Abstract
Murine polyoma virus (MPyV) is a small DNA virus that induces tumors in multiple tissues of infected host. In this investigation, we show that cell lines derived from wild type virus-induced breast tumors are resistant to the growth inhibitory action of interferon β (IFN-β). Furthermore, replication of heterologous viruses such as vesicular stomatitis virus and encephalomyocarditis virus was not inhibited by IFN-β in these cells. This effect was due to inhibition of IFN-stimulated gene expression by viral T antigen. Activation of IFN-stimulated gene factor 3 was inhibited in cells derived from a tumor induced by wild-type MPyV but not those from a mutant that lacks the pRB binding site of the large T antigen. Similarly IFN-γ-inducible gene expression was also inhibited in cells transformed by wild-type virus. The levels of components of IFN-stimulated gene factor 3 and signal transducing Janus tyrosine kinases were comparable between the cells transformed by the wild-type and mutant viruses. The viral large T antigen bound to Janus tyrosine kinase 1 and inactivated signaling through IFN receptors. Thus, these studies identify a mechanism of viral resistance to IFN action.
Keywords: antiviral response, anti-growth response, cytokines, viral inhibition
Interferons (IFNs) are multifunctional cytokines that inhibit virus replication, tumor cell growth, and modulate host immunological functions (1). A number of IFN-stimulated genes (ISGs) have been shown to mediate the pleiotropic effects of IFNs (2). Binding of IFN-α/β to their multisubunit receptor initiates the tyrosine phosphorylation of Janus kinases Tyk2 and JAK1 and the receptor (3, 4). Subsequently, two cytoplasmic signal transducing activators of transcription (STAT) proteins, STAT1 and STAT2, are phosphorylated at specific tyrosine residues leading to their nuclear translocation. These then associate with a 48-kDa DNA binding protein (p48 or ISGF3γ) to form the active complex, ISGF3, and induce transcription of genes that contain the IFN-stimulated response element (ISRE). Similarly, binding of IFN-γ to its receptor stimulates the tyrosine phosphorylation of Janus kinases JAK1 and JAK2, which then phosphorylate STAT1 but not STAT2 (3). Activated STAT1 migrates to cell nucleus, binds to γ-IFN activated site to induce gene expression. Thus, JAK1 and STAT1 are the common components of IFN signal transduction pathway. Two major pathways activated by IFNs are thought to inhibit cellular or viral growth (1, 2). The first involves an endoribonuclease, RNaseL, which upon activation by the products of IFN-stimulated 2′,5′-oligoadenylate synthetases (5) cleaves cellular and viral mRNAs to inhibit growth. The second includes a protein kinase, protein kinase R, that phosphorylates the eukaryotic protein synthesis initiation factor 2α leading to cessation of protein synthesis (6). Down-regulation of Myc (7), up-regulation (8), and hypophosphorylation (9) of pRB occur during growth inhibition by IFNs in certain tumor cells. Thus, biochemical pathways necessary for both viral and cellular growth are inhibited by IFNs.
Murine polyoma virus (MPyV) is a small DNA virus that under permissive conditions replicates in cells leading to the propagation of viral progeny (10). Alternatively, it transforms host cells under nonpermissive conditions. As a result of its strong oncogenic potential in multiple tissues, this virus serves as a good model for understanding the mechanisms of carcinogenesis. The 5-kb genome of MPyV encodes viral structural proteins VP1, VP2, and VP3, and an early gene that encodes the large (LT), middle (MT), and small (ST) T antigens (10). LT and MT are essential for virus replication and cellular transformation. The role of ST is unclear at present. LT stimulates viral DNA replication, transcription, and immortalization of primary cells by binding to retinoblastoma (Rb) tumor suppressor protein (11, 12). Mutation of Rb-binding site results in a crippled virus that fails to replicate in primary cells. MT interferes with cellular signaling machinery to initiate mitogen-independent cell division (10, 13, 14). This inner membrane-anchoring protein is tyrosine phosphorylated at positions 250, 315, and 322, each of which is capable of associating with a distinct signaling molecule involved in cellular proliferation (10, 13, 14). Hence, T antigens play a crucial role in subverting cellular pathways. Previous studies with viral mutants have shown that wild-type (PTA) MPyV but not a mutant that lacks the pRb binding site of LT gene (RB1) is capable of inducing tumor formation with high frequencies in kidneys and thymus of newborn C3H/BiDa mice (11). Another difference between the mutant and wild-type MPyV is the relative delay in the onset of death of infected mice due to tumor burden. Mice infected by wild type are moribund much earlier than those infected with mutant (11). These observations indicate that the mutant virus is less capable of counteracting host defenses against viral replication. One such primary host defense is the production of IFN that inhibits viral replication and tumor growth (1, 2). Therefore, reduction of tumorigenicity of the mutant virus may be in part due to its inability to counteract the effects of IFNs.
