Abstract
Epidemiological data have indicated that some infections are associated with a low risk of allergic diseases, thus supporting the idea (hygiene hypothesis) that the microbial load is an important environmental factor conferring protection against the development of allergies. We set out to test the hygiene hypothesis in a unique epidemiological setting in two socio-economically and culturally markedly different, although genetically related, populations living in geographically adjacent areas. The study cohorts included 266 schoolchildren from the Karelian Republic in Russia and 266 schoolchildren from Finland. The levels of total IgE and allergen-specific IgE for birch, cat and egg albumen were measured. Microbial antibodies were analysed against enteroviruses (coxsackievirus B4), hepatitis A virus, Helicobacter pylori and Toxoplasma gondii. Although total IgE level was higher in Russian Karelian children compared to their Finnish peers, the prevalence of allergen-specific IgE was lower among Russian Karelian children. The prevalence of microbial antibodies was, in turn, significantly more frequent in the Karelian children, reflecting the conspicuous difference in socio-economic background factors. Microbial infections were associated with lower risk of allergic sensitization in Russian Karelian children, enterovirus showing the strongest protective effect in a multivariate model. The present findings support the idea that exposure to certain infections, particularly in childhood, may protect from the development of atopy. Enterovirus infections represent a new candidate to the list of markers of such a protective environment. However, possible causal relationship needs to be confirmed in further studies.
Keywords: allergy, atopy, bacteria, viruses, viral immunity, immunoglobulins
Introduction
In recent decades an increase in the prevalence of allergic diseases such as allergic rhinitis and eczema has been documented in developed countries [1–3]. There is also accumulating evidence that the prevalence of atopy, as measured by skin prick testing and specific IgE, is increasing [4–6]. Several studies have revealed an East–West gradient in the prevalence of symptoms of allergic diseases [7–11], as well as in the prevalence of atopy across European countries [9–11].
A series of environmental factors has been proposed to account for the increasing prevalence of allergic diseases and the variation between geographically adjacent areas. An inverse association between the number of siblings and allergic diseases has been documented in epidemiological surveys [12,13]. Growing up on a farm seems to be associated with a lower prevalence of allergic rhinitis and sensitization [11,14,15]. Children who do not live on a farm but have regular contact with livestock had also a lower prevalence of allergic sensitization [14]. The underlying reasons behind these associations are largely unknown, but the ‘hygiene hypothesis’ provides a possible explanation suggesting that exposure to a variety of microbes in childhood protects against atopic diseases by promoting the maturation of the immune system [13,16].
Several studies have suggested a role for T helper 2 (Th2)-polarized CD4+ T cells in the pathogenesis of asthma and allergy [17–19], but the exact immunological mechanisms regulating allergic sensitization are not known. Th1-biased immune responses may down-regulate the effects of Th2 cells [17] or regulatory T cells may control the Th1/Th2 balance [18,19]. There is also epidemiological evidence that some infections, such as hepatitis A virus (HAV) [20–23]Toxoplasma gondii[22,23] and Helicobacter pylori[4,22,23], and bacterial components [24–26] are associated with reduced risk of atopic diseases, thus supporting the hypothesis that the microbial load is an important environmental factor conferring protection against the development of allergies in childhood [27].
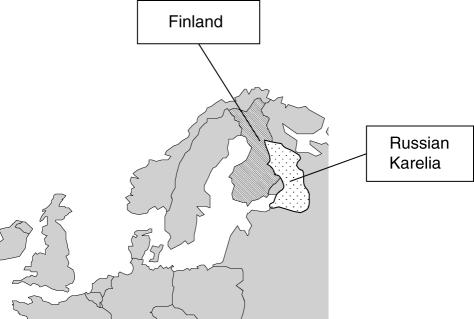
The objective of this study was to investigate variations and associations in the prevalence of microbial infections and allergic sensitization in children in Finland and Russia, in order to test the hygiene hypothesis in a unique epidemiological setting in two socio-economically and culturally markedly different, although geographically adjacent, areas (Fig. 1).
