Abstract
151 neurologists at US epilepsy centers responded to a survey regarding stopping medications in patients following successful resective epilepsy surgery. 62% said patients should be ≥2 years seizure-free before stopping medication. While respondents tended to agree about the importance of many of the queried factors (e.g. focal pathology in favor of and persistent auras against stopping AEDs), it is unclear how well these factors determine seizure outcome in this setting.
Keywords: AEDs, epilepsy surgery, management policies, stopping drugs, survey
Introduction
Epilepsy surgery often brings about complete seizure freedom.1–4 Many patients and physicians then wish to stop antiepileptic drugs (AEDs). There is little evidence to guide this decision. Post-surgical seizure-free patients who taper with the intent of stopping AEDs experience about a 30% relapse rate.3, 5–7 In two of three studies, patients who tapered AEDs did not relapse more or less often than those who continued AEDs 3,7 The third reported a substantially higher risk in those who completely stopped AEDs;8 however, that was in comparison to a very low relapse rate in those who continued AEDs. The risk in those who stopped AEDs was comparable to that in the other two studies.
Patients who taper AEDs differ from those who do not taper in ways that are associated with relapse risk, regardless of treatment status.3, 6, 7, 9 Without a randomized trial, it is extremely difficult to disentangle the effect on relapse risk of patient-based differences from the effect of tapering AEDs.
To inform future observational studies and an eventual randomized trial, we surveyed US epilepsy center neurologists to assess the range of self-reported practices about AED discontinuation after surgery, including which factors influence their decisions, and for each factor they report as influencing those decisions, whether it weighs for or against AED discontinuation and its importance.
Methods
We identified centers through the National Association of Epilepsy Centers and the Early Randomized Surgery for Epilepsy Trial websites, supplemented by additional centers known to the investigators. Any adult neurologist at the center was eligible; each center was contacted to verify the neurologist’s eligibility. Three centers that refused to confirm their website’s information or were unreachable were excluded.
Surveys were mailed in March 2005 with a postage-paid return envelope and a $25 US gift card. Two subsequent surveys were mailed to non-respondents at one-month intervals. All procedures received Institutional Review Board approval.
The survey addressed eliminating one of several AEDs and separately, elimination of the last AED with the intent of rendering the patient drug-free (“stopping” AEDs). Because responses to the two situations were very similar, only results for the latter situation are reported here. Questions covered the minimum time a patient should be seizure-free and the frequency with which drug levels, an EEG, and an MRI should be obtained before stopping AEDs. For each of several factors, respondents were asked the extent to which each factor influenced their recommendation for or against stopping AEDs. Response choices were “sole/overriding,” “important in conjunction with other information,” “ancillary relative to other more important information,” or not influencing the decision or recommendation. Respondents could list additional factors perceived as important. Selected center and physician characteristics were assessed.
SAS version 9.1 was used to generate descriptive statistics and univariate distributions.
Results
Surveys were sent to 236 neurologists in 74 centers. Thirteen individuals were subsequently found ineligible. (Nine individuals responded that either they did not see many post surgical epilepsy patients or they were not physicians, despite their institutions’ earlier responses; four questionnaires were returned because the individuals no longer worked in the US). We received completed surveys from 151 (67.7%) out of 223 potentially eligible respondents representing 66 centers. Median number of respondents per represented center was 2 (range=1 to 6; Table 1). Missing data typically ranged from 2 to 5 per item.
Table 1.
Characteristics of respondents and centers
| Number of respondents per center | Number of centers | ||
|---|---|---|---|
| 1 | 22 | ||
| 2 | 20 | ||
| 3 | 14 | ||
| 4 | 5 | ||
| 5 | 3 | ||
| 6 | 2 | ||
| Completed epilepsy fellowship N (%) | 132 (89.8%) | ||
| Mean (SD) | Median [IQR] | Range | |
| Years since completing residency | 14.2 (8.4) | 13 [7.5, 20] | 2 – 38 |
| Number of adult postsurgical epilepsy patients under respondent’s care at a given time | 86 (125) | 40 [20, 100] | 0 – 1000 |
| Number of patients per year respondent reports as having resective surgery at center* | 42 (34) | 32 [20, 50] | 5 – 200 |
| Number of years respondent reports that epilepsy surgery program has been in operation* | 16.9 (8.2) | 15 [13, 20] | 2 – 50 |
When there were multiple respondents per center, the mean or median response for the center was used.
