Abstract
Apoptosis in the liver is generated mainly by the Fas system. Tumour necrosis factor-related apoptosis-inducing ligand (TRAIL) has been proposed recently as a new apoptotic inducer. In the liver environment hepatocytes and biliary epithelial cells express TRAIL receptors which are up-regulated by increased levels of bile acids and during viral hepatitis. As for FasL, a soluble form of TRAIL has been described. To explore the commitment and level of activation of these two apoptotic systems in patients affected by primary biliary cirrhosis (PBC) or chronic hepatitis C (CH-C), a comparative study was drawn. Thirty patients with PBC on ursodeoxycholic acid have been enrolled. This group was compared with 30 patients with CH-C and with 20 healthy subjects. Soluble Fas ligand (sFasL) and soluble TRAIL (sTRAIL) levels were evaluated by double determinant immune assay and enzyme-linked immunosorbent assay (ELISA), respectively. Soluble FasL molecules were higher in PBC compared to CH-C (P = 0·009). Soluble FasL was not detected in controls. Soluble TRAIL was significantly higher in CH-C patients compared to PBC (P = 0·0001). Soluble TRAIL levels were higher in PBC and in CH-C than in controls (P = 0·015 and P < 0·001, respectively). No correlation between sFasL and sTRAIL, stage of disease, liver histology in each disease and cytolysis was present. Our data show different levels of commitment of TRAIL and Fas apoptosis-inducing systems in CH-C and PBC. Thus a different prominent role of TRAIL and Fas systems in the pathogenesis of these two conditions can be speculated: the former by inducing the death of infected hepatocytes, the latter by mediating the disappearance of bile duct.
Keywords: apoptosis, chronic hepatitis C, Fas, PBC, TRAIL
Introduction
Primary biliary cirrhosis (PBC) is a cholestatic liver disease in which only small bile ducts are destroyed, characterized serologically by the presence of anti-mitochondrial antibodies (AMA). The precise mechanisms of duct lesion and destruction are still unknown.
Several groups [1–5] have demonstrated that apoptosis occurs frequently in biliary epithelial cells (BECs), but the apoptotic trigger remains elusive.
The Fas receptor–Fas ligand (FasL) pathway is the most important apoptotic initiator in the liver [6], and increased expression of Fas has been demonstrated in BECs from PBC patients, as well as increased expression of FasL in infiltrating mononuclear cells [2].
The native and functional forms of Fas and FasL are membrane-bound proteins [2], but a soluble form can be generated from alternative mRNA splicing for soluble Fas (sFas) and metalloproteinase processing for soluble FasL (sFasL), with controversial function [7]. The pathogenic role of sFas and sFasL in PBC is still debated [1,8].
Tumour necrosis factor-related apoptosis-inducing ligand (TRAIL) has been proposed recently as a new apoptotic inducer in liver disease [9]. TRAIL is expressed by a wide variety of human cells, including T cells, monocytes, dendritic cells and natural killer cells.
At least five TRAIL receptors have been identified: receptors 4 and 5 (DR4 and DR5) are death receptors and activate the apoptosis signalling cascade, whereas receptors 1 and 2 and the soluble osteoprotegerin are decoy receptors, lacking the death domain transducing the death signal [10]. In the liver environment hepatocytes and BEC do express TRAIL receptors [11], which are up-regulated by increased levels of bile acids [12] and during viral hepatitis [13,14].
Although expressed primarily as type II transmembrane protein, TRAIL may exist in a soluble form (sTRAIL), generated either through enzymatic shedding, or realized in association with vesicles.
Similarly to sFasL, sTRAIL, the surface-bound molecule, was shown to induce apoptosis rapidly in susceptible tumour cells [15,16] and to inhibit T cell activation and proliferation [17]. Recently, we have shown high levels of sTRAIL in chronic hepatitis C (CH-C) [18], but no data are available on sTRAIL in PBC.
On such a basis, we have conducted a comparative study to evaluate sFasL and sTRAIL levels in peripheral blood of patients affected by PBC and chronic hepatitis C (CH-C), another chronic immunomediated liver disease, to explore the commitment and level of activation of these two apoptotic systems in these diseases.
Patients and methods
Patients
Thirty patients with PBC, 30 patients with CH-C and 20 healthy subjects were enrolled in this study. Patients' characteristics are summarized in Table 1. Written informed consent was obtained from all participants and the local ethical committee approved the study.
Table 1.