Fig. 1.
Geographic location of the two study areas.
The Karelian Republic is situated in the north-western part of Russia adjacent to the Finnish border. Even though these two areas share the same geographical and climatic environment, they differ markedly in culture, economy and standards of living (e.g. the gross national product per capita is about US$32 790 in Finland compared to US$3410 in Russia). Consequently, many lifestyle-related factors, such as the general level of hygiene and related exposures to infections and commensal microbes, are perceived to differ between these two regions. To test the effect of these presumed differences in hygiene levels and microbial load on the risk of allergic sensitization, we analysed the prevalence of microbes that are considered commonly to reflect the level of hygiene, such as HAV, enterovirus, H. pylori and T. gondii infections as well as allergen-specific and total IgE in the general population (schoolchildren) in these two regions. This unique epidemiological setting makes it possible to study the role of environmental factors in allergic sensitization, particularly because the two study populations had similar ethnical and genetic background, the children from Russian Karelia being of Finnish–Karelian ancestry.
Methods
Subjects
Both the Russian Karelian study cohort and the Finnish study cohort comprised 266 schoolchildren. The children represented the mainstream populations and were not selected according to possible allergic or other diseases. All the children from the Karelian Republic had both parents of either Finnish or Karelian ethnicity, which confers an ethnic background close to that of the children in Finland [28]. Altogether, the study cohorts included 114 boys and 152 girls from each country. The mean age at sampling was 11·4 years (range 7–15 years) in both cohorts.
The Karelian cohort was recruited as a part of the type 1 diabetes-related EPIVIR-project (EU INCO-Copernicus programme, contract number IC15-CT98-0316, Coordinator Professor Hyöty). In this project blood samples were taken from a total of 1988 randomly selected schoolchildren in Karelia in the period 1997–99. The ethnic backgrounds of both the mother and father were recorded, and all children whose both parents were of either Finnish or Karelian ethnicity were included in the present study (n = 266). Samples were taken during the months March, April and May. For the Karelian children, a cohort of Finnish children was matched pairwise by age, gender and date of the sample (no more than 1 month apart), thus minimizing the effect of the season on exposure to microbes and allergens. The Finnish cohort was recruited in the same way as the Karelian cohort and initially included 3654 schoolchildren living in the Oulu region of Finland [29]. Blood samples were taken in 1994. All children had parental consent to participate in the study. The study was approved by the ethical committee of the Faculty of Medicine, University of Oulu, Finland, and by the Ministry of Health in the Karelian Republic of Russia.
IgE and microbial antibodies
The levels of total IgE and allergen-specific IgE were measured using the UniCAP® fluoroenzyme immunoassay (Pharmacia Diagnostics, Uppsala, Sweden). Specific IgE for two common inhalant allergens (birch and cat) and for egg albumin was analysed according to the manufacturer's instructions. These allergens were selected because the exposure to them can be expected to be quite similar in both populations (e.g. mite allergens were not included because the strength of exposure may differ). For allergen-specific IgE, values of 0·35 IU/l or more were considered positive. In previous studies total IgE values exceeding 100 IU/l have been considered as markers of atopic predisposition [9]. Microbial antibodies were analysed against coxsackievirus B4 (representing enteroviruses), HAV, H. pylori and T. gondii. IgG class enterovirus antibodies were measured using enzyme immunoassay (EIA) against a highly purified coxsackievirus B4 antigen (CBV4), as described previously [30]. IgG class HAV antibodies were measured using Enzygnost® anti-HAV commercial EIA kit, IgG class H. pylori antibodies Enzygnost® anti-H. pylori/IgG assay and Toxoplasma IgG by Enzygnost® toxoplasmosis IgG assay, according to the manufacturer's instructions (Dade Behring, Marburg, Germany). A Behring enzyme-linked immunosorbent assay (ELISA) Processor III was used for further processing of the tests and for the calculation of the antibody levels.
