Abstract and Introduction
Abstract
Listeria monocytogenes, although uncommon as a cause of illness in the general population, can result in serious illness when it affects pregnant women, neonates, the elderly, and immunocompromised individuals. Typically, it is a food-borne organism. This report describes a case of brain-stem listeriosis in a previously healthy 51-year-old woman. The diagnosis was based on clinical findings, the results of cerebrospinal fluid (CSF) analysis, CSF culture, and magnetic resonance imaging (MRI) findings. MRI demonstrated upper brain stem and cerebellar peduncle involvement. In addition, Tc-99m exametazime (HMPAO)-labeled single photon emission computed tomography (SPECT) of the brain revealed bilateral cerebellar hypoperfusion. Antibiotic therapy resulted in partial clinical recovery after 3 weeks. At the end of 6 months, brain-stem findings had nearly resolved. However, although minimal residual findings were observed on MRI at 6 months, bilateral diffuse cerebellar hypoperfusion remained on Tc-99m HMPAO brain SPECT.
Introduction
Listeriosis is a serious infection acquired by eating food contaminated with the bacterium Listeria monocytogenes. This bacterium may be found in a variety of raw foods, such as uncooked meats, vegetables, and dairy products made from unpasteurized milk. The organism is a facultative, non-spore-forming, gram-positive bacillus. The risk of a healthy person developing listeriosis after eating contaminated food is very low.[1]
Brain-stem encephalitis caused by L monocytogenes infection is a well-defined entity characterized by progressive brain-stem dysfunction. In humans, brain-stem encephalitis occurs in 10% of the listeriosis cases.[2] In autopsy series, it has been described as inflammatory infiltrates predominantly located in lower cranial nerves.[3]
We present this case because of its unique features, including development of symptomatic listeriosis in an immunocompetent patient, the involvement of upper and mid-brain-stem regions, and the findings in single photon emission computed tomography (SPECT) of the brain.
Case History
A healthy 51-year-old woman arrived in the emergency ward complaining of fatigue, vertigo, nausea, vomiting, and anorexia, and was diagnosed with influenza infection. The patient returned to the emergency ward 5 days later with complaints of disequilibrium and diplopia. A holiday trip to a rural region and the consumption of milk products 2 months previously were noted in her history.
Physical examination revealed temperature of 38°C and normal system examination findings. The neurologic examination findings included neck stiffness, defect in bilateral conjugated eye movements, cerebellar dysarthria, dysmetry, dysdiadokokinesia, and central facial paralysis with mild left hemiparesis (4/5). In addition, deep tendon reflexes were depressed and Babinski's sign was positive on the affected side.
Cerebrospinal fluid (CSF) exam demonstrated 270 leukocytes/mm3, 33 mg/dL glucose (with blood glucose levels at 144 mg/dL), 100 mg/dL protein, and 109 mmol/L chloride. Gram's stain of CSF showed no bacteria. The patient tested negative for cytomegalovirus IgG, anti-HIV, VDRL, Rose Bengal, acid-fast adenosine deaminase, Mycobacterium tuberculosis DNA (polymerase chain reaction), Epstein-Barr virus, IgG and IgM antibodies.
With these laboratory findings, a course of ampicillin 12g/day was prescribed as an empiric therapy. The second CSF examination, performed 2 days later, detected 1200 leukocytes/mm3, 11 mg/dL glucose, and 100 mg/dL protein. In the clinical microbiology laboratory, the second CSF sample was centrifuged and inoculated from sediment to general media (sheep blood 5%, chocolate agar, eozin methylene blue [EMB] agar, thioglycolate broth), and BACTEC 9050 hemoculture bottle (Becton, Dickinson and Company). After incubation for 2 days, no growth was seen on the general media, but CSF culture on hemoculture medium was positive. Gram-positive bacilli were visible on gram preparation from the hemoculture bottle. Bacteria were identified as L monocytogenes by the API Coryne system (bioMérieux). The strain was found to be susceptible to all of the antimicrobials tested, and gentamicin 300 mg/day was added to the therapy regimen.
Cerebral computed tomography (CT) was normal, but magnetic resonance imaging (MRI) revealed hypointense lesions and limited diffusion in the T1-weighted sequence, and in the T2 and fluid attenuated inversion recovery (FLAIR) sequences the lesions were hyperintense, beginning posteriorly at the level of the pons in the brain stem and extending to the level of the mesencephalon, partially including both cerebellar peduncles with no contrast enhancement (Figure 1). Bilateral cerebellar hypoperfusion was observed on the Tc-99m HMPAO SPECT of the brain performed during this period.