DNA viruses are relatively resistant to the inhibitory actions of IFNs (2). We have chosen MPyV as a model to understand the mechanisms of IFN resistance, because this virus induces a variety of tumors in the infected host. The strong oncogenic potential of MPyV in vivo may include the ablation of growth suppressive signals emanating from the host. In this study, we have examined the antiviral and antitumor activities of IFNs in MPyV-transformed cells. We show that LT inhibits cellular responses to IFNs. Expression of ISGs is inhibited in cells transformed by wild type but not by a mutant that lacks the pRb binding site. LT binds to JAK1 and renders it inactive.
MATERIALS AND METHODS
Cells, Viruses, Plasmids and Antibodies.
PTA and RB1 cell lines were derived from breast carcinoma tumors in C3H/BiDa mice induced by MPyV wild type and a mutant that fails to bind pRb (11). These cells did not produce virus but expressed T antigens. Human JAK1 mutant cell line U4A has been described (15). Cells were maintained in DMEM supplemented with 10% fetal bovine serum. Vesicular stomatitis virus (VSV), New Jersey serotype, and encephalomyocarditis virus were used for antiviral studies. Murine IFN-β (Toray Industries, Tokyo) and murine and human IFN-γ (Boehringer Mannheim) were employed. Wild-type JAK1 and kinase-negative JAK1(JAK1-KE) cDNAs cloned in mammalian expression vector pRK5 were reported (4, 16). ISG 561-luciferase, ISG 6-16-CAT, palindromic IFN response element (pIRE)-luciferase and GBP-CAT were described earlier (17, 18). LT cDNA in a retroviral expression vector (19) and murine 2′,5′-oligoadenylate synthetase, and protein kinase R cDNAs were described elsewhere (6, 20). mAb specific for STAT1 and rabbit polyclonal antibodies against p48, STAT2, JAK1, and JAK2 were from Santa Cruz Biotechnology. mAbs against Tyk2 and JAK1 were from Transduction Laboratories. mAb specific for LT, MT, and ST was described (21).
Cell Growth and Antiviral Assays.
Cell growth inhibition assays were performed as described (22). Antiviral assays were performed as described (23) with the following modifications. At the end of the assay the surviving cells were stained with sulforhodamine B and the bound dye was quantitated in a microplate reader at 570 nm. Increase in A570 with IFN treatment as compared with untreated but virus-infected cells was taken as cell protective effect of IFN-β.
Gene Expression Analyses.
Northern blots and reporter gene (CAT and luciferase) assays were performed as described earlier (23, 24). Reporter gene activities were normalized to cotransfected β-actin-β-galactosidase gene. Total amount of DNA transfected in the parallel controls was kept constant by adding the pRK5 expression vector, wheras multiple plasmids were cotransfected. Electrophoretic mobility shift assays (EMSA) with 32P-labeled ISRE or pIRE probes were performed as described (24). Immunoprecipitation and Western blot analyses were performed as described (25).
RESULTS
IFN-β Fails to Activate Biological Responses in MPyV-Transformed Cells.
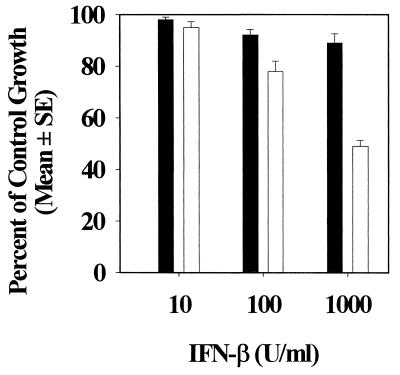
Because the RB1 mutant failed to induce tumors in certain tissues and a clear delay in the onset of death was observed compared with wild-type MPyV infected mice (11), we hypothesized that the mutant virus failed to counteract host-produced IFN. Therefore, we first examined the effect of murine IFN-β on the growth of breast carcinoma cells transformed by MPyV. Two cell lines PTA and RB1 derived from breast tumors induced by wild-type and mutant virus were employed to examine the cell growth inhibitory effects of IFN-β. Cells were incubated with various doses of IFN-β (10–1000 units/ml) for 5 days and examined for growth arrest. As shown in Fig. 1, IFN-β failed to inhibit growth of PTA cells at all doses tested. However, RB1 was readily inhibited by IFN-β in a dose-dependent manner (Fig. 1). Similar results were also obtained with two other cell lines that were derived from different mice infected with wild-type or mutant viruses (data not shown). Thus, the IFN resistance in PTA cells may not be a clonal effect.
Figure 1.