Statistical methods
Statistical analyses were performed with the spss program version 12·0 (SPSS Inc., Chicago, IL, USA) and confidence interval analyses (CIA) [31]. Prevalence of specific IgE, high values (> 100 IU/l) of total IgE and microbial antibodies between two paired cohorts was compared using McNemar's test. Comparisons of total IgE levels (skewly distributed continuous variable) between paired cohorts were performed using Wilcoxon's signed-ranks test. Cross-tabulation and χ2 test or Fisher's exact test were applied for the analyses of associations between microbial antibodies, high values of total IgE and specific IgE in Russian Karelia and Finland. The Mann–Whitney U-test was used when associations between total IgE levels and specific IgE (classified as positive or negative) were analysed and also in the analyses of associations between CBV4 IgG levels and specific IgE. As a multivariate technique, logistic regression was applied to identify the independent effect of each parameter when appropriate. The model selection was based on a forward stepwise procedure, where the limit to enter and to remove the term was equal to 0·10. The results are supported by the assessment of odds ratio (OR) and 95% confidence intervals (CI). If there were missing or indifferent values, cases were not included in the analyses involving those particular parameters. The number of such cases was small; for example, for microbial serologies in Russian Karelian children, 0–2 missing cases per each microbe analysed. All analyses were two-sided. Statistically significant P-values (< 0·05) are given.
Results
Total IgE concentrations and the prevalence of allergen-specific IgE antibodies among Finnish and Russian Karelian subjects are shown in Table 1. Total IgE levels and the frequency of high total IgE were significantly higher in Russian Karelian than in Finnish children. In contrast, the prevalence of allergen-specific IgE was significantly lower in Russian Karelian children. In both geographical areas total IgE was significantly higher among children who were positive for at least one allergen than in children with no specific IgE responses, median IU/l-values (range) being 140 (12–3328) and 29 (0–2842) in Finland (P < 0·001) and 460 (31–3522) and 70 (2–2678) in Russian Karelia (P < 0·001), respectively.
Table 1.
Total IgE levels and the prevalence (% and 95% CI) of allergen-specific IgE in schoolchildren in Finland and Russian Karelia
| Finland (n = 266) | Russian Karelia (n = 266) | P-value | |
|---|---|---|---|
| Total IgE | |||
| Median IU/l (range) | 39 (0–3328) | 77 (2–3522) | < 0·001 |
| > 100 IU/l (%) | 26 (21–32) | 40 (34–46) | 0·001 |
| Cat (%) | 11 (8–16) | 2 (1–5) | < 0·001 |
| Birch (%) | 11 (8–16) | 2 (1–5) | < 0·001 |
| Egg albumen (%) | 6 (4–10) | 3 (2–6) | 0·093 |
| At least one positive (%) | 22 (17–27) | 6 (4–10) | < 0·001 |
The prevalence of all microbial antibodies was significantly higher in children in Russian Karelia than in children in Finland (Table 2). In addition, in Russian Karelia allergic sensitization was more rare in children who had a high number of microbial antibodies (Table 3). Only 1·2% (1/85) of the children who were seropositive for more than two microbes of the four tested had at least one positive specific IgE compared to 9·1% (16/176) of those who were seropositive for fewer microbes (OR: 0·12; 95% CI: 0·016–0·91; P = 0·015). When the logistic regression analysis was applied to identify the independent effect of each microbial seropositivity, that of enterovirus (CBV4) had the strongest effect on allergic sensitization. A similar trend was also observed for H. pylori but not for T. gondii and HAV. For example, 22% of the children who were enterovirus seronegative had at least one positive specific IgE result compared to 5% of seropositive children. The median enterovirus antibody level was 74 enzyme immunoassay units (EIU) (range: 0–224) in children who had no specific IgE compared to 49 EIU (range: 0–154) in those who had at least one allergen-specific IgE (P= 0·048).
Table 2.