Figure 1.
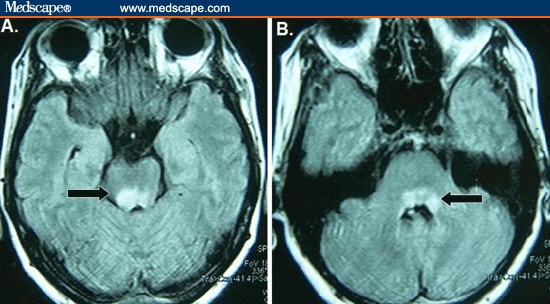
On initial MRI, FLAIR images reveal involvement of the mesencephelon (A), with lesions extending to the cerebellar peduncles at the level of the pons (B).
Antibiotic therapy was continued for 3 weeks. At the end of this period, mild left hemiparesis and cerebellar findings were observed and the patient's speech had become more understandable. At the end of 6 months, cerebellar dysfunction and bilateral disconjugated eye movements had almost resolved. Although MRI demonstrated minimal residual findings (Figure 2), Tc-99m HMPOA brain SPECT continued to show diffuse bilateral cerebellar hypoperfusion (Figure 3).
Figure 2.
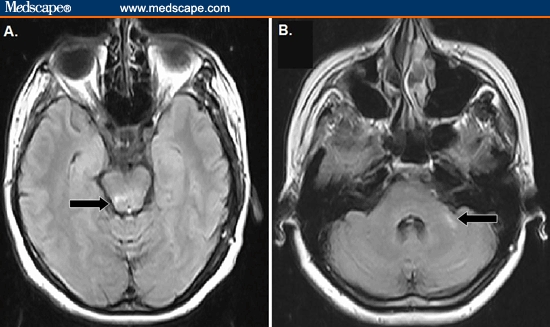
FLAIR images at 6-month follow-up reveal minimal involvement of the mesencephelon (A); lesion extending to just left of the cerebrallar peduncle in the pons level on cranial MRI (B).
Figure 3.
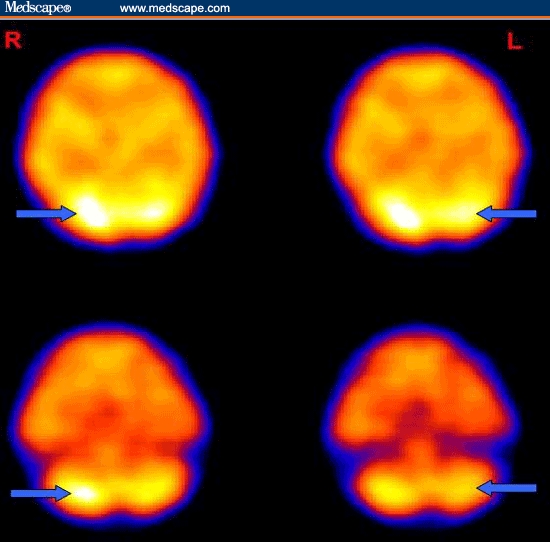
Tc-99 HMPAO brain SPECTs - initial (top) and at the end of 6 months –showing bilateral cerebellar hypoperfusion on a transverse slide (bottom).
Discussion
L monocytogenes infection (listeriosis) may cause bacteremia, endocarditis, and meningitis.[4] This food-borne pathogen, which affects the central nervous system (CNS), is most likely to cause illness in older adults and immunosuppressed patients.[5] Our patient was immunocompetent. The history of intense consumption of milk and milk products in a rural area 2 months prior to the onset of her illness indicated that the patient might have been infected by the bacteria during this time. The incubation period for L monocytogenes is usually 3–10 days[4]; however, the incubation period might have been longer in our patient. The influenza infection findings observed for 1 week before the onset of CNS symptoms may have represented a prodromal period.
L monocytogenes is difficult to identify clinically; thus, a culture is essential to making a definitive diagnosis.[4] In this particular case, centrifugation of CSF and inoculation in blood culture medium improved the recovery rate of the organism. L monocytogenes was isolated only in the second CSF sample.