Nearly 90% of respondents had completed an epilepsy fellowship. There was a wide range in surgery patient volume and age of the surgery programs across centers (Table 1).
For stopping AEDs, 2% would recommend this after less than one year seizure-free, 25% indicated at least a year was necessary, and 62% felt a patient should be ≥2 years seizure-free before tapering the last drug. Three percent had no set opinion and 9% never recommended stopping all AEDs.
When stopping AEDs, 71.9% of respondents indicated they would obtain an EEG most or all of the time. MRIs were infrequently obtained and AED levels were more often than not obtained before stopping AEDs (Table 2).
Table 2.
Self-reported frequency of obtaining EEG, MRI, and AED levels prior to stopping AEDs.
| How often do you obtain the following before stopping AEDs?* | |||||
|---|---|---|---|---|---|
| Test (# of missing responses to specific question) | Almost never | <half the time | Half to 3/4s of time | Most of the time | Nearly always |
| EEG (2) | 9.4% | 13.4% | 5.4% | 14.8% | 57.1% |
| MRI (1) | 50.7% | 21.6% | 6.8% | 7.4% | 13.5% |
| AED level (2) | 19.6% | 12.2% | 13.5% | 16.2% | 38.5% |
Exact wording of question is “When you reduce the dosage of the last AED in post-surgical seizure-free patients with the intent of completely eliminating the AED, how often do you perform the following tests as a guide to clinical decision making before proceeding with the reduction? Please consider the patient who is on only one AED and in whom the intent is to have the patient off all AEDs.”
Quantitative ranges applied to descriptors were, “almost never,” <5% of the time; < half the time, 5–49%, half to three quarters, 50–74%; most of the time, 75–95%; nearly always, >95%.
With respect to factors influencing decision to stop AEDs (Figure 1), the patient’s desire to stop AEDs weighed in favor of stopping for 93% of respondents, but only 5% of respondents indicated that it was the sole basis for such a recommendation. Analogously, the patient’s desire to drive weighed against stopping AEDs according to 70% of respondents, but only one out of ten of these respondents (7% of the total sample) indicated this was a sole or overriding basis for that recommendation.
Figure 1.
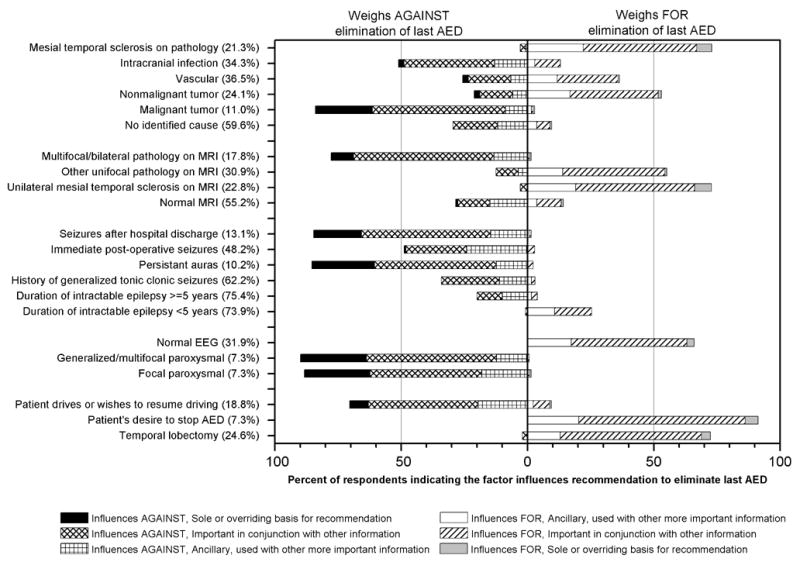
Percentage of respondents for each factor who indicate the factor influences for or against their recommendation to eliminate the last AED, as well as the level of importance of that factor (sole or overriding basis for recommendation; important in conjunction with other information; or ancillary, used with other more important information) in their recommendation or decision. The percent who indicated the factor does not influence the decision or are not sure is shown in parentheses. Data for age at onset, age at surgery, focal slowing on most recent post-surgical EEG, and nonspecific or generalized slowing on most recent post-surgical EEG are not shown as 71 to 83% of respondents indicated these factors did not influence the decision or were not sure.