Prevalence (% and 95% CI) of microbial antibodies in schoolchildren in Finland and Russian Karelia
| Finland (n = 266) | Russian Karelia (n = 266) | P-value | |
|---|---|---|---|
| Coxsackievirus B4 | 77 (72–82) | 93 (90–96) | < 0·001 |
| Helicobacter pylori (%) | 5 (3–8) | 73 (64–78) | < 0·001 |
| Toxoplasma gondii (%) | 5 (3–9) | 24 (19–29) | < 0·001 |
| Hepatitis A virus (%) | 2 (1–5)* | 24 (19–29) | < 0·001 |
Only 166 Finnish children were screened for HAV antibodies.
Table 3.
Proportion of children (% and 95% CI) positive for at least one allergen-specific IgE in relation to seropositivity for microbial antibodies in schoolchildren in Russian Karelia
| Logistical model* | |||||
|---|---|---|---|---|---|
| Microbe-seropositive | Microbe-seronegative | P-value | OR (95% CI) | P-value | |
| Coxsackievirus B4 | 13/247 (5%; 3–9%) | 4/18 (22%; 9–45%) | 0·020 | 0·16 (0·04–0·6) | 0·006 |
| Helicobacter pylori | 9/194 (5%; 3–9%) | 8/72 (11%; 6–20%) | 0·055 | 0·33 (0·1–0·9) | 0·037 |
| Toxoplasma gondii | 1/64 (2%; 0–9%) | 16/201 (8%; 5–13%) | 0·082 | n.s. | |
| Hepatitis A virus | 5/63 (8%; 3–17%) | 12/201 (6%; 3–10%) | 0·579 | n.s. | |
n.s.: Not significant.
Forward stepwise model (P for entry and removal 0·10).
In Finland the number of H. pylori, T. gondii and HAV seropositive children was very low (Table 2), which made it difficult to analyse their association with allergen-specific IgE. However, enterovirus antibodies were frequent in the Finnish children but, in contrast to those in Russian Karelia, they showed no association with allergen-specific IgE responses (18% of the enterovirus seronegative children had at least one positive specific IgE result compared to 23% of the seropositive children).
In Russian Karelia the total IgE levels were higher in children who were seropositive for T. gondii compared to seronegative children: 51% (95% CI: 39–63%) versus 36% (95% CI: 30–43%) of the children had IgE > 100 IU/l, respectively (P= 0·041). Other microbial antibodies showed no association with total IgE. In Finland, none of the microbial antibodies correlated with total IgE, but the number of seropositive children was too small for proper comparisons (except for children positive for enterovirus antibodies).
Discussion
In the present study, the prevalences of microbial antibodies perceived as markers of microbial exposure and poor hygiene were significantly higher in Russian Karelian children than in Finnish children. Among the microbes analysed in this study, HAV, H. pylori and T. gondii have been linked previously to a reduced risk of atopy [21–23]. In line with this, we observed that atopic sensitization was indeed significantly less common in Russian Karelian children than in Finnish children, and the number of positive microbial serologies correlated inversely with the prevalence of allergic sensitization to the tested allergens in the children in Russian Karelia. In addition to the humoral immune response to the three above-mentioned microbes, we also measured antibodies against enteroviruses, which are transmitted mainly through the faecal–oral route and can be used as an indicator of hygiene and overcrowding. Interestingly, the strongest inverse association in this study was observed between the prevalence of enteroviruses (CBV4) and atopy in Karelia. On the other hand, HAV had no protective effect at all, which is in contrast with some previous surveys [21–23]. Accordingly, the results support the hygiene hypothesis suggesting that certain microbial infections are associated with lower risk of atopic sensitization. We found that enteroviruses may represent a new candidate for a marker of such a protective environment.