Patients' characteristics
| PBC | |
| No. of patients | 30 |
| Median age (range) | 62 (41–81) |
| Sex (male : female) | 1 : 29 |
| Mayo risk score (median and range) | 5·0 (3·7–10·0) |
| Histological stage: | |
| II | 18 |
| III | 12 |
| CH-C | |
| No. of patients | 30 |
| Median age (range) | 56 (26–77) |
| Sex (male : female) | 21 : 9 |
| HCV genotype (1 : not 1) | 12 : 18 |
| Controls | |
| No. of patients | 20 |
| Median age (range) | 35 (24–40) |
| Sex (male : female) | 8 : 12 |
PBC was diagnosed by positive anti-mitochondrial antibodies, alkaline phosphatase 1·5 times above the normal limit and compatible liver histology. All PBC patients were hepatitis B surface antigen- and antibody to HIV and hepatitis C virus HCV)-negative; they were taking ursodeoxycholic acid (12–13 mg/kg/day). Histological examination showed patients with 18 stage II and 12 stage IV.
All CH-C patients were hepatitis B surface antigen- and antibody to HIV-negative; they were naive to any anti-viral treatment and no cirrhosis was present in the liver biopsy. HCV RNA was detectable in all patients (Cobas Amplicor HCV Monitor; cut-off 1000 copies/ml; Roche Spa, Milan, Italy).
Blood samples from patients and healthy donors were centrifuged shortly after clot formation. All samples were stored at −80°C in aliquots and thawed only before the test.
Measurements of soluble molecules sFasL
Concentrations of sFasL were determined by double determinant immune assay. Briefly, 96-well polyvinylchloride microtitre plates (Becton Dickinson, Oxnard, CA, USA) were coated overnight at 4°C with a solution of monoclonal antibody (MoAb) NOK-2 (10 µg/ml) in NaHCO3 buffer. After three washings with 0·05% Tween 20/phosphate-buffered saline (PBS), the wells were blocked by 10% antibody serum for 1 h at 37°C. After additional washings, biotinylated MoAb NOK-1 (5 µg/ml) was added and incubated for 1 h at 37°C. After additional washings, peroxidase-conjugated streptavidin (Pierce, Rockford, IL, USA) was added at a concentration of 1 µg/ml for 1 h at 37°C. Plates were developed with 100 µl of 1 mg/ml orthophenylenediamine in 50 mmol/l citrate phosphate buffer (pH 5·0) containing 0·03% H2O2 and stopped with 100 µl of 2 N H2SO4. Optical density was measured at 490 nm on at automated enzyme-linked immunosorbent assay (ELISA) reader. Serial dilutions (0·1–100 ng/ml) of human recombinant sFasL (Alexis, Co, Läufelfingen, Switzerland) were used to construct the standard curve and results were expressed as nanograms per millilitre.
sTRAIL
Concentrations of sTRAIL were measured using a commercially available solid phase sandwich ELISA kit (soluble TRAIL/apo2L from Diaclone Research, Besançon, France) according to the manufacturer's instructions.
Briefly, 100 µl of sample or diluted standard in duplicate were added to the plate wells precoated with a monoclonal antibody specific for sTRAIL. Then, 50 µl of diluted biotinylated anti-sTRAIL antibody was added to all wells and the plate was incubated for 3 h at room temperature. After thorough washing, 100 µl of streptavidin–horseradish peroxidase (HRP)-conjugate was added and the plate was incubated for 30 min at room temperature. Plates were developed with tetramethylbenzidine (TMB) substrate solution and optical density was measured on a spectrophotometer using 450 nm as the primary wave length and optionally 620 nm as the reference wavelength.
Statistical analysis
The results were analysed with nonparametric tests (χ2, Wilcoxon, Mann–Whitney U-test and Spearman's rank correlation tests) as appropriate. All calculations were performed on a personal computer with Statistica (StatSoft, Tulsa, OK, USA).
Results
Soluble FasL levels
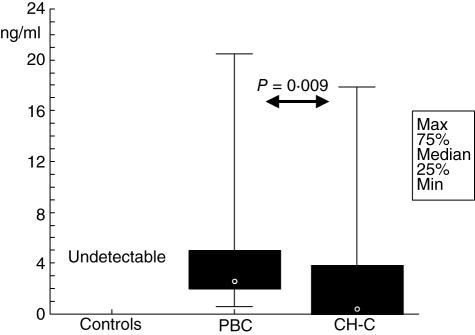
Soluble FasL was not detectable in controls, while it was elevated significantly in PBC and in CH-C patients. Soluble FasL was higher in PBC patients compared to CH-C (P = 0·009) (Fig. 1). Values expressed as median and range were: 2·63 ng/ml (0·57–20·50 ng/ml) for PBC and 0·22 ng/ml (0·0–17·84 ng/ml) for CH-C.
Fig. 1.
Soluble Fas ligand (sFasL) in controls, primary biliary cirrhosis (PBC) and chronic hepatitis C (CH-C). PBC and CH-C present high levels of sFasL, which is undetectable in controls. Soluble FasL is higher in PBC than in CH-C.
No correlation between sFasL and the histological stage of the disease or with the Mayo score was found in PBC patients. In CH-C patients no correlation between sFasL and both cytolysis [expressed as alanine amino transferase (ALT) levels] and HCV viraemia was present.
sTRAIL levels
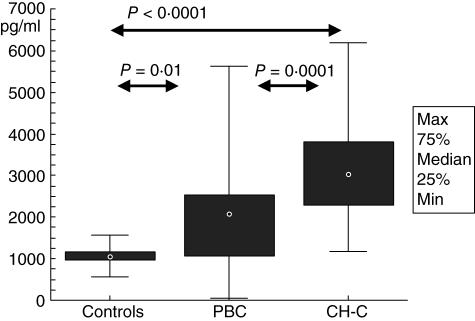
sTRAIL levels were significantly higher in PBC and in CH-C patients than in controls (P = 0·01) (Fig. 2). Values expressed as median and range were: 1045 pg/ml (573–1558 pg/ml) for healthy subjects, 2968 pg/ml (43–5620 pg/ml) for PBC and 3038 pg/ml (1181–6183 pg/ml) for CH-C. Soluble TRAIL was higher in CH-C patients compared to PBC (P = 0·0001).
Fig. 2.
Soluble tumour necrosis factor-related apoptosis-inducing ligand (sTRAIL) in controls, primary biliary cirrhosis (PBC) and chronic hepatitis C (CH-C). PBC and CH-C present higher levels than controls and sTRAIL is higher in PBC than in CH-C.
Similarly to sFasL, sTRAIL levels correlated neither with the severity of the disease (histology and Mayo score) in PBC patients nor with cytolysis or HCV viraemia in CH-C patients.
Discussion
Several levels of evidence indicate that apoptosis is the major mode of cell death in most liver disease [19].
In this study we have shown that soluble pro-apoptotic molecules are elevated significantly in PBC and in CH-C patients compared to healthy subjects. This indicates an overall activation of the soluble pathway of apoptosis, which correlates with the tissue-bound activation mechanisms described previously in these diseases [2,11,20].
We have observed higher serum concentrations of sFasL in PBC than in CH-C patients. Although the Fas/FasL system has been proved widely to be pathogenic in PBC [2], the demonstration of sFasL presence in peripheral blood is still controversial [1,8], due to the different methodological approach, to the different patient characteristics, or treatment. Our study provides further evidence of an increased concentration of sFasL in PBC, confirming an activated efferent arm of the Fas system, while no differences related to the histological stage of disease were found.
A significantly higher expression of sTRAIL was found in CH-C compared to PBC. This observation on serum soluble molecules is in agreement with previous studies on liver tissue, which reported an up-regulation of TRAIL receptors (DR4 and DR5) and over-expression of TRAIL in hepatitis virus infection [13,14,21], thereby activating the TRAIL-specific death pathway solely in infected hepatocytes [14]. Moreover, high levels of sTRAIL have been demonstrated recently for hepatitis B virus [22] and by our group for hepatitis C virus [18]. The over-expression of TRAIL and sTRAIL in viral hepatitis could be seen as a defensive mechanism to eliminate infected cells and limit viral replication.
More intriguing is the sTRAIL behaviour in PBC. TRAIL receptors are expressed on BECs and bile acid up-regulates TRAIL receptors in hepatocytes, sensitizing them to TRAIL-mediated apoptosis [12,23] and suggesting that TRAIL may be hepatotoxic in cholestasis. Our data on serum soluble molecules mirror these previous histological findings, showing increased levels in the context of an up-regulation of the apoptosis system.
It can be argued that all our patients were receiving treatment with ursodeoxycholic acid, which has been shown to protect against apoptosis [24]. This makes a definitive evaluation of sTRAIL in PBC difficult, and suggests a comparative study before and after therapy to be useful. The same consideration has to be established for the duration of the treatment.
The lack of correlation between biochemical disease activity and clinical or histological state, on one hand, and soluble pro-apoptotic molecules on the other hand, deserves two considerations.
First, it is known that apoptosis may occur in the absence of significant transaminase elevation, thereby confirming the lack of correlation between biochemical activity and liver cell histological injury [25].
Secondly, clearance of apoptosis debris through phagocytosis may directly stimulate fibrogenesis [26], but fibrosis occurs over a long period of time, whereas soluble molecule expression is likely to be more dynamic, so that a linear relationship between these two processes is difficult to demonstrate.
One interesting point, which needs to be addressed in future studies, is the impact of the different sex distribution in the two diseases. The 90% predominance of females in PBC is well known, while among CH-C patients a large majority of men is present [27]. However, although our cohort is clearly not adequate to underline possible gender or age influences on pro-apoptotic molecule levels, Choi et al. report no significant age- and gender-related differences in Fas and TRAIL concentrations [28,29].
In conclusion, our findings indicate the possibility of evaluating the level of activation of these two apoptosis systems in liver diseases by their soluble molecules, which appear to reflect the histological findings. Studies able to show a linear correspondence between histological expression and serum levels of these molecules are therefore warranted.
Moreover, our data show different levels of commitment of TRAIL- and Fas apoptosis-inducing systems in the CH-C and PBC. Thus, a different prominent role of TRAIL and Fas systems in the pathogenesis of these two conditions can be speculated: the former by inducing the death of infected hepatocytes, the latter by mediating the disappearance of bile duct.
References
- 1.Gozlan J, Nion I, Chazouilleres O, et al. Soluble Fas is increased in serum of patients with primary biliary cirrhosis, but is not a useful marker for disease activity. Am J Gastroenterol. 2000;95:3328–9. doi: 10.1111/j.1572-0241.2000.03327.x. [DOI] [PubMed] [Google Scholar]
- 2.Harada K, Ozaki S, Gershwin ME, et al. Enhanced apoptosis relates to bile duct loss in primary biliary cirrhosis. Hepatology. 1997;26:1399–405. doi: 10.1002/hep.510260604. [DOI] [PubMed] [Google Scholar]
- 3.Harada K, Kono N, Tsuneyama K, et al. Cell-kinetic study of proliferating bile ductules in various hepatobiliary diseases. Liver. 1998;18:277–84. doi: 10.1111/j.1600-0676.1998.tb00166.x. [DOI] [PubMed] [Google Scholar]
- 4.Koga H, Sakisaka S, Ohishi M, et al. Nuclear DNA fragmentation and expression of Bcl-2 in primary biliary cirrhosis. Hepatology. 1997;25:1077–84. doi: 10.1002/hep.510250505. [DOI] [PubMed] [Google Scholar]
- 5.Tinmouth J, Lee M, Wanless IR, et al. Apoptosis of biliary epithelial cells in primary biliary cirrhosis and primary sclerosing cholangitis. Liver. 2002;22:228–34. doi: 10.1046/j.0106-9543.2002.01595.x. [DOI] [PubMed] [Google Scholar]
- 6.Faubion WA, Guicciardi ME, Miyoshi H, et al. Toxic bile salts induce rodent hepatocyte apoptosis via direct activation of Fas. J Clin Invest. 1999;103:137–45. doi: 10.1172/JCI4765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strasser A, O'Connor L. Fas ligand − caught between Scylla and Charybdis. Nat Med. 1998;4:21–2. doi: 10.1038/nm0198-021. [DOI] [PubMed] [Google Scholar]
- 8.Tortorella C, Sacco R, Orlando P, et al. sICAM-1, sCD95 and sCD95L levels in chronic liver diseases of different etiology. Immunopharmacol Immunotoxicol. 2000;22:19–33. doi: 10.3109/08923970009016403. [DOI] [PubMed] [Google Scholar]
- 9.Zheng SJ, Wang P, Tsabary G, et al. Critical roles of TRAIL in hepatic cell death and hepatic inflammation. J Clin Invest. 2004;113:58–64. doi: 10.1172/JCI200419255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sheridan JP, Marsters SA, Pitti RM, et al. Control of TRAIL-induced apoptosis by a family of signaling and decoy receptors. Science. 1997;277:818–21. doi: 10.1126/science.277.5327.818. [DOI] [PubMed] [Google Scholar]
- 11.Spierings DC, de Vries EG, Vellenga E, et al. Tissue distribution of the death ligand TRAIL and its receptors. J Histochem Cytochem. 2004;52:821–31. doi: 10.1369/jhc.3A6112.2004. [DOI] [PubMed] [Google Scholar]
- 12.Higuchi H, Grambihler A, Canbay A, et al. Bile acids up-regulate death receptor 5/TRAIL-receptor 2 expression via a c-Jun N-terminal kinase-dependent pathway involving Sp1. J Biol Chem. 2004;279:51–60. doi: 10.1074/jbc.M309476200. [DOI] [PubMed] [Google Scholar]
- 13.Janssen HL, Higuchi H, Abdulkarim A, et al. Hepatitis B virus enhances tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) cytotoxicity by increasing TRAIL-R1/death receptor 4 expression. J Hepatol. 2003;39:414–20. doi: 10.1016/s0168-8278(03)00265-4. [DOI] [PubMed] [Google Scholar]
- 14.Mundt B, Kuhnel F, Zender L, et al. Involvement of TRAIL and its receptors in viral hepatitis. FASEB J. 2003;17:94–6. doi: 10.1096/fj.02-0537fje. [DOI] [PubMed] [Google Scholar]
- 15.Wiley SR, Schooley K, Smolak PJ, et al. Identification and characterization of a new member of the TNF family that induces apoptosis. Immunity. 1995;3:673–82. doi: 10.1016/1074-7613(95)90057-8. [DOI] [PubMed] [Google Scholar]
- 16.Hao C, Song JH, Hsi B, et al. TRAIL inhibits tumor growth but is nontoxic to human hepatocytes in chimeric mice. Cancer Res. 2004;64:8502–6. doi: 10.1158/0008-5472.CAN-04-2599. [DOI] [PubMed] [Google Scholar]
- 17.Lunemann JD, Waiczies S, Ehrlich S, et al. Death ligand TRAIL induces no apoptosis but inhibits activation of human (auto)antigen-specific T cells. J Immunol. 2002;168:4881–8. doi: 10.4049/jimmunol.168.10.4881. [DOI] [PubMed] [Google Scholar]
- 18.Pelli N, Torre F, Delfino A, et al. Soluble tumor necrosis factor-related ligand (sTRAIL) levels and kinetics during antiviral treatment in chronic hepatitis C. J Interferon Cytokine Res. 2006;26:119–23. doi: 10.1089/jir.2006.26.119. [DOI] [PubMed] [Google Scholar]
- 19.Jaeschke H, Gujral JS, Bajt ML. Apoptosis and necrosis in liver disease. Liver Int. 2004;24:85–9. doi: 10.1111/j.1478-3231.2004.0906.x. [DOI] [PubMed] [Google Scholar]
- 20.Fox CK, Furtwaengler A, Nepomuceno RR, et al. Apoptotic pathways in primary biliary cirrhosis and autoimmune hepatitis. Liver. 2001;21:272–9. doi: 10.1034/j.1600-0676.2001.021004272.x. [DOI] [PubMed] [Google Scholar]
- 21.Sedger LM, Shows DM, Blanton RA, et al. IFN-gamma mediates a novel antiviral activity through dynamic modulation of TRAIL and TRAIL receptor expression. J Immunol. 1999;163:920–6. [PubMed] [Google Scholar]
- 22.Han LH, Sun WS, Ma CH, et al. Detection of soluble TRAIL in HBV infected patients and its clinical implications. World J Gastroenterol. 2002;8:1077–80. doi: 10.3748/wjg.v8.i6.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higuchi H, Bronk SF, Taniai M, et al. Cholestasis increases tumor necrosis factor-related apoptotis-inducing ligand (TRAIL)-R2/DR5 expression and sensitizes the liver to TRAIL-mediated cytotoxicity. J Pharmacol Exp Ther. 2002;303:461–7. doi: 10.1124/jpet.102.040030. [DOI] [PubMed] [Google Scholar]
- 24.Rodrigues CM, Fan G, Ma X, et al. A novel role for ursodeoxycholic acid in inhibiting apoptosis by modulating mitochondrial membrane perturbation. J Clin Invest. 1998;101:2790–9. doi: 10.1172/JCI1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kountouras J, Zavos C, Chatzopoulos D. Apoptosis in hepatitis C. J Viral Hepatol. 2003;10:335–42. doi: 10.1046/j.1365-2893.2003.00452.x. [DOI] [PubMed] [Google Scholar]
- 26.Canbay A, Friedman S, Gores GJ. Apoptosis: the nexus of liver injury and fibrosis. Hepatology. 2004;39:273–8. doi: 10.1002/hep.20051. [DOI] [PubMed] [Google Scholar]
- 27.Sherlock S, Dooley J. Diseases of the liver and biliary system. 11. Oxford: Blackwell Publishing; 2002. [Google Scholar]
- 28.Choi JW, Song JS, Pai SH. Associations of serum TRAIL concentrations, anthropometric variables, and serum lipid parameters in healthy adults. Ann Clin Lab Sci. 2004;34:400–4. [PubMed] [Google Scholar]
- 29.Choi JW. Associations of Fas (CD95), tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL), and biochemical manifestations in elderly persons. Clin Chim Acta. 2006;365:113–8. doi: 10.1016/j.cca.2005.08.004. [DOI] [PubMed] [Google Scholar]