Growth inhibitory effect of IFN-β in MPyV-transformed PTA (▪) and RB1 (□) cells. Cells (2 × 103 per well) in 96-well microplate were exposed to indicated doses of murine IFN-β for 5 days. At the end of the experiment, the cells were stained with sulforhodamine B and the growth was monitored by using a colorimetric assay (22). Growth of the treated cells were expressed as a percentage of growth of untreated cells. Bar = mean ± SEM of quadruplicate measurements.
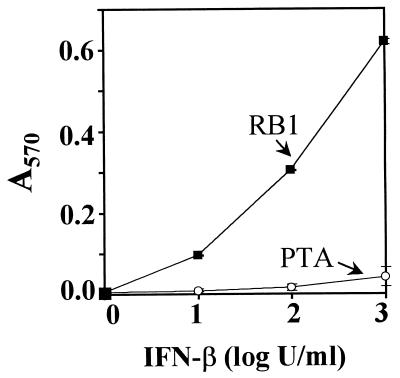
We then examined whether such difference existed in the antiviral responses of PTA and RB1 cells upon IFN-β treatment. Cells were treated with various doses of IFN-β for 16 h followed by an infection with 10 multiplicity of infection of VSV or encephalomyocarditis virus. Forty hours later cells were stained with sulforhodamine B and cell protection was quantitated by using the colorimetric assay described in Fig. 1. IFN-β failed to protect PTA cells against the challenge of VSV (Fig. 2) or encephalomyocarditis virus (data not shown). However, a dose-dependent protection of RB1 cells against VSV infection by IFN-β was noted. Thus, IFN-β failed to exert two of its biological actions in PTA cells.
Figure 2.
Antiviral action of IFN-β in PTA and RB1 cells. Cells (5 × 104) were exposed to IFN-β as indicated for 16 h. They were then challenged with 10 multiplicity of infection of VSV and monitored for cell protection by using the colorimetric assay described in Fig. 1. Increase in A570 indicates the protective effect of IFN-β. Mock-infected and virus-infected cells served as controls in these experiments.
ISG Expression in MPyV-Transformed Cells.
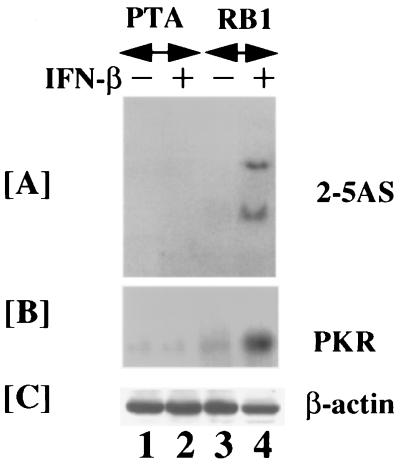
To test whether loss of IFN responses correlated with a failure of ISG expression Northern blot analyses were performed. Total RNA from untreated and IFN-β treated PTA and RB1 cells was prepared, analyzed by Northern blot, and hybridized to gene specific probes corresponding to murine 2′,5′oligoadenylate sythetase or protein kinase R. Neither of these genes was induced by IFN-β in PTA cells. Contrary to this, these mRNAs were readily induced in RB1 cells (Fig. 3). Consistent with the presence of multiple 2′,5′-oligoadenylate sythetase gene products (20), at least two species of 2′,5′-oligoadenylate sythetase mRNAs were induced in these cells. Expression of β-actin mRNA was similar in both the cells. Thus, a global transcriptional block was not responsible for the failure of ISG induction.
Figure 3.
Expression of ISG mRNAs. Cells were exposed to IFN-β (150 units/ml) for 6 h. Total RNA (30 μg) was Northern blotted and probed with indicated 32P-labeled ISG cDNAs (23). “−” and “+” indicate no treatment and IFN treatment, respectively.
Transcriptional inhibition of ISG expression was also studied by using reporter genes regulated by enhancers of several ISGs. Expression of chloramphenicol acetyltransferase (CAT) and luciferase reporters driven by the ISG 6–16 and ISG 561 promoters was not stimulated by IFN-β in PTA cells in transfection assays. However, these reporters were strongly induced in RB1 cells upon IFN-β treatment (Fig. 4 A and B). Expression of β-actin promoter-driven CAT was comparable in these cells (data not presented). We also examined whether IFN-γ-stimulated gene expression was affected similarly. IFN-γ-induced expression of guanylate binding protein gene promoter-driven CAT and a pIRE-regulated luciferase gene was not observed in PTA cells. However, a strong induction of these reporters was observed in RB1 cells (Fig. 4 C and D). Thus, IFN-β and IFN-γ inducible gene expression was blocked in cells transformed by wild-type MPyV.
Figure 4.
