension of the liver in donor operation: a gradual tape-repositioning technique. Transplantation. 2003;76:803–807. [DOI] [PubMed] [Google Scholar]
- 4.Ettorre GM, Vennarecci G, Santoro R, et al. Modified liver hanging maneuver during orthotopic liver transplantation with inferior vena cava preservation. Transplantation. 2003;75:247–249. [DOI] [PubMed] [Google Scholar]
- 5.Ettorre GM, Vennarecci G, Boschetto A, et al. Feasibility of hanging maneuvers in orthotopic liver transplantation with inferior vena cava preservation and in liver surgery. J Hepatobiliary Pancreat Surg. 2004;11:155–158. [DOI] [PubMed] [Google Scholar]
- 6.Suzuki M, Unno M, Katayose Y, et al. Hepatic resection through an anterior approach employing a modified liver hanging maneuver in patients with a massive liver tumor severely oppressing the inferior vena cava. Hepatogastroenterology. 2004;51:1459–1463. [PubMed] [Google Scholar]
- 7.Suh KS, Lee HJ, Kim SH, et al. Hanging maneuver in left hepatectomy. Hepatogastroenterology. 2004;51:1464–1466. [PubMed] [Google Scholar]
- 8.Couinaud C. Surgical Anatomy of the Liver, Revisited. Paris: Couinaud, 1989:115. [Google Scholar]
- 9.Chang RWH, Shan-Quan S, Yen WWC. An applied anatomical study of the ostia venae hepaticae and retrohepatic segment of the inferior vena cava. J Anat. 1989;164:41–47. [PMC free article] [PubMed] [Google Scholar]
- 10.Sleiman Raad Camargo AM, Gracioli Teixeira G, Ortale JR. Anatomy of the ostia venae hepaticae and the retrohepatic segment of the inferior vena cava. J Anat. 1996;188:59–64. [PMC free article] [PubMed] [Google Scholar]
- 11.Sato TJ, Hirai I, Murakami G, et al. An anatomical study of short hepatic veins, with special reference to delineation of the caudate lobe for hanging maneuver of the liver without the usual mobilization. J Hepatobiliary Pancreat Surg. 2002;9:55–60. [DOI] [PubMed] [Google Scholar]
- 12.Hirai I, Murakami G, Kimura W, et al. How should we treat short hepatic veins and paracaval branches in anterior hepatectomy using the hanging maneuver without mobilization of the liver? An anatomical and experimental study. Clin Anat. 2003;16:224–232. [DOI] [PubMed] [Google Scholar]
- 13.Meng WC, Shao CX, Mak KL, et al. Anatomical justification of Belghiti's ‘liver hanging manoeuvre’ in right hepatectomy with anterior approach. Aust NZ J Surg. 2003;73:407–409. [DOI] [PubMed] [Google Scholar]
- 14.Trotovsek B, Belghiti J, Gadzijev EM, et al. Anatomical basis of the liver hanging maneuver. Hepatogastroenterology. 2005;52:728–730. [PubMed] [Google Scholar]
- 15.Belghiti J, Ogata S. Assessment of hepatic reserve for the indication of hepatic resection. J Hepatobiliary Pancreat Surg. 2005;12:1–3. [DOI] [PubMed] [Google Scholar]
- 16.Knodell RG, Ishak KG, Black WC, et al. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology. 1981;1:431–435. [DOI] [PubMed] [Google Scholar]
- 17.Scatton O, Belghiti J, Dondero F, et al. Harvesting the middle hepatic vein with a right hepatectomy does not increase the risk for the donor. Liver Transpl. 2004;10:71–76. [DOI] [PubMed] [Google Scholar]
- 18.Farges O, Belghiti J, Kianmanesh R, et al. Portal vein embolization before right hepatectomy: prospective clinical trial. Ann Surg. 2003;237:208–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kianmanesh R, Farges O, Abdalla EK, et al. Right portal vein ligation: a new planned two-step all-surgical approach for complete resection of primary gastrointestinal tumors with multiple bilateral liver metastases. J Am Coll Surg. 2003;197:164–170. [DOI] [PubMed] [Google Scholar]
- 20.Kokudo N, Imamura H, Sano K, et al. Ultrasonically assisted retrohepatic dissection for a liver hanging maneuver. Ann Surg. 2005;242:651–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamamoto H, Nagino M, Kamiya J, et al. Surgical treatment for colorectal liver metastases involving the paracaval portion of the caudate lobe. Surgery. 2005;137:26–32. [DOI] [PubMed] [Google Scholar]
- 22.Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 2004;240:644–657. [DOI] [PMC free article] [PubMed] [Google Scholar]