In previous studies, food-borne and faecal–oral microbes such as HAV, T. gondii and H. pylori rather than airborne viruses have been related to reduced risk of atopy [22,23,27]. On the other hand, seropositivity for intestinal bacterial pathogens (Clostridium difficile, Campylobacter jejuni and Yersinia enterocolitica) was associated with a higher prevalence of atopy among Danish adults [23]. Moreover, an independent inverse association was observed between the number of gastrointestinal infections before the age of 5 years and the risk of atopy in the United Kingdom [32]. Recently, Benn et al. reported that infectious diseases during the first 6 months of life (mainly upper respiratory infections) increase the risk of atopy [33], and Bager and collaborators observed a growing risk of atopy with an increasing number of infections caused by airborne viruses (measles, rubella, mumps and varicella) before the age of 1 year [34]. In the present study HAV infections, which are transmitted through the faecal–oral route, were not associated with protection against atopic sensitization, while other microbes with faecal–oral transmission showed a protective effect (e.g. enteroviruses). This suggests that there may be microbe-specific effects possibly linked to other microbe–host interactions than the transmission route per se, or that there are only certain specific food-borne or faecal–oral infections which are relevant and which still remain uncovered.
The fact that an association between infections and prevalence of atopy was observed only in Russian Karelian children but not in the Finnish children could be explained by the assumption that Finnish children are infected at an older age, as the circulation of enteroviruses and other microbes is conspicuously lower in Finland. According to the hygiene hypothesis, infections occurring during the first months of life may be the most important ones, as at this age they can have a marked effect on the maturation of the gut-associated immune system and the developing Th1/Th2 balance. On the other hand it is also possible that some other factors, which are associated with these infections in the Russian but not in the Finnish population, are responsible for the effect. Thus, the effect of enteroviruses is not necessarily specific, but may be linked to some unknown factors which are not present in the Finnish population. In addition, enterovirus infections may have a different pattern of transmission in Russia compared to Finland, due to differences in the hygiene levels (for example, in Russia the faecal–oral transmission route may predominate, whereas respiratory transmission may be more common in Finland). At this point it remains open whether associations between infections and risk of atopy observed in Russian Karelian children are causal or merely reflect other environmental factors that play a role in the development of atopy.
The two study cohorts comprised children of similar ancestry, which minimizes the possible confounding effect of genetic factors on the risk of atopy and makes it possible to analyse the role of environmental factors in atopic sensitization. In a previous study we have shown that the distributions of human leucocyte antigen (HLA-DQ) genotypes does not differ between the two populations [28] supporting their genetic relationship. However, we cannot exclude small differences in the frequency of non-HLA genes, which may have an influence on microbe–host interactions, even though it is unlikely that such small variations in allele frequencies could explain the observed marked difference in allergic sensitization between the two populations.
The fact that samples from Russian Karelia and Finland were taken during different years might affect the results. However, the samples from the Finnish children were collected before the samples from the Russian Karelia children. Assuming that the prevalence of allergy is increasing [4] and that the prevalence of microbial infections is decreasing in Finland [4,35], it might be expected that the temporal interval of about 4 years between the sample collections would diminish rather than increase the observed differences between the two regions. Hypothetically, it is also possible that atopic children have a defective immune response against microorganisms, which could lead to false seronegativity in microbe antibodies. This kind of defective immune response has been described in vaccine studies [36].
Our results are in line with earlier observations suggesting lower prevalence of allergy, as measured by skin prick test or IgE concentrations to common aeroallergens, in Russian Karelian than in Finnish subjects [9,11,37]. Thus, we were able to replicate this observation, and found that it correlates with the difference in microbial exposures. In contrast to allergen-specific IgE, the levels of total IgE showed an opposite difference between the regions compared, being significantly higher in Russian Karelia. The reason for the high levels of total IgE in a region characterized by a low prevalence of allergic sensitization is not clear. In the present study we observed that high total IgE levels were associated with T. gondii infections, suggesting that the difference in total IgE concentrations can be explained partly by the higher prevalence of parasite infections in Russian Karelia compared to Finland.