Listeria rhombencephalitis results in considerably higher morbidity and a higher incidence of persistent neurologic impairment than simple meningitis.[6,7] Predominant involvement of the lower cranial nerves that innervate the oropharynx has been demonstrated both at autopsy and in clinical series.[3,8] Observations of bacteria within lower cranial nerves led to the hypothesis that food-borne L monocytogenes enters the brain stem through the neural pathways connecting the brain stem and the upper gastrointestinal tract. The involvement of the mid-pons and mesencephalon in our patient, and the fact that the lower brain stem was unaffected, are partly incompatible with this hypothesis.[2,3,9] Although MRI failed to show diffuse involvement of the cerebellum, the simultaneously performed brain Tc-99-HMPAO SPECT examination revealed diffuse symmetric cerebellar hypoperfusion. This finding might be interpreted as indicating that the infection caused capillary damage and reduced perfusion in the peduncular area.
A previous study found the Tc-99m HMPAO brain SPECT to be more sensitive and to provide better localization than CT or MRI in children with acute viral encephalitis. The investigators of that study suggested that the SPECT investigation may be more valuable than MRI for observation of capillary damage in the blood-brain barrier.[10,11]
We conclude that sequential SPECT studies in addition to MR imaging may facilitate understanding of the prognosis in cases of encephalitis.
Contributor Information
Sevki Sahin, Department of Neurology, Faculty of Medicine, Maltepe University, Istanbul, Turkey.
Ayse S. Arisoy, Department of Clinical Microbiology and Infectious Disease. Faculty of Medicine, Maltepe University, Istanbul, Turkey.
Aynur E. Topkaya, Department of Microbiology and Clinical Microbiology, Faculty of Medicine, Maltepe University, Istanbul, Turkey.
Sibel Karsidag, Department of Neurology, Faculty of Medicine, Maltepe University Istanbul, Turkey Author's Email: drsahin@gmail.com.
References
- 1.Schuchat A, Broome V. Infection caused by Listeria monocytogenes. In: Kasper DL, Braunwald E, Fauci AS, et al., editors. Harrison's Principles of Internal Medicine. 16th edition. New York, NY: McGraw-Hill; 2004. pp. 915–918. [Google Scholar]
- 2.Antal EA, Loberg EM, Bracht P, et al. Evidence for intraaxonal spread of Listeria monocytogenes from the periphery to the central nervous system. Brain Pathol. 2001;11:432–438. doi: 10.1111/j.1750-3639.2001.tb00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antal EA, Loberg EM, Dietrichs E, Meahlen J. Neuropathological findings in 9 cases of Listeria monocytogenes brain stem encephalitis. Brain Pathol. 2005;15:187–191. doi: 10.1111/j.1750-3639.2005.tb00519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hof H, Nichterlein T, Kretschmar M. Management of listeriosis. Clin Microbiol Rev. 1997;10:345–357. doi: 10.1128/cmr.10.2.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lever N, Haas L. Serial MRI in listeria mesenrhombencephalitis: a case report. J Neurol Neurosurg Psychiatry. 1995;59:524–527. doi: 10.1136/jnnp.59.5.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armstrong RW, Fung PC. Brainstem encephalitis (rhombencephalitis) due to Listeria monocytogenes: case report and review. Clin Infect Dis. 1993;16:689–702. doi: 10.1093/clind/16.5.689. [DOI] [PubMed] [Google Scholar]
- 7.Drevets DA, Leenen PJ, Greenfield RA. Invasion of the central nervous system by intracellular bacteria. Clin Microbiol Rev. 2004;17:323–347. doi: 10.1128/CMR.17.2.323-347.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Midi I, Ekinci G, Yaroglu S, Aktan S. Brain abscesses due to Listeria monocytognes: case report. Firat Medical Journal (Turkey) 2005;10:36–39. [Google Scholar]
- 9.Alper G, Knepper L, Kanal E. MR findings in listerial rhombencephalitis. AJNR Am J Neuroradiol. 1996;17:593–596. [PMC free article] [PubMed] [Google Scholar]
- 10.Kao CH, Wang SJ, Mak SC, et al. Viral encephalitis in children: detection with technetium-99m HMPAO brain single-photon emission CT and its value in prediction of outcome. AJNR Am J Neuroradiol. 1994;15:1369–1373. [PMC free article] [PubMed] [Google Scholar]
- 11.Ametani M, Ogawa T, Tanabe Y, et al. Sequential MR imaging and SPECT studies in herpes simplex encephalitis with crossed cerebellar hyperperfusion. Ann Nucl Med. 2005;19:151–155. doi: 10.1007/BF03027395. [DOI] [PubMed] [Google Scholar]