Induction of transfected ISG promoter driven reporter genes by IFNs. Cells (5 × 105) in A and B were electroporated with 10 μg of ISG 561-luciferase and ISG 6-16-CAT respectively. IFN-β (150 units/ml) treatment was performed for 18 h. Luciferase and CAT assays were performed by using cell extracts (60 μg) as described. Transfection efficiency was monitored by measuring the expression of cotransfected β-actin-β-galactosidase (3 μg). Experiments in C and D are similar to A and B except that IFN-γ-inducible pIRE-Luciferase and guanylate binding protein-CAT reporter genes were used, respectively. Cells were treated with murine IFN-γ (150 U/ml) for 18 h before the assays.
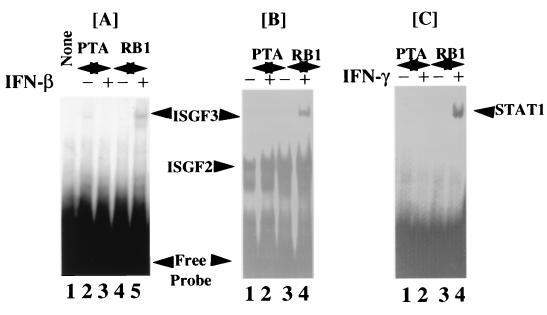
Inhibition of IFN-Activated DNA Binding of Transcription Factors.
Because ISG expression is dependent on specific transcription factors (3), IFN-activated DNA binding of transactivating factors was examined in PTA and RB1 cells. Two types of IFN responsive elements, ISRE (23) and pIRE (18), were employed as probes for detection of transcription factor binding in EMSA. Cytoplasmic and nuclear extracts were prepared after stimulation of PTA and RB1 cells (Fig. 5A). They were then incubated with 32P-labeled probes in EMSA. IFN-activated binding of ISGF3 was not detected in PTA cytoplasmic extracts before or after IFN-β treatment (Fig. 5A, lanes 2 and 3). In RB1 cells ISGF3 was rapidly induced (Fig. 5A, lanes 4 and 5). EMSA with nuclear extracts also yielded similar results. In the nuclear extracts, two factors bound to ISRE constitutively (Fig. 5B). One of these was ISGF2 (IFN-regulatory factor 1) as detected by specific antibodies (data not presented). An inducible factor, ISGF-3 was formed with IFN-β-stimulated RB1 nuclear extracts but not with those from PTA cells (Fig. 5B compare lanes 4, 2). The identity of this factor as ISGF3 was established by inhibition of formation of the complex upon preincubation of the extracts with specific antibodies against p48 and STAT1 (data not shown). EMSA was also performed with IFN-γ-stimulated nuclear extracts and labeled pIRE as a probe. Binding of STAT1 to pIRE was not observed with nuclear extracts from untreated cells (Fig. 5C, lanes 1 and 3). IFN-γ robustly induced the binding of STAT1 to pIRE in RB1 cells but not in PTA cells (Fig. 5C, compare lanes 4 and 2). These results suggest that lack of ISG expression may be due to a failure to activate IFN-stimulated transcription factors (3, 4) in PTA cells. However, no differences were noted in the levels of IFN-γ receptor chains, STAT or JAK kinases between PTA and RB1 cells. Further, no detectable tyrosine phosphorylation of STAT1 was seen in PTA cells at low doses of IFN used (data not shown). High doses of IFN-γ (1,500 units/ml) activated STAT1 binding to DNA in PTA, lower than that observed in RB1 cells, indicating that IFN was able to partially over come the inhibition. There was also no significant difference in the levels of T antigens in PTA and RB1 cells (data not shown).
Figure 5.
IFN activated DNA binding of transcription factors. Cells were treated with indicated IFNs (150 units/ml) for 30 min and EMSA was performed with 32P-labeled ISRE (A and B) or pIRE (C). In A and B cytoplasmic and nuclear extracts (4 μg) from the same cells were used. None, no extract. “−” and “+” signs are similar to Fig. 2. Positions of specific complexes were indicated. In C nuclear extracts (3 μg) were used for EMSA.
LT Binds to JAK1.