In conclusion, the present study shows that allergic sensitization is conspicuously more common in Finland than in Russian Karelia. These two populations are living in geographically adjacent areas and are related genetically, but they differ markedly for several other factors linked to the sharp gradient in prosperity across the border. This suggests that environmental factors related to these differences in standard of living between the two populations are important in allergic sensitization, and according to the present observations microbial infections may play an important role in this process. Thus, the results support the hygiene hypothesis and enterovirus infections represent a new candidate to be added to the list of markers of such a protective environment. This epidemiological setting provides unique new possibilities to study further the role of microbe–host interactions in atopic sensitization. Such studies are currently under way.
The EPIVIR study group
The EPIVIR study group includes the following researchers: H. Hyöty (coordinator), M. Knip and H. Viskari, University of Tampere, Finland; J. Ilonen, University of Turku, Finland, A. Reunanen, National Public Health Institute, Helsinki, Finland; R. Uibo (scientific coordinator), University of Tartu, Estonia; J. Ludvigsson, University of Linköping, Sweden, D. Marciulionyte, University of Kaunas, Lithuania; R. Hermann, G. Soltesz, University of Pécs, Hungary; M. Fuechtenbusch and A. Ziegler, Munich, Germany; A. Kondrashova and A. Romanov, University of Petrozavodsk, Russia.
Acknowledgments
This study received support from the European Union as a part of the EPIVIR project (INCO-Copernicus Program, contract number IC15-CT98-0316) and has been supported by grants from the Päivikki and Sakari Sohlberg Foundation, the Academy of Finland, the Tuberculosis Foundation in Tampere, the University of Tampere and the Medical Research Fund of Tampere University Hospital. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. The corresponding author had full access to all the data for the study and made the final decision to submit for publication.
References
- 1.Butland BK, Strachan DP, Lewis S, Bynner J, Butler N, Britton J. Investigation into the increase in hay fever and eczema at age 16 observed between the 1958 and 1970 British birth cohorts. BMJ. 1997;315:717–21. doi: 10.1136/bmj.315.7110.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ninan TK, Russell G. Respiratory symptoms and atopy in Aberdeen schoolchildren: evidence from two surveys 25 years apart. BMJ. 1992;304:873–5. doi: 10.1136/bmj.304.6831.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linneberg A, Nielsen NH, Madsen F, Frolund L, Dirksen A, Jorgensen T. Increasing prevalence of allergic rhinitis symptoms in an adult Danish population. Allergy. 1999;54:1194–8. doi: 10.1034/j.1398-9995.1999.00180.x. [DOI] [PubMed] [Google Scholar]
- 4.Kosunen TU, Hook-Nikanne J, Salomaa A, Sarna S, Aromaa A, Haahtela T. Increase of allergen-specific immunoglobulin E antibodies from 1973 to 1994 in a Finnish population and a possible relationship to Helicobacter pylori infections. Clin Exp Allergy. 2002;32:373–8. doi: 10.1046/j.1365-2222.2002.01330.x. [DOI] [PubMed] [Google Scholar]
- 5.Linneberg A, Jorgensen T, Nielsen NH, Madsen F, Frolund L, Dirksen A. The prevalence of skin-test-positive allergic rhinitis in Danish adults: two cross-sectional surveys 8 years apart. The Copenhagen Allergy Study. Allergy. 2000;55:767–72. doi: 10.1034/j.1398-9995.2000.00672.x. [DOI] [PubMed] [Google Scholar]
