The patient
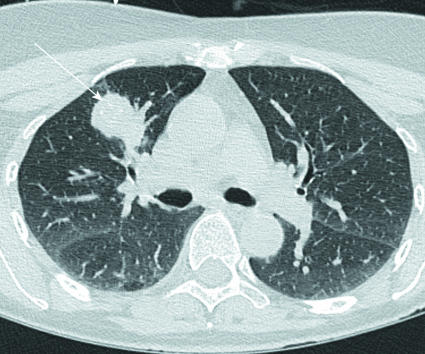
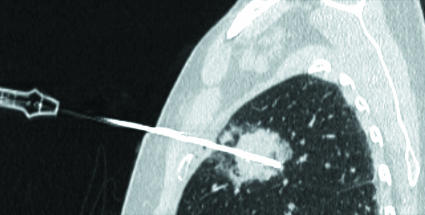
A 59 year old woman had an anterior resection for primary Dukes's C rectal carcinoma in 2004 followed by adjuvant chemotherapy. Two years later, on routine computed tomography surveillance, she was found to have liver (fig 1) and lung (fig 2) metastases.
Fig 1 Axial computed tomography of the liver showing two irregular hypoattenuating mass lesions, 4.0 cm and 4.3 cm in diameter (arrows). This is the typical appearance of colorectal liver metastases
Fig 2 Axial computed tomography section through the lung showing a 3.8 cm tumour in the right upper lobe (arrow)
Imaging for surveillance after resection of primary colorectal cancer
Surveillance is indicated in patients with Dukes's B or Dukes's C colorectal carcinoma who are potential candidates for further therapeutic intervention. The optimal surveillance strategy is a matter of debate.1 2 3 An ongoing trial (FACS) is looking at the cost effectiveness of intensive follow-up or no follow-up in patients with successfully resected colorectal cancer (www.facs.soton.ac.uk/). Currently, most centres opt for computed tomography scans at six or 12 monthly intervals for the first two or three years, combined with regular measurements of serum carcinoembryonic antigen.
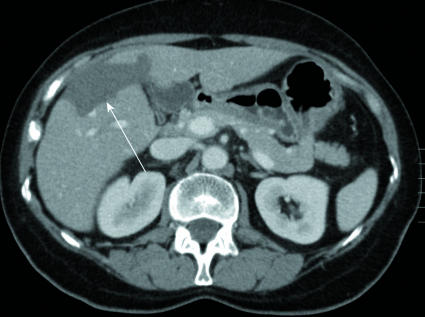
Because the liver metastases were centrally located in our patient, surgery would have involved removal of three quarters of the liver, followed by pulmonary lobectomy for the lung metastasis. Liver resection and pulmonary resection are associated with a small increase in mortality—less than 5% for liver resection and less than 2% for pulmonary resection—and combined liver and lung resection has been reported to improve survival for patients with metastases from colorectal cancer.4 However, in light of the substantial morbidity (<37%) associated with major liver surgery and the need for two surgical procedures, the patient opted for radiofrequency ablation to both areas (fig 3).
Fig 3 Oblique reformatted computed tomography image, along the line of the electrode, taken during the lung ablation shows the electrode inserted through the anterior chest wall into the tumour
Our standard investigation for radiofrequency ablation is high quality, contrast enhanced, multidetector computed tomography, with occasional positron emission tomography-computed tomography or liver magnetic resonance imaging where specific questions need to be answered. These last two tests are used more often when investigating patients for liver resection; this is warranted given that resection is a more invasive and expensive procedure.
After written informed consent, the liver lesions were ablated under general anaesthesia using an array of three water cooled electrodes. One month later, the patient had ablation of the lung metastasis, which was performed under conscious sedation (midazolam and fentanyl) with a single water cooled electrode. After ablation, she received systemic chemotherapy with oxaliplatin and fluorouracil.
Outcome
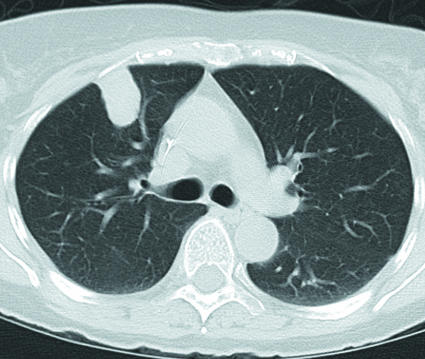
Follow-up scans performed four to five months after ablation show absent enhancement at the treated sites in the liver and lung consistent with ablated tumour (figs 4, 5).
Fig 4 Computed tomography scans of the liver at five months after ablation showing a shrinking zone of ablation (arrows). Viable tumour is not seen
Fig 5 Computed tomography scan of the lung at four months after ablation showing a homogeneous ablation zone with no enhancement, indicating successful ablation
What is radiofrequency ablation?
