Introduction
The incidence of gastrointestinal tract duplication cysts is 1:100,000, with only about 160 cases described in adults.[1] The main locations of these duplication cysts are the ileum (50%), esophagus (25%), colon (15%), stomach (5%), duodenum (4%), and pancreas with biliary tree (< 1%).[1–3]
There are several anomalies of foregut duplication that can present as cystic masses in the chest. The esophageal duplication cyst represents one of the two most common types of bronchopulmonary foregut malformations.[4,5] The bronchogenic-type cyst occurs more frequently and is usually located in the mediastinum around the tracheobronchial tree, whereas esophageal duplication cysts are most frequently located in the right posterior inferior mediastinum.[5,6]
The primitive foregut gives rise to the pharynx and lower respiratory tract as well as to the upper gastrointestinal tract. Foregut cysts are lined by a ciliated epithelium, which lines both the early tracheobronchial tree and esophagus. Thus, from a pathology point of view, mediastinal cysts can be classified as esophageal duplications if they are close to the esophageal wall; are covered by 2 muscle layers; and if the lining is squamous, columnar, cuboid, pseudostratified, or ciliated epithelium.[4,6,7]
Esophageal duplication cysts become symptomatic in early childhood in 80% of cases.[4,8] In adults, esophageal duplication cysts are usually asymptomatic or cause mild dysphagia.[2,6,9] These cysts can be complicated by intracystic hemorrhage, cystic rupture, and infection, especially those with bronchial and esophageal communication.[10–12] Squamous metaplasia and malignant transformation have also been reported.[13,14]
The treatment of choice consists of open excision by thoracotomy or laparotomy and minimally invasive techniques.[6] Cases of esophageal duplication cyst removal by laparoscopic, thoracoscopic, and even transluminal (transesophageal) endoscopic approaches have been reported.[1, 15–17]
This is the first case report of laparoscopic robotic-assisted transhiatal esophageal duplication cyst removal.
-
1.Which of the following mediastinal lesions can be represented as a cystic mass?
- Hodgkin's lymphoma
- Neuroma
- Germ cell tumor
- Thymoma
- All of the above
Cystic Masses of the Mediastinum
Many tumors can undergo cystic degeneration. Lesions, such as thymomas, Hodgkin's lymphoma, germ cell tumors (mature teratoma), mediastinal carcinomas, metastases to lymph nodes, and nerve root tumors – especially if they undergo radiation therapy or chemotherapy – may demonstrate mixed solid and cystic elements on computed tomographic (CT) or magnetic resonance imaging (MRI) exam. If degeneration is extensive, such tumors may be virtually indistinguishable from congenital cysts. Thymic cysts (congenital and acquired) represent 1% of all mediastinal masses.[18] Acquired thymic cysts may occur in patients after radiation therapy for Hodgkin's disease, in association with thymic tumors, and after thoracotomy. Other cystic lesions that can be found in the mediastinum include lymphangioma (0.7% to 4.5% of all mediastinal tumors), choriocarcinoma, cystic schwannoma, lateral thoracic meningocele, and pericardial cyst.[18] A mediastinal abscess or pancreatic pseudocyst can also appear as a fluid-containing mediastinal cystic mass.[19]
-
2.
Which of the following studies is most likely to confirm the diagnosis of an esophageal duplication cyst: chest x-ray, upper gastrointestinal barium studies, CT scan, repeat esophagogastroscopy, esophagogastroscopy with endoscopic ultrasound (EUS), MRI, positron emission tomography (PET), or radionuclide scanning?
Esophagogastroscopy with EUS is the study that is most likely to confirm the diagnosis of an esophageal duplication cyst. Click on “Next Page” for an in-depth discussion of this topic.
Diagnostic Imaging
On chest x-ray, benign mediastinal cysts appear as sharply marginated, round, or oval areas of increased opacity. Their appearance is similar to that of other cystlike lesions, but the location in the mediastinum can suggest the diagnosis and guide subsequent imaging procedures. However, many midline midsize lesions located in the lower mediastinum may not be seen on chest x-ray.
