Abstract
There is limited evidence that dipyridamole is generally an effective antithrombotic agent when used alone, nor is there convincing evidence that the combination of aspirin and dipyridamole is more effective than aspirin alone, except perhaps in cerebrovascular disease. There is no consistent evidence to support the routine use of dipyridamole after coronary artery bypass grafting and in patients with occlusive peripheral vascular disease, although these remain common reasons for its use. Dipyridamole is a useful agent in ‘pharmacological stress’ testing in nuclear cardiology imaging and may be valuable when combined with warfarin in certain patient groups, such as those with prosthetic heart valves. When combined with aspirin, dipyridamole may be of value in the secondary prophylaxis of cerebrovascular disease, although further studies are clearly needed. In a significant proportion of cases, evidence-based medicine cannot support the current widespread continued prescription of dipyridamole in cardiological practice, but the jury is still out on cerebrovascular disease.
Keywords: dipyridamole, aspirin, thrombosis, platelets
Introduction
Dipyridamole (Persantin) was originally introduced in 1959 as an antianginal medication, since it was found to have coronary vasodilator properties, supposedly increasing coronary blood flow without significantly affecting myocardial oxygen consumption [1]. Antiplatelet effects were subsequently demonstrated in animals and humans, and since then, the drug has been advocated as an antithrombotic agent.
Since its introduction, however, the clinical significance of its antianginal and antiplatelet properties and the precise role of dipyridamole in clinical practice has been the focus of much controversy. In 1988, the Committee for the Review of Medicines decided that there was insufficient evidence to continue the previously wide ranging licensing indications for dipyridamole. Since that time the product has only been ‘officially’ licensed for use as an adjunct to oral anticoagulation for prophylaxis of thromboembolism associated with prosthetic heart valves. Despite this, dipyridamole is still a widely prescribed drug in the United Kingdom, with over 750 000 prescriptions issued each year in general practice [3], and amongst cardiovascular physicians and surgeons. A recent study of its use in an elderly American population has also suggested that the use of dipyridamole has actually increased since 1979, and that in only 20% of cases was it for its licensed indication [3]. Nevertheless, dipyridamole may be useful as a pharmacological stress agent in nuclear cardiology and recent evidence suggests some benefit from this drug as an antithrombotic agent in the secondary prevention of cerebrovascular disease.
Pathophysiology
Dipyridamole is a pyrimidi-pyrimidine compound that inhibits platelet phosphodiesterase, thereby preventing the degradation of cAMP (cyclic AMP) to AMP [4]. The increased platelet cAMP reduces platelet reactivity by decreasing cytoplasmic calcium and inhibiting platelet prostaglandin synthesis. The adenosine transport blocking effects of dipyridamole also produce elevation of tissue adenosine levels. Furthermore, dipyridamole potentiates the effects of prostacyclin by increasing synthesis, enhancing release and inhibiting the metabolic degradation of prostacyclin [5].
It is well recognised that platelets contribute to arterial thrombosis by virtue of platelet adhesion, release and aggregation. Adenosine and prostacyclin are potent inhibitors of platelet aggregation and dipyridamole acts to increase the level of adenosine at the platelet vascular-interface by reducing its cellular uptake and metabolism [6]. The drug therefore has a substantial effect in prolonging platelet survival when it is shortened in states of accelerated platelet turnover, such as in patients with prosthetic heart valves or in severe atherosclerosis [7, 8]. In combination with aspirin, the effect of dipyridamole on platelet survival is enhanced so that a dose of 100 mg when combined with aspirin has an effect as great as 400 mg daily of dipyridamole given alone [8]. Dipyridamole at high doses also inhibits platelet aggregation, inhibits the release reaction and may prevent platelet adhesion to exposed vascular sub-endothelial tissue [9]. However, the relevance of these actions to usual clinical practice where lower doses are often used is open to debate, particularly since there is little information available about the antithrombotic effectiveness at different doses of dipyridamole.