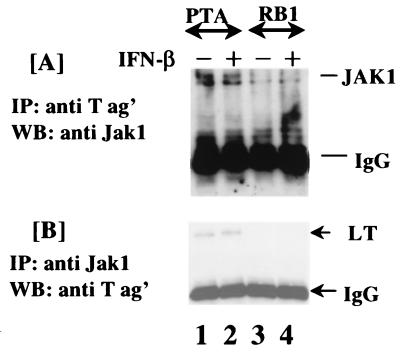
Because there were no obvious changes in the levels of components of IFN signal transduction pathway and of the T antigens, we tested whether inhibition of ISG expression was due to a selective binding of STAT1 or JAK1 by the T antigens. Immunoprecipitation analyses with a mAb that detects all the T antigens revealed no association of STAT1 and JAK2 in PTA and RB1 cells (data not shown). However, JAK1 was coimmunoprecipitated by an antibody against T antigen in PTA but not in RB1 cells (Fig. 6A). Western blot analysis of T antigen immunoprecipitates identified a 130 kDa protein by a mAb against JAK1. IFN-β treatment had no significant effect on the binding of JAK1 to T antigen (lanes 1, 2). However, not all the JAK1 was bound by LT quantitatively. Contrary to this, JAK1 did not immunoprecipitate along with T antigen in RB1 cells (Fig. 6A, lanes 3, 4). Because JAK1 was coimmunoprecipitated with T antigens, we next determined which of the T antigens interacted with JAK1. Cell extracts were immunoprecipitated with anti-JAK1 antibody followed by Western blot analysis with antibody against T antigen. These assays revealed that LT coprecipitates with JAK1 in PTA (Fig. 6A, lanes 1 and 2) but not in RB1 cells (Fig. 6A, lanes 3 and 4). MT, and ΔLT were not observed in these immunoprecipitates (Fig. 6B). All these lanes expressed similar levels of JAK1 (data not shown). Thus, JAK1 and LT appeared to interact with each other. Quantitatively, all the LT in the extracts was not immunoprecipitated by JAK1. The LT:JAK1 immunoprecipitates had no detectable kinase activity (data not presented).
Figure 6.
Coprecipitation of JAK1 with LT. Cell extracts (300 μg) were immunoprecipitated with indicated antibodies and then probed with specific antibodies in Western blot analyses (shown on left). Positions of JAK1, LT, and IgG are identified. All the lanes had equal amounts of T antigen or JAK1 (not shown).
Overexpression of JAK1 Restores IFN Responses.
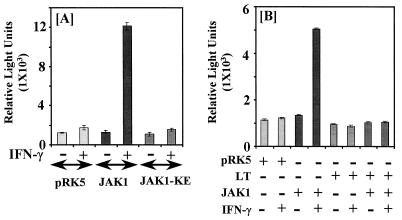
Because the above results indicated loss of IFN-responses and an interaction between LT and JAK1 in PTA cells, we next examined whether overexpression of JAK1 would restore IFN-γ responses in PTA cells (Fig. 7A). Cells were transfected with pIRE-luciferase vector along with a control (pRK5) or JAK1 expression vector (16). Cotransfection of expression vector alone followed by IFN-γ treatment did not significantly induce luciferase gene expression (Fig. 7A, bars 1, 2). Introduction of JAK1 expression vector conferred a strong IFN-γ inducibility to the reporter gene (Fig. 7A, bars 3 and 4). In a similar experiment, cotransfection of JAK1-KE (a mutant that lacks kinase activity) failed to restore IFN-γ responses (Fig. 7A, bars 5 and 6). Thus, JAK1 appeared to be a target of T antigen mediated inhibition. Under the same conditions, JAK1 caused only a marginal elevation of reporter expression in IFN-treated RB1 cells that was not significantly different from that of untransfected cells (data not shown).
Figure 7.
Overexpression of JAK1 restores IFN-γ stimulated gene expression (A). PTA cells (5 × 105) were electroporated with pIRE-luciferase (10 μg) and 5 μg of indicated expression vector. They were then treated with murine IFN-γ (150 units/ml) for 18 h prior to luciferase assay with equal amount of cell extracts (70 μg). Bars = mean luciferase activity ± SEM of triplicate samples. pRK5, expression vector alone; JAK1, pRK5 with wild-type JAK1 cDNA; JAK1-KE, pRK5 with a mutant JAK1 cDNA that lacks kinase activity. LT inhibits JAK1 function (B) U4A cells were transfected with pIRE-luciferase (8 μg) and indicated expression vector (4 μg). Total amount of DNA (12 μg) transfected was kept constant by adding pRK5 where necessary. Luciferase assay was performed as in panel A except that cells were treated with human IFN-γ (150 U/ml). “+” and “−” indicate presence or absence of the plasmid in transfection mixture, respectively. In the case of IFN-γ they indicate treatment or nontreatment, respectively.
To further examine the effect of LT on JAK1, expression vectors carrying LT or JAK1 introduced into U4A (15), a mutant human cell line that lacked endogenous JAK1 (Fig. 7B). Transfection of control vector pRK5 followed by IFN-γ treatment did not induce pIRE luciferase activity (Fig. 7B, bars 1 and 2). Cotransfection of JAK1 expression vector restored IFN-inducibility in this cell line (Fig. 7B, bars 3 and 4). These results are consistent with previous studies in this cell line (15). LT alone had no effect on the reporter and IFN-γ treatment did not induce gene expression (bars 5, 6). Cotransfection of LT along with JAK1 clearly suppressed the IFN inducibility of the luciferase reporter (Fig. 7B, bars 7 and 8). Thus, LT counteracted ligand activated JAK1 action. Under these conditions cotransfection of a MT expression vector had no effect on gene expression (data not shown).