Because most adult patients with esophageal duplication cysts are asymptomatic or present with mild dysphagia, the best initial radiologic intervention is upper gastrointestinal barium studies. Barium examination of the upper digestive tract will show extrinsic or intramural compression due to close contact with the esophagus.
Esophagogastroscopy would be the next logical step in diagnostic work-up, although duplication cysts are often difficult to see on initial endoscopy. Repeat esophagogastroscopy with biopsy will exclude an esophageal mucosa-originated malignancy and other comorbidities, as well as possible communication with the cyst cavity. This modality will help define the degree of stenosis (extraluminal compression) and location of the mass in relation to the gastroesophageal junction.
Benign mediastinal cysts have the following features on a CT scan: a smooth, oval or, tubular mass with a well-defined thin wall that usually enhances after intravenous contrast, and no infiltration of adjacent mediastinal structures. However, esophageal duplication cysts contain nonserous fluid; because its thick mucinous content can have high attenuation on CT exam, it may be mistaken for a solid lesion.[19]
MRI can be useful in showing the cystic nature of these masses because these lesions continue to have characteristically high signal intensity when imaged with T2-weighted sequences, regardless of the nature of the cyst contents. However, the appearance of esophageal duplication cysts on CT or MRI exam is identical to that of bronchogenic cysts, except that the wall of the lesion may be thicker and in more intimate contact with the esophagus.[17,18]
Esophagogastroscopy and EUS can facilitate accurate preoperative diagnosis of an esophageal duplication cyst, differentiating the lesion from other mediastinal cysts. In most patients, the cyst lumen appears to be filled with a relatively echogenic material. Most important, EUS can accurately demonstrate contiguity of the muscularis propria of the esophagus with the muscle layer of the cyst wall. Esophagogastroscopy usually can suggest a fullness but cannot make the diagnosis alone.
This most reliable nonsurgical method for the diagnosis of this lesion should be used as a final preoperative test, not as an initial approach.[1,6,16,18]
PET imaging is highly accurate in the restaging of esophageal cancer. Overall, it compares favorably to anatomic imaging in the evaluation of tumor recurrence because metabolic abnormalities usually precede a structural change. Initial imaging of mediastinal cystic lesions, which are usually benign, with PET is inappropriate and costly. However, this study may be used in patients with confirmed malignization of the cyst to exclude local invasion and lymph node spread.
Radionuclide scanning with Tc-99m sodium pertechnetate may be helpful in pediatric patients, in 50% of whom thoracic duplication cysts contain ectopic gastric mucosa.[19] There is no evidence for using radionuclide scanning in the diagnosis of mediastinal cystic lesions in adults.
-
3.Which of the following strategies is the treatment of choice for a patient with an esophageal duplication cyst?
- Observation, because the vast majority of esophageal duplication cysts are benign
- EUS-guided fine-needle aspiration; if no malignancy, then observation
- CT scan-guided biopsy; if no malignancy, then observation
- Surgery if symptomatic; observation if asymptomatic
- Surgery in all cases
Approach to Therapy
Complete excision of the cyst is the treatment of choice. Several reports in the literature suggest that observation is the appropriate strategy, including one case report of a patient who remained asymptomatic during 13 years of follow-up.[9] However, the largest series with patient observation suggested that most adults with mediastinal cysts develop symptoms and/or complications.[6,20] In a reported series of 86 patients, St-Georges and colleagues[20] noted that with prolonged observation, 72% of patients became symptomatic and/or experienced complications. Mediastinal cysts can be complicated by hemorrhage, infection, rapid cyst enlargement, cyst rupture, and malignant transformation.[10–14] The most commonly reported malignancy is squamous followed by adenocarcinoma.[14,15] This is a rare event with no specific data on the risk for transformation. All presumed mediastinal cysts should be resected because an operation can be more hazardous when the cyst becomes symptomatic and because definitive diagnosis can be established only on the surgical specimen. Thus, any additional invasive diagnostic attempts, such as EUS or CT-guided needle aspiration/biopsy, do not provide further information, but may cause cyst or mediastinal infection.
-
4.Which of the following surgical approaches can be used to treat esophageal duplication cysts?
