Abstract
In the present study, we examined the effect of the loss of the human leucocyte antigen (HLA)-B*3501-restricted nucleoprotein (NP)418−426 epitope on interferon (IFN)-γ-production and lytic activity of the human cytotoxic T lymphocyte (CTL) response in vitro. Extensive amino acid variation at T cell receptor contact residues of the NP418−426 epitope has led to repeated evasion from specific CTL. We generated recombinant influenza viruses with variants of the NP418−426 epitope, which were used to stimulate peripheral blood mononuclear cells obtained from six HLA-B*3501-positive study subjects in order to expand virus-specific CTL. Loss of the NP418−426 epitope resulted in a significant reduction of IFN-γ-expressing CD8+ T cells, similar to that observed previously after the loss of the HLA-B*2705-restricted NP383−391 epitope. In addition, the effect of the loss of the NP418−426 epitope on the lytic activity of the virus-specific CTL response was assessed. Also this functional property of the virus-specific CTL response was affected significantly by the loss of this and the NP383−391 epitope, as determined using the newly developed fluorescent antigen-transfected target cell (FATT)–CTL assay. These findings indicate that the loss of single immunodominant epitopes affects the functionality of the virus-specific CTL response significantly.
Keywords: cytotoxic T lymphocytes, epitopes, escape, human, influenza virus
Introduction
Cytotoxic T lymphocytes (CTL) play an important role in the control of viral infections, including those caused by influenza viruses. In mice, mortality caused by influenza virus infection was reduced and more efficient viral clearance was shown upon adoptive transfer of virus-specific CTL [1–5]. In addition, mice lacking major histocompatibility complex (MHC) class I-restricted CD8+ T cells show delayed viral clearance and increased mortality [6–8]. In humans, the level of influenza virus-specific CTL activity correlated with the rate of viral clearance upon infection [9,10]. However, like certain other viruses [11–13], influenza A viruses can evade CTL responses by amino acid substitutions in CTL epitopes [14–18]. The R384G substitution in the influenza virus nucleoprotein (NP) is at the anchor residue of the human leucocyte antigen (HLA)-B*0801-restricted NP380−388 epitope and the HLA-B*2705-restricted NP383−391 epitope, and prevented binding of the epitopes to their corresponding MHC class I molecules and recognition by specific CTL [16,18,19]. Also, amino acid variation at T cell receptor (TCR) contact residues, like the amino acid substitutions at positions 421, 422, 423 and 425 of the hypervariable HLA-B*3501-restricted NP418−426 epitope, can result in evasion from specific CTL. Variants of the NP418−426 epitope emerged over time, and NP418−426-specific CTL directed against earlier virus strains failed to recognize more recent variants of influenza A virus, indicating escape from CTL immunity [17]. The high degree of amino acid variability in the latter epitope is driven probably by CTL that recognize their epitope with high functional avidity [20]. Amino acid substitutions at anchor residues were not observed in the NP418−426 epitope, which may be explained by functional constraints, as we have shown recently that the replacement of the anchor residue at position 419 of the NP impaired viral fitness [21]. For some NP418−426 epitope variants, a small proportion of the CTL directed against one epitope variant cross-reacted with another epitope variant [22,23]. In a subsequent infection with an influenza virus with the corresponding variant epitope these cross-reactive CTL may be expanded further, indicating that immune evasion may be only temporary.
In the present study, we examined the impact of the loss of the NP418−426 epitope on the human influenza virus-specific CTL response in vitro. We have shown previously that the loss of the HLA-B*2705-restricted NP383−391 epitope affected the human influenza virus-specific CTL response in vitro significantly, as measured by the number of IFN-γ-producing CD8+ T lymphocytes [19]. However, for the elimination of virus-infected cells and viral clearance, the lytic activity of virus-specific CTL may be more important [24–27]. Therefore, we investigated the effect of the loss of the HLA-B*2705-restricted NP383−391 and the HLA-B*3501-restricted NP418−426 epitope on the lytic activity of the influenza virus NP-specific response, in addition to the effect on IFN-γ production. To this end, influenza viruses with various NP418−426 epitope sequences were generated by reverse genetics. Using in vitro-stimulated peripheral blood mononuclear cell (PBMC) cultures, we assessed the virus-specific CD8+ T cell response directed against influenza virus with variants of the NP418−426 epitope by tetramer and intracellular IFN-γ staining and flow cytometry. For measurement of the lytic activity of clonal and in vitro-expanded polyclonal T cell populations, we used the newly developed fluorescent antigen-transfected target cell (FATT)–CTL assay, which is based on the use of target cells transfected with plasmids expressing viral proteins fused to green fluorescent protein (GFP) [28]. This procedure allowed the detection of a significant reduction of the NP-specific lytic activity of the human influenza virus-specific CTL response caused by the loss of the HLA-B*2705-restricted NP383−391 and the HLA-B*3501-restricted NP418−426 epitopes.
Materials and methods
Plasmids
For the generation of recombinant influenza viruses, a bidirectional reverse genetics system based on influenza virus A/Netherlands/178/95 (A/NL/178/95; H3N2) was used [21]. Site-directed mutagenesis (QuikChange site-directed mutagenesis kit; Stratagene, La Jolla, CA, USA) of the NP segment was performed to alter the NP383−391 or NP418−426 sequence, as listed in Table 1. For the construction of FATT–CTL assay vectors, the variant NP genes were cloned into the multiple cloning site of Living Colors vector enhanced green fluorescence protein gene (pEGFP)-N1 (Becton Dickinson, Alphen a/d Rijn, the Netherlands) in frame with the open-reading frame of GFP, using restriction enzymes NheI and AgeI. Read-through of the GFP gene was achieved by deleting the stop codon of the NP gene. Sequence analysis was performed for all recombinant plasmids, using a Big Dye Terminator version 3·1 cycle sequencing kit (Applied Biosystems, Foster City, CA, USA) and an ABI PRISM 3100 Genetic Analyser (Applied Biosystems), according to the manufacturer's instructions. All polymerase chain reaction (PCR) primer sequences and plasmid maps are available on request.
Table 1.
