Abstract
BACKGROUND
A high prevalence of comorbid psychiatric disorders has been demonstrated in individuals with an alcohol use disorder in both community and treatment samples, with higher comorbidity in treatment samples. In this study, we examined lifetime and current psychiatric diagnoses in long-term abstinent alcoholics (LTAA; mean abstinence = 6.3 years; n = 52) compared to age and gender-comparable non-alcoholic controls (NC; n = 48). We asked the following questions: 1) to achieve long-term abstinence, must an individual be relatively psychiatrically healthy (i.e., comparable to NC) and 2) can ongoing abstinence be maintained in the face of a current psychiatric disorder?
METHODS
Lifetime and current (prior 12-months) psychiatric diagnoses were assessed in the mood, anxiety, and externalizing disorder domains using the computerized Diagnostic Interview Schedule (c-DIS).
RESULTS
Over 85% of LTAA had a lifetime psychiatric diagnosis, compared to 50% of NC. LTAA had a higher prevalence than NC of lifetime mood, anxiety, and externalizing disorder diagnoses. LTAA also had a greater prevalence than NC of current mood and anxiety diagnoses. Although LTAA had a greater lifetime prevalence of an antisocial personality disorder (ASPD) than NC, no LTAA or NC had a current ASPD diagnosis. Finally, there was no association of duration of abstinence with lifetime or current psychiatric diagnoses, consistent with psychiatric diagnoses having little effect on relapse.
CONCLUSIONS
Our results suggest that: 1) the presence of a lifetime psychiatric diagnosis does not militate against achieving long-term abstinence, 2) abstinence can be maintained in the presence of a current mood or anxiety disorder, and 3) a current diagnosis of ASPD may not be compatible with long-term abstinence. The relatively low levels of antisocial behavior compared to pre-abstinence (as indicated by no LTAA meeting current criteria for ASPD) raises the question of whether the neurobiology underlying antisocial behavior is changed in abstinence, or brought under increased executive control, or both.
Keywords: alcoholism, mood, anxiety, antisocial, dual-diagnosis
INTRODUCTION
Over the past 15 years the high prevalence of comorbid psychiatric disorders in individuals with an alcohol use disorder (AUD) or drug use disorder (DUD) has been documented in a number of large sample epidemiological studies such as the Epidemiologic Catchment Area Study (Regier et al., 1990), the National Comorbidity Survey (Kessler et al., 1997), and the National Epidemiologic Survey on Alcohol Use and Related Conditions (Grant et al., 2004a; Grant et al., 2004b). These epidemiological surveys, along with studies of samples in treatment settings, establish the pervasiveness of psychiatric comorbidity in AUDs and DUDs. For example, in the Epidemiologic Catchment Area Study, approximately 45% of persons with an AUD (and 72% of those with a DUD) had at least one co-occurring psychiatric disorder (a ‘dual-diagnosis’) (Regier et al., 1990). The National Comorbidity Study found that 78% of alcoholic men and 86% of alcoholic women met criteria for a lifetime psychiatric diagnosis (Kessler et al., 1997). Psychiatric comorbidity is greater in individuals with a DUD than in those with an AUD (Currie et al., 2005; Grant et al., 2004b; Regier et al., 1990), thus increasing the psychiatric comorbidity rates for samples of AUDs that include individuals with comorbid DUDs. Psychiatric comorbidity is also greater in samples drawn from substance abuse treatment settings than in untreated community samples (Helzer and Pryzbeck, 1988; Regier et al., 1990; Tomasson and Vaglum, 1995). Indeed, a large cross-national investigation of comorbidity between substance use and psychiatric disorders in six studies participating in the International Consortium in Psychiatric Epidemiology reported strong associations of anxiety, mood, and antisocial personality disorders with substance use disorders, even in the context of large differences in the prevalence of these disorders across study sites (Merikangas et al., 1998). That study found that the more severe the substance use (on the continuums of use, problems, or dependence), the stronger the association with comorbid psychiatric disorders and, conversely, the greater the number of comorbid psychiatric disorders, the more severe the substance use pattern (this relationship was particularly pronounced for drug use, as opposed to alcohol use).
The literature on the effects of psychiatric disorders comorbid with SUDs (substance abuse disorders; a term that combines AUDs and DUDs) on SUD treatment outcome has not yielded uniform results. Most of the early studies reported a negative association between psychiatric comorbidity and treatment outcome (e.g., (Hesselbrock et al., 1985; Rounsaville et al., 1987; Schuckit, 1983)). Loosen and colleagues (Loosen et al., 1990) found that individuals with comorbid depression remained abstinent an average of 3.3 years compared to 6.8 years for those without comorbid depression. Similarly, Hasin et al. (Hasin et al., 2002) showed that Major Depressive Disorder during sustained abstinence predicted relapse to alcohol dependence. Some recent studies also report on the difficulty of maintaining abstinence in the face of a comorbid disorder. Greenfield and colleagues (Greenfield et al., 1998) found that depressive symptoms and a diagnosis of major depressive disorder at treatment entry were predictive of both a shorter time to first drink and a higher incidence of relapse, although scores on the Beck Depression Inventory were non-predictive. Burns et al. (Burns et al., 2005) found that patients entering treatment with comorbid DSM-IV disorders were more disabled and drank more heavily than those without a psychiatric disorder at commencement of treatment. At 3-month follow-up, although the groups with and without a comorbid psychiatric diagnosis improved overall, the comorbid group was still more disabled and drank more heavily.