- Laparoscopic/robotic transhiatal excision of the cyst
- Thoracoscopic cystectomy
- Laparotomy, transhiatal esophageal dissection, and cystectomy
- Endoluminal transesophageal cystectomy
- All of the above
Surgical Techniques
Robotic-assisted transhiatal removal of the paraesophageal cyst would provide a 3-dimensional view and precise movements that allow for separation of the cyst wall, which is intimately attached to the esophagus and which prevents esophageal perforation. Robotic-assisted Heller myotomy has been shown to be superior to conventional laparoscopy in terms of esophageal perforation rate.[21]
The size and location of the esophageal duplication cysts make them amenable to laparoscopic transhiatal removal. Avoidance of esophageal perforation is important. If the cyst is more concentrated in the esophageal wall, has a common muscular layer, or has fistulous communication with the esophageal lumen, conversion to an open procedure could still be performed.
Laparotomy and thoracotomy are acceptable approaches in this setting as well. The conventional surgical approach for removal of mediastinal cysts is a posterolateral thoracotomy. One of the largest series on surgical treatment of esophageal duplication cysts in adults was reported by Cioffi and colleagues[6] in 1998. Esophageal duplication cysts should be excised by carefully preserving the muscle layer. Both vagal nerves should be identified and preserved. Mucosal integrity should be checked intraoperatively by air insufflation through the nasogastric tube.
One case in the literature described transluminal total endoscopic removal of the esophageal duplication cyst with good results.[1] However, this approach required multiple attempts and only partial cyst removal was achieved, with a residual cavity left for observation by repeated endoscopy. It is important to note that recurrence has been reported after incomplete excision of mediastinal cysts.[10]
Case Report
The patient is a 23-year-old woman with a history of dysphagia and chest pain. As part of the initial work-up, she underwent an abdominal/pelvic CT scan that revealed a distal esophageal mass. She then underwent an upper gastrointestinal study (Figure 1), chest CT scan (Figure 2), and upper endoscopy to further evaluate the radiographic finding.
Figure 1.

Upper gastrointestinal study shows mass effect of the cyst.
Figure 2.
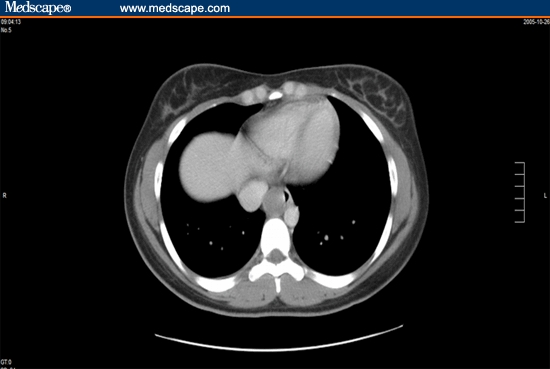
CT scan shows typical round mass displacing the esophagus.
The upper gastrointestinal double-contrast study revealed a submucosal mass in the distal esophagus with concave margins. The mass was located in the right posterior esophagus, 10 cm proximal to the gastroesophageal junction. The chest CT scan with oral and intravenous contrast revealed a 2.1- × 2.2-cm intramural distal esophageal mass on the right side. The lesion appeared to cause some mass effect on the esophageal lumen, without obstruction. There was some hypodensity noted within the mass. Likewise, the esophagogastroscopy revealed an extrinsic mass effect on the esophageal mucosa proximal to the gastroesophageal junction. Except for a small hiatal hernia, no other mucosal abnormalities were revealed. The remainder of the patient's medical history was unremarkable, including no chronic illness or previous surgery. Physical examination was normal.
The patient was scheduled for a laparoscopic robotic-assisted enucleation of the esophageal mass via a transhiatal approach.
Surgical Procedure
Video clip: da Vinci Cystectomy Click "Play" to view the video.
Following induction of general anesthesia and endotracheal intubation, 4 ports were placed. The camera port was placed 3 cm above the umbilicus just left of the midline. Two 10-mm ports were introduced just caudal to the costal margin on the left, one at the midclavicular line and one in the anterior axillary line. The final port was introduced in the right upper quadrant in the midclavicular line, 5 cm below the costal margin. A laparoscopic liver retractor was placed through the epigastrium to lift the left lobe of the liver anteriorly.