DISCUSSION
Successful establishment of transformed state by oncogenic viruses is dependent on their ability to inhibit host pathways that impose constraints on their replication (1, 2). For example, the adenovirus E1A and hepatitis B viral terminal protein interfere with the activation of ISGF3 by reducing levels of p48 and STAT1 (23, 26–29). Inhibition of CREB binding protein (CBP) interaction with STAT2 protein could partly account for a loss of IFN responses in E1A expressing cells (30). However, a recent study showed that ablated IFN responses could be restored to normalcy upon overexpression of p48 in E1A-transformed cells (31). Thus, reduction in the physical levels of transcription factors and their interaction with coactivators such as CBP may inhibit IFN responses in E1A-transformed cells. Epstein–Barr viral nuclear antigen-2 also suppresses IFN action (32). Certain large DNA viruses such as Kaposi sarcoma-associated herpes virus (KSHV) and pox virus and myxoma virus encode IFN-regulatory factor-like transcription factors or IFN receptor analogs for inhibiting the antiviral actions (33–36). Other viruses employ inhibitors of protein kinase R and RNaseL to evade IFN action (2). These mechanisms may not only permit unabated viral replication but also play a crucial role in establishing persistent infection or cellular transformation. The strong oncogenic potential of MPyV (10) may include not only a subversion of growth promoting pathways but also an inhibition of growth suppressive mechanisms. In this investigation we have shown that antiviral and antitumor actions of IFN-β was inhibited in cells transformed by wild-type MPyV. Although there was no significant change in the levels of IFN receptor or signaling components, both IFN-β- and IFN-γ-inducible gene expression was not observed. Therefore, a component common for both these signaling pathways was dysfunctional in the MPyV-transformed cells. Indeed, overexpression of JAK1 restored IFN-stimulated gene expression in PTA cells (Fig. 7A). Additionally, in a mutant cell line that lacked JAK1, transient coexpression of JAK1 restored the IFN-γ response that was suppressed by LT alone (Fig. 7B). Consistent with these observations, JAK1 coimmunoprecipitated with LT. Such interaction did not occur with a LT that harbored a mutation in the pRb binding site. Therefore, JAK1:LT interaction may in part account for the observed inhibition of IFN responses. Our studies do not rule out a possibility that LT induces cellular inhibitor(s) of JAK1, because all the JAK1 in the cells is not quantitatively bound by LT. These observations also suggest that a balance between the levels of LT or JAK1 determine the resistant or responsive states of the host cell. Thus, our studies identified a novel inhibitory mechanism of IFN signals. More importantly, they reflect a natural phenomenon because PTA cells were derived from the tumors that arose from virus infection in vivo rather than by an in vitro selection of cells that overexpressed viral proteins.
In PTA and RB1 cells, in addition to the full length LT, a truncated LT that represents the N-terminal region of LT is also present (12). Full length LT contains the oligomerization and pRb binding domains (10, 37) but the truncated one lacks the oligomerization domain (12). Curiously, in the immunoprecipitates full length LT but not the truncated one is seen. These observations suggest that the oligomerization domain of LT is important for interaction with JAK1. LT oligomerization may permit the formation of a pseudo-structure that serves as a JAK1 binding interface. Such structure may be reminiscent of JAK binding sites of cytokine receptors, wherein multiple receptor subunits interact with JAK1 (4). However, there is no discernible homology between cytokine receptors and the LT. Interestingly, mutation in pRb binding site (N-terminal) inhibits anti-IFN activity. It is likely that this mutation induces a conformational change that disrupts the formation of JAK1 interacting surface. IFNs also induce hypophosphorylation of Rb (9), leading to cellular growth arrest. Binding of Rb by LT (10, 11) also prevents its participation in IFN-initiated growth suppression. Simultaneous disarming of cell growth control by ablation of Rb function and IFN action by suppressing JAK1 activity by LT may reflect the versatility of small DNA viruses in dominating the cellular functions with a minimal number of proteins. Our results are also consistent with the observations that disruption of receptor function or JAK-STAT pathway results in a loss of tumor growth inhibitory properties of IFNs (38–41). What function, if any, does JAK1 perform in association with T antigen? Although JAKs function by associating with a number of cytokine or growth factor receptors in the cell membrane, recent studies show that JAKs are also present in the nucleus (42). These observations indicate a broader role for JAKs in the modulation of cellular functions. Because LT influences DNA synthesis and transcription in virus infected and transformed cells (10), its interaction with JAKs may permit the modulation factors involved in those processes.