Substitutions introduced in influenza A virus cytotoxic T lymphocyte (CTL) epitopes.
| Epitope | Amino acid substitutions | Designated name | Year of isolation | TCID50/mla | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NP383−391 | S | R | Y | W | A | I | R | T | R | 384R | < 1993 | 6·875 |
| G | 384G | 1993–2006 | 7·000 | |||||||||
| NP418−426 | L | P | F | E | K | S | T | V | M | ESV | 1980–2004 | 7·175 |
| D | P | I | DPI | 1957–72 | 7·000 | |||||||
| D | R | T | I | DRI | 1934 | 7·125 | ||||||
Upon rescue of recombinant viruses containing the respective epitope sequence, the infectious virus titres were determined and expressed as TCID50/ml (Log). NP: nucleoprotein.
Generation of viruses
Recombinant viruses were generated and titrated as described previously [19,21,29,30], and were designated corresponding to the substitutions indicated in Table 1. To confirm the introduction of the mutations and to exclude the introduction of second site mutations, the nucleotide sequences of the corresponding full-length genes were assessed.
Isolation and stimulation of virus-specific CD8+ T lymphocytes
HLA-typed PBMC from healthy blood donors, between 35 and 50 years of age, were isolated from heparinized blood (Sanquin Bloodbank, Rotterdam, the Netherlands) by density gradient centrifugation using Lymphoprep (Axis-Shield PoC, Oslo, Norway) and were cryopreserved at − 135°C. All study subjects had serum antibodies against one or more influenza A virus strains (H1N1 or H3N2) [22,31], indicating one or more exposures to influenza A virus. Permission to use the PBMC for scientific research was obtained from the blood donors by informed consent.
In vitro stimulation of PBMC with influenza A viruses was performed as described previously [31]. CD8+ cells were isolated from the in vitro-expanded PBMC cultures by magnetic sorting, using a CD8 MicroBeads kit (Miltenyi Biotech GmbH, Bergisch Gladbach, Germany), according to the manufacturer's instructions. The isolated CD8+ cells were used as effector cells in the FATT–CTL assays.
Generation of CD8+ T cell clones directed against the HLA-A*0101-restricted epitope NP44−52, the HLA-A*0201-restricted epitope M158−66, the HLA-B*2705-restricted epitope NP383−391 and the different variants of theHLA-B*3501-restricted epitope NP418−426 has been described previously [18,22].
Target cells
B-lymphoblastoid cell lines (BLCL) [32] and an HLA-B*3501-transfected C1R cell line, kindly provided by M. Takiguchi, were used as target cells. For infection with recombinant influenza viruses, 106 target cells were infected at a multiplicity of infection (MOI) of 3 in a volume of 1 ml. After incubation for 1 h at 37°C the cells were resuspended in RPMI-1640 medium (Cambrex, East Rutherford, NJ, USA) supplemented with 10% fetal calf serum (FCS), 2 mM l-glutamine, 100 IU/ml penicillin and 100 µg/ml streptomycin (R10F) and incubated for 16–18 h. For exogenous protein labelling, 50 µg recombinant influenza virus nucleoprotein (rNP), derived from influenza virus A/PR/8/34 (rNP-PR), A/HK/2/68 (rNP-HK) or A/NL/18/94 (rNP-NL), was added to 106 cells in 1 ml R10F [33]. Peptide labelling was performed by incubating 106 cells/ml overnight with 5 µM peptide in R10F. Peptides were manufactured, high-performance liquid chromatography (HPLC)-purified (immunograde, 85% purity) and analysed with mass spectrometry (Eurogentec, Seraing, Belgium). For transfection, 8 µg plasmid DNA (1 µg/µl) was added to 2 × 106 BLCL, resuspended in 100 µl solution V (Amaxa Biosystems, Cologne, Germany) at room temperature. Subsequently, the cells were electroporated in 2 mm electroporation cuvettes (Amaxa Biosystems), using program T16 in the Nucleofector™ (Amaxa Biosystems). Immediately after electroporation, 500 µl R10F (37°C) was added. Cells were transferred to a 24-well plate for overnight incubation.
Cell staining and flow cytometry
Tetramer staining was performed on the in vitro influenza virus-expanded PBMC cultures, as described previously [22]. The allophycocyanin (APC)-conjugated tetramers consisted of HLA-B*3501 molecules complexed with the NP418−426 epitope variants ESV and DPI. In addition, phycoerythrin (PE)-conjugated tetramers were used, consisting of HLA-A*0101- and -A*0201 molecules complexed with the NP44−52 or M158−66 epitope, respectively. At least 104 CD8+ events were acquired using a fluorescence activated cell sorter (FACS)Calibur (Becton Dickinson) flow cytometer.
Intracellular IFN-γ-staining was performed as described previously [19]. Approximately 5 × 103 CD3+ CD8+ events were acquired by flow cytometry. The data were analysed using the software program CellQuest Pro (Becton Dickinson).
Assays to determine the lytic activity of the CTL response
Classical chromium-release assays were performed as described previously [31]. For the newly developed FATT–CTL assay [28], 1000 viable GFP-positive target cells were incubated with CTL clone at effector : target (E : T) ratios of 10, 3, 1, 0·3 and 0·1 for 4 h at 37°C, or with CD8+ cells isolated from in vitro expanded PBMC cultures at E : T ratios of 10, 3, 1 and 0·3 for 4 h at 37°C, or with ex vivo (non-stimulated) PBMC at E : T ratios of 100, 30, 10 and 3 for 18 h at 37°C in 200 µl R10F supplemented with rIL-2 (50 U/ml). The flow rate (µl/s) was determined by calibrated number of beads (TruCOUNT tubes; Becton Dickinson). Ethylenediamine tetraacetic acid (EDTA) (final concentration 2·5 mmol/l) and the fluorescent dye TOPRO-3 iodide (final concentration 25 nmol/l; Molecular Probes, Invitrogen, Paisley, UK) were added to prevent clustering of cells and to identify viable (TOPRO-3-negative) cells, respectively, and the samples were incubated for an additional 20 min at 37°C. Each sample was acquired for a fixed period of 60 s. The forward-scatter acquisition threshold was set to exclude debris. The FL-1 (GFP) acquisition threshold was set to reduce GFP-negative events. A constant flow rate was monitored in a time–event histogram. The data were analysed with CellQuest Pro. The percentage-specific lysis was calculated with the formula: [(viable GFP+ events without effector-viable GFP+ events with effector)/(viable GFP+ events without effector)] × 100%. The FATT–CTL assays were performed in duplicate and the data were presented as the average.
Results
Replication and recognition of influenza NP418−426-variant viruses
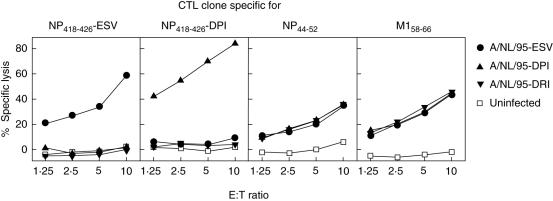
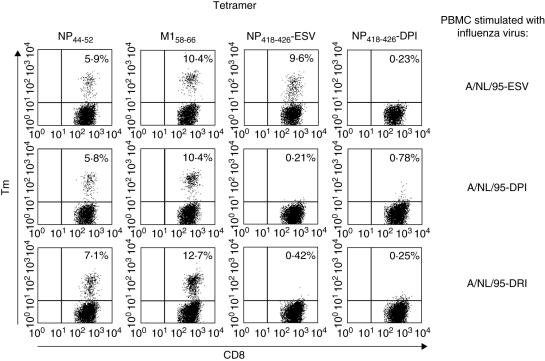
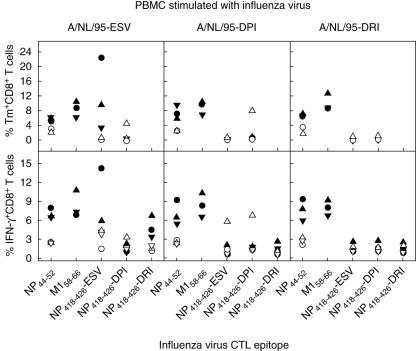
By reverse genetics, identical influenza viruses A/NL/178/95 were generated which differed regarding only their NP418−426 epitope sequence. Because the next evading amino acid substitution within the NP418−426 epitope cannot be predicted, we used the historical epitope sequence of influenza virus A/PR/8/34 (LPFDRTTIM, referred to further as DRI), isolated in 1934, and the sequence of an epitope variant that circulated from 1957 to 1972 (LPFDKPTIM, referred to further as DPI) for the generation of viruses ‘without’ the NP418−426 epitope. Both epitope sequences are not recognized by CTL specific for the current epitope variant (LPFEKSTVM, referred to further as ESV) [17,22]. In addition, we hypothesized that these natural sequences would not be detrimental to viral fitness and would yield viable viruses. The recombinant viruses could indeed be rescued and replicated to similar titres in MDCK cells. The growth kinetics of all three viruses was similar (data not shown). The infection rate of BLCL was also comparable, as determined by positive staining for NP (data not shown). BLCL that were infected with the three NP418−426-variant viruses were all recognized equally well by CD8+ T cell clones specific for the conserved HLA-A*0101-restricted NP44−52 and HLA-A*0201-restricted M158−66 epitopes (Fig. 1), indicating that the substitutions did not affect infection, antigen processing or presentation of the mutant viruses. In contrast, T cell clones directed against the NP418−426 epitope variants DPI and ESV lysed only cells that were infected with the influenza virus that contained the homologous epitope. Influenza virus A/NL/95-DRI infected cells were not recognized by either of these NP418−426 epitope-specific CTL clones. Next, the three variant viruses were used to stimulate PBMC obtained from HLA-B*3501-positive study subjects (Table 2) in order to expand virus-specific CD8+ T lymphocytes. The proportion of ESV- and DPI-specific CTL within the CD8+ population was determined by tetramer staining. A representative result obtained with the PBMC of an HLA-B*3501-positive study subject is shown in Fig. 2. On average 7·2% (ranging from 0·1 to 22·4%) of all CD8+ T cells were ESV-specific in PBMC cultures stimulated with influenza virus A/NL/95-ESV. In contrast, ESV-specific CD8+ T cells were virtually absent in PBMC cultures stimulated with influenza virus A/NL/95-DPI and -DRI. In the A/NL/95-ESV-stimulated PBMC cultures of two HLA-B*3501-positive study subjects (5507 and 5526), ESV-specific CD8+ T cells were undetectable; however, in the PBMC expanded after stimulation with influenza virus A/NL/95-DPI of one of these two study subjects (5526), 7·9% DPI-specific CD8+ T cells were detected. Tetramer staining for NP44−52- and M158−66-specific CD8+ T lymphocytes indicated that the infection of PBMC and subsequent stimulation was successful after stimulation with the three viruses, as the percentage of NP44−52 and M158−66-specific CTL was comparable in the three PBMC cultures of the individual study subjects. The results obtained for each individual study subject are shown in Fig. 3 (upper panel).
Fig. 1.
Recognition of B-lymphoblastoid cell lines (BLCL) infected with recombinant influenza viruses by cytotoxic T lymphocyte (CTL) clones. HLA-A*0101, -A*0201 and -B*3501-positive BLCL were infected with influenza virus A/NL/95-ESV (•), -DPI (▴) or -DRI (▾), or left untreated (□), and used as target cells for CD8+ T cell clones specific for the human leucocyte antigen (HLA)-A*0101-restricted nucleoprotein (NP)44−52 epitope, the HLA-A*0201-restricted M158−66 epitope or the HLA-B*3501-restricted NP418−426 epitopes ESV or DPI in a classical chromium-release assay. CTL clones were added at different effector : target ratios as indicated, and specific lysis was calculated. The chromium-release assay was performed in quadruplicate and the data are presented as the average.
Table 2.
Human leucocyte antigen (HLA)-A and -B genotypes of the six individuals included in this study, and proportions of virus- and nucleoprotein (NP)418−426 epitope-specific CD8+ T cells in peripheral blood mononuclear cells (PBMC) stimulated with influenza virus A/NL/95-ESV.a
| % of CD8+ T cells specific for | Relative proportion (%) specific for | |||||||
|---|---|---|---|---|---|---|---|---|
| Symbols | Donor | HLA-A and -B haplotypes | A/NL/95-ESV | NP418−426 ESV | NP418−426 ESV | |||
| • | 3180 | A*0101 | A*0201 | B*0801 | B*3501 | 40·02 | 14·20 | 35·5 |
| ▴ | 6358 | A*0101 | A*0201 | B*0801 | B*3501 | 38·41 | 5·89 | 15·3 |
| ▾ | 0775 | A*0101 | A*0201 | B*0801 | B*3501 | 27·70 | 4·12 | 14·9 |
| ○ | 5507 | A*0101 | A*0301 | B*0801 | B*3501 | 14·75 | 1·50 | 10·2 |
| ▵ | 5526 | A*0101 | A*0301 | B*0801 | B*3501 | 19·05 | 4·37 | 22·9 |
| ▿ | 6877 | A*0101 | A*0301 | B*0801 | B*3501 | 18·72 | 3·73 | 19·9 |
Determined by interferon (IFN)-γ expression in in vitro influenza virus A/NL/95-ESV-stimulated PBMC after restimulation with A/NL/95-ESV-infected or nucleoprotein (NP)418−426 peptide-pulsed major histocompatibility complex (MHC) class I-matched BLCL.
Fig. 2.
Tetramer staining of peripheral blood mononuclear cell (PBMC) expansion cultures stimulated with various influenza virus variants. PBMC stimulated with influenza virus A/NL/95-ESV, -DPI or -DRI were stained with phycoerythrin (PE)-conjugated tetramers consisting of human leucocyte antigen (HLA)-A*0101- and -A*0201-molecules complexed with the nucleoprotein (NP)44−52 or M158−66 epitope, respectively, and allophycocyanin (APC)-conjugated tetramers consisting of HLA-B*3501 molecules complexed with the NP418−426 epitope variants ESV and DPI as indicated. The data of a representative experiment are shown (study subject 6358). The percentages indicate the proportion of tetramer-specific cytotoxic T lymphocytes (CTL) within the CD8+ T cell population.
Fig. 3.
Recognition of nucleoprotein (NP)418−426 epitope variants by human leucocyte antigen (HLA)-B*3501-positive peripheral blood mononuclear cell (PBMC) cultures. PBMC obtained from HLA-B*3501-positive study subjects were stimulated with influenza virus A/NL/95-ESV, -DPI and -DRI as indicated. The symbols correspond to individual study subjects listed in Table 2. The cells were stained with tetramer (upper panels) as indicated. In addition, epitope-specific CD8+ T cells were detected by staining for interferon (IFN)-γ expression after restimulation with major histocompatibility complex (MHC) class I-matched B-lymphoblastoid cell lines (BLCL) incubated with the peptides M158−66 (GILGFVFTL), nucleoprotein (NP)44−52 (CTELKLSDY) or NP418−426 (ESV, DPI, DRI) (lower panels). The M158−66-specific responses were indicated only for the subjects that were also HLA-A*0201-positive.
Effect of mutations in the NP418−426 epitope on the virus-specific CTL response in vitro
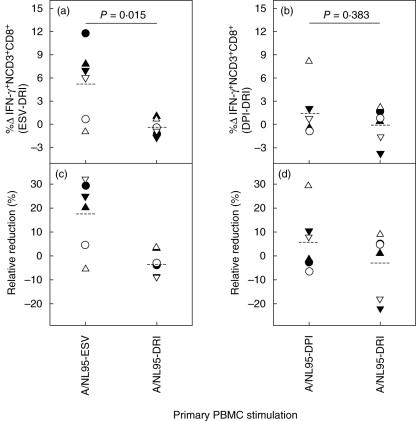
To assess the effect of the loss of the NP418−426 (ESV) epitope on the influenza virus-specific CTL response in vitro, PBMC obtained from the six HLA-B*3501-positive study subjects were stimulated with influenza viruses A/NL/95-ESV, -DPI or -DRI. After expansion, the number of virus-specific CD8+ T cells was determined upon induction of IFN-γ expression by restimulation with MHC class I-matched BLCL or HLA-B*3501-transfected C1R cells that were infected with the three viruses. The percentage of IFN-γ+ CD8+ T cells after restimulation of the expanded PBMC cultures with peptide-labelled stimulator cells correlated with the results of the tetramer staining (Table 2 and Fig. 3, lower panels). In four of the six study subjects similar T cell recognition patterns were observed, as shown in Fig. 4. The highest frequency of virus-specific CTL was observed in PBMC stimulated with influenza virus A/NL/95-ESV and restimulated with the same virus. Restimulation with influenza virus A/NL/95-DPI or -DRI resulted in IFN-γ expression in a smaller number of CD8+ T cells. After primary stimulation of PBMC with influenza virus A/NL/95-DPI or -DRI the number of virus-specific CTL was also reduced, regardless of the influenza virus that was used for restimulation. For two study subjects (5507 and 5526) this was not the case, which correlated with the absence of NP418−426 (ESV)-specific CD8+ T cells (Fig. 3, upper left panel). The difference in the percentage of IFN-γ+ CD8+ T cells after restimulation with virus with or without the epitope (i.e. DRI) is plotted in Fig. 5, and ranged from no difference to 12% in the two subjects without a NP418−426 ESV-specific response. The average difference of 5·4% was statistically significant [analysis of variance (anova); P < 0·05]. In the influenza virus A/NL/95-DPI-stimulated PBMC of the six HLA-B*3501-positive study subjects, no differences in the number of virus-specific cells were observed with influenza virus A/NL/95-DRI-stimulated PBMC, apart from the PBMC obtained from study subject 5526 (Fig. 5b,d), who had an appreciable response specific for the NP418−426 DPI epitope (Fig. 3). In the four HLA-B*3501-positive study subjects with a response to NP418−426 ESV, the response to this epitope was immunodominant within the NP-specific response, as was shown by using recombinant NP (Fig. 4, upper panels). It was also an immunodominant HLA-B*3501-restricted response, as was shown by using virus-infected C1R cells that express only HLA-B*3501 for restimulation (Fig. 4, lower panels). The loss of the NP418−426 ESV epitope resulted in a relative reduction in virus-specific CTL response in vitro of 20–32% (Fig. 5c).
Fig. 4.
Percentages of virus-specific CD8+ T cells in in vitro-stimulated peripheral blood mononuclear cell (PBMC) cultures. Percentages of interferon (IFN)-γ + CD8+ T cells were determined in influenza virus A/NL/95-ESV, -DPI and -DRI-stimulated PBMC cultures. The expanded PBMC were restimulated with major histocompatibility complex (MHC) class I-matched B-lymphoblastoid cell lines (BLCL) (upper panels) or human leucocyte antigen (HLA)-B*3501-transfected C1R-cells (lower panels) that were infected with influenza virus A/NL/95-ESV, -DPI or -DRI, or that were incubated with recombinant influenza virus nucleoprotein (rNP), derived from influenza virus A/PR/8/34 (rNP-PR), A/HK/2/68 (rNP-HK) or A/NL/18/94 (rNP-NL). Virus-specific cytotoxic T lymphocytes (CTL) were visualized after staining with monoclonal antibodies specific for CD3, CD8 and IFN-γ. The data of a representative experiment are shown (study subject 3180).
Fig. 5.
Reduction of the influenza virus-specific cytotoxic T lymphocyte (CTL) response in vitro caused by amino acid variation within the nucleoprotein (NP)418−426 epitope. Reduction in the percentages of virus-specific interferon (IFN)-γ + CD8+ T cells in the recombinant virus stimulated peripheral blood mononuclear cell (PBMC) cultures is shown for all six study subjects. Reduction was calculated by subtracting the percentage of IFN-γ + CD8+ T cells after restimulation with influenza virus A/NL/95-DRI from the percentage of IFN-γ + CD8+ T cells after restimulation with influenza virus A/NL/95-ESV (a, c) or -DPI (b, d). The percentage of IFN-γ + CD8+ T cells is based on the analysis as depicted in Fig. 4 (upper panels). The relative reduction in the percentages of virus-specific IFN-γ + CD8+ T cells in PBMC cultures (c, d) was calculated as follows: 100 × [(percentage of IFN-γ + CD8+ T cells after restimulation with influenza virus A/NL/95-DRI × 100)/percentage of IFN-γ + CD8+ T cells after restimulation with influenza virus A/NL/95-ESV or -DPI]. In all four panels, the average is shown (–). The symbols refer to the study subjects listed in Table 2.
NP-specific killing of target cells in vitro is reduced by the loss of the NP418−426 epitope
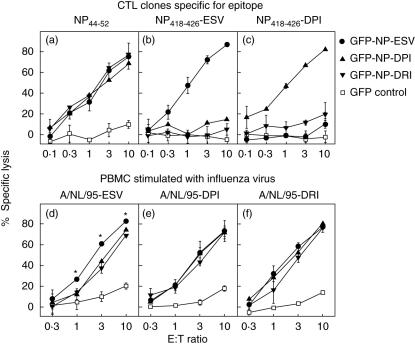
Because the lytic activity of CTL is probably most relevant for the elimination of infected cells and clearance of infections, we wished to investigate the effect of epitope loss on the lytic activity of the CTL response in vitro. First, the newly developed FATT–CTL assay was evaluated for this purpose. This assay allows the detection and quantification of the extent of target cell elimination by flow cytometry upon transfection of the target cells, with plasmids expressing the gene of interest as GFP-fusion proteins [28]. MHC class I-matched BLCL were transfected with plasmid expressing NP-GFP with the ESV, DPI or DRI variant of the NP418−26 epitope and were incubated with CTL clones specific for the conserved NP44−52 epitope or CTL clones specific for the NP418−426 ESV or DPI epitope. As shown in Fig. 6, both NP418−426-specific CTL clones lysed BLCL transfected with plasmids expressing the corresponding homologous NP418−426 epitope variants and failed to lyse BLCL expressing the NP with the DRI variant of the NP418−426 epitope, whereas the control NP44−52-specific CTL clone lysed BLCL transfected with each of the variant NP-GFP plasmids (Fig. 6a–c). To study the impact of the loss of the NP418−426 epitope on the lytic activity of polyclonal virus-specific CD8+ T cell populations, PBMC of the HLA-B*3501-positive study subjects 3180, 6358 and 0775 were stimulated with influenza viruses A/NL/95-ESV, -DPI and -DRI. The highest lytic activity was observed against cells transfected with plasmid GFP-NP ESV in polyclonal CD8+ T cell populations stimulated with influenza virus A/NL/95-ESV (Student's t-test, P < 0·05). The lytic activity in these cultures against cells transfected with plasmids GFP-NP-DPI and -DRI was comparable to that observed in PBMC cultures stimulated with influenza viruses A/NL/95-DPI and -DRI. In all three study subjects tested, similar lytic activity was observed, as shown in Fig. 6d–f).
Fig. 6.
Amino acid variation in the nucleoprotein (NP)418−426 epitope affects the lytic activity of cytotoxic T lymphocytes (CTL) in vitro. Human leucocyte antigen (HLA)-A*0101- and -B*3501-positive B-lymphoblastoid cell lines (BLCL) were transfected with plasmid expressing only GFP (□), GFP-NP ESV (•), -DPI (▴) or -DRI (▾) and were used as target cells for CTL clones specific for the HLA-A*0101-restricted NP44−52 epitope (a) or the HLA-B*3501-restricted NP418−426 epitopes ESV (b) or DPI (c), or as target cells for CD8+ cells isolated from peripheral blood mononuclear cell (PBMC) cultures stimulated with influenza virus A/NL/95-ESV (d), -DPI (e) or -DRI (f) in the fluorescent antigen-transfected target cell (FATT)–CTL assay. Effector cells were added at different effector : target ratios as indicated, and percentages of specific lysis were calculated. The error bars indicate the standard deviation. The asterisks indicate statistical significance (Student's t-test, P < 0·05). For graphs d–f, the result of a representative experiment is shown (study subject 6358).
Discussion
In the present study, we examined the effect of the loss of the hypervariable NP418−426 epitope on the human influenza virus-specific CTL response in vitro. The loss of this epitope affected the virus-specific CTL response of HLA-B*3501-positive study subjects significantly, resulting in reduced IFN-γ production and lytic activity.
In order to study CTL responses against influenza viruses with or without the NP418−426 epitope in vitro, three identical recombinant influenza viruses were generated, differing only in their NP418−426 amino acid sequence. We used the epitope sequence of variants that are not recognized by CTL specific for the contemporary variant of the epitope [17,22], which was confirmed by showing that MHC class I-matched BLCL infected with influenza virus A/NL/95-DRI were not recognized by clonal or polyclonal CTL populations specific for the NP418−426 ESV variant of the epitope (Figs 1 and 3). The introduction of historic influenza virus NP418−426 amino acid sequences into a more recent influenza virus-backbone did not affect viral fitness, infection, antigen processing or presentation. Both with clonal and polyclonal NP418−426-specific T cell populations, no or very little cross-reactivity was observed with heterologous peptide variants, which is in accordance with previous findings [17,22], and which justified the use of these NP418−426-variant sequences as epitopes no longer recognized by ESV-specific CTL. Indeed,ESV-specific CD8+ T cells that were detected in four of the six HLA-B*3501-positive subjects studied did not cross-react with the two peptide variants. In one of the two other subjects, a response was detected against the DPI-variant epitope, which cross-reacted to some extent with the ESV-variant epitope. The differences in NP418−426 response most probably represent differences in history of infection and exposure to the various variants [22]. In none of the PBMC cultures stimulated with influenza virus with the DRI variant of the epitope were CTL detected as reactive with the ESV or the DPI variant. The data obtained with tetramer staining were confirmed by intracellular IFN-γ staining upon restimulation with the respective peptide variants. In influenza virus A/NL/95-ESV-stimulated T cell populations a statistically significant reduction was observed after restimulation with influenza virus A/NL/95-DRI, especially in the study subjects with an appreciable response to the ESV variant of the epitope. In these subjects the reduction accounted for 20–32% of the overall influenza virus-specific CTL response. A similar reduction of the in vitro CTL response was observed after the loss of the HLA-B*2705-restricted NP383−391 epitope [19]. Next, we wished to determine whether the reduction of the IFN-γ response correlated with a reduction in lytic activity of these virus-specific CTL, as the elimination of virus-infected cells is considered to be important for the viral clearance and control of the infection in vivo [26,27]. The NP is a major target for the human influenza virus-specific CTL response [34] and most CTL epitopes that have been identified are located in this protein [15,35]. Therefore, we measured NP-specific lytic activity of the in vitro-expanded polyclonal T cell populations in the FATT–CTL assay. In contrast to the traditional chromium-release assay, the FATT–CTL assay allows the identification of protein-expressing target cells, which increases the sensitivity of the assay and the window of opportunity to measure small differences in the lytic activity of T cell populations [28]. We assessed the effect of variation in epitope sequences on the NP-specific lytic activity of polyclonal CTL responses in vitro. Amino acid substitutions at the TCR contact residues of the NP418−426 epitope reduced the lytic activity of CTL obtained from HLA-B*3501-positive individuals significantly. Similar results were obtained with influenza viruses with and without the NP383−391 epitope and polyclonal virus-specific CTL populations (data not shown). Thus, both amino acid substitutions at TCR contact residues and anchor residues can result in impairment of the lytic activity of the CTL response. During chronic virus infections a potent and focused CD8+ T cell response is correlated with a strong decline in virus titres [36–39]. However, the emergence of amino acid substitutions within immunodominant epitopes can diminish CTL recognition, resulting in loss of control of virus replication [11–13]. The mutant virus becomes predominant and the wild-type virus eliminated, as a result of intrahost selective pressure by virus-specific CTL [40–44]. Because influenza A viruses cause acute infections, the selective pressure within individual patients may be limited. There is no evidence that the NP418−426 epitope sequence varies within or between individual patients during a single outbreak. Influenza viruses are present in the human population persistently, causing worldwide epidemics annually. Therefore, selective pressure by CTL on influenza viruses may take place at the population level. Indeed, in a theoretical model small intrahost advantages and population dynamics could explain the rapid fixation of mutations in CTL epitopes [45]. As expected, and in accordance with previous reports [46–49], reduction of the lytic capacity of the CTL response correlated with a reduction in the number of virus-specific CD8+ T cells that could respond. Although it has been possible with the FATT–CTL assay to measure lytic activity against HIV-1 in PBMC ex vivo, without prior expansion of virus-specific CTL [28] this was not possible for influenza virus-specific CTL (data not shown). Most probably, the number of virus-specific CTL in chronically infected HIV-1 patients is much higher and they may have the effector phenotype, unlike the influenza virus-specific memory cells in peripheral blood [50,51].
Collectively, the data show that the loss of, or the variation in, individual CTL epitopes can affect the influenza A virus-specific immune response significantly. It results not only in a reduction of the number of virus-specific CD8+ T cells that can respond to produce cytokines, such as IFN-γ, but it also impaired the lytic activity towards infected cells. This, in turn, may result in delayed clearance of influenza virus infection accompanied with more severe disease and increased mortality rates, as was also shown in C57BL/6 mice infected with a virus from which the immunodominant H-2Db-restricted NP366−374 epitope was deleted [52]. Their high mutation rate and adaptive nature allow influenza viruses to evade both humoral and cell-mediated host immunity, which may contribute to their persistence in the human population. Furthermore, the variability in CTL epitopes may have implications for the development of vaccines, which also aim at the induction of CTL responses. The use of influenza virus A/PR/8/34 as vaccine-backbone strain or other influenza virus strains (e.g. the cold adapted strains), of which CTL epitope sequences do not match fully with current epidemic strains or future heterosubtypic pandemic strains, may lead to suboptimal CTL responses, which may in turn affect vaccine effectiveness.
Acknowledgments
This work was supported financially by European Union grant QLRT-2001–01034 (Novaflu). The authors thank T. M. Bestebroer for excellent technical assistance, and B. Tomson and Y. Kruyt for the selection of HLA-typed blood donors (Sanquin Bloodbank).
References
- 1.Taylor PM, Askonas BA. Influenza nucleoprotein-specific cytotoxic T-cell clones are protective in vivo. Immunology. 1986;58:417–20. [PMC free article] [PubMed] [Google Scholar]
- 2.Yap KL, Ada GL, McKenzie IF. Transfer of specific cytotoxic T lymphocytes protects mice inoculated with influenza virus. Nature. 1978;273:238–9. doi: 10.1038/273238a0. [DOI] [PubMed] [Google Scholar]
- 3.Wells MA, Ennis FA, Albrecht P. Recovery from a viral respiratory infection. II. Passive transfer of immune spleen cells to mice with influenza pneumonia. J Immunol. 1981;126:1042–6. [PubMed] [Google Scholar]
- 4.Yap KL, Ada GL. The recovery of mice from influenza virus infection: adoptive transfer of immunity with immune T lymphocytes. Scand J Immunol. 1978;7:389–97. doi: 10.1111/j.1365-3083.1978.tb00469.x. [DOI] [PubMed] [Google Scholar]
- 5.Mackenzie CD, Taylor PM, Askonas BA. Rapid recovery of lung histology correlates with clearance of influenza virus by specific CD8+ cytotoxic T cells. Immunology. 1989;67:375–81. [PMC free article] [PubMed] [Google Scholar]
- 6.Bender BS, Croghan T, Zhang L, Small PA., Jr Transgenic mice lacking class I major histocompatibility complex-restricted T cells have delayed viral clearance and increased mortality after influenza virus challenge. J Exp Med. 1992;175:1143–5. doi: 10.1084/jem.175.4.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wells MA, Albrecht P, Ennis FA. Recovery from a viral respiratory infection. I. Influenza pneumonia in normal and T-deficient mice. J Immunol. 1981;126:1036–41. [PubMed] [Google Scholar]
- 8.Schulman JL, Petigrow C, Woodruff J. Effects of cell mediated immunity in influenza virus infection in mice. Dev Biol Stand. 1977;39:385–90. [PubMed] [Google Scholar]
- 9.McMichael AJ, Gotch FM, Noble GR, Beare PA. Cytotoxic T-cell immunity to influenza. N Engl J Med. 1983;309:13–17. doi: 10.1056/NEJM198307073090103. [DOI] [PubMed] [Google Scholar]
- 10.McMichael AJ, Michie CA, Gotch FM, Smith GL, Moss B. Recognition of influenza A virus nucleoprotein by human cytotoxic T lymphocytes. J Gen Virol. 1986;67:719–26. doi: 10.1099/0022-1317-67-4-719. [DOI] [PubMed] [Google Scholar]
- 11.Koup RA. Virus escape from CTL recognition. J Exp Med. 1994;180:779–82. doi: 10.1084/jem.180.3.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oldstone MB. How viruses escape from cytotoxic T lymphocytes. molecular parameters and players. Virology. 1997;234:179–85. doi: 10.1006/viro.1997.8674. [DOI] [PubMed] [Google Scholar]
- 13.Ploegh HL. Viral strategies of immune evasion. Science. 1998;280:248–53. doi: 10.1126/science.280.5361.248. [DOI] [PubMed] [Google Scholar]
- 14.Price GE, Ou R, Jiang H, Huang L, Moskophidis D. Viral escape by selection of cytotoxic T cell-resistant variants in influenza A virus pneumonia. J Exp Med. 2000;191:1853–67. doi: 10.1084/jem.191.11.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker CE, Gould KG. Influenza A virus − a model for viral antigen presentation to cytotoxic T-lymphocytes. Semin Virol. 1996;7:61–73. [Google Scholar]
- 16.Rimmelzwaan GF, Boon AC, Voeten JT, Berkhoff EG, Fouchier RA, Osterhaus AD. Sequence variation in the influenza A virus nucleoprotein associated with escape from cytotoxic T lymphocytes. Virus Res. 2004;103:97–100. doi: 10.1016/j.virusres.2004.02.020. [DOI] [PubMed] [Google Scholar]
- 17.Boon AC, de Mutsert G, Graus YM, et al. Sequence variation in a newly identified HLA-B35-restricted epitope in the influenza A virus nucleoprotein associated with escape from cytotoxic T lymphocytes. J Virol. 2002;76:2567–72. doi: 10.1128/jvi.76.5.2567-2572.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Voeten JT, Bestebroer TM, Nieuwkoop NJ, Fouchier RA, Osterhaus AD, Rimmelzwaan GF. Antigenic drift in the influenza A virus(H3N2) nucleoprotein and escape from recognition by cytotoxic T lymphocytes. J Virol. 2000;74:6800–7. doi: 10.1128/jvi.74.15.6800-6807.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkhoff EG, Boon AC, Nieuwkoop NJ, et al. A mutation in the HLA-B*2705-restricted NP383-391 epitope affects the human influenza A virus-specific cytotoxic T-lymphocyte response in vitro. J Virol. 2004;78:5216–22. doi: 10.1128/JVI.78.10.5216-5222.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boon AC, de Mutsert G, Fouchier RA, Osterhaus AD, Rimmelzwaan GF. The hypervariable immunodominant NP418-426 epitope from the influenza A virus nucleoprotein is recognized by cytotoxic T lymphocytes with high functional avidity. J Virol. 2006;80:6024–32. doi: 10.1128/JVI.00009-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berkhoff EG, de Wit E, Geelhoed-Mieras MM, et al. Functional constraints of influenza A virus epitopes limit escape from cytotoxic T lymphocytes. J Virol. 2005;79:11239–46. doi: 10.1128/JVI.79.17.11239-11246.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boon AC, de Mutsert G, van Baarle D, et al. Recognition of homo- and heterosubtypic variants of influenza A viruses by human CD8+ T lymphocytes. J Immunol. 2004;172:2453–60. doi: 10.4049/jimmunol.172.4.2453. [DOI] [PubMed] [Google Scholar]
- 23.Haanen JB, Wolkers MC, Kruisbeek AM, Schumacher TN. Selective expansion of cross-reactive CD8(+) memory T cells by viral variants. J Exp Med. 1999;190:1319–28. doi: 10.1084/jem.190.9.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nguyen HH, van Ginkel FW, Vu HL, Novak MJ, McGhee JR, Mestecky J. Gamma interferon is not required for mucosal cytotoxic T-lymphocyte responses or heterosubtypic immunity to influenza A virus infection in mice. J Virol. 2000;74:5495–501. doi: 10.1128/jvi.74.12.5495-5501.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Graham MB, Dalton DK, Giltinan D, Braciale VL, Stewart TA, Braciale TJ. Response to influenza infection in mice with a targeted disruption in the interferon gamma gene. J Exp Med. 1993;178:1725–32. doi: 10.1084/jem.178.5.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen HH, Boyaka PN, Moldoveanu Z, et al. Influenza virus-infected epithelial cells present viral antigens to antigen-specific CD8+ cytotoxic T lymphocytes. J Virol. 1998;72:4534–6. doi: 10.1128/jvi.72.5.4534-4536.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Baalen CA, Guillon C, van Baalen M, et al. Impact of antigen expression kinetics on the effectiveness of HIV-specific cytotoxic T lymphocytes. Eur J Immunol. 2002;32:2644–52. doi: 10.1002/1521-4141(200209)32:9<2644::AID-IMMU2644>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 28.van Baalen CA, Kwa D, Verschuren EJ, et al. Fluorescent antigen-transfected target cell cytotoxic T lymphocyte assay for ex vivo detection of antigen-specific cell-mediated cytotoxicity. J Infect Dis. 2005;192:1183–90. doi: 10.1086/444546. [DOI] [PubMed] [Google Scholar]
- 29.de Wit E, Spronken MI, Bestebroer TM, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. Efficient generation and growth of influenza virus A/PR/8/34 from eight cDNA fragments. Virus Res. 2004;103:155–61. doi: 10.1016/j.virusres.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 30.Rimmelzwaan GF, Baars M, Claas EC, Osterhaus AD. Comparison of RNA hybridization, hemagglutination assay, titration of infectious virus and immunofluorescence as methods for monitoring influenza virus replication in vitro. J Virol Meth. 1998;74:57–66. doi: 10.1016/s0166-0934(98)00071-8. [DOI] [PubMed] [Google Scholar]
- 31.Boon AC, de Mutsert G, Graus YM, et al. The magnitude and specificity of influenza A virus-specific cytotoxic T-lymphocyte responses in humans is related to HLA-A and -B phenotype. J Virol. 2002;76:582–90. doi: 10.1128/JVI.76.2.582-590.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rimmelzwaan GF, Nieuwkoop N, Brandenburg A, et al. A randomized, double blind study in young healthy adults comparing cell mediated and humoral immune responses induced by influenza ISCOM vaccines and conventional vaccines. Vaccine. 2000;19:1180–7. doi: 10.1016/s0264-410x(00)00310-8. [DOI] [PubMed] [Google Scholar]
- 33.Voeten JT, Rimmelzwaan GF, Nieuwkoop NJ, Fouchier RA, Osterhaus AD. Antigen processing for MHC class I restricted presentation of exogenous influenza A virus nucleoproteinby B-lymphoblastoid cells. Clin Exp Immunol. 2001;125:423–31. doi: 10.1046/j.1365-2249.2001.01613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gotch F, McMichael A, Smith G, Moss B. Identification of viral molecules recognized by influenza-specific human cytotoxic T lymphocytes. J Exp Med. 1987;165:408–16. doi: 10.1084/jem.165.2.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epstein SL, Yewdell JW, Bennink JR. Known influenza virus antigenic peptides listed by restricting major histocompatibility complex molecules. The Influenza Sequence Database (ISD) [18 December 2006];2003 Available at: http://www.flu.lanl.gov/.
- 36.Koup RA, Safrit JT, Cao Y, et al. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J Virol. 1994;68:4650–5. doi: 10.1128/jvi.68.7.4650-4655.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borrow P, Lewicki H, Hahn BH, Shaw GM, Oldstone MB. Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J Virol. 1994;68:6103–10. doi: 10.1128/jvi.68.9.6103-6110.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guidotti LG, Ishikawa T, Hobbs MV, Matzke B, Schreiber R, Chisari FV. Intracellular inactivation of the hepatitis B virus by cytotoxic T lymphocytes. Immunity. 1996;4:25–36. doi: 10.1016/s1074-7613(00)80295-2. [DOI] [PubMed] [Google Scholar]
- 39.Lechner F, Wong DK, Dunbar PR, et al. Analysis of successful immune responses in persons infected with hepatitis C virus. J Exp Med. 2000;191:1499–512. doi: 10.1084/jem.191.9.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guglietta S, Garbuglia AR, Pacciani V, et al. Positive selection of cytotoxic T lymphocyte escape variants during acute hepatitis C virus infection. Eur J Immunol. 2005;35:2627–37. doi: 10.1002/eji.200526067. [DOI] [PubMed] [Google Scholar]
- 41.Borrow P, Lewicki H, Wei X, et al. Antiviral pressure exerted by HIV-1-specific cytotoxic T lymphocytes (CTLs) during primary infection demonstrated by rapid selection of CTL escape virus. Nat Med. 1997;3:205–11. doi: 10.1038/nm0297-205. [DOI] [PubMed] [Google Scholar]
- 42.Burrows JM, Burrows SR, Poulsen LM, Sculley TB, Moss DJ, Khanna R. Unusually high frequency of Epstein–Barr virus genetic variants in Papua New Guinea that can escape cytotoxic T-cell recognition: implications for virus evolution. J Virol. 1996;70:2490–6. doi: 10.1128/jvi.70.4.2490-2496.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Campos-Lima PO, Levitsky V, Brooks J, et al. T cell responses and virus evolution: loss of HLA A11-restricted CTL epitopes in Epstein–Barr virus isolates from highly A11-positive populations by selective mutation of anchor residues. J Exp Med. 1994;179:1297–305. doi: 10.1084/jem.179.4.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pircher H, Moskophidis D, Rohrer U, Burki K, Hengartner H, Zinkernagel RM. Viral escape by selection of cytotoxic T cell-resistant virus variants in vivo. Nature. 1990;346:629–33. doi: 10.1038/346629a0. [DOI] [PubMed] [Google Scholar]
- 45.Gog JR, Rimmelzwaan GF, Osterhaus AD, Grenfell BT. Population dynamics of rapid fixation in cytotoxic T lymphocyte escape mutants of influenza A. Proc Natl Acad Sci USA. 2003;100:11143–7. doi: 10.1073/pnas.1830296100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Betts MR, Price DA, Brenchley JM, et al. The functional profile of primary human antiviral CD8+ T cell effector activity is dictated by cognate peptide concentration. J Immunol. 2004;172:6407–17. doi: 10.4049/jimmunol.172.10.6407. [DOI] [PubMed] [Google Scholar]
- 47.Valitutti S, Muller S, Dessing M, Lanzavecchia A. Different responses are elicited in cytotoxic T lymphocytes by different levels of T cell receptor occupancy. J Exp Med. 1996;183:1917–21. doi: 10.1084/jem.183.4.1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lim DG, Bieganowska Bourcier K, Freeman GJ, Hafler DA. Examination of CD8+ T cell function in humans using MHC class I tetramers: similar cytotoxicity but variable proliferation and cytokine production among different clonal CD8+ T cells specific to a single viral epitope. J Immunol. 2000;165:6214–20. doi: 10.4049/jimmunol.165.11.6214. [DOI] [PubMed] [Google Scholar]
- 49.Betts MR, Brenchley JM, Price DA, et al. Sensitive and viable identification of antigen-specific CD8+ T cells by a flow cytometric assay for degranulation. J Immunol Meth. 2003;281:65–78. doi: 10.1016/s0022-1759(03)00265-5. [DOI] [PubMed] [Google Scholar]
- 50.Ravkov EV, Myrick CM, Altman JD. Immediate early effector functions of virus-specific CD8+CCR7+ memory cells in humans defined by HLA and CC chemokine ligand 19 tetramers. J Immunol. 2003;170:2461–8. doi: 10.4049/jimmunol.170.5.2461. [DOI] [PubMed] [Google Scholar]
- 51.de Bree GJ, van Leeuwen EM, Out TA, Jansen HM, Jonkers RE, van Lier RA. Selective accumulation of differentiated CD8+ T cells specific for respiratory viruses in the human lung. J Exp Med. 2005;202:1433–42. doi: 10.1084/jem.20051365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Webby RJ, Andreansky S, Stambas J, et al. Protection and compensation in the influenza virus-specific CD8+ T cell response. Proc Natl Acad Sci USA. 2003;100:7235–40. doi: 10.1073/pnas.1232449100. [DOI] [PMC free article] [PubMed] [Google Scholar]