Conventional laparoscopy was used to expose the esophageal hiatus. The gastrohepatic ligament was divided with ultrasonic shears exposing the right crus of the diaphragm. The remainder of the hiatus was then exposed and defined with both blunt and sharp dissection, again with ultrasonic shears. Upon exposure of the esophagus at the hiatus, a penrose drain was placed around the gastroesophageal junction to provide caudal retraction. Extended mediastinal esophageal mobilization was then undertaken until the proximal extent of the cyst was identified.
The robotic cart was positioned and docked. An esophageal myotomy was initiated 2 cm distal to the cyst with hook cautery and continued over the cyst until its anterior surface was completely exposed. With the use of blunt and sharp dissection, the cyst was enucleated and separated from the esophageal mucosa. It was subsequently placed in a specimen bag and extracted from the abdominal cavity. A thorough inspection of the mucosa, including a leak test, did not reveal any lacerations of the mucosa or communication with the esophageal lumen.
The myotomy was loosely reapproximated with 2-0 silk suture in a running fashion over the endoscope. A posterior cruroplasty was performed with 0 silk stitches, and then a standard Dor fundoplication was created covering the myotomy site.
Clinical Outcome
On postoperative day 1, an upper gastrointestinal exam showed no evidence of a leak. The patient was started on a liquid diet and reported no dysphagia; she was discharged home on postoperative day 1. Pathologic examination of the specimen revealed characteristics consistent with a developmental esophageal duplication cyst.
Footnotes
Readers are encouraged to respond to George Lundberg, MD, Editor of MedGenMed, for the editor's eye only or for possible publication via email: glundberg@medscape.net
Contributor Information
Chad Ringley, Department of Surgery, University of Nebraska Medical Center, Omaha, Nebraska.
Victor Bochkarev, Department of Surgery, University of Nebraska Medical Center, Omaha, Nebraska.
Dmitry Oleynikov, University of Nebraska Medical Center, Omaha, Nebraska.
Brant K Oelschlager, University of Washington, Seattle; Director, Swallowing Center, University of Washington Medical Center, Seattle, Washington.
Carlos A Pellegrini, Center for Videoendoscopic Surgery, Department of Surgery, University of Washington, Seattle.
References
- 1.Will U, Meyer F, Bosseckert H. Successful endoscopic treatment of an esophageal duplication cyst. Scand J Gastroenterol. 2005;40:995–999. doi: 10.1080/00365520510023125. [DOI] [PubMed] [Google Scholar]
- 2.Diaz de Liano A, Ciga MA, Trujillo R, et al. Congenital esophageal cysts: two cases in adult patients. Hepatogastroenterology. 1999;46:2405–2408. [PubMed] [Google Scholar]
- 3.Wootton-Gorges SL, Eckel GM, Poulos ND, et al. Duplication of the cervical esophagus: a case report and review of the literature. Pediatr Radiol. 2002;32:533–535. doi: 10.1007/s00247-002-0693-8. [DOI] [PubMed] [Google Scholar]
- 4.Gerle RD, Jaretzki A, III, Ashley CA, Berne AS. Congenital bronchopulmonary foregut malformation. N Engl J Med. 1968;278:1413–1419. doi: 10.1056/NEJM196806272782602. [DOI] [PubMed] [Google Scholar]
- 5.Rodgers BM, Harman PK, Johnson AM. Bronchopulmonary foregut malformations. The spectrum of anomalies. Ann Surg. 1986;203:517–524. doi: 10.1097/00000658-198605000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cioffi U, Bonavina L, De Simone M, et al. Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest. 1998;113:1492–1496. doi: 10.1378/chest.113.6.1492. [DOI] [PubMed] [Google Scholar]