Radiofrequency ablation is a minimally invasive, image guided technique that delivers focused thermal energy directly to the tumour. Needle electrodes are positioned percutaneously into the tumour and an alternating current is applied which produces ionic agitation, frictional heating, and cell death. After successful ablation, computed tomography scans show an area of absent enhancement, which becomes smaller over time. Radiofrequency ablation for primary and secondary liver and lung tumours has been approved by the National Institute for Health and Clinical Excellence within the context of ongoing audit and research (www.nice.org.uk/). Other focal ablative techniques for the destruction of tumour include cryotherapy, microwaves, lasers, and high intensity focused ultrasound, but radiofrequency ablation is the most widely used technique at present.
Complications
Complications after liver ablation include bleeding and abscess formation. Thermal injury to adjacent vulnerable structures, such as the bowel, can usually be avoided. Complications after lung ablation include pneumothorax (which occurs in about 40% of patients, although only 10% need aspiration or intercostal tube insertion), haemorrhage, pleural effusion, and infection. Contraindications to radiofrequency ablation include a predisposition to bleeding or, in the case of lung ablation, limited pulmonary reserve (forced expiratory volume in one second <1.0 litre). Treatment of small areas can be performed under conscious sedation; general anaesthesia is needed for larger treatments. Most patients spend one night in hospital.
Indications
Radiofrequency ablation is used in patients with limited numbers of moderately sized (<5 cm diameter) metastases for whom surgical resection is not an option. Surgery may be contraindicated for many reasons including the location or distribution of the tumour or associated comorbidity. As a result, only 15% of patients with liver metastases are candidates for surgery. Yet colon cancer is the third most common cause of death from cancer, and 50% of patients with colorectal cancer develop liver metastases. In the absence of imaging follow-up most patients present with extensive tumour. As both liver resection and ablation can be applied only to patients with limited disease, surveillance scans, which detect limited disease that can subsequently be treated, should help improve survival. Radiofrequency can be used in isolation or in conjunction with surgical resection or chemotherapy.
Survival
Although no randomised controlled trials exist to date, several centres have published results from case series of more than 100 patients. In our series of 167 patients with colorectal liver metastases who could not undergo resection, a subgroup of patients with five or fewer metastases, the largest of which measured less than 5 cm, and with no extrahepatic disease had a five year survival of 29%.5 Other groups report similar results.6 These results are not dissimilar to those for surgical resection in patients suitable for surgery, who have a five year survival of around 40%. Anecdotal evidence suggests that the combination of destruction of all macroscopically detected tumours with radiofrequency ablation followed by aggressive systemic chemotherapy improves survival the most. We therefore gave our patient systemic chemotherapy after ablation. Systemic chemotherapy is the first line of treatment for patients whose tumours are too large for them to undergo ablation or resection. This treatment aims to reduce the size of the tumour, so that surgery or ablation can be carried out.
Learning points
Regular computed tomography is the recommended imaging technique for the follow-up of patients with colorectal cancer
Radiofrequency ablation is less invasive than surgery and can provide a five year survival of 29% for patients with limited liver metastases after primary colorectal cancer
Radiofrequency ablation is also effective for lung tumours, either primary or secondary
Footnotes
This series provides an update on the best use of different imaging methods for common or important clinical presentations. The series editors are Fergus Gleeson, consultant radiologist, Churchill Hospital, Oxford, and Kamini Patel, consultant radiologist, Homerton University Hospital, London
References
- 1.Chau I, Allen MJ, Cunningham D, Norman AR, Brown G, Ford HE, et al. The value of routine serum carcino-embryonic antigen measurement and computed tomography in the surveillance of patients after adjuvant chemotherapy for colorectal cancer. J Clin Oncol 2004;22:1420-9. [DOI] [PubMed] [Google Scholar]
- 2.Mortazavi A, Shaukat A, Othman E, Kepner JL, Fakih MG, Kuvshinoff BW, et al. Postoperative computed tomography scan surveillance for patients with stage II and III colorectal cancer: worthy of further study? Am J Clin Oncol 2005;28:30-5. [DOI] [PubMed] [Google Scholar]
- 3.Desch CE, Benson AB III, Somerfield MR, Flynn PJ, Krause C, Loprinzi CL, et al. Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline. J Clin Oncol 2005;23:8512-9. [DOI] [PubMed] [Google Scholar]
- 4.Shah SA, Haddad R, Al Sukhni W, Kim RD, Greig PD, Grant DR, et al. Surgical resection of hepatic and pulmonary metastases from colorectal carcinoma. J Am Coll Surg 2006;202:468-75. [DOI] [PubMed] [Google Scholar]
- 5.Gillams AR, Lees WR. Radio-frequency ablation of colorectal liver metastases in 167 patients. Eur Radiol 2004;14:2261-7. [DOI] [PubMed] [Google Scholar]
- 6.Solbiati L, Livraghi T, Goldberg SN, Ierace T, Meloni F, Dellanoce M, et al. Percutaneous radio-frequency ablation of hepatic metastases from colorectal cancer: long-term results in 117 patients. Radiology 2001;221:159-66. [DOI] [PubMed] [Google Scholar]