Acknowledgments
We thank George Stark for U4A cells, James Ihle for wild-type and mutant JAK1 expression vectors, Bryan Williams for anti-STAT1 antibody, and Robert Schreiber for murine IFN-γ receptor specific antibodies.
Footnotes
This paper was submitted directly (Track II) to the Proceedings Office.
Abbreviations: IFN, interferon; JAK, Janus tyrosine kinase; MPyV, murine polyoma virus; ISG, IFN-stimulated gene; ISGF, ISG factor; ISRE, IFN-stimulated response element; VSV, vesicular stomatitis virus; STAT, signal transducing activator of transcription; pIRE, palindromic IFN-response element; LT, large T antigen; MT, middle T antigen; ST, small T antigen; Rb, retinoblastoma; CAT, chloramphenicol acetyltransferase; EMSA, electrophoretic mobility shift assay.
References
- 1.Kalvakolanu D V, Borden E C. Cancer Invest. 1996;14:25–53. doi: 10.3109/07357909609018435. [DOI] [PubMed] [Google Scholar]
- 2.Vilcek J, Sen G C. In: Fields Virology. Fields B N, Knipe D M, editors. New York: Raven; 1994. pp. 375–399. [Google Scholar]
- 3.Darnell J E, Jr, Kerr I M, Stark G R. Science. 1994;264:1415–1421. doi: 10.1126/science.8197455. [DOI] [PubMed] [Google Scholar]
- 4.Ihle J N. Adv Cancer Res. 1996;68:23–65. doi: 10.1016/s0065-230x(08)60351-6. [DOI] [PubMed] [Google Scholar]
- 5.Zhou A, Hassel B A, Silverman R H. Cell. 1993;72:753–765. doi: 10.1016/0092-8674(93)90403-d. [DOI] [PubMed] [Google Scholar]
- 6.Meurs E, Chong K, Galabru J, Thomas N S, Kerr I M, Williams B R, Hovanessian A G. Cell. 1990;62:379–390. doi: 10.1016/0092-8674(90)90374-n. [DOI] [PubMed] [Google Scholar]
- 7.Kimchi A, Resnitzky D, Ber R, Gat G. Mol Cell Biol. 1988;8:2828–2836. doi: 10.1128/mcb.8.7.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar R, Atlas I. Proc Natl Acad Sci USA. 1992;89:6599–6603. doi: 10.1073/pnas.89.14.6599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Resnitzky D, Tiefenbrun N, Berissi H, Kimchi A. Proc Natl Acad Sci USA. 1992;89:402–406. doi: 10.1073/pnas.89.1.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fluck M M, Bertino J R, editors. Encyclopedia of Cancer. San Diego: Academic; 1997. pp. 1926–1939. [Google Scholar]
- 11.Freund R, Bronson R T, Benjamin T L. Oncogene. 1992;7:1979–1987. [PubMed] [Google Scholar]
- 12.Freund R, Bauer P H, Crissman H A, Bradbury E M, Benjamin T L. J Virol. 1994;68:7227–7234. doi: 10.1128/jvi.68.11.7227-7234.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Talmage D A, Freund R, Young A T, Dahl J, Dawe C J, Benjamin T L. Cell. 1989;59:55–65. doi: 10.1016/0092-8674(89)90869-6. [DOI] [PubMed] [Google Scholar]
- 14.Dahl J, Freund R, Blenis J, Benjamin T L. Mol Cell Biol. 1996;16:2728–2735. doi: 10.1128/mcb.16.6.2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muller M, Briscoe J, Laxton C, Guschin D, Ziemiecki A, Silvennoinen O, Harpur A G, Barbieri G, Witthuhn B A, Schindler C, Pellegrini S, Wilks A F, Ihle J N, Stark G R, Kerr I M. Nature (London) 1993;366:129–135. doi: 10.1038/366129a0. [DOI] [PubMed] [Google Scholar]
- 16.Briscoe J, Rogers N C, Witthuhn B A, Watling D, Harpur A G, Wilks A F, Stark G R, Ihle J N, Kerr I M. EMBO J. 1996;15:799–809. [PMC free article] [PubMed] [Google Scholar]
- 17.Bandyopadhyay S K, Leonard G T, Jr, Bandyopadhyay T, Stark G R, Sen G C. J Biol Chem. 1995;270:19624–19629. doi: 10.1074/jbc.270.33.19624. [DOI] [PubMed] [Google Scholar]
- 18.Kanno Y, Kozak C A, Schindler C, Driggers P H, Ennist D L, Gleason S L, Darnell J E, Jr, Ozato K. Mol Cell Biol. 1993;13:3951–3963. doi: 10.1128/mcb.13.7.3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cherington V, Morgan B, Spiegelman B M, Roberts T M. Proc Natl Acad Sci USA. 1986;83:4307–4311. doi: 10.1073/pnas.83.12.4307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghosh S K, Kusari J, Bandyopadhyay S K, Samanta H, Kumar R, Sen G C. J Biol Chem. 1991;266:15293–15299. [PubMed] [Google Scholar]