- 7.Kim KW, Kim WS, Cheon JE, et al. Complex bronchopulmonary foregut malformation: extralobar pulmonary sequestration associated with a duplication cyst of mixed bronchogenic and oesophageal type. Pediatr Radiol. 2001;31:265–468. doi: 10.1007/s002470000410. [DOI] [PubMed] [Google Scholar]
- 8.Sundaramoorthi T, Behranwala AA, Codispoti M, Mankad PS. Asymptomatic congenital oesophageal cyst infiltrating the lung: an unusual complication. Eur J Cardiothorac Surg. 2000;18:117–119. doi: 10.1016/s1010-7940(00)00443-7. [DOI] [PubMed] [Google Scholar]
- 9.Versleijen MW, Drenth JP, Nagengast FM. A case of esophageal duplication cyst with a 13-year follow-up period. Endoscopy. 2005;37:870–872. doi: 10.1055/s-2005-870219. [DOI] [PubMed] [Google Scholar]
- 10.Al-Sadoon H, Wiseman N, Chernick V. Recurrent thoracic duplication cyst with associated mediastinal gas. Can Respir J. 1998;5:149–151. doi: 10.1155/1998/305489. [DOI] [PubMed] [Google Scholar]
- 11.Neo EL, Watson DI, Bessell JR. Acute ruptured esophageal duplication cyst. Dis Esophagus. 2004;17:109–111. doi: 10.1111/j.1442-2050.2004.00385.x. [DOI] [PubMed] [Google Scholar]
- 12.Kuwashima S, Chikatsu H, Kohno T, et al. Esophageal duplication cyst complicated by Mycobacterium avium complex infection. Pediatr Int. 2005;47:592–594. doi: 10.1111/j.1442-200x.2005.02111.x. [DOI] [PubMed] [Google Scholar]
- 13.Singh S, Lal P, Sikora SS, Datta NR. Squamous cell carcinoma arising from a congenital duplication cyst of the esophagus in a young adult. Dis Esophagus. 2001;14:258–261. doi: 10.1046/j.1442-2050.2001.00204.x. [DOI] [PubMed] [Google Scholar]
- 14.Lee MY, Jensen E, Kwak S, Larson RA. Metastatic adenocarcinoma arising in a congenital foregut cyst of the esophagus: a case report with review of the literature. Am J Clin Oncol. 1998;21:64–66. doi: 10.1097/00000421-199802000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Michel JL, Revillon Y, Montupet P, et al. Thoracoscopic treatment of mediastinal cysts in children. J Pediatr Surg. 1998;33:1745–1748. doi: 10.1016/s0022-3468(98)90276-7. [DOI] [PubMed] [Google Scholar]
- 16.Noguchi T, Hashimoto T, Takeno S, Wada S, Tohara K, Uchida Y. Laparoscopic resection of esophageal duplication cyst in an adult. Dis Esophagus. 2003;16:148–150. doi: 10.1046/j.1442-2050.2003.00314.x. [DOI] [PubMed] [Google Scholar]
- 17.Machado MA, Santos VR, Martino RB, et al. Laparoscopic resection of gastric duplication: successful treatment of a rare entity. Surg Laparosc Endosc Percutan Tech. 2003;13:268–270. doi: 10.1097/00129689-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Bhutani MS, Hoffman BJ, Reed C. Endosonographic diagnosis of an esophageal duplication cyst. Endoscopy. 1996;28:396–397. doi: 10.1055/s-2007-1005489. [DOI] [PubMed] [Google Scholar]
- 19.Jeung MY, Gasser B, Gangi A, et al. Imaging of cystic masses of the mediastinum. Radiographics. 2002;22:S79–93. doi: 10.1148/radiographics.22.suppl_1.g02oc09s79. [DOI] [PubMed] [Google Scholar]
- 20.St-Georges R, Deslauriers J, Duranceau A, et al. Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg. 1991;52:6–13. doi: 10.1016/0003-4975(91)91409-o. [DOI] [PubMed] [Google Scholar]
- 21.Horgan S, Galvani C, Gorodner MV, et al. Robotic-assisted Heller myotomy versus laparoscopic Heller myotomy for the treatment of esophageal achalasia: multicenter study. J Gastrointest Surg. 2005;9:1020–1029. doi: 10.1016/j.gassur.2005.06.026. [DOI] [PubMed] [Google Scholar]