- 6.Linneberg A, Nielsen NH, Madsen F, Frolund L, Dirksen A, Jorgensen T. Increasing prevalence of specific IgE to aeroallergens in an adult population: two cross-sectional surveys 8 years apart: the Copenhagen Allergy Study. J Allergy Clin Immunol. 2000;106:247–52. doi: 10.1067/mai.2000.108312. [DOI] [PubMed] [Google Scholar]
- 7.Williams H, Robertson C, Stewart A, et al. Worldwide variations in the prevalence of symptoms of atopic eczema in the international study of asthma and allergies in childhood. J Allergy Clin Immunol. 1999;103:125–38. doi: 10.1016/s0091-6749(99)70536-1. [DOI] [PubMed] [Google Scholar]
- 8.Bjorksten B, Dumitrascu D, Foucard T, et al. Prevalence of childhood asthma, rhinitis and eczema in Scandinavia and Eastern Europe. Eur Respir J. 1998;12:432–7. doi: 10.1183/09031936.98.12020432. [DOI] [PubMed] [Google Scholar]
- 9.Vartiainen E, Petays T, Haahtela T, Jousilahti P, Pekkanen J. Allergic diseases, skin prick test responses, and IgE levels in North Karelia, Finland, and the Republic of Karelia, Russia. J Allergy Clin Immunol. 2002;109:643–8. doi: 10.1067/mai.2002.123307. [DOI] [PubMed] [Google Scholar]
- 10.Nicolai T, Bellach B, Mutius EV, Thefeld W, Hoffmeister H. Increased prevalence of sensitization against aeroallergens in adults in West compared with East Germany. Clin Exp Allergy. 1997;27:886–92. [PubMed] [Google Scholar]
- 11.von Hertzen L, Mäkelä M, Petäys T, et al. Growing disparities in atopy between the Finns and the Russians: a comparison of 2 generations. J Allergy Clin Immunol. 2006;117:151–7. doi: 10.1016/j.jaci.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 12.Karmaus W, Botezan C. Does a higher number of siblings protect against the development of allergy and asthma? A review. J Epidemiol Commun Health. 2002;56:209–17. doi: 10.1136/jech.56.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strachan DP. Family size, infection and atopy: the first decade of the ‘hygiene hypothesis’. Thorax. 2000;55(Suppl. 1):S2–10. doi: 10.1136/thorax.55.suppl_1.s2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riedler J, Eder W, Oberfeld G, Schreuer M. Austrian children living on a farm have less hay fever, asthma and allergic sensitization. Clin Exp Allergy. 2000;30:194–200. doi: 10.1046/j.1365-2222.2000.00799.x. [DOI] [PubMed] [Google Scholar]
- 15.Kilpelainen M, Terho EO, Helenius H, Koskenvuo M. Farm environment in childhood prevents the development of allergies. Clin Exp Allergy. 2000;30:201–8. doi: 10.1046/j.1365-2222.2000.00800.x. [DOI] [PubMed] [Google Scholar]
- 16.Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299:1259–60. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mosmann TR, Sad S. The expanding universe of T-cell subsets: Th1, Th2 and more. Immunol Today. 1996;17:138–46. doi: 10.1016/0167-5699(96)80606-2. [DOI] [PubMed] [Google Scholar]
- 18.Umetsu DT, Akbari O, Dekruyff RH. Regulatory T cells control the development of allergic disease and asthma. J Allergy Clin Immunol. 2003;112:480–7. [PubMed] [Google Scholar]
- 19.Curotto de Lafaille MA, Lafaille JJ. CD4(+) regulatory T cells in autoimmunity and allergy. Curr Opin Immunol. 2002;14:771–8. doi: 10.1016/s0952-7915(02)00408-9. [DOI] [PubMed] [Google Scholar]
- 20.McIntire JJ, Umetsu SE, Macaubas C, et al. Immunology: hepatitis A virus link to atopic disease. Nature. 2003;425:576. doi: 10.1038/425576a. [DOI] [PubMed] [Google Scholar]
- 21.Matricardi PM, Rosmini F, Ferrigno L, et al. Cross sectional retrospective study of prevalence of atopy among Italian military students with antibodies against hepatitis A virus. BMJ. 1997;314:999–1003. doi: 10.1136/bmj.314.7086.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matricardi PM, Rosmini F, Riondino S, et al. Exposure to foodborne and orofecal microbes versus airborne viruses in relation to atopy and allergic asthma: epidemiological study. BMJ. 2000;320:412–7. doi: 10.1136/bmj.320.7232.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linneberg A, Ostergaard C, Tvede M, et al. IgG antibodies against microorganisms and atopic disease in Danish adults: the Copenhagen allergy study. J Allergy Clin Immunol. 2003;111:847–53. doi: 10.1067/mai.2003.1335. [DOI] [PubMed] [Google Scholar]
- 24.Gereda JE, Leung DY, Liu AH. Levels of environmental endotoxin and prevalence of atopic disease. JAMA. 2000;284:1652–3. doi: 10.1001/jama.284.13.1652. [DOI] [PubMed] [Google Scholar]
- 25.Gereda JE, Leung DY, Thatayatikom A, et al. Relation between house-dust endotoxin exposure, type 1 T-cell development, and allergen sensitisation in infants at high risk of asthma. Lancet. 2000;355:1680–3. doi: 10.1016/s0140-6736(00)02239-x. [DOI] [PubMed] [Google Scholar]
- 26.von Mutius E, Braun-Fahrlander C, Schierl R, et al. Exposure to endotoxin or other bacterial components might protect against the development of atopy. Clin Exp Allergy. 2000;30:1230–4. doi: 10.1046/j.1365-2222.2000.00959.x. [DOI] [PubMed] [Google Scholar]
- 27.Matricardi PM, Ronchetti R. Are infections protecting from atopy? Curr Opin Allergy Clin Immunol. 2001;1:413–9. doi: 10.1097/01.all.0000011054.18314.67. [DOI] [PubMed] [Google Scholar]
- 28.Kondrashova A, Romanov A, Reunanen A, et al. A six-fold gradient in the incidence of type 1 diabetes at the eastern border of Finland − evidence of a critical role of environment in the disease pathogenesis. Ann Med. 2005;37:67–72. doi: 10.1080/07853890410018952. [DOI] [PubMed] [Google Scholar]
- 29.Mäki M, Mustalahti K, Kokkonen J, et al. Prevalence of celiac disease among children in Finland. N Engl J Med. 2003;348:2517–24. doi: 10.1056/NEJMoa021687. [DOI] [PubMed] [Google Scholar]
- 30.Salminen K, Sadeharju K, Lönnrot M, et al. Enterovirus infections are associated with the induction of beta-cell autoimmunity in a prospective birth cohort study. J Med Virol. 2003;69:91–8. doi: 10.1002/jmv.10260. [DOI] [PubMed] [Google Scholar]
- 31.Altman D, Altman DG, Bryant T, Gardner M, Gardner MJ, Machin D. Statistics with confidence. London: BMJ Books; 2000. [Google Scholar]
- 32.Cullinan P, Harris JM, Newman Taylor AJ, et al. Can early infection explain the sibling effect in adult atopy? Eur Respir J. 2003;22:956–61. doi: 10.1183/09031936.03.00039102. [DOI] [PubMed] [Google Scholar]
- 33.Benn CS, Melbye M, Wohlfahrt J, Bjorksten B, Aaby P. Cohort study of sibling effect, infectious diseases, and risk of atopic dermatitis during first 18 months of life. BMJ. 2004;328:1223. doi: 10.1136/bmj.38069.512245.FE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bager P, Westergaard T, Rostgaard K, Hjalgrim H, Melbye M. Age at childhood infections and risk of atopy. Thorax. 2002;57:379–82. doi: 10.1136/thorax.57.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Viskari H, Ludvigsson J, Uibo R, et al. Relationship between the incidence of type 1 diabetes and maternal enterovirus antibodies: time trends and geographical variation. Diabetologia. 2005;48:1280–7. doi: 10.1007/s00125-005-1780-9. [DOI] [PubMed] [Google Scholar]
- 36.Arkwright PD, Patel L, Moran A, Haeney MR, Ewing CI, David TJ. Atopic eczema is associated with delayed maturation of the antibody response to pneumococcal vaccine. Clin Exp Immunol. 2000;122:16–9. doi: 10.1046/j.1365-2249.2000.01338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Klemola T, St Masyuk V, von Hertzen L, Haahtela T. Occurrence of atopy among russian and finnish schoolchildren. Allergy. 2004;59:465–6. doi: 10.1046/j.1398-9995.2003.00371.x. [DOI] [PubMed] [Google Scholar]