Abstract
Background
The number of cases of mumps in the UK has increased during 2004–2005. Understanding why some people are more susceptible to mumps infection will help target vaccination and other control measures in the future. This paper describes a mumps outbreak in a boarding school in Scotland (October to November 2004).
Objectives
To describe the characteristics of cases in a mumps outbreak; and to conduct a case-control study looking at the effect of previous measles-mumps-rubella (MMR) vaccination.
Design
Descriptive epidemiology.
Data sources
Clinical, laboratory and surveillance data.
Setting
A private school with 600 boarding and day pupils.
Results
Fifty cases were notified to the public health department as having mumps. Twenty of the cases (40%) were confirmed virologically, all born between 1987–1991. A matched case-control study was conducted to explore the effect of prior MMR vaccination. Compared to no vaccine, MMR protected against mumps (odds ratio = 0.7), two doses offering best protection (odds ratio = 0.5), but the study was not large enough to detect a statistically significant difference.
Conclusion
Some children and young people in the UK are currently incompletely vaccinated. This outbreak illustrates the potential of a mumps outbreak to disrupt the medical, educational and social life of a school. All children should be vaccinated with two doses of MMR vaccine before school entry. Children and young people born between 1979–1991 should be given the necessary additional dose(s) of MMR vaccine.
Keywords: measles-mumps-rubella vaccine, mumps infection, outbreaks
INTRODUCTION
Mumps is caused by a paramyxovirus. Symptoms are typically mild and include fever, malaise and a characteristic parotid swelling. Complications include aseptic meningitis, pancreatitis, orchitis and oophritis. Some cases may, however, be subclinical or have an atypical presentation.1 The virus is spread by airborne droplets and the incubation period is 14–21 days, with an infectious period from 2 days before onset of parotitis to 9 days afterwards.
In the UK mumps was a relatively common childhood infection until the introduction of the measles-mumps-rubella (MMR) vaccine in 1988. There were 3095 notifications in 1989 falling to 155 notifications in 2001.2 Recently, however, there has been an increase in the number of cases of mumps in Scotland, from 182 (2003) to 3592 (2004).3
The rise in cases has included outbreaks in schools and colleges of further education across Scotland and the rest of the UK.4 This increase in cases has a number of possible explanations. MMR vaccination was introduced in a single dose in 1988, with a second dose offering increased protection introduced in 1996. People born between 1979 and 1991 may be incompletely vaccinated and may not have come into contact with the wild mumps strain and could therefore be at particular risk of mumps infection. Secondly, discredited scientific papers published in the late 1990s5 led to poor uptake of MMR vaccine in some communities. Uptake of MMR varies internationally.6
This report describes an outbreak of mumps in a co-educational private school in Lothian, Scotland with a large number of international pupils. The school takes around 600 boarding and day pupils aged 7–18 years and has a well-resourced medical centre. The school is split into a number of ‘houses’ that operate independently for much of the school day although pupils come together at assembly and mealtimes. The aim of the study was to describe the groups at risk of mumps infection so that these groups can be given the MMR vaccine to reduce the chances of further outbreak of mumps elsewhere. Additionally, a case-control study was conducted to explore the effect of previous MMR vaccination.
METHOD
Four outbreak control team meetings were held in the school to discuss the epidemiology and control of the outbreak. Participants included school medical and nursing staff, senior teaching staff, a consultant virologist and members of the local public health department. A number of control measures were put in place following the first outbreak control team meeting. Vaccination was planned in conjunction with the Health Protection Team of the public health department, but the administration of vaccine was delayed for some pupils because of questions and concerns from parents about MMR vaccine. Movement between school houses was restricted and social and sporting functions with other schools were also cancelled. Patients with mumps were not allowed to return to school for 10 days following onset of parotid swelling, and were asked to either return home or stay in the school medical centre during the period of recovery.
Participants were all suspected cases of mumps (n = 50) from a single boarding school notified to the consultant in public health medicine (October to November 2004). Data were collected by clinical staff involved in the management of the outbreak, supplemented subsequently with laboratory and surveillance data. The agreed case definition was parotid swelling, viral illness and no other reasonable cause. Virology results were available from the local virology laboratory and the national reference laboratory. Acute cases of mumps were identified using a combination of parotid swab, acute and convalescent sera, urine or salivary testing. Virologically confirmed cases (n = 20) met the case definition and had one or more positive tests on virological testing. Clinical cases (n = 30) met the case definition but without virological testing or with only negative results.
How this fits in
Children and young people born between 1979 and 1991 who have not received both doses of MMR may be at particular risk of mumps infection. All virologically confirmed cases of mumps in this outbreak were born between 1987 and 1991, and were therefore in the age group thought to be most at risk. Prior MMR vaccination (particularly two doses of MMR) appeared to offer protection against mumps infection in this outbreak. Children and young people should have additional doses of MMR if they are incompletely vaccinated or unvaccinated.
Data about vaccination status were available from a number of sources, including pupil medical notes held in the school, telephone and email communication with parents and, for local pupils, the Scottish Immunisation Recall System.
A case-control study was conducted using pre-outbreak vaccination status from controls matched to controls for age, sex, residential status and whether they were a UK or international student. Two controls were selected for each case. Controls had no record of previous mumps infection. Day pupils were less likely to have had virological testing so no further analysis based on residential status or usual country of residence has been attempted beyond the case-control study.
Data collection was performed by school nursing and medical staff and the principal author. Data analysis was performed in Microsoft Excel®. Sample size calculations for the case control study were estimated for statistical power 0.8 and statistical significance 0.05 using published equations.7
RESULTS
There were 50 cases notified as having mumps (30 clinical with 20 virologically confirmed). The mumps virus genotype identified was G2, identical to a currently circulating wild-type strain (L Jin, personal communication, 2005). Virologically confirmed cases (n = 20) were all born between 1987–1991 and in total 48/50 (96%) notified cases were in this age group. There were 18 boarding pupils and two day pupils with virologically confirmed mumps. There were equal numbers of students from the UK (n = 10) and other countries (n = 10) with virologically confirmed mumps. None of the cases required admission to hospital and none of the cases had complications of mumps.
The outbreak curve is shown in Figure 1. The index case became ill on day 1, with secondary cases starting on day 18. The number of cases peaked on day 21. Following the second wave of cases, all but one of the subsequent cases were clinical, without virological confirmation. There have been no further cases of mumps in the school (to November 2005). The timing of the first outbreak control team meeting, vaccinations and half-term holiday are also shown in Figure 1. Control measures were put in place at the outbreak control team meeting.
Figure 1.
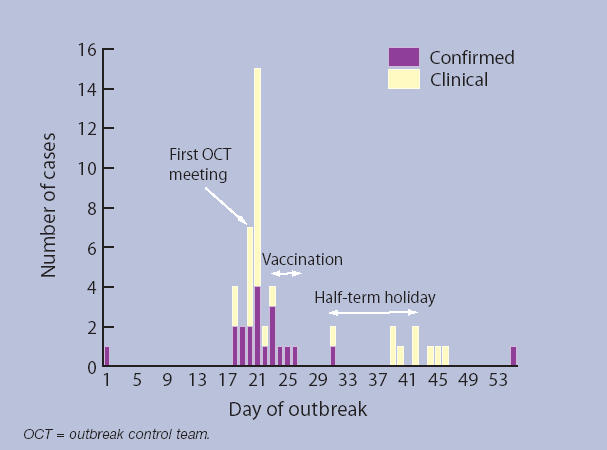
Outbreak curve (date of onset not known for one participant, so n = 58).
Table 1 shows the results of the case-control study. Compared to no vaccine, MMR vaccine appeared to protect against mumps (odds ratio = 0.7; 95% confidence interval (CI) = 0.2 to 2.0) and two doses of MMR vaccine offered best protection (odds ratio = 0.5; 95% CI = 0.1 to 3.2).
Table 1.
Results of case-control study (n = 60, 20 virologically confirmed cases, 40 controls without signs or symptoms of mumps). Two controls were matched to each virologically confirmed case, matched for age, sex, residential status and whether UK or international student.
| Odds ratios (and 95% CIs) | ||||||
|---|---|---|---|---|---|---|
| No MMR vaccine | One dose of MMR vaccine | Two doses of MMR vaccine | No vaccine versus any MMR | No vaccine versus two doses of MMR | One dose of MMR versus two doses of MMR | |
| Cases (n = 20) | 9 | 9 | 2 | 0.66 (0.22 to 2.00) | 0.52 (0.09 to 3.16) | 0.74 (0.12 to 4.40) |
| Controls (n = 40) | 14 | 20 | 6 | – | – | – |
DISCUSSION
Summary of main findings
There were 50 clinical cases of mumps in this outbreak and 20 were virologically confirmed. All the confirmed cases were in patients in their teenage years (born between 1987–1991). This outbreak included day and boarding pupils and UK and international pupils.
MMR vaccination prior to the outbreak appeared to be protective against mumps infection, particularly two doses of MMR vaccine. However the case-control study was not large enough to detect a statistically significant difference. Using the odds ratio comparing no MMR vaccine with two doses of MMR, the number of cases of mumps required to identify a statistically significant difference would have been 378.
Other public health measures taken to limit the spread of infection included restriction in movement of pupils in the school, cancellation of school events, and exclusion for 10 days. These control measures may have limited the spread of mumps infection, but the half-term holiday may also have limited the number of cases. The control measures resulted in considerable disruption to staff, parents and pupils at the school and school medical centre, impacting on educational, social and sporting activities at the school.
Strengths and limitations of the study
This study has described the epidemiology of a mumps outbreak in a UK boarding school. The study has used clinical data provided by pupils, parents, and medical staff, and virology data from the standard laboratory tests recommended during the outbreak. The findings are therefore particularly relevant to clinical practice.
The reliance on clinical information has, however, resulted in important limitations to this study. Only 40% of notified cases were virologically confirmed as many cases were incompletely investigated. Day pupils were less likely to have had virological testing, particularly if they attended their own doctor rather than the school medical centre. While the undersampling is unfortunate from an epidemiological perspective, this is not unexpected as there were other clinical priorities during the outbreak. Controls in the case-control study had not had virological testing, and it is possible therefore that some controls were infected during the outbreak but remained asymptomatic or had atypical symptoms, and it is possible that some controls had been infected previously.
There were also questions about the accuracy of the reported vaccination status of some children. Children and parents were frequently not aware of which vaccines had been given in the past, with confusion about single vaccines, the measles-rubella vaccine given in the early 1990s and MMR. These concerns about the accuracy of diagnosis, recording of previous infection, and recording of vaccination status were important sources of potential bias in the case-control study.
Comparison with existing literature
The age group affected by this mumps outbreak (those born between 1987–1991) was the age group expected to be at highest risk of mumps infection because of the 8-year period between introducing the first and second doses of MMR in the UK. This finding is consistent with other UK studies.4 This observation is also consistent with recommendations from the Chief Medical Officer in Scotland who recommended opportunistic vaccination of children and young people born between 1979–1991 (August 2004).8
Implications for future research and clinical practice
The findings have relevance for primary care staff and Health Protection Teams across the UK. This outbreak occurred in a private boarding school, but the findings may also be relevant to colleges of further education and universities, many of which have residential students. The findings also reinforce the continuing concern that some parents have about MMR vaccination. This suggests that there is still more work to be done in educating parents about the safety of MMR vaccine and the wide-ranging effects that can result from mumps outbreaks as a consequence of inadequate levels of vaccination.
Many teenagers and young adults are at risk of mumps infection because they are incompletely vaccinated with MMR vaccine and have not been exposed to infection in the past. With suboptimal levels of vaccination in the UK outbreaks are now relatively common. In this outbreak children born between 1987–1991 were at particular risk, with boarding and day pupils both affected. There was widespread disruption to pupils, parents and staff beyond the effects on health. Incompletely vaccinated or unvaccinated children and young people MMR should receive full vaccination (two doses of MMR). There should also be better assessment and recording of vaccination status at entry into schools and colleges.
Acknowledgments
The authors would like to thank the staff at the Specialist Virology Centre, Edinburgh Royal Infirmary, and the staff and pupils at the boarding school for their input to this outbreak and Dr Claire Cameron and Dr John Cowden, Health Protection Scotland, for their advice about conducting a case-control study.
Funding body
This study required no additional funding
Ethics committee
The data were collected as part of the Public Health management of the outbreak. This collection of data was discussed with the local Caldicott Guardian, Acting Director of Public Health, who also agreed to the submission of the findings for publication. Staff at the school medical centre participated fully at all stages of the outbreak and subsequently in the analysis and preparation of this paper
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Ramsay ME, Brown DW, Eastcott HR, Begg NT. Saliva antibody testing and vaccination in a mumps outbreak. CDR. 1991;1:R96–R98. [PubMed] [Google Scholar]
- 2.Scottish Health on the Web. Mumps. www.show.scot.nhs.uk/scieh/Surveillance/mumps.htm (accessed 16 Feb 2005)
- 3.Cameron C. Mumps update. Health Protection Scotland Weekly Report. 2005;39:4. [Google Scholar]
- 4.Pugh RN, Akinosi B, Pooransingh S, et al. An outbreak of mumps in the metropolitan area of Walsall, UK. Int J Infect Dis. 2002;6:283–287. doi: 10.1016/s1201-9712(02)90162-1. [DOI] [PubMed] [Google Scholar]
- 5.Jackson T. TV Programme raises fresh allegations about MMR doctor. BMJ. 2004;329:1254. doi: 10.1136/bmj.329.7477.1254-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fleck F. UK and Italy have low MMR uptake. BMJ. 2003;327:1124. doi: 10.1136/bmj.327.7424.1124-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirkwood BR, Sterne JAC. Essential medical statistics. 2nd edn. Oxford: Blackwell Sciences; 2003. [Google Scholar]
- 8. Chief Medical Officer Letter. Mumps outbreaks in Scotland: offer of MMR to high risk individuals in high risk settings http://www.show.scot.nhs.uk/sehd/cmo/DC20040804mumps.pdf (accessed 5 Jun 2006)