Myocardial ischaemia is believed to result from an imbalance between oxygen supply and demand. The rationale for the presumed anti-ischaemic effect of dipyridamole was presumably related to both its antithrombotic and vasodilatatory properties. Dipyridamole markedly increases oxygen supply without significantly augmenting oxygen demand, thus suggesting it should re-establish the normal oxygen balance [1]. Although initial uncontrolled studies were encouraging, dipyridamole has been largely discarded for this indication on the basis of inconsistent results in placebo controlled trials, mainly showing a lack of an acute or short-term effect. It is also considered that coronary arterial vasodilatation can be pro-ischaemic by triggering a coronary ‘steal’ phenomenon.
Clinical uses of dipyridamole
Angina and secondary prevention of myocardial infarction
The role of dipyridamole in the treatment of angina and secondary prevention of myocardial infarction has frequently been advocated, but there is limited evidence from only a few studies [10].
The first Persantin-Aspirin Reinfarction Study (PARIS I) [11] directly compared aspirin with the combination of aspirin plus dipyridamole in the secondary prevention of myocardial infarction. A total of 2026 patients were randomized to receive aspirin 324 mg three times daily or the same dose of aspirin plus dipyridamole 75 mg three times daily. The patients in each group were followed for an average of 41 months for the primary endpoints of total mortality, coronary mortality and fatal plus non-fatal myocardial infarction. Although there was a tendency toward a reduction in total mortality for each of these endpoints in both active treatment groups, this was not statistically significant.
In the second PARIS study (PARIS II) [12] patients who had survived a myocardial infarction 4 weeks to 4 months earlier were randomly assigned to receive either aspirin plus dipyridamole or placebo. Whilst there was a 24% reduction in the incidence of coronary events in the aspirin-dipyridamole treatment group, a group receiving aspirin alone was not included in the PARIS II study design. It was therefore not possible to establish directly whether aspirin, dipyridamole or the combination accounted for the beneficial result.
There have otherwise been relatively few studies to directly compare the value of aspirin alone with dipyridamole alone, or with the combination of aspirin plus dipyridamole in the treatment of angina or the secondary prevention of myocardial infarction. One reason for this is that differences between the antiplatelet regimes are likely to be relatively small and large scale studies are required of sufficient size to have power to demonstrate a significant number of vascular events. Nevertheless, a 1988 metaanalysis of 1l published randomized placebo-controlled trials evaluating the efficacy of dipyridamole for prophylaxis of angina pectoris showed that there was perhaps some evidence of a slight benefit from the drug [13]. Only published trials with random allocation of treatment, double-blind and placebo-controlled were included in the analysis [14–23]. Meta-analyses are often criticized for including many trials of heterogeneous design and size—nevertheless, a meta-analysis does attempt to make sense of a large number of smaller trials, and to give a precise answer where otherwise there is confusion. Caution is suggested, however, as meta-analyses may suggest a beneficial effect of a particular drug, whilst large, well-conducted randomized comparisons (‘mega-trials’) of the same drug(s) may show otherwise. For example, previous meta-analyses of the use of nitrates or magnesium in acute myocardial infarction have suggested a marked beneficial effect on mortality post-myocardial infarction [24, 25], but the large ISIS-4 and GISSI-3 studies did not show any significant benefit [26, 27]. Limited indirect comparisons of aspirin plus dipyridamole have so far failed to provide any clear evidence that combination therapy is more effective than medium dose aspirin alone (75–325 mg) in angina and secondary prevention of myocardial infarction [14].
Coronary artery bypass surgery
Dipyridamole continues to be commonly prescribed following coronary bypass surgery and the value of aspirin and dipyridamole in maintaining graft patency has been assessed in a number of controlled trials.
One early study randomly assigned 407 patients undergoing coronary artery bypass surgery to either combined aspirin and dipyridamole, or matching placebo [28]. Dipyridamole was started 48 h before surgery and continued post-operatively. Aspirin (325 mg) was then started a few hours following surgery and at follow up, and both early (median 8 days) and late (median 12 months) bypass graft patency were shown to be superior in the aspirin-dipyridamole treatment group [28]. However, aspirin was started at a much earlier stage than in other studies and a number of subsequent trials have indicated that aspirin (rather than dipyridamole) may well be the more important anti-thrombotic agent.
In a multicentre double-blind placebo-controlled series, 927 consecutive patients were randomized to aspirin 50 mg three times daily, aspirin 50 mg three times daily plus dipyridamole 75 mg three times daily and placebo [29, 30]. The aspirin and the aspirin plus dipyridamole groups reduced the occlusion rate of grafts compared with placebo, but only the aspirin-dipyridamole combination reduced the number of patients with at least one occluded graft. This one study suggested that perhaps the combination of aspirin and dipyridamole may be more effective than aspirin alone, although the incidence of early reoperation and hospital mortality was actually similar in all three groups [30].
By contrast, the Veterans Affairs study, which used preoperative and early postoperative aspirin, showed an impressive effect on early graft patency, also demonstrated that dipyridamole added nothing to the effects of aspirin [31]. Pantely et al. [32] reported that failure to administer dipyridamole pre-operatively and delaying aspirin-dipyridamole therapy until the third post-operative day offered no advantage over placebo. By contrast, starting aspirin within 60 h of surgery appears to significantly improve graft patency, compared with aspirin started after 60 h [33]. In all these studies, the addition of dipyridamole to either of the aspirin treatment groups did not seem to significantly improve graft patency rates.
In summary, aspirin alone has been shown to be an effective anti-thrombotic agent in patients undergoing coronary artery bypass surgery [34] and at present there is no consistent or reliable evidence to indicate that dipyridamole provides additional long term benefits on morbidity and mortality in such patients.
Coronary angioplasty
The role of combination antiplatelet therapy in coronary angioplasty was studied in a randomized double-blind placebo controlled trial by Schwartz et al. [35]. An aspirin-dipyridamole combination (330 mg-75 mg three times daily) was started 24 h prior to angioplasty and follow up coronary angiography was performed 4–7 months later. The incidence of transmural myocardial infarction was reduced in the treatment group compared with placebo, although the restenosis rate was similar.
However, combination therapy has not been shown to be superior to aspirin alone following coronary angioplasty. In addition, when compared with aspirin alone, a randomized trial of oral dipyridamole (75 mg four times daily) has not been shown to offer additional protection against abrupt closure following angioplasty [36]. However, a small retrospective study by Danchin et al. [37] using intravenous dipyridamole found a lower rate of ischaemic complications, including acute occlusion rate, following coronary interventions.
There is no evidence to support the routine use of dipyridamole in preventing coronary stent thrombosis. Until more evidence is supportive of a beneficial effect, dipyridamole is therefore not recommended for routine clinical use in coronary interventions.
Peripheral vascular disease
Antiplatelet therapy has been shown to reduce occlusion rates in peripheral vascular disease. Dipyridamole has therefore been used in peripheral vascular disease in an attempt to slow disease progression and graft occlusion rates.
An analysis of data from the Antiplatelet Trialists’ Collaboration demonstrated a substantial absolute reduction in the risk of peripheral artery occlusion (that is, 15.7% of patients treated with antiplatelet agents compared with 24.9% of corresponding controls) [38], although there is no evidence that combination therapy with regimes including dipyridamole were more effective than using aspirin alone.
A double-blind placebo controlled study of 240 patients with peripheral vascular disease, in which patients were allocated to receive either high dose aspirin (1 g day), aspirin (1 g day) plus dipyridamole (225 mg) or placebo, suggested that combination therapy with aspirin and dipyridamole was more effective than aspirin alone and placebo in reducing disease progression [39]. However, those patients assigned to receive aspirin alone had significantly more stenotic arterial lesions initially when compared to those in the combination therapy and placebo groups. There was also no evidence of an improvement in graft patency rates in patients treated prophylactically with aspirin and dipyridamole, following lower limb bypass grafts for periperal vascular disease [40].
Prosthetic heart valves
Anticoagulation significantly reduces the incidence of thromboembolic complications in patients with mechanical valve prostheses and it has been suggested that dipyridamole may serve to augment this role.
One early double-blind trial randomly assigned dipyridamole (100 mg four times daily) or placebo to patients who had been anticoagulated with warfarin following valve replacements [41]. The patients were followed up for one year and thromboembolic complications were significantly reduced in the dipyridamole treated group (1.3% vs 14.3% in placebo, P<0.01), although there was no reduction in overall mortality. However, more patients were withdrawn from the warfarin-dipyridamole group before the end of one year and there was little detailed information about the degree of anticoagulation and its relation to embolic events in both groups [42]. Nevertheless, based on evidence from this study, dipyridamole is still officially licenced for use as an adjunct to oral anticoagulation for the prophylaxis of thromboembolism associated with prosthetic heart valves.
The potential benefits of dipyridamole plus warfarin in patients with mechanical heart valves cannot be extrapolated to patients with native mitral valve disease [43] or bioprosthetic heart valves [44]. In addition, although dipyridamole has been found to reduce platelet consumption in patients with artificial valves and other arterial disease [45, 46], there is no evidence to support the use of dipyridamole alone in these patients. A prospective controlled trial of aspirin (1.3 g day−1) plus dipyridamole (200 mg daily) in patients with Starr-Edwards valves also failed to demonstrate any significant reduction in thromboembolic events [7].
Cerebrovascular disease
The role of antiplatelet therapy in cerebrovascular disease has been closely examined over recent years. For example, the Antiplatelet Trialists’ Collaboration reported an aspirin-related benefit with respect to all vascular events in high risk patients corresponding to a risk reduction of about 25% [10]. Whilst the value of aspirin is fairly well established, a number of trials have also utilized dipyridamole in combination with aspirin.
In the Accidents Ischimiques Cerebraux Lies a l’Atherosclerose (AICLA) trial 604 patients recovering from a transient ischaemic attack (TIA) or mild stroke were randomized to aspirin, aspirin plus dipyridamole or placebo [47]. The rate of cerebral infarction during the 3 year follow up was 18% in the placebo group compared with 10.5% in the aspirin group and 10.5% in the combination therapy group. Thus, the addition of dipyridamole did not appear to confer additional benefit.
The Persantine-Aspirin Trial [48] randomized patients with carotid territory TIA or minor stroke to receive aspirin (325 mg four times daily) or aspirin with dipyridamole (75 mg four times daily). There were no significant differences in the rates of cerebral infarction, retinal infarction and death between the groups and one small scale study of dipyridamole alone, in patients with a previous history of TIA, failed to show any significant reduction in cerebrovascular events or death 14 or 25 months after the start of the study [49].
The first European Stroke Prevention Study (ESPS-1) investigated the use of dipyridamole 225 mg (75 mg three times daily) with aspirin 990 mg (330 mg three times daily) in patients with a prior ischaemic stroke or transient ischaemic attack; combination treatment resulted in a 38% reduction in secondary stroke over placebo, which was substantially more than that in trials using aspirin alone [50]. However, this study did not show the relative contributions of aspirin alone or dipyridamole alone to the combination treatment results.
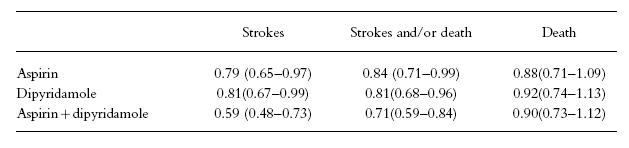
However, recent data have been more encouraging. The second European Stroke Prevention Study (ESPS-2) was a randomized, placebo-controlled, double-blind trial to investigate the role of aspirin (50 mg), modified-release dipyridamole (400 mg daily) and their combination in the secondary prevention of ischaemic stroke, thus addressing the deficiencies in ESPS-1 [51]. The odds ratios and 95% confidence intervals for the active treatment vs placebo on the principal endpoints of stroke, stroke or death, and death are summarized in Table 1. After 2 years’ follow up in over 6600 patients, there was a reduction of stroke risk compared with placebo, of 18% with aspirin alone (P = 0.013), 16% with dipyridamole alone (P = 0.015) and 37% with combination therapy (P<0.001) [51]. Risk of stroke or death was reduced by 13% with aspirin alone (P = 0.016), 15% with dipyridamole alone (P = 0.015) and 24% with combination therapy (P<0.001). However, there was no significant effect on death rate alone. There was a clear additive benefit in stroke reduction (36%) when aspirin and dipyridamole were used in combination, when compared with placebo; the combination being significantly more effective than either aspirin or dipyridamole prescribed singly [51].