In contrast, two recent studies, one with a large sample and the other an epidemiology survey, failed to find an effect of psychiatric comorbidity on SUD outcome. Chi and colleagues (Chi et al., 2006) showed that individuals with psychiatric disorders co-occurring with SUDs (104 individuals out of a total sample of 747) had comparable SUD outcomes to individuals with SUDs but no comorbid psychiatric disorders at one year. Bischof et al. (Bischof et al., 2005) examined the effects of non-psychotic psychiatric comorbidity on treatment utilization and natural recovery from alcoholism in a population survey. They contacted 4,075 individuals (response rate: 70.2%) in Northern Germany, of whom 3.8% met DSM-IV lifetime criteria for alcohol dependence and 1.3% were alcohol dependent in the last year. One hundred and fifty-three lifetime alcohol dependent individuals were assessed, among whom 98 fulfilled the criteria for sustained long-term remission according to the Diagnostic and Statistical Manual version II (DSM-IV) criteria (American Psychiatric Association, 2000). The rate of individuals who remitted from alcohol dependence without formal help was 36.9% in individuals without comorbid psychiatric diagnoses and 42.6% in individuals with psychiatric comorbidity. Utilization of formal help was unrelated to Axis I psychiatric comorbidity in this epidemiological study (i.e., comorbidity was no greater in individuals who availed themselves of treatment than in those who did not).
In the current study, we examined lifetime and current psychiatric comorbidity in long-term abstinent alcoholics (LTAA) compared to age and gender-comparable non-alcoholic controls (NC). We asked the following questions: 1) how does the prevalence of lifetime psychiatric diagnoses in LTAA compare to that of NC (i.e., to achieve long-term abstinence, must an individual be relatively psychiatrically healthy, that is, comparable to non-alcoholic controls)? and 2) how does the prevalence of current psychiatric diagnoses in LTAA compare to that of NC (i.e., can ongoing abstinence be maintained in the face of a current psychiatric disorder)?
METHODS
Subjects
A total of 100 participants were recruited from the community by postings at AA meeting sites, mailings, newspaper advertisements, a local Internet site, and subject referrals. The study consisted of two subject groups: LTAA and NC. The LTAA group (n = 52) comprised 24 women and 28 men, ranging from 35 to 57 years of age (mean = 46.5 years), abstinent from 6 months to 21 years (mean = 6.3 years). The inclusion criteria for the LTAA group were: 1) met lifetime DSM-IV (American Psychiatric Association, 2000) criteria for alcohol dependence, 2) had a lifetime drinking average of at least 100 standard drinks per month for men, and 80 standard drinks per month for women, and 3) were abstinent for at least 6 months. A standard drink was defined as 12 oz. beer, 5 oz. wine, or 1.5 oz. liquor. Nine of the LTAA had attended inpatient treatment only, 13 had attended outpatient treatment only, 6 had attended both inpatient and outpatient treatment, 4 had attended both inpatient treatment and Alcoholics Anonymous, 14 had gotten sober in Alcoholics Anonymous (without going to formal treatment), and 6 had gotten sober on their own (without AA or formal treatment). The NC consisted of 23 women and 25 men, ranging in age from 34 to 59 years of age (mean = 45.6 years). The inclusion criterion for the NC group was a lifetime drinking average of less than 30 standard drinks per month, with no periods of drinking more than 60 drinks per month.
Exclusion criteria for both groups were: 1) lifetime or current diagnosis of schizophrenia or schizophreniform disorder using the computerized Diagnostic Interview Schedule (c-DIS; (Bucholz et al., 1991; Erdman et al., 1992; Levitan et al., 1991; Robins et al., 1998)), 2) history of or current drug abuse or dependence (other than nicotine or caffeine), 3) significant history of head trauma or cranial surgery, 4) history of significant neurological disease, 5) history of diabetes, stroke, or hypertension that required medical intervention, 6) laboratory evidence of hepatic disease, or 7) clinical evidence of Wernicke-Korsakoff syndrome.
Procedures
All individuals were fully informed of the study’s procedures and aims, and signed a consent form prior to their participation. Participants completed four sessions that lasted between one hour and a half and three hours, and included clinical, neuropsychological, electrophysiological, and neuroimaging assessments. Non-alcoholic controls were asked to abstain from consuming alcohol for at least 24 hours prior to any lab visit. A Breathalyzer (Intoximeters, Inc., St. Louis, MO) test was administered to all participants. A 0.00 alcohol concentration was required of all participants in all sessions. Participants were compensated for time and travel expenses upon completion of each session. Individuals who completed the entire study were also given a completion bonus.
General Assessment
All participants participated in the following assessments: 1) psychiatric diagnoses and symptoms were gathered using the c-DIS assessment (Robins et al., 1998), 2) individuals were interviewed on their drug and alcohol use using the lifetime drinking history methodology (Skinner and Allen, 1982; Skinner and Sheu, 1982; Sobell and Sobell, 1990; Sobell et al., 1988), 3) medical histories were reviewed, 4) blood was drawn to test liver function, and 5) the Family History Drinking Questionnaire was administered based on the methodology of Mann et al. (Mann et al., 1985; Stoltenberg et al., 1998).
Family Drinking Density
Family Drinking Density was assessed using the Family History Drinking Questionnaire (Mann et al., 1985; Stoltenberg et al., 1998). Participants were asked to rate their biological relatives as being alcohol abstainers, alcohol users with no problem, or problem drinkers. The proportion of first-degree relatives that were identified as problem drinkers was determined from this questionnaire. Table 1 presents a summary of the demographic, family drinking density, and alcohol use variables.
Table 1.
Demographic and Alcohol Use Measures
| Abstinent Alcoholics | Non-Alcoholic Controls | ||||
|---|---|---|---|---|---|
| Variables | Female (n = 24) | Male (n = 28) | Female (n = 23) | Male (n = 25) | Effect Size a |
| Age | 48.4 ± 6.4 | 44.9 ± 6.9 | 48.0 ± 6.6 | 43.4 ± 6.3 | 0.6 |
| Years of education | 15.5 ± 2.4 | 15.5 ± 2.0 | 16.0 ± 1.9 | 16.3 ± 2.2 | 2.2 |
| Proportion of 1st degree relative problem drinkers b | 0.44 ± 0.30 | 0.40 ± 0.26 | 0.17 ± 0.21 | 0.14 ± 0.22 | 24.0 *** |
| Ethnicity c | 24 C | 1 AA, 24 C, 1 H, 2 B | 1 AA, 15 C, 2 H, 3 B, 2 A | 2 AA, 15 C, 2 H, 1 B, 5 A | |
| Alcohol Use Variables | |||||
| Age at first drink | 17.1 ± 5.6 | 14.8 ± 2.9 | 20.4 ± 4.9 | 18.8 ± 4.9 | 13.8 *** |
| Age at first heavy use of alcohol | 25.3 ± 7.6 | 21.6 ± 4.5 | N/A | N/A | N/A |
| Dose last 6 months (drinks per month) | 245.8 ± 213.0 | 269.5 ± 266.3 | 5.5 ± 9.7 | 5.5 ± 8.7 | 34.8 d |
| Duration of abstinence in years | 6.3 ± 5.6 | 6.3 ± 6.1 | N/A | N/A | N/A |
| Lifetime alcohol dose (drinks per month) | 129.3 ± 77.5 | 177.3 ± 146.7 | 6.8 ± 7.6 | 6.9 ± 8.3 | 42.5 d |
| Lifetime use (dose x duration in months) | 39628 ± 37755 | 53520 ± 59039 | 1953 ± 2346 | 1779 ± 2194 | 28.1 d |
| Peak alcohol dose (drinks per month) | 270 ± 201 | 340 ± 253 | 17 ± 22 | 15 ± 14 | 43.8 d |
| Peak use (dose x duration in months) | 24535 ± 29143 | 26428 ± 43777 | 1006 ± 1501 | 899 ± 1501 | 17.3 d |
Percent of variance of the dependent variable accounted for by group membership
Before analysis, the proportions were normalized using the arcsin transformation
AA = African American, C = Caucasian, H = Hispanic, B = Bi/Multiracial, A = Asian
Alcohol dependence was a selection criteria, therefore, statistical comparisons between groups is inappropriate
p ≤ 0.001,
p ≤ 0.01,
p ≤ 0.05
Psychiatric Diagnoses
The c-DIS was administered to all participants by a research associate. We found it helpful to have the research associate ask the c-DIS questions and navigate through the c-DIS decision tree to avoid the participants’ frustration with this process. In addition, this allowed the research associate to compare participants’ answers to the c-DIS with their phone screen and other volunteered information. (We found this verification of information especially helpful in studies of individuals with active SUDs.)
The c-DIS was used to assess for the following potential current and lifetime diagnoses in the mood and anxiety disorder domains: Bipolar Disorder, Dysthymia, Hypomania, Mania, Major Depressive Disorder, Agoraphobia, Compulsive Disorder, Obsessive Disorder, Panic Disorder, Post-Traumatic Stress Disorder, and Social Phobia. In the domain of externalizing disorders potential current and lifetime diagnoses assessed were Antisocial Personality Disorder, with the addition of Conduct Disorder without ASPD in the lifetime diagnosis domain only.
Statistical Analysis
The data were analyzed using the Statistical Package for Social Sciences (SPSS) (SPSS Inc., 2004). First, we looked for gender differences in controls, so that we would have a context for subsequent examination of the effects of alcoholism on psychiatric diagnoses of men versus women. Comparisons of the frequencies of diagnoses across groups were analyzed using the chi-square statistic. In the analysis of current diagnoses (last 12 months prevalence), we removed all LTAA with less than 18 months of abstinence, so that diagnoses during the period of drinking and the first six months of abstinence would not be included. This resulted in the exclusion of 12 LTAA, and the analysis of 40 LTAA for current diagnoses. We examined diagnoses in three domains: mood disorders, anxiety disorders, and externalizing disorders. We used a variant of Fisher’s protected t-test to control for multiple comparisons within psychiatric domains (Cohen and Cohen, 1983). First, we examined a summary measure for the domain (e.g., individuals having any mood diagnoses). Only if there was a significant result for the summary measure did we proceed to examine individual diagnoses in that domain. Finally, we used Spearman correlations (which are resistant to the effects of outliers) to examine correlations between diagnosis rates and alcohol use variables and family history measures.
RESULTS
Demographic and Alcohol Use Measures
LTAA had a higher proportion of first-degree relatives who were problem drinkers than NC (F1,96 = 30.27, p < 0.0001). Since alcohol dependence was a selection variable, statistical comparison between groups on alcohol use variables was not valid. Nonetheless, the average lifetime monthly alcohol dose for LTAA was 20 times the NC dose for women and 30 times the NC dose for men. LTAA also began drinking at an earlier age than NC (F1,96 = 15.06, p < 0.001).
Correlations of Diagnoses with Alcohol Use Measures
Lifetime ASPD was associated with drinking at an earlier age (r = −.346, p = .016). A current mood disorder diagnosis was associated with lower lifetime dose (r = −.333, p = .021) and a lower peak dose (r = −.304, r = .035). Neither of the above p-values were corrected for multiple comparisons. Finally, duration of abstinence was not associated with the presence of a lifetime or current diagnosis (‘any diagnosis,’ or a mood, anxiety, or externalizing diagnosis) (all | r |’s < 0.225, all p’s > 0.11, not corrected for multiple comparisons). This lack of association of duration of abstinence with diagnoses is displayed graphically in Figure 1. The distribution of abstinence duration in individuals without a current or lifetime diagnosis (circles) is similar to that in individuals with either a current or a lifetime diagnosis (squares and triangles).
Figure 1.
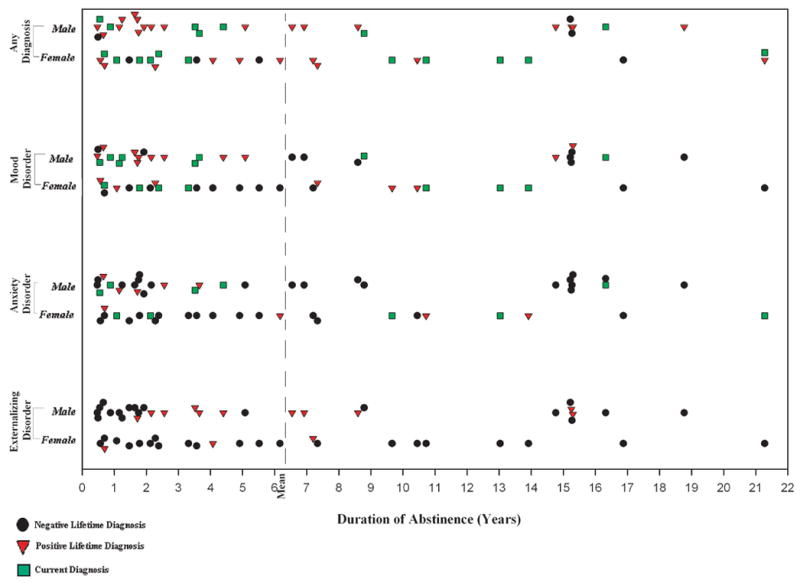
Individuals with no psychiatric diagnoses, current diagnoses, and lifetime diagnoses have similar distributions of abstinence duration.
Lifetime Psychiatric Diagnoses
Presence of Any Lifetime Diagnoses
There was a non-significant difference between NC genders, with 14/23 women and 10/25 men having a lifetime psychiatric diagnosis (Fisher’s Exact Test two-sided, p = .69). LTAA had almost twice the rate of a lifetime diagnosis as NC (45/52 = 87% vs. 24/48 = 50%; (χ2 = 15.58, p < .0001).
Presence of Lifetime Mood Disorder Diagnoses
A lifetime mood diagnosis was present in 61% of NC women compared to only 20% of NC men (χ2 = 8.37, p = .004). In LTAA, the rate of mood diagnoses was increased; this increase occurred entirely in men, where the rate was over four times that of NC (χ2 = 15.99, p = .0001). LTAA women had an almost identical rate of lifetime mood diagnoses as NC (χ2 = 0.031, p = .86). Averaged over gender, there was a group effect, which was carried entirely by the increased rate of mood diagnoses in LTAA men. When we examined the individual mood diagnoses, the effects described above were carried entirely by the Major Depressive Disorder diagnosis.
Presence of Lifetime Anxiety Disorder Diagnoses
An anxiety diagnosis was present in 17% of NC women and 12% of NC men (χ2 = 0.28, p = .60). LTAA had more than twice the rate of an anxiety diagnosis as NC (χ2 = 6.25, p = .012). When we examined individual anxiety diagnoses, this effect was carried entirely by the Post-Traumatic Stress Disorder diagnosis.
Presence of Lifetime Externalizing Disorder Diagnoses
There was a gender effect in NC (χ2 = 4.02, p = .045); there were zero lifetime externalizing disorder diagnoses in NC women, while externalizing disorders were present in 16 % of NC men. There was a group effect (χ2 = 4.91, p = .027), with 25% of LTAA having a lifetime externalizing disorder diagnosis compared to 8.3% of NC . Both the gender effect in NC and the group effect were carried entirely by ASPD.
Excluding individuals with less than one year of abstinence
We repeated the analysis of lifetime diagnosis rates after excluding all LTAA with less than one year’s abstinence (8 individuals). The results were unchanged when examining this reduced data set.
Current Psychiatric Diagnoses
Presence of Any Current Diagnoses
There was a trend toward a gender effect in NC (χ2 = 3.49, p = .062); 13% of NC women had a current diagnoses but no NC men had a current diagnosis. Thirty-five percent of LTAA had a current psychiatric diagnosis compared to 6.25% of NC (χ2 = 11.57, p < .001).
Presence of Current Mood Disorder Diagnoses
There was a trend toward a gender effect in NC (χ2 =3.48, p = .062); 13 % of women and 0% of men had a current mood diagnosis. Note that all of the current diagnoses in the NC group were Major Depressive Disorder diagnoses. There was a group effect (χ2 = 6.09, p = .014); LTAA had over four times the rate of a current mood diagnosis as NC. This finding was carried entirely by the Major Depressive Disorder diagnosis.
Presence of Current Anxiety Disorder Diagnoses
There were no current anxiety diagnoses in NC. There was a group effect (χ2 = 10.26, p = .001), with 17.5 % of LTAA having a current anxiety diagnosis, much greater than the 0% in NC. This finding was carried almost entirely by the Post-Traumatic Stress Disorder diagnosis.
Presence of Current Externalizing Disorder Diagnoses
No NC or LTAA had a current externalizing disorder diagnosis.
DISCUSSION
To our knowledge, this study is one of the very few of lifetime and current psychiatric disorders in alcohol dependent individuals who have attained long-term abstinence. We have three primary findings. First, LTAA had an increased prevalence of lifetime diagnoses compared to NC in all of the psychiatric domains assessed (mood, anxiety and externalizing disorders). Second, LTAA also had an increased prevalence of current mood and anxiety diagnoses compared to NC. Third, although 25% of LTAA had lifetime diagnoses of externalizing psychopathology, none had a current externalizing disorder diagnosis. Finally, there was no association of duration of abstinence with lifetime or current psychiatric diagnoses, consistent with psychiatric diagnoses having little or no effect on relapse once individuals achieved at least six months abstinence.
Regarding lifetime diagnosis rates, it is not possible to compare our rates to those of the major US epidemiological surveys. Not only is our sample size relatively small, but there are major differences in sampling design and assessment instruments among the epidemiological surveys (the Epidemiologic Catchment Area Study, the National Comorbidity Study, and the National Epidemiologic Survey on Alcohol Use and Related Conditions) which may underlie differences in their reported rates of comorbid psychiatric illness. However, our data still strongly support the idea that lifetime psychiatric comorbidity does not militate against achieving long-term abstinence. In fact, psychiatric comorbidity is the norm, with over 85% of the LTAA sample having a lifetime psychiatric diagnosis, comparable to the rates in the National Comorbidity Study cited in the Introduction. Although our sample cannot be directly compared to either treated or community samples in the literature, our rates of lifetime comorbid psychopathology are as high as any rates reported. Our study definitively demonstrates that long-term abstinence can be attained in a sample of alcohol-dependent individuals (without comorbid drug use disorders), most of whom have a lifetime psychiatric diagnosis.
Our results also suggest that the presence of a current (1 year prevalence) mood or anxiety disorder does not militate against maintaining long-term abstinence. Our 1 year prevalence rates for these disorders are comparable to those in the NESARC study, except that the NESARC reported about a 10% one year prevalence of anxiety disorders in their respondents without a substance use disorder (Grant et al., 2004a), while we find a zero one year prevalence in this sample. Our data clearly show that individuals with comorbid current mood or anxiety disorders (fully 26% of the LTAA sample) can maintain abstinence in the context of their current mood or anxiety disorder. There is support for this finding (that sobriety can be achieved and maintained in the face of a current diagnosis) beyond the studies of Chi et al. (Chi et al., 2006) and Bischof et al. (Bischof et al., 2005) mentioned in the introduction. Mann and colleagues (Mann et al., 2004) examined relapse in 118 consecutive admissions to a University treatment center. There was a lifetime history of a psychiatric disorder in 65% of female patients, but only 28% of male patients. Overall, at one year follow-up, 39% of all patients suffered a relapse. The relapse rate among women without a comorbid psychiatric diagnosis was 55% compared to only 28% of women with a comorbid diagnosis. The relapse rate in men without a psychiatric diagnosis was 35.3%, and the rate in men with a comorbid diagnosis was 40.9% (essentially equivalent rates). Two smaller studies had comparable results when reviewing the impact of current depression on treatment outcome. Davidson and Blackburn (Davidson and Blackburn, 1998) found no significant difference in treatment outcome between depressive and non-depressive groups of patients. Charney et al. (Charney et al., 1998) showed that, at 3-month follow-up after treatment, depressed patients had a longer duration of abstinence.
The inability to maintain psychobiological homeostasis (Koob and Le Moal, 1997) is central to addiction, and therefore important in a discussion of abstinence of any length. Unfortunately, there are few human studies that examine the psychobiological aspects of the stress response and its association with active addiction and relapse. Moreover, most of the studies that do exist are in relation to drug dependence rather than alcohol dependence, and are largely correlational, rather than causal in nature. Excessive human stress, including mood and anxiety disorders or externalizing disorders in the form of ASPD, has been shown to change human neural circuitry (especially stress and reward systems) in a way that is maladaptive to future coping with stress. Further, the dependence on substances can itself cause maladaptive changes to stress and reward circuits (see review R.. Sinha (Sinha, 2001)). (In addition, both psychiatric disorders and alcohol dependence accrue stressful negative consequences in daily life. A continuing and increasing downward spiral develops as the maladaptation increases in neural circuitry whose function is coping with stress. Alcoholism and comorbid psychiatric disorders may increase or become more intractable, more negative life consequences follow, and ‘coping’ neural circuitry becomes even more damaged). Sinha (Sinha, 2001) reviews models of the role of stress in addiction and relapse, along with differentiating the role of mood and anxiety disorders from that of externalizing disorders, especially ASPD. Vis-à-vis the question of how the individuals in the current study attained both initial and long-term abstinence in the face of these serious current or lifetime psychiatric disorders, we must recognize that the mechanism(s) involved in achieving initial abstinence may be different than the mechanism(s) involved in maintaining long-term abstinence.
In the current sample, the prevalence of a lifetime ASPD diagnosis was about 25% in LTAA compared to 6% in NC. Again, we cannot parallel prevalence rates due to our relatively small sample size, and also due to discrepancies in rates among the major epidemiological studies. However, we would like to present a context for our findings with regard to ASPD. Compton et al. (Compton et al., 2005), using data from the NESARC, found that the comorbidity of AUDs with antisocial syndromes is very common in the U.S. population; indeed, virtually all of the associations between ASPD and adult antisocial behavior and SUDs in the NESARC were positive and statistically significant (p < .05). Similarly Ross, in a study of the lifetime prevalence of AUDs and associated patterns of psychiatric comorbidity in the Mental Health Supplement (n = 9953) to the Ontario Health Survey, found that the odds of having other drug use disorders and ASPD are very high in individuals with an alcohol use disorder compared to those without (Ross, 1995).
These surveys and our study are in agreement that lifetime ASPD is more prevalent in those with AUDs compared to NC. We are very cautious about interpreting our lifetime ASPD rates in the LTAA because of the caveats presented below; nevertheless, our data are consistent with the literature presented in the last paragraph suggesting that individuals with a lifetime ASPD diagnosis may be less likely to achieve long-term abstinence. Although our lifetime ASPD rates in the LTAA group are lower than those in the epidemiological surveys, what we find most interesting is that no LTAA evidenced a current ASPD diagnosis. There are multiple investigations in the literature that document the incompatibility of abstinence and ASPD. Hesselbrock (Hesselbrock, 1991), in a study of 266 alcoholics, reported that alcoholics who were also diagnosed with ASPD reported poorer one year treatment outcomes than non-ASPD alcoholics. A Veterans Administration study that used multiple measures of psychopathology to predict which type of symptoms would predict very long-term drinking outcome among 255 alcoholic men found that antisocial personality characteristics alone were consistently associated with a worse long-term drinking outcome (Hunter et al., 2000). Another Veterans Administration study reported on the long-term outcomes of 360 men who were hospitalized for alcoholism during 1980 to 1984 and followed for 10 to 14 years (Powell et al., 1998). Overall, one of best predictors of poor outcome (of the psychosocial, alcohol-related, and psychiatric measures assessed) was the presence of a diagnosis of ASPD. Westermeyer and Thuras evaluated 606 individuals who met criteria for a SUD in treatment programs located in two university medical centers. Their major finding was that the morbidity in these addicted individuals (as measured number and types of substance-related problems and by all treatment variables) was considerably greater in those that also had a co-occurring diagnosis of ASPD (Westermeyer and Thuras, 2005).
It is possible that the strong disinhibitory and socially deviant behavior reflected in a diagnosis of ASPD must decrease for long-term sobriety to be maintained. Disinhibitory and socially deviant tendencies can be also be traced to neurobiological deficits, such a deficiencies in amygdala or ventromedial prefrontal cortex function (Bechara et al., 1999). Deficiencies may also lie in areas of the brain that act to inhibit impulsive behavior, such as prefrontal cortex (the substrate for executive control). This LTAA sample has already been shown to exhibit poor decision-making on the Iowa Gambling Task (Fein et al., 2004) and reduced amygdala volumes (Fein et al., 2006b). We interpreted the reduced amygdala volumes as suggesting that these LTAA attached less emotional valence to negative events, and the poor Iowa Gambling Task performance as suggesting that these LTAA were driven more by immediate reward than by delayed punishment. In addition, when we examined psychological measures of social deviance in these individuals, we found that the LTAA compared to NC had tremendously higher MMPI psychopathic deviate scale scores and lower Socialization scores on the California Psychological Inventory (Fein et al., 2006a); in other words, they showed a much higher propensity toward social deviance than NC, even though they did not meet criteria for a current diagnosis of ASPD. Future studies investigating the processes that result in the decrease of overt disinhibitory behavior in LTAA (in the face of their continuing psychological tendency toward social deviance) is critical to understanding how individuals are successful in achieving long-term abstinence.
There are a number of caveats in our study design that must be taken into consideration in interpreting the results. First, generalizations from these results to the population of abstinent alcoholics should be done with great caution because the sample size is relatively small and was recruited from the same geographical area. Second, we studied a sample who responded to advertisements for a research study that required a commitment to four study sessions; alcoholics with current ASPD may have been less likely to respond to our recruitment efforts. Third, it is unclear to what degree antisocial behavior in these samples was linked to intoxication. It would have been better to ascertain separately those antisocial symptoms that took place while intoxicated (or seeking drugs or alcohol, or while in withdrawal) versus those antisocial symptoms that occurred without concurrent intoxication. Finally, in hindsight, we should have included an assessment of Borderline Personality Disorder (BPD) in the externalizing domain. BPD is strongly associated with impulsivity (Dowson et al., 2004), is comorbid with AUD (Bowden-Jones et al., 2004; Dom et al., 2006), and has been associated with disadvantageous decision-making deficits (Bazanis et al., 2002; Bowden-Jones et al., 2004; Dom et al., 2006).
This study provides definitive (although preliminary) evidence that alcoholics can achieve abstinence despite a lifetime psychiatric disorder (in fact, most all LTAA in the current sample had a lifetime psychiatric disorder). Our results also show that alcoholics can maintain long-term abstinence in the context of a current psychiatric disorder. These findings present the hopeful possibility that dual-diagnosis patients can achieve and maintain sobriety.
Table 2.
Lifetime Psychiatric Diagnoses for Abstinent Alcoholics and Non-Alcoholic Controls
| Abstinent Alcoholics
|
Non-Alcoholic Controls
|
|||
|---|---|---|---|---|
| Lifetime Diagnoses | Female (n = 24) | Male (n = 28) | Female (n = 23) | Male (n = 25) |
| Any Mood Disorder | 14 | 21 | 14 | 5 |
| Bipolar Disorder | 0 | 3 | 0 | 1 |
| Dysthymia | 2 | 0 | 0 | 0 |
| Hypomania | 0 | 1 | 0 | 0 |
| Mania | 0 | 0 | 0 | 0 |
| Major Depressive Disorder | 14 | 17 | 14 | 4 |
| Any Anxiety Disorder | 9 | 10 | 4 | 3 |
| Agoraphobia | 0 | 0 | 0 | 0 |
| Compulsive Disorder | 2 | 1 | 0 | 0 |
| Obsessive Disorder | 0 | 0 | 0 | 0 |
| Panic Disorder | 1 | 2 | 2 | 0 |
| Post-Traumatic Stress Disorder | 6 | 7 | 1 | 1 |
| Social Phobia | 2 | 5 | 1 | 2 |
| Any Externalizing Disorder | 2 | 11 | 0 | 4 |
| Antisocial Personality Disorder (ASPD) | 2 | 10 | 0 | 3 |
| Conduct Disorder without ASPD | 0 | 1 | 0 | 1 |
| Any Lifetime Diagnosis | 20 | 25 | 14 | 10 |
Table 3.
Current Psychiatric Diagnoses for Abstinent Alcoholics and Non-Alcoholic Controls
| Abstinent Alcoholics
|
Non-Alcoholic Controls
|
|||
|---|---|---|---|---|
| Current Diagnoses | Female (n = 19) a | Male (n = 21) a | Female (n = 23) | Male (n = 25) |
| Any Mood Disorder | 6 | 4 | 3 | 0 |
| Bipolar Disorder | 0 | 1 | 0 | 0 |
| Dysthymia | 1 | 0 | 0 | 0 |
| Hypomania | 0 | 0 | 0 | 0 |
| Mania | 0 | 0 | 0 | 0 |
| Major Depressive Disorder | 6 | 3 | 3 | 0 |
| Any Anxiety Disorder | 4 | 3 | 0 | 0 |
| Agoraphobia | 0 | 0 | 0 | 0 |
| Compulsive Disorder | 0 | 1 | 0 | 0 |
| Obsessive Disorder | 0 | 0 | 0 | 0 |
| Panic Disorder | 0 | 1 | 0 | 0 |
| Post-Traumatic Stress Disorder | 3 | 1 | 0 | 0 |
| Social Phobia | 1 | 1 | 0 | 0 |
| Any Externalizing Disorder | 0 | 0 | 0 | 0 |
| Antisocial Personality Disorder | 0 | 0 | 0 | 0 |
| Attention Deficit/Hyperactivity Disorder | 0 | 0 | 0 | 0 |
| Any Current Diagnosis | 9 | 5 | 3 | 0 |
Abstinent alcoholics with abstinence duration of 18 months or greater (5 females and 7 males excluded)
Footnotes
This work was supported by Grants AA11311 (GF) and AA13659 (GF), both from the National Institute of Alcoholism and Alcohol Abuse.
References
- American Psychiatric Association. DSM-IV-R: Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Publishing, Inc; Washington, DC: 2000. [Google Scholar]
- Bazanis E, Rogers RD, Dowson JH, Taylor P, Meux C, Staley C, Nevinson-Andrews D, Taylor C, Robbins TW, Sahakian BJ. Neurocognitive deficits in decision-making and planning of patients with DSM-III-R borderline personality disorder. Psychol Med. 2002;32(8):1395–405. doi: 10.1017/s0033291702006657. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Damasio AR, Lee GP. Different contributions of the human amygdala and ventromedial prefrontal cortex to decision-making. J Neurosci. 1999;19(13):5473–81. doi: 10.1523/JNEUROSCI.19-13-05473.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischof G, Rumpf HJ, Meyer C, Hapke U, John U. Influence of psychiatric comorbidity in alcohol-dependent subjects in a representative population survey on treatment utilization and natural recovery. Addiction. 2005;100(3):405–13. doi: 10.1111/j.1360-0443.2005.01008.x. [DOI] [PubMed] [Google Scholar]
- Bowden-Jones O, Iqbal MZ, Tyrer P, Seivewright N, Cooper S, Judd A, Weaver T. Prevalence of personality disorder in alcohol and drug services and associated comorbidity. Addiction. 2004;99(10):1306–14. doi: 10.1111/j.1360-0443.2004.00813.x. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Robins LN, Shayka JJ, Przybeck TR, Helzer JE, Goldring E, Klein MH, Greist JH, Erdman HP, Skare SS. Performance of two forms of a computer psychiatric screening interview: version I of the DISSI. J Psychiatr Res. 1991;25(3):117–29. doi: 10.1016/0022-3956(91)90005-u. [DOI] [PubMed] [Google Scholar]
- Burns L, Teesson M, O'Neill K. The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction. 2005;100(6):787–96. doi: 10.1111/j.1360-0443.2005.001069.x. [DOI] [PubMed] [Google Scholar]
- Charney DA, Paraherakis AM, Negrete JC, Gill KJ. The impact of depression on the outcome of addictions treatment. J Subst Abuse Treat. 1998;15(2):123–30. doi: 10.1016/s0740-5472(97)00183-9. [DOI] [PubMed] [Google Scholar]
- Chi FW, Satre DD, Weisner C. Chemical dependency patients with cooccurring psychiatric diagnoses: service patterns and 1-year outcomes. Alcohol Clin Exp Res. 2006;30(5):851–9. doi: 10.1111/j.1530-0277.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 2. Lawrence Erlbaum Associates, Inc; Mahwah, NJ: 1983. [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66(6):677–85. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Currie SR, Patten SB, Williams JV, Wang J, Beck CA, El-Guebaly N, Maxwell C. Comorbidity of major depression with substance use disorders. Can J Psychiatry. 2005;50(10):660–6. doi: 10.1177/070674370505001013. [DOI] [PubMed] [Google Scholar]
- Davidson KM, Blackburn IM. Co-morbid depression and drinking outcome in those with alcohol dependence. Alcohol Alcohol. 1998;33(5):482–7. doi: 10.1093/alcalc/33.5.482. [DOI] [PubMed] [Google Scholar]
- Dom G, De Wilde B, Hulstijn W, van den Brink W, Sabbe B. Decision-making deficits in alcohol-dependent patients with and without comorbid personality disorder. Alcohol Clin Exp Res. 2006;30(10):1670–7. doi: 10.1111/j.1530-0277.2006.00202.x. [DOI] [PubMed] [Google Scholar]
- Dowson J, Bazanis E, Rogers R, Prevost A, Taylor P, Meux C, Staley C, Nevison-Andrews D, Taylor C, Robbins T, Sahakian B. Impulsivity in patients with borderline personality disorder. Compr Psychiatry. 2004;45(1):29–36. doi: 10.1016/j.comppsych.2003.09.013. [DOI] [PubMed] [Google Scholar]
- Erdman HP, Klein MH, Greist JH, Skare SS, Husted JJ, Robins LN, Helzer JE, Goldring E, Hamburger M, Miller JP. A comparison of two computer-administered versions of the NIMH Diagnostic Interview Schedule. J Psychiatr Res. 1992;26(1):85–95. doi: 10.1016/0022-3956(92)90019-k. [DOI] [PubMed] [Google Scholar]
- Fein G, Di Sclafani V, Finn P, Scheiner DL. Sub-diagnostic psychiatric comorbidity in alcoholics. Drug Alcohol Depend. 2006a doi: 10.1016/j.drugalcdep.2006.08.009. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Klein L, Finn P. Impairment on a simulated gambling task in long-term abstinent alcoholics. Alcohol Clin Exp Res. 2004;28(10):1487–91. doi: 10.1097/01.alc.0000141642.39065.9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Landman B, Tran H, McGillivray S, Finn P, Barakos J, Moon K. Brain atrophy in long-term abstinent alcoholics who demonstrate impairment on a simulated gambling task. Neuroimage. 2006b;32(3):1465–71. doi: 10.1016/j.neuroimage.2006.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004a;61(8):807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004b;61(4):361–8. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: a prospective study. Arch Gen Psychiatry. 1998;55(3):259–65. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002;59(4):375–80. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. J Stud Alcohol. 1988;49(3):219–24. doi: 10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- Hesselbrock MN. Gender comparison of antisocial personality disorder and depression in alcoholism. J Subst Abuse. 1991;3(2):205–19. doi: 10.1016/s0899-3289(05)80037-9. [DOI] [PubMed] [Google Scholar]
- Hesselbrock MN, Meyer RE, Keener JJ. Psychopathology in hospitalized alcoholics. Arch Gen Psychiatry. 1985;42(11):1050–5. doi: 10.1001/archpsyc.1985.01790340028004. [DOI] [PubMed] [Google Scholar]
- Hunter EE, Powell BJ, Penick EC, Nickel EJ, Liskow BI, Cantrell PJ, Landon JF. Comorbid psychiatric diagnosis and long-term drinking outcome. Compr Psychiatry. 2000;41(5):334–8. doi: 10.1053/comp.2000.8997. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54(4):313–21. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug abuse: hedonic homeostatic dysregulation. Science. 1997;278(5335):52–8. doi: 10.1126/science.278.5335.52. [DOI] [PubMed] [Google Scholar]
- Levitan RD, Blouin AG, Navarro JR, Hill J. Validity of the computerized DIS for diagnosing psychiatric inpatients. Can J Psychiatry. 1991;36(10):728–31. [PubMed] [Google Scholar]
- Loosen PT, Dew BW, Prange AJ. Long-term predictors of outcome in abstinent alcoholic men. Am J Psychiatry. 1990;147(12):1662–6. doi: 10.1176/ajp.147.12.1662. [DOI] [PubMed] [Google Scholar]
- Mann K, Hintz T, Jung M. Does psychiatric comorbidity in alcohol-dependent patients affect treatment outcome? Eur Arch Psychiatry Clin Neurosci. 2004;254(3):172–81. doi: 10.1007/s00406-004-0465-6. [DOI] [PubMed] [Google Scholar]
- Mann RE, Sobell LC, Sobell MB, Pavan D. Reliability of a family tree questionnaire for assessing family history of alcohol problems. Drug Alcohol Depend. 1985;15(1–2):61–7. doi: 10.1016/0376-8716(85)90030-4. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23(6):893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Powell BJ, Landon JF, Cantrell PJ, Penick EC, Nickel EJ, Liskow BI, Coddington TM, Campbell JL, Dale TM, Vance MD, Rice AS. Prediction of drinking outcomes for male alcoholics after 10 to 14 years. Alcohol Clin Exp Res. 1998;22(3):559–66. doi: 10.1111/j.1530-0277.1998.tb04293.x. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. Jama. 1990;264(19):2511–8. [PubMed] [Google Scholar]
- Robins LN, Cottler L, Buckholz K, Compton W. The Diagnostic Interview Schedule for DSM-IV. Washington University School of Medicine; St. Louis, MO.: 1998. [Google Scholar]
- Ross HE. DSM-III-R alcohol abuse and dependence and psychiatric comorbidity in Ontario: results from the Mental Health Supplement to the Ontario Health Survey. Drug Alcohol Depend. 1995;39(2):111–28. doi: 10.1016/0376-8716(95)01150-w. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Arch Gen Psychiatry. 1987;44(6):505–13. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- Schuckit M. Alcoholic patients with secondary depression. Am J Psychiatry. 1983;140(6):711–4. doi: 10.1176/ajp.140.6.711. [DOI] [PubMed] [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl) 2001;158(4):343–59. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: measurement and validation. J Abnorm Psychol. 1982;91(3):199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Sheu WJ. Reliability of alcohol use indices. The Lifetime Drinking History and the MAST. J Stud Alcohol. 1982;43(11):1157–70. doi: 10.15288/jsa.1982.43.1157. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Self-reports issues in alcohol abuse: State of the art and future directions. Behaviorial Assessment. 1990;12:77–90. [Google Scholar]
- Sobell LC, Sobell MB, Riley DM, Schuller R, Pavan DS, Cancilla A, Klajner F, Leo GI. The reliability of alcohol abusers' self-reports of drinking and life events that occurred in the distant past. J Stud Alcohol. 1988;49(3):225–32. doi: 10.15288/jsa.1988.49.225. [DOI] [PubMed] [Google Scholar]
- SPSS 13.0 for Windows. computer program].Ver 13.0. Chicago IL: SPSS Inc; 2004. [Google Scholar]
- Stoltenberg SF, Mudd SA, Blow FC, Hill EM. Evaluating measures of family history of alcoholism: density versus dichotomy. Addiction. 1998;93(10):1511–20. doi: 10.1046/j.1360-0443.1998.931015117.x. [DOI] [PubMed] [Google Scholar]
- Tomasson K, Vaglum P. A nationwide representative sample of treatment-seeking alcoholics: a study of psychiatric comorbidity. Acta Psychiatr Scand. 1995;92(5):378–85. doi: 10.1111/j.1600-0447.1995.tb09600.x. [DOI] [PubMed] [Google Scholar]
- Westermeyer J, Thuras P. Association of antisocial personality disorder and substance disorder morbidity in a clinical sample. Am J Drug Alcohol Abuse. 2005;31(1):93–110. [PubMed] [Google Scholar]