- 21.Pallas D C, Schley C, Mahoney M, Harlow E, Schaffhausen B S, Roberts T M. J Virol. 1986;60:1075–1084. doi: 10.1128/jvi.60.3.1075-1084.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skehan P, Storeng R, Scudiero D, Monks A, McMahon J, Vistica D, Warren J T, Bokesch H, Kenney S, Boyd M R. J Natl Cancer Inst. 1990;82:1107–1112. doi: 10.1093/jnci/82.13.1107. [DOI] [PubMed] [Google Scholar]
- 23.Kalvakolanu D V, Bandyopadhyay S K, Harter M L, Sen G C. Proc Natl Acad Sci USA. 1991;88:7459–7463. doi: 10.1073/pnas.88.17.7459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weihua X, Kolla V, Kalvakolanu D V. Proc Natl Acad Sci USA. 1997;94:103–108. doi: 10.1073/pnas.94.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ausubel F M, Brent R, Kingston R E, Moore D D, Seidman J G, Smith J A, Struhl K, editors. Current Protocols in Molecular Biology. New York: Wiley-Interscience; 1994. [Google Scholar]
- 26.Ackrill A M, Foster G R, Laxton C D, Flavell D M, Stark G R, Kerr I M. Nucleic Acids Res. 1991;19:4387–4393. doi: 10.1093/nar/19.16.4387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gutch M J, Reich N C. Proc Natl Acad Sci USA. 1991;88:7913–7917. doi: 10.1073/pnas.88.18.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leonard G T, Sen G C. Virology. 1996;224:25–33. doi: 10.1006/viro.1996.0503. [DOI] [PubMed] [Google Scholar]
- 29.Foster G R, Ackrill A M, Goldin R D, Kerr I M, Thomas H C, Stark G R. Proc Natl Acad Sci USA. 1991;88:2888–2892. doi: 10.1073/pnas.88.7.2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhattacharya S, Eckner R, Grossman S, Oldread E, Arany Z, D’Andrea A, Livingston D M. Nature (London) 1996;383:344–347. doi: 10.1038/383344a0. [DOI] [PubMed] [Google Scholar]
- 31.Leonard G T, Sen G C. J Virol. 1997;71:5095–5101. doi: 10.1128/jvi.71.7.5095-5101.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kanda K, Decker T, Aman P, Wahlstrom M, von Gabain A, Kallin B. Mol Cell Biol. 1992;12:4930–4936. doi: 10.1128/mcb.12.11.4930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore P S, Boshoff C, Weiss R A, Chang Y. Science. 1996;274:1739–1744. doi: 10.1126/science.274.5293.1739. [DOI] [PubMed] [Google Scholar]
- 34.Symons J A, Alcami A, Smith G L. Cell. 1995;81:551–560. doi: 10.1016/0092-8674(95)90076-4. [DOI] [PubMed] [Google Scholar]
- 35.Alcami A, Smith G L. J Virol. 1995;69:4633–4639. doi: 10.1128/jvi.69.8.4633-4639.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colamonici O, Domanski P, Sweitzer S M, Larner A, Buller R M L. J Biol Chem. 1995;270:15974–15978. doi: 10.1074/jbc.270.27.15974. [DOI] [PubMed] [Google Scholar]
- 37.Rose P E, Schaffhausen B S. J Virol. 1995;69:2842–2849. doi: 10.1128/jvi.69.5.2842-2849.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dighe A S, Richards E, Old L J, Schreiber R D. Immunity. 1994;1:447–456. doi: 10.1016/1074-7613(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 39.Chin Y E, Kitagawa M, Su W-C S, You Z-H, Iwamoto Y, Fu X-Y. Science. 1996;272:719–722. doi: 10.1126/science.272.5262.719. [DOI] [PubMed] [Google Scholar]
- 40.Bromberg J F, Horvath C M, Wen Z, Schreiber R D, Darnell J E., Jr Proc Natl Acad Sci USA. 1996;93:7673–7678. doi: 10.1073/pnas.93.15.7673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shuai K, Liao J, Song M M. Mol Cell Biol. 1996;16:4932–4941. doi: 10.1128/mcb.16.9.4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lobie P E, Ronsin B, Silvennoinen O, Haldosen L A, Norstedt G, Morel G. Endocrinology. 1996;137:4037–4045. doi: 10.1210/endo.137.9.8756581. [DOI] [PubMed] [Google Scholar]