The management of acute gallstone pancreatitis can be quite different depending on who is taking care of the patient. Many surgeons tend to watch expectantly and perform cholecystectomy with intraoperative cholangiogram at a variable interval, usually on the same hospital admission, while our gastroenterology colleagues will often do an endoscopic retrograde cholangiopancreatography (ERCP) early in the clinical course.1–3 It should be mentioned, however, that often this ERCP is done at the request of the surgeon who wants the bile duct cleared preoperatively as he/she is not too excited about a positive intraoperative cholangiogram being an indication for possible laparoscopic common duct exploration. Despite many available training courses and the prepackaged laparoscopic CBD exploration kits available in the OR, the truth is that few surgeons are doing laparoscopic common duct exploration.
The existing randomized clinical trials addressing gallstone pancreatitis have been interpreted by some to support early ERCP in gallstone pancreatitis even though close inspection of these studies demonstrates no proven benefit in the absence of cholangitis.4–6 Although these trials address important aspects of this problem, each suffers some lack or problem that leaves the door open to speculation on the issue of usefulness and safety of ERCP for routine gallstone pancreatitis with preoperative evidence of biliary obstruction in the absence of cholangitis. These issues explain the appeal of the preoperative ERCP to treat potential choledocholithiasis and ameliorate gallstone pancreatitis prior to surgery. Oria et al7 have provided us with an excellent randomized clinical trial addressing this issue. They have carefully delineated the issues of pancreatitis, biliopancreatic obstruction, and cholangitis to clearly address the usefulness of ERCP in the absence of acute cholangitis.
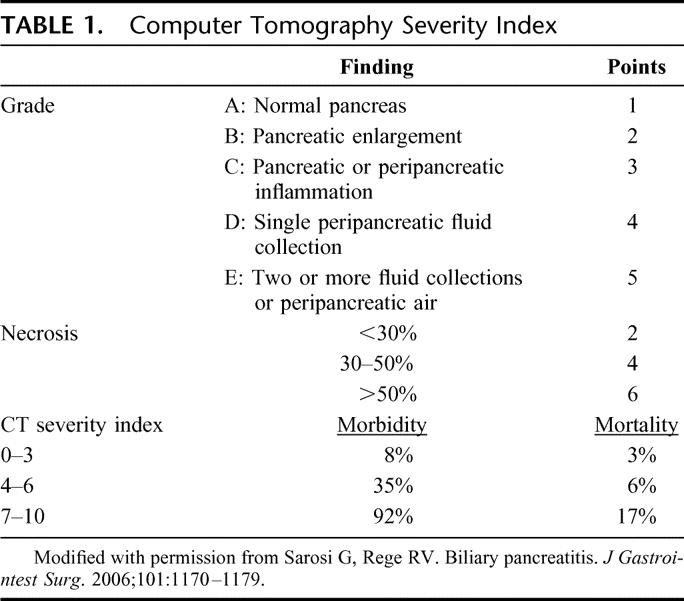
There are 3 generally accepted assessment scales used to evaluate the severity of pancreatitis attacks: Ranson’s criteria, Glasgow Pancreatitis Severity Score, and the Computer Tomography Severity Index.8–10 The Apache II scoring system has been used as well in pancreatitis patients but is not specific to pancreatitis and has not been generally adopted in the assessment for these therapeutic decisions. One of the problems with the prior randomized trials is that their assessment of severity of the pancreatitis attack is based on Ranson’s Criteria or the Glasgow Pancreatitis Severity Scale, both of which have criteria that are not assessed until 48 hours postadmission. The benefits of early ERCP in these prospective studies are limited to the cases with severe pancreatitis and that cannot be determined at admission using these criteria. Acosta et al,11 in a prospective randomized trial, have shown that the period of time during which disobstruction of the ampulla may be effective is probably very short and not longer than 48 hours from the onset of symptoms. The current study used the CT Severity Index, which can be assessed on admission and may be a better tool for determining necessity of early ERCP in acute gallstone pancreatitis (Table 1).
TABLE 1. Computer Tomography Severity Index
Among the other randomized trials done, 2 single-institution trials showed reduced morbidity, but only in patients predicted to have severe pancreatitis.4,5 The third study, which was a multicenter European trial, showed no benefit with early ERCP and actually demonstrated an increase in severe complications with an early endoscopic approach.6 Close analysis of these apparent conflicting results reveals that the trials demonstrating reduced morbidity with ERCP had patients with biliary obstruction included, while the other trial excluded jaundiced patients. Thus, the optimal treatment of patients with gallstone pancreatitis who have evidence of biliary obstruction was thought to be early ERCP. The current authors have determined that many of the patients included in those earlier studies had cholangitis. If those patients are excluded, then the results may not hold true. Indeed, the current study, which excluded cholangitis and also excluded patients without evidence of biliopancreatic obstruction, demonstrates no benefit to early ERCP in the resolution or stabilization of the acute pancreatitis. Thus patients with acute gallstone pancreatitis, even when the pancreatitis is severe, do not need early ERCP unless associated cholangitis is present. The downside to early ERCP is the risk of worsening the pancreatitis with the contrast injection, causing clinically significant bleeding in a critically ill patient, and the possibility of inducing cholangitis or cholecystitis.6,12 These factors and risks must be considered in each individual case when making the decision to proceed with early ERCP in the face of severe pancreatitis.
The Achilles heel in this process is the difficulty in excluding the diagnosis of cholangitis when you have a sick patient with elevated white blood count and fever due to pancreatitis. If there is jaundice or radiologic evidence of biliary obstruction, cholangitis may exist but be hidden by the accompanying symptoms of severe pancreatitis. The authors identify this as an issue and comment that Charcot triad may be insufficient to definitively diagnose cholangitis in this setting. Certainly, if in doubt, and cholangitis may be coexistent, early endoscopic sphincterotomy may indeed be warranted.
In my current practice, the patient with mild gallstone pancreatitis with a resolving enzyme pattern and decreasing bilirubin gets a delayed cholecystectomy and cholangiogram without ERCP. The patient with rapidly worsening pancreatitis and associated jaundice gets an ERCP, particularly if the bilirubin is rising. The clarity of this study will prompt me to carefully analyze laboratory values and clinical presentation to find some evidence of cholangitis in this latter group before proceeding with an ERCP.
Footnotes
Reprints: Gary C. Vitale, MD, Department of Surgery, School of Medicine, University of Louisville, Louisville, KY 40292. E-mail: gcvita01@earthlink.net.
REFERENCES
- 1.Stone HH, Fabian TC, Dunlop WE. Gallstone pancreatitis biliary tract pathology in relation to time of operation. Ann Surg. 1981;194:305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelly TR, Wagner DS. Gallstone pancreatitis: a prospective randomized trial of the timing of surgery. Surgery. 1988;104:600–605. [PubMed] [Google Scholar]
- 3.Nowak A, Marek TA, Nowakowska-Dulawa E, et al. Biliary pancreatitis need endoscopic retrograde cholangiopancreatography with endoscopic sphincterotomy for cure. 1998;30(suppl 2):256–259. [DOI] [PubMed] [Google Scholar]
- 4.Neoptolemos JP, Carr-Locke DL, London NJ, et al. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet. 1988;2:979–983. [DOI] [PubMed] [Google Scholar]
- 5.Fan ST, Lai EC, Mok FP, et al. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. N Engl J Med. 1993;328:228–232. [DOI] [PubMed] [Google Scholar]
- 6.Folsch UR, Nitsche R, Ludtke R, et al. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis: the German Study Group on Acute Biliary Pancreatitis. N Engl J Med. 1997;336:237–242. [DOI] [PubMed] [Google Scholar]
- 7.Oria A, Alvarez J, Chiappetta L, et al. Choledocholithiasis in acute gallstone pancreatitis: incidence and clinical significance. Arch Surg. 1991;126:566–568. [DOI] [PubMed] [Google Scholar]
- 8.Ranson JH, Rifkind KM, Roses DF, et al. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet. 1974;139:69–81. [PubMed] [Google Scholar]
- 9.Imrie CW, Benjamin IS, Ferguson JC, et al. A single-centre double-blind trial of Trasylol therapy in primary acute pancreatitis. Br J Surg. 1978;65:337–341. [DOI] [PubMed] [Google Scholar]
- 10.Balthazar EJ, Robinson DL, Megibow AJ, et al. Acute pancreatitis: value of CT. Radiology. 1985;174:331–336. [DOI] [PubMed] [Google Scholar]
- 11.Acosta JM, Katkhouda N, Debian KA, et al. Early ductal decompression versus conservative management for gallstone pancreatitis with ampullary obstruction: a prospective randomized clinical trial. Ann Surg. 2006;243:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sees DW, Martin RR. Comparison of preoperative endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy with operative management of gallstone pancreatitis. Am J Surg. 1997;174:719–722. [DOI] [PubMed] [Google Scholar]