The presence of paroxysmal EEG abnormalities weighed against eliminating drugs by about 9 out of 10 respondents; it was considered a sole or overriding factor by 26% of respondents. In contrast, focal slowing and nonspecific findings were of no influence for approximately 80% of respondents (not graphed).
Respondents were about evenly split regarding whether generalized tonic-clonic seizures before surgery and seizures in the immediate post-operative period influenced against or did not influence the decision to stop AEDs. By contrast, seizures after hospital discharge and persistent auras tended to weigh against stopping AEDs, with 25% citing persistent auras as an over-riding factor against stopping AEDs.
Unilateral mesial temporal sclerosis by MRI or on pathology weighed in favor of stopping AEDs for nearly three-fourths of respondents, but multifocal or bilateral findings on MRI weighed against AED elimination. A normal MRI was of no influence or only ancillary importance to most respondents. Responses for other pathologies varied considerably by specific pathology, except that almost 90% of respondents indicated that malignant tumors weighed against stopping AEDs.
Age at onset and age at surgery (not graphed) and duration of intractable epilepsy were not considered important by about three-quarters of respondents. In response to a question that allowed respondents to list any other factors they considered important in making recommendations about elimination of AEDs and not covered in the questionnaire, the three most common factors that were written in were medication side effects (n=28), pregnancy concerns (n=13), and cost of AEDs (n=7); no other factor was written in by more than 5 survey respondents.
In the event of a relapse, 71% said that typically they would restart the last AED that patient had been taking, 13% would start a different AED, and 16% would not restart AEDs.
Discussion
Little information is available to guide decisions to discontinue AEDs in post-surgical seizure-free patients. These results indicate what neurologists at US epilepsy centers report as relevant to this decision. There is moderate consensus regarding duration of seizure freedom before AED reduction. In addition, most respondents indicated that AED levels and an EEG, but not an MRI, are typically done before stopping AEDs. Generally, a good candidate for stopping drugs had a temporal lobectomy or well-defined focal pathology, is completely seizure-and aura-free after surgery, and does not have persistent EEG evidence of seizure susceptibility. Patients considered least appropriate are those with diffuse or multifocal disease, continued EEG evidence of seizure susceptibility, and seizures or auras after surgery.
There is little direct literature regarding prognostic factors for seizure outcomes after stopping AEDs in post-surgical patients. The apparent good agreement among respondents for factors such as paroxysmal EEG abnormalities may be due to neurologists generalizing from the literature on stopping AEDs in nonsurgical patients. However, factors for which there was substantial variation in reported practice (e.g. age at onset of epilepsy) suggest areas where there is very little evidence from any source to guide practice. It was unusual for respondents to say they would recommend stopping AEDs solely based on any single factor, including patient preferences. In contrast, many indicated that certain factors alone were sufficient to prevent them from recommending discontinuation of AEDs.
Regarding limitations of this study, self-reported practice styles and actual care may not be the same. In the survey instructions, respondents were told that if their response depended on the type of surgery, to “provide responses for your recommendations for patients who have undergone an anterior temporal lobectomy.” Thus, the responses likely primarily reflect approaches to patients who had anterior temporal lobectomies. However, this may have varied across respondents, and this variation cannot be teased apart.