Table 1.
The second European Stroke Prevention Study (ESPS-2): odds ratios and 95% confidence intervals for the active treatment versus placebo on the principal endpoints of stroke, stroke or death, and death (modified from reference 51).
Whilst preliminary data on the additive effect of dipyridamole to aspirin are promising, particularly with recent publication of ESPS-2, further work is still required to establish the precise role of dipyridamole in patients with cerebrovascular disease, particularly in the presence of carotid disease and in medical conditions that predispose to a high risk of stroke and thromboembolism, such as atrial fibrillation.
Deep venous thrombosis and pulmonary embolism
Antiplatelet therapy appears to reduce the risk of deep venous thrombosis and pulmonary embolism in a wide range of general and orthopaedic surgical patients [52]. Aspirin in combination with dipyridamole appears to be an effective therapy, although further research is needed to determine whether this combination is more effective than aspirin alone in preventing deep venous thrombosis. The addition of dipyridamole to aspirin, however, did not appear to bring about a further reduction in the incidence of pulmonary thromboembolism.
Pharmacological stress testing
Dipyridamole is as effective as dynamic exercise testing in the detection of coronary artery disease [53] and is particularly valuable in patients who are unable to perform an exercise test. The drug is normally administered by the intravenous route and is relatively safe, although it provokes chest pain in approximately 29% of patients and non-cardiac side effects in one third. In one large scale study of 3911 patients, for example, four (0.1%) patients suffered myocardial infarction within 24 h of dipyridamole infusion, although three of these had previous unstable angina [54].
Discussion
On review of the reported clinical trials, there is limited evidence that dipyridamole is generally an effective antithrombotic agent when used alone, nor is there convincing evidence that the combination of aspirin and dipyridamole is more effective than aspirin alone in the reduction of vascular events. However, a small increase in benefit from the combination cannot be excluded, particularly in patients with cerebrovascular disease. The lack of any statistically significant difference between various antiplatelet regimes (for example, aspirin-dipyridamole compared to aspirin alone) does not necessarily mean that these regimen are exactly equivalent. For example, the Antiplatelet Trialists’ Collaboration report that whilst the direct comparisons of aspirin plus dipyridamole versus aspirin alone indicates that dipyridamole may produce no worthwhile additional reduction in vascular events (316/2661 with aspirin plus dipyridamole, vs 312/2656 with aspirin alone), it does not prove this [10]. If there are real differences between one antiplatelet regimen and another, these differences are unlikely to be large; instead, large, direct randomized comparisons may be needed, such as ESPS-2 [51], to detect the moderate additional effects of aspirin-dipyridamole combination against dipyridamole alone or aspirin alone.
Although there is no consistent evidence to support the routine use of dipyridamole after coronary artery bypass grafting and in patients with occlusive peripheral vascular disease, these conditions remain common reasons for its use. However, dipyridamole is a useful agent in ‘pharmacological stress’ testing in nuclear cardiology imaging and may be valuable when combined with warfarin, in some patients with prosthetic valves. In addition, one recent study has suggested that when combined with aspirin [51], it may be of value (and additive in benefit) in the secondary prophylaxis of cerebrovascular disease. Whilst very encouraging, further studies are clearly needed.
Conclusion
In a significant proportion of cases, evidence-based medicine cannot support the current widespread continued prescription of dipyridamole in cardiological practice, but the jury is still out on cerebrovascular disease.
References
- 1.Picano E. Dipyridamole-echocardiography test: the historical background and the physiologic basis. Eur Heart J. 1989;10:365–376. doi: 10.1093/oxfordjournals.eurheartj.a059494. [DOI] [PubMed] [Google Scholar]
- 2.Metcalfe MJ, Lip GYH, Dunn FG. Dipyridamole. Lancet. 1992;339:1229. doi: 10.1016/0140-6736(92)91166-6. [DOI] [PubMed] [Google Scholar]
- 3.Stewart RB, Marks RG, Padgett PD, Hale WE. A longitudinal evaluation of dipyridamole drug use in an ambulatory elderly population. Chest. 1995;107:1049–1052. doi: 10.1378/chest.107.4.1049. [DOI] [PubMed] [Google Scholar]
- 4.Smith JB, Mills DCB. Inhibition of adenosine 3′5′—cyclic monophosphate phosphodiesterase. Biochem J. 1970;120 doi: 10.1042/bj1200020pa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moncada S, Korbut R. Dipyridamole and other phosphodiesterase inhibitors act as antithrombotic agents by potentiating endogenous prostacyclin. Lancet. 1978;i:1286–1289. doi: 10.1016/s0140-6736(78)91269-2. [DOI] [PubMed] [Google Scholar]
- 6.Newsholme EA. The control of the mechanism and the hormonal control of adenosine. Essays Biochem. 1978;14:82–123. [PubMed] [Google Scholar]
- 7.Harker LA, Slichter SJ. Studies of platelet and fibrinogen kinetics in patients with prosthetic heart valves. N Engl J Med. 1970;283:1302–1305. doi: 10.1056/NEJM197012102832402. [DOI] [PubMed] [Google Scholar]
- 8.Ritchie JL, Harker LA. Platelet and fibrinogen survival in coronary atherosclerosis. Response to medical and surgical therapy. Am J Cardiol. 1997;39:595–598. doi: 10.1016/s0002-9149(77)80171-9. [DOI] [PubMed] [Google Scholar]
- 9.Harker LA, Kadatz RA. Mechanism of action of dipyridamole. Thromb Res. 1983;(suppl 4):39. doi: 10.1016/0049-3848(83)90356-0. [DOI] [PubMed] [Google Scholar]
- 10.Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy-I. Prevention of death, myocardial infarction and stroke by prologed antiplatelet therapy in various categories of patients. Br Med J. 1994;308:81–106. [PMC free article] [PubMed] [Google Scholar]
- 11.The Persantine-Aspirin Reinfarction Study Research Group. Persantine and Aspirin in Coronary Heart Disease. Circulation. 1980;3:449–460. doi: 10.1161/01.cir.62.3.449. [DOI] [PubMed] [Google Scholar]
- 12.Klimt CR, Knatterud OL, Stamler J, Meier P. Persantine-Aspirin Reinfarction Study II. Secondary coronary prevention with Persantine and aspirin. J Am Coll Cardiol. 1986;7:251–269. doi: 10.1016/s0735-1097(86)80489-2. [DOI] [PubMed] [Google Scholar]
- 13.Sacks HS, Ancona-Berk VA, Berrier B, Nagalingam R, Chalmers TC. Dipyridamole in the treatment of angina pectoris: a meta-analysis. Clin Pharmacol Ther. 1988;43:610–615. doi: 10.1038/clpt.1988.84. [DOI] [PubMed] [Google Scholar]
- 14.Becker MC. Angina pectoris: a double-blind study with dipyridamole. J Newark Beth Israel Hospital. 1967;18:88–94. [Google Scholar]
- 15.Dewar HA, Horler AR. A clinical trial of Persantin and crodimyl in the treatment of angina of effort. Scot Med J. 1961;6:149–152. doi: 10.1177/003693306100600403. [DOI] [PubMed] [Google Scholar]
- 16.Foulds T, Mackinnon J. Controlled double-blind trial of ‘Persantin’ in treatment of angina pectoris. Br Med J. 1960;2:835. doi: 10.1136/bmj.2.5202.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Igloe MC. Treatment of angina pectoris with dipyridamole: a double-blind study. J Am Geriatric Soc. 1970;18:233–241. doi: 10.1111/j.1532-5415.1970.tb02124.x. [DOI] [PubMed] [Google Scholar]
- 18.Kinsella D, Troup W, McGregor M. Studies with a new coronary vasodilator durg: Persantin. Am Heart J. 1962;63:146–151. doi: 10.1016/0002-8703(62)90190-4. [DOI] [PubMed] [Google Scholar]
- 19.Leiberman A, Guglielmelli S. Persantin: a double-blind study. Angiology. 1964;15:290–292. doi: 10.1177/000331976401500608. [DOI] [PubMed] [Google Scholar]
- 20.Neumann M, Luisada AA. Effect of rapid and slow-acting ‘coronary’ drugs on precordial pain of the aged. Am J Med Sci. 1964;247:156–163. doi: 10.1097/00000441-196402000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Sbar S, Schiant RC. Dipyridamole in the treatment of angina pectoris. JAMA. 1967;201:865–867. [PubMed] [Google Scholar]
- 22.Wirecki M. Treatment of angina pectoris with dipyridamole: a long-term double-blind study. J Chronic Dis. 1967;20:139–145. doi: 10.1016/0021-9681(67)90048-3. [DOI] [PubMed] [Google Scholar]
- 23.Zion MM, Bradlow BA. A controlled clinical trial of ‘Persantin’ (RA8) in angina pectoris. South Afr Med J. 1961;35:11–13. [PubMed] [Google Scholar]
- 24.Teo KK, Yusuf S, Collins R, held PH, Peto R. Effects of intravenous magnesium in suspected actute myocardial infarction: an overview of randomised trials. Br Med J. 1991;303:1499–1503. doi: 10.1136/bmj.303.6816.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yusuf S, Collins R, MacMahon S, Peto R. Effect of intravenous nitrates on mortality in acute myocardial infarction: an overview of the randomised trials. Lancet. 1988;i:1088–1092. doi: 10.1016/s0140-6736(88)91906-x. [DOI] [PubMed] [Google Scholar]
- 26.ISIS-4 Collaborative Group. ISIS-4: A randomised factorial trial assessing early oral captopril, oral mononitrate and intravenous magnesium sulphate in 58 050 patients with susupected acute myocardial infarction. Lancet. 1995;345:669–685. [PubMed] [Google Scholar]
- 27.Gruppo per Italiano per lo Studio della Sopravivenza nell’Infarto Miocardico. GISSI-3: Effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Lancet. 1994;343:1115–1122. [PubMed] [Google Scholar]
- 28.Chesebro JH, Fuster V, Elveback LR, et al. Effect of dipyridamole and aspirin on late vein-graft patency after coronary bypass operations. N Engl J Med. 1984;310:209–214. doi: 10.1056/NEJM198401263100401. [DOI] [PubMed] [Google Scholar]
- 29.Sanz G. (GESIC Study) Does low dose aspirin prevent aorto-coronary vein bypass graft occlusion? Thromb Res. 1990;(suppl XII):11–21. doi: 10.1016/0049-3848(90)90435-f. [DOI] [PubMed] [Google Scholar]
- 30.Sanz G, Pajaron A, Alegria W, et al. Prevention of early aorto-coronary bypass occlusion by low dose aspirin and dipyridamole. Circulation. 1990;82:765–773. doi: 10.1161/01.cir.82.3.765. [DOI] [PubMed] [Google Scholar]
- 31.Goldman S, Copeland D, Moritz T, et al. Improvement in early saphenous vein graft patency after coronary artery bypass surgery with antiplatelet therapy; results of a Veterans Administration Co-operative Study. Circulation. 1988;77:1324–1332. doi: 10.1161/01.cir.77.6.1324. [DOI] [PubMed] [Google Scholar]
- 32.Pantely GA, Goodnight SH, Rahimtoola SH, et al. Failure of antiplatelet and anticoagulant therapy to improve patency of grafts after coronary artery bypass. N Engl J Med. 1979;301:962–966. doi: 10.1056/NEJM197911013011803. [DOI] [PubMed] [Google Scholar]
- 33.Brown BG, Cukingnan PA, DeRouen T, et al. Improved graft patency in patients treated with platelet- inhibiting therapy after coronary bypass surgery. Circulation. 1985;72:138–146. doi: 10.1161/01.cir.72.1.138. [DOI] [PubMed] [Google Scholar]
- 34.Lorenz RL, Weber M, Kotzur J, et al. Improved aorto-coronary bypass patency by low dose aspirin (100 mg daily): Effects on platelet aggregation and thromboxane formation. Lancet. 1984;i:1261–1264. doi: 10.1016/s0140-6736(84)92446-2. [DOI] [PubMed] [Google Scholar]
- 35.Schwartz L, Bourassa MG, Lesperance J, et al. Aspirin and dipyridamole in the prevention of restenosis after percutaneous transluminal coronary angioplasty. N Engl J Med. 1988;318:1714–1719. doi: 10.1056/NEJM198806303182603. [DOI] [PubMed] [Google Scholar]
- 36.Lembo NJ, Black AJ, Roubin GS, et al. Effect of pretreatment with aspirin versus aspirin plus dipyridamole on frequency and type of acute complications of percutaneous transluminal coronary angioplasty. Am J Cardiol. 1990;65:422–426. doi: 10.1016/0002-9149(90)90804-a. [DOI] [PubMed] [Google Scholar]
- 37.Danchin N, Juilliere Y, Kettani C, Buffet P, Anconina J, Cuilliere M, Cherrier F. Effect on early acute occlusion rate of adjunctive antithrombotic treatment with intravenously administered dipyridamole during percutaneous transluminal coronary angioplasty. Am Heart J. 1994;127:494–498. doi: 10.1016/0002-8703(94)90655-6. [DOI] [PubMed] [Google Scholar]
- 38.Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy-II: Maintenance of vascular graft or arterial patency by antiplatelet therapy. Br Med J. 1994;308:159–168. [PMC free article] [PubMed] [Google Scholar]
- 39.Hess H, Mietashk A, Deichsel G. Drug-induced inhibition of platelet function delays progression of peripheral occlusive arterial disease. Lancet. 1985;i:415–419. doi: 10.1016/s0140-6736(85)91144-4. [DOI] [PubMed] [Google Scholar]
- 40.Kohler TR, Kaufman JL, Kacoyanis G, et al. Effect of aspirin and dipyridamole on the patency of lower extremity bypass grafts. Surgery. 1984;96:462–466. [PubMed] [Google Scholar]
- 41.Sullivan JM, Harken DE, Gorlin A. Pharmacologic control of thromboembolic complications of cardiac-valve replacement. N Engl J Med. 1971;284:1391–1394. doi: 10.1056/NEJM197106242842501. [DOI] [PubMed] [Google Scholar]
- 42.Oates JA, Wood AJJ. Dipyridamole. N Engl J Med. 1987;316:1247–1257. doi: 10.1056/NEJM198705143162005. [DOI] [PubMed] [Google Scholar]
- 43.Harker LA, Slichter SJ. Platelet and fibrinogen consumption in man. N Engl J Med. 1972;287:999–1005. doi: 10.1056/NEJM197211162872001. [DOI] [PubMed] [Google Scholar]
- 44.Brott WH, Zajtchuk R, Bowen TE, Davia J, Green DC. Dipyridamole-aspirin as thromboembolic prophylaxis in patients with aortic valve prostheses: prospective study with the model 2320 Starr-Edwards prosthesis. J Thorac Cardiovasc Surg. 1981;81:632–635. [PubMed] [Google Scholar]
- 45.Hirsh J, Fuster V, Salzman E. Dose of antiplatelet agents: the relationship among side effects and antithrombotic effectiveness. Arch Intern Med. 1986;146:465–466. doi: 10.1378/chest.89.2_supplement.4s. [DOI] [PubMed] [Google Scholar]
- 46.Stein PD, Collins JJ, Kantrowitz A. Antithrombotic therapy in mechanical and biological prosthetic heart valves and saphenous vein bypass grafts. Arch Intern Med. 1986;146:468–469. doi: 10.1378/chest.89.2_supplement.46s. [DOI] [PubMed] [Google Scholar]
- 47.Bousser MG, Eschwege E, Haguenau M, et al. ‘AICLA’ controlled trial of aspirin and dipyridamole in the secondary prevention of athero-thrombotic cerebral ischaemia. Stroke. 1983;14:5–14. doi: 10.1161/01.str.14.1.5. [DOI] [PubMed] [Google Scholar]
- 48.American-Canadian Co-Operative Study Group. Persantine aspirin trial in cerebral ischaemia. Part II. Endpoint results. Stroke. 1985;16:406–415. doi: 10.1161/01.str.16.3.406. [DOI] [PubMed] [Google Scholar]
- 49.Acheson J, Danta G, Hutchinson EC. Controlled trial of dipyridamole in cerebