Abstract
Mannan-binding lectin (MBL) is a collectin plasma protein activating the lectin pathway of the complement system, enhancing opsonophagocytosis and modulating the cytokine response to inflammation. Deficiency of MBL, caused by structural mutations or promoter polymorphisms in the MBL2 gene, has been associated with increased susceptibility to infection and autoimmune disease. Thus, as infective endocarditis remains a severe disease requiring intensive and long-term treatment with antibiotics, we examined whether there was an association between MBL and clinical outcome in 39 well-characterized patients with infective endocarditis. Five patients (13%) had MBL concentrations < 100 µg/l and were considered MBL-deficient. This proportion was similar to that in a healthy control group of blood donors. Mortality 3 months after diagnosis was 20% in patients with MBL-deficiency and 9% in patients with normal MBL. The 5-year mortality was 80% and 25%, respectively. MBL-deficiency was on univariate survival statistics associated with significantly higher mortality on follow-up (P= 0·03). In conclusion, this is the first report of an association between MBL-deficiency and survival in infective endocarditis. The present observation is important, as replacement therapy in MBL-deficient patients is possible. For certain high-risk subgroups, it opens new perspectives for improvement of treatment and outcome in infective endocarditis.
Keywords: infective endocarditis, innate immune system, mannan-binding lectin deficiency, mannan-binding lectin
Introduction
Infective endocarditis remains a serious condition with high mortality, despite improvements in diagnostics and treatment. Recent investigations have reported a short-term mortality of 14–15% and long-term 5-year mortality of around 40%. A number of risk factors for poor outcome have been identified. Staphylococcus aureus endocarditis, prosthetic valve endocarditis and high age are associated with higher mortality, whereas surgery is associated with lower mortality [1–3].
Mannan-binding lectin (MBL) is a member of a family of Ca2+-dependent collagenous lectins, most of which are components of the innate immune system. It is secreted by the liver and exhibits acute phase reactant behaviour. MBL binds to carbohydrate structures on the surface of microorganisms and mediates deposition of complement factors using MBL-associated serine protease 2 (MASP-2) for activation of the lectin pathway of the complement cascade [4–6]. Structural mutations or promoter polymorphisms in the MBL2 gene, coding for MBL, are associated with low plasma concentration of MBL [7] and a blunted acute phase response during infections. This causes defective opsonization and phagocytosis and has been associated with recurrent and chronic infections in infants as well as in adults [8,9]. Thus, MBL-deficiency has been associated with poorer outcome of human immunodeficiency virus infection, cystic fibrosis, systemic lupus erythromatosus and sepsis [10–13].
On this basis, the purpose of the present investigation was to evaluate whether MBL-deficiency may affect the outcome of infective endocarditis. Hence, we examined the serum concentration of MBL in 39 well-characterized patients with infective endocarditis and examined for an association between MBL-deficiency and mortality.
Materials and methods
Patients
Thirty-nine Danish patients with infective endocarditis with serum samples available for diagnostic purposes were recruited from an endocarditis cohort of consecutively diagnosed patients at Rigshospitalet, Copenhagen University Hospital [3]. Causes of death in deceased patients were extracted from the official death certificates. Controls were 234 blood donors from Rigshospitalet, Copenhagen University Hospital. The study was approved by the regional Science Ethics Committee (KF-01319107).
MBL quantification
Serum samples preserved with sodium azide had been stored at − 80°C until analysis. Concentrations of MBL in serum were measured by a time-resolved immunofluorometric (TrIFMA) assay essentially as described earlier [14,15] with the modification that polystyrene coating with antibody was conducted in phosphate-buffered saline. Values above 3000 µg/l were truncated. Cut-off between normal and MBL-deficiency was chosen to be 100 µg/l, as the log-concentration frequency distribution in the control group was bimodal and had local minimum at approximately 100 µg/l.
Statistics
Contingency tables were tested with Fisher's exact test. Survival analysis was performed ad modum Kaplan–Meyer. Univariate analysis was performed with the log-rank test. Statistical analysis was performed using the InStat 3·0 and Prism 4·0 programs from GraphPad Software Inc. (San Diego, California, USA).
Results
Median MBL concentration in the 39 patients was 2649 µg/l; 17 patients had MBL concentration > 3000 µg/l. Five patients (13%) had MBL concentration below 100 µg/l and were considered MBL-deficient. Five, 10 and 20 percentiles were 22, 31 and 350 µg/l, respectively. In controls, the median MBL concentration was somewhat lower with a median in the 234 blood donors of 1992 µg/l. MBL concentration was below 100 µg/l in 26 (11%) controls. The 5, 10 and 20 percentiles were 14, 65 and 433 µg/l, respectively.
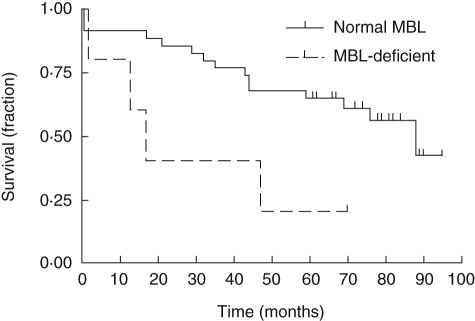
MBL-deficient patients were, on average, 12 years older than those with normal MBL (Table 1). There were no statistically significant differences in other baseline clinical characteristics between patients with MBL-deficiency and patients with normal MBL. However, we observed a trend towards a higher proportion of MBL-deficiency in patients with prosthetic valve endocarditis [two of eight (25%) versus three of 31 (10%), P = 0·27] and in patients treated without surgery [four of 16 (25%) versus one of 23 (4%), P = 0·14]. Survival from infective endocarditis in patients with MBL-deficiency and normal MBL was evaluated ad modum Kaplan–Meyer (Fig. 1). A significantly higher mortality in the patients with MBL-deficiency was observed (P= 0·03). The curves indicate that the mortality rate for MBL-deficient patients was twice as high as for patients with normal MBL. Mortality after 3 months was 20% and 9% in the patients with MBL-deficiency and normal MBL, respectively. The 5-year mortality was 80% and 35%, respectively, for the two groups.
Table 1.
Demographic and clinical data related to MBL
| Normal MBL | MBL-deficient | |
|---|---|---|
| Patients | 34 | 5 |
| Age | ||
| Median | 54 | 65 |
| Average | 50 | 62 |
| Gender | ||
| Male | 15 | 3 |
| Female | 19 | 2 |
| Native/prosthetic valve | ||
| NVE | 28 | 3 |
| PVE | 6 | 2 |
| Valve affected | ||
| Aortic | 13 | 3 |
| Mitral | 11 | 1 |
| Aortic + mitral | 5 | 0 |
| Tricuspid | 3 | 0 |
| Aortic + mitral + tricuspid | 1 | 0 |
| Not determined | 1 | 1 |
| Microbiology | ||
| Staphylococcus aureus | 7 | 2 |
| Staphylococci, coag.neg. | 4 | 0 |
| Viridans streptococci | 8 | 0 |
| Other streptococci | 1 | 0 |
| Enterococcus faecalis | 4 | 1 |
| Other | 2 | 0 |
| Culture-negative | 8 | 2 |
| Valve surgery | ||
| Yes | 22 | 1 |
| No | 12 | 4 |
| Intravenous drug abuse | ||
| Yes | 3 | 0 |
| No | 31 | 5 |
Fig. 1.
Survival from infectious endocarditis in patients with normal mannan-binding lectin (MBL) and MBL-deficiency. Survival in 39 patients with infectious endocarditis stratified to MBL plotted ad modum Kaplan–Meyer as a function of observation time after infective endocarditis was diagnosed. MBL was determined in serum as described earlier [14,15]. Patients with MBL < 100 µg/l were considered MBL-deficient.
Survival was stratified further for microorganisms. No statistically significant differences were found in mortality between patients with normal MBL and MBL-deficient patients when comparing the various single groups of bacteria. However, in S. aureus endocarditis there was a trend towards higher mortality in patients with MBL deficiency. Thus, the 5-year mortality was 100% in MBL-deficient patients and 29% in patients with normal MBL (P= 0·17).
During the follow-up period of up to 95 months a total of 19 patients died − four MBL-deficient patients and 15 patients with normal MBL. The cause of death as ascertained from death certificates was cardiac-related diseases in 16 (84%) patients; two (11%) patients died from non-cardiac infections and one (5%) patient died from extracardial vascular thrombosis.
Discussion
The important observation in the present study is that MBL-deficient patients (serum MBL concentration < 100 µg/l) with infective endocarditis had around twice the mortality rate compared to patients with normal MBL. To our knowledge this is the first time that an association between survival from infective endocarditis and MBL-deficiency is reported.
MBL-deficiency has been reported previously to influence the course of infection with S. aureus in humans as well as in animal models. Thus, after binding to S. aureus, human MBL has been found to enhance complement activation and opsonophagocytosis [16]. In mice devoid of MBL activity, it was found that all died within 48 h after intravenous exposure to S. aureus, whereas the mortality was only 45% in normal control mice [17]. These observations correspond well to the trend towards higher mortality associated with MBL-deficiency among patients with S. aureus endocarditis in the present study. In vitro experiments have shown that MBL binds to S. aureus but not to viridans streptococci [18], which could explain why MBL-deficiency might be of importance for the clinical course of S. aureus infection but not viridans streptococcus infection. MBL-deficiency has been associated with familial recurrent staphylococcal furunculosis supporting a particular role for MBL in the defence against staphylococcal infections [19]. Similarly, the risk of invasive meningococcal disease is increased in MBL-deficient children [20].
However, the mechanism behind the increased mortality in MBL-deficient patients with endocarditis is not necessarily explained solely by an interaction of MBL with the microorganism. Thus, this mechanism is considered to be of significance only in the early phase of infection, e.g. in post-burn infections with Pseudomonas aeruginosa in mice [21]. Another mechanism could be modulation of the cytokine response to a chronic inflammation/infection, as has been demonstrated for MBL in rheumatoid arthritis [22], human immunodeficiency virus infection [23] and systemic inflammatory syndrome [24]. Interestingly, the clinical significance of MBL-deficiency disappears in conditions with severe granulocytopenia [25], further suggesting that MBL functions as a modulator of the immune system. The present evaluation of death certificates showed that 84% of deaths were registered as caused primarily by cardiac disease. Of course, death certificates sampled retrospectively without post mortem should be evaluated with caution. However, the observation is interesting, as it has been shown that variant MBL alleles in combination with a positive Clamydia titre is associated with accelerated arteriosclerosis [26,27]. Taken together, this may indicate that the higher long-term mortality from infective endocarditis in MBL-deficient patients compared to patients with normal MBL levels may be due, in part, to increased progression of arteriosclerosis. The precise mechanisms of the interaction between MBL and long-term survival in coronary artery disease as well as the mechanism of decreased survival demonstrated in the present study are, however, not yet known. A more complex mechanism might be the interference of innate immune activation with endocrine functions in MBL-deficient patients, as suggested from the finding of a defective reproductive endocrinological function in mice stimulated by CD40 ligation [28], which mimics downstream modulation from the innate immune system. These reports provide further evidence for the importance of MBL, although a previous study found no statistically significant association between general mortality and MBL-deficiency [29].
It should be noted that the proportion of MBL-deficient patients of the study cohort was not different from the normal population [14], as confirmed by comparing our patients with the control group of healthy blood donors. Thus, MBL does not seem to protect against infection, but when infection occurs it may be deleterious for MBL-deficient patients. Our finding of a 33% higher median MBL concentration in infected patients compared to controls is compatible with the known acute phase reactant behaviour of MBL [5]. It should be noted that the present MBL-deficient patients were, on average, 12 years older than those with normal MBL. Thus, influence of comorbidity on mortality in MBL-deficient patients cannot be excluded. Furthermore, a minor decrease in MBL concentration with age may contribute towards lower MBL concentration [30]. MBL-deficiency in the present study had a tendency towards being more common in patients with prosthetic valve endocarditis and in patients treated without surgery. These two factors have been associated previously with higher mortality [1,3]. Thus, in addition to MBL-deficiency, they could contribute to a higher mortality in this group.
In the present study we assessed serum concentrations of MBL. We have minimized the importance of not genotyping by choosing a low cut-off level (100 µg/l) between normal levels and MBL-deficiency. In agreement, Minchinton et al. [7] found good separation using similar cut-off level and reported a close association between MBL levels and the MBL2 genotype. At variance, others have published studies using higher cut-off levels.
The present study should form the basis for initiation of large-scale prospective studies evaluating MBL in infective endocarditis. Clearly, such studies should also include full-blood sampling for MBL genotyping. Furthermore, the present findings could form the basis for improvements in the treatment of patients with infective endocarditis. MBL replacement therapy has been shown to be safe [31] and could be used experimentally, particularly in patients with bacteria to which MBL binds, including S. aureus. In addition, the identification of MBL-deficiency as a risk factor for severe outcome may contribute to the identification of patients at risk of infective endocarditis and for whom special preventive measures should be taken. At exposure to bacteria they should be ensured efficient antibiotic prophylaxis and follow-up with blood cultures. A clear definition of the routine indication for MBL substitution in patients with infective endocarditis and the prospect of MBL as prophylaxis in selected high-risk cases will have to await clinical studies.
Acknowledgments
Lone Rabøl is thanked for technical assistance with the MBL analysis. Novo Nordisk Foundation, the Lundbeck Foundation, Rigshospitalets Research Council, the Danish National Research Foundation, the Villadsen Family Foundation and the Jeppe & Ovita Juhls Foundation are thanked for financial support.
References
- 1.Bishara J, Leibovici L, Gartman-Israel D, et al. Long-term outcome of infective endocarditis: the impact of early surgical intervention. Clin Infect Dis. 2001;33:1636–43. doi: 10.1086/323785. [DOI] [PubMed] [Google Scholar]
- 2.Pedersen SA, Foghsgaard J, Launbjerg J. [Infectious endocarditis in the county of Frederiksborg, 1990–2000. Clinical findings and prognostic aspects] 2. Ugeskr Laeger. 2004;166:2441–6. [PubMed] [Google Scholar]
- 3.Tran CT, Kjeldsen K. Endocarditis at a tertiary hospital: reduced acute mortality but poor long term prognosis. Scand J Infect Dis. 2006;38:664–70. doi: 10.1080/00365540600585180. [DOI] [PubMed] [Google Scholar]
- 4.Kuhlman M, Joiner K, Ezekowitz RA. The human mannose-binding protein functions as an opsonin. J Exp Med. 1989;169:1733–45. doi: 10.1084/jem.169.5.1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thiel S, Holmskov U, Hviid L, Laursen SB, Jensenius JC. The concentration of the C-type lectin, mannan-binding protein, in human plasma increases during an acute phase response. Clin Exp Immunol. 1992;90:31–5. doi: 10.1111/j.1365-2249.1992.tb05827.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmskov U, Thiel S, Jensenius JC. Collections and ficolins: humoral lectins of the innate immune defense. Annu Rev Immunol. 2003;21:547–78. doi: 10.1146/annurev.immunol.21.120601.140954. [DOI] [PubMed] [Google Scholar]
- 7.Minchinton RM, Dean MM, Clark TR, Heatley S, Mullighan CG. Analysis of the relationship between mannose-binding lectin (MBL) genotype, MBL levels and function in an Australian blood donor population. Scand J Immunol. 2002;56:630–41. doi: 10.1046/j.1365-3083.2002.01167.x. [DOI] [PubMed] [Google Scholar]
- 8.Petersen SV, Thiel S, Jensenius JC. The mannan-binding lectin pathway of complement activation: biology and disease association. Mol Immunol. 2001;38:133–49. doi: 10.1016/s0161-5890(01)00038-4. [DOI] [PubMed] [Google Scholar]
- 9.Turner MW, Hamvas RM. Mannose-binding lectin: structure, function, genetics and disease associations. Rev Immunogenet. 2000;2:305–22. [PubMed] [Google Scholar]
- 10.Jack DL, Turner MW. Anti-microbial activities of mannose-binding lectin. Biochem Soc Trans. 2003;31:753–7. doi: 10.1042/bst0310753. [DOI] [PubMed] [Google Scholar]
- 11.Garred P, Pressler T, Lanng S, et al. Mannose-binding lectin (MBL) therapy in an MBL-deficient patient with severe cystic fibrosis lung disease. Pediatr Pulmonol. 2002;33:201–7. doi: 10.1002/ppul.10064. [DOI] [PubMed] [Google Scholar]
- 12.Casanova JL, Abel L. Human mannose-binding lectin in immunity: friend, foe, or both? J Exp Med. 2004;199:1295–9. doi: 10.1084/jem.20040537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garred P, Strom J, Quist L, Taaning E, Madsen HO. Association of mannose-binding lectin polymorphisms with sepsis and fatal outcome, in patients with systemic inflammatory response syndrome. J Infect Dis. 2003;188:1394–403. doi: 10.1086/379044. [DOI] [PubMed] [Google Scholar]
- 14.Lipscombe RJ, Sumiya M, Hill AV, et al. High frequencies in African and non-African populations of independent mutations in the mannose binding protein gene. Hum Mol Genet. 1992;1:709–15. doi: 10.1093/hmg/1.9.709. [DOI] [PubMed] [Google Scholar]
- 15.Locht H, Christiansen M, Laursen I. Reactive arthritis and serum levels of mannose binding lectin − lack of association. Clin Exp Immunol. 2003;131:169–73. doi: 10.1046/j.1365-2249.2003.02023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neth O, Jack DL, Johnson M, Klein NJ, Turner MW. Enhancement of complement activation and opsonophagocytosis by complexes of mannose-binding lectin with mannose-binding lectin-associated serine protease after binding to Staphylococcus aureus. J Immunol. 2002;169:4430–6. doi: 10.4049/jimmunol.169.8.4430. [DOI] [PubMed] [Google Scholar]
- 17.Shi L, Takahashi K, Dundee J, et al. Mannose-binding lectin-deficient mice are susceptible to infection with Staphylococcus aureus 2. J Exp Med. 2004;199:1379–90. doi: 10.1084/jem.20032207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neth O, Jack DL, Dodds AW, Holzel H, Klein NJ, Turner MW. Mannose-binding lectin binds to a range of clinically relevant microorganisms and promotes complement deposition. Infect Immun. 2000;68:688–93. doi: 10.1128/iai.68.2.688-693.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kars M, van Dijk H, Salimans MM, Bartelink AK, van de Wiel A. Association of furunculosis and familial deficiency of mannose-binding lectin. Eur J Clin Invest. 2005;35:531–4. doi: 10.1111/j.1365-2362.2005.01521.x. [DOI] [PubMed] [Google Scholar]
- 20.Hibberd ML, Sumiya M, Summerfield JA, Booy R, Levin M. Association of variants of the gene for mannose-binding lectin with susceptibility to meningococcal disease. Meningococcal Research Group. Lancet. 1999;353:1049–53. doi: 10.1016/s0140-6736(98)08350-0. [DOI] [PubMed] [Google Scholar]
- 21.Moller-Kristensen M, Ip WK, Shi L, et al. Deficiency of mannose-binding lectin greatly increases susceptibility to postburn infection with Pseudomonas aeruginosa. J Immunol. 2006;176:1769–75. doi: 10.4049/jimmunol.176.3.1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graudal NA, Madsen HO, Tarp U, et al. The association of variant mannose-binding lectin genotypes with radiographic outcome in rheumatoid arthritis. Arthritis Rheum. 2000;43:515–21. doi: 10.1002/1529-0131(200003)43:3<515::AID-ANR6>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 23.Heggelund L, Mollnes TE, Espevik T, et al. Modulatory effect of mannose-binding lectin on cytokine responses: possible roles in HIV infection. Eur J Clin Invest. 2005;35:765–70. doi: 10.1111/j.1365-2362.2005.01579.x. [DOI] [PubMed] [Google Scholar]
- 24.Fidler KJ, Wilson P, Davies JC, Turner MW, Peters MJ, Klein NJ. Increased incidence and severity of the systemic inflammatory response syndrome in patients deficient in mannose-binding lectin. Intensive Care Med. 2004;30:1438–45. doi: 10.1007/s00134-004-2303-8. [DOI] [PubMed] [Google Scholar]
- 25.Bergmann OJ, Christiansen M, Laursen I, et al. Low levels of mannose-binding lectin do not affect occurrence of severe infections or duration of fever in acute myeloid leukaemia during remission induction therapy. Eur J Haematol. 2003;70:91–7. doi: 10.1034/j.1600-0609.2003.00012.x. [DOI] [PubMed] [Google Scholar]
- 26.Rugonfalvi-Kiss S, Endresz V, Madsen HO, et al. Association of Chlamydia pneumoniae with coronary artery disease and its progression is dependent on the modifying effect of mannose-binding lectin. Circulation. 2002;106:1071–6. doi: 10.1161/01.cir.0000027137.96791.6a. [DOI] [PubMed] [Google Scholar]
- 27.Danesh J, Whincup P, Walker M. Chlamydia pneumoniae IgA titres and coronary heart diseaseL prospective study and meta-analysis. Eur Heart J. 2003;24:881. doi: 10.1016/s0195-668x(02)00801-1. [DOI] [PubMed] [Google Scholar]
- 28.Erlebacher A, Zhang D, Parlow AF, Glimcher LH. Ovarian insufficiency and early pregnancy loss induced by activation of the innate immune system. J Clin Invest. 2004;114:39–48. doi: 10.1172/JCI20645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dahl M, Tybjaerg-Hansen A, Schnohr P, Nordestgaard BG. A population-based study of morbidity and mortality in mannose-binding lectin deficiency. J Exp Med. 2004;199:1391–9. doi: 10.1084/jem.20040111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ip WK, To YF, Cheng SK, Lau YL. Serum mannose-binding lectin levels and mbl2 gene polymorphisms in different age and gender groups of southern Chinese adults. Scand J Immunol. 2004;59:310–4. doi: 10.1111/j.0300-9475.2004.01392.x. [DOI] [PubMed] [Google Scholar]
- 31.Valdimarsson H, Vikingsdottir T, Bang P, et al. Human plasma-derived mannose-binding lectin: a phase I safety and pharmacokinetic study. Scand J Immunol. 2004;59:97–102. doi: 10.1111/j.0300-9475.2004.01357.x. [DOI] [PubMed] [Google Scholar]