Prior reports about stopping AEDs in post-surgical seizure free patients are observational and either retrospective or secondary analyses within larger studies. Thus, it is likely that patients selected to taper AEDs differ in their risk profiles from those who continue AEDs. In one study, those who tapered their AEDs were also more likely to have entered complete remission immediately after surgery compared with those who continued AEDs.7 Immediate remission was also strongly associated with a lower risk of recurrent seizures in general.9 Thus, any additional risk of stopping AEDs may have been masked by the fact that those who tapered their AEDs had an inherently lower recurrence risk than those whose AEDs were not tapered. After adjustment for this factor, there was still no discernible difference in recurrence risk associated with tapering AEDs, but that study was not designed to measure several other potentially important factors that might be associated with the risk of recurrence when tapering AEDs and with the decision itself to stop AEDs. Other studies have also described differences between patients who do and do not taper their AEDs. 3,6
Although observational studies can be designed to minimize confounding and to approach the validity of randomized trials,10 this requires a clear understanding of potential confounding factors. While this survey was not designed to evaluate prognostic importance of these factors, it does provide insight about what US epilepsy specialists report as their current practice styles – including areas of consensus and variation - important information in designing future studies of outcomes of AED discontinuation.
Supplementary Material
Acknowledgments
We thank Sandra Ruger for her assistance with performing this survey.
Footnotes
Supported by a grant from the National Institutes of Health, NINDS NS-32375
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Engel J, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy. Neurology. 2003;60:538–547. doi: 10.1212/01.wnl.0000055086.35806.2d. [DOI] [PubMed] [Google Scholar]
- 2.Wiebe S, Blume WT, Girvin JP, Eliasziw M. A randomized controlled trial of surgery for temporal-lobe epilepsy. N Eng J Med. 2001;345:311–318. doi: 10.1056/NEJM200108023450501. [DOI] [PubMed] [Google Scholar]
- 3.McIntosh AM, Kalnins RM, Mitchell RA, Fabinyi GCA, Briellmann RS, Berkovic SF. Temporal lobectomy: long-term seizure outcome, late recurrence and risks for seizure recurrence. Brain. 2004;2004:2018–2030. doi: 10.1093/brain/awh221. [DOI] [PubMed] [Google Scholar]
- 4.McIntosh AM, Wilson SJ, Berkovic SF. Seizure outcome after temporal lobectomy: current research practice and findings. Epilepsia. 2001;42:1288–1307. doi: 10.1046/j.1528-1157.2001.02001.x. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt D, Baumgartner C, Loscher W. Seizure recurrences after planned discontinuation of antiepileptic drugs in seizure-free patients following epilepsy surgery: A review of current clinical experience. Epilepsia. 2004;45:179–186. doi: 10.1111/j.0013-9580.2004.37803.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim YD, Heo K, Park SC, et al. Antiepileptic drug withdrawal after successful surgery for intractable temporal lobe epilepsy. Epilepsia. 2005;46:251–257. doi: 10.1111/j.0013-9580.2005.28004.x. [DOI] [PubMed] [Google Scholar]
- 7.Berg AT, Vickrey BG, Langfitt JT, et al. Reduction of AEDs in postsurgical patients who attain remission. Epilepsia. 2006;47:64–71. doi: 10.1111/j.1528-1167.2006.00371.x. [DOI] [PubMed] [Google Scholar]
- 8.Schiller Y, Cascino GD, So EL, Marsh WR. Discontinuation of antiepileptic drugs after successful epilepsy surgery. Neurology. 2000;54:346–349. doi: 10.1212/wnl.54.2.346. [DOI] [PubMed] [Google Scholar]
- 9.Spencer SS, Berg AT, Vickrey BG, et al. Predicting long-term seizure outcome after resective epilepsy surgery. Neurology. 2005;65:912–918. doi: 10.1212/01.wnl.0000176055.45774.71. [DOI] [PubMed] [Google Scholar]
- 10.Benson K, Hartz A. A comparison of observational studies and randomized controlled trials. N Eng J Med. 2000;342:1878–1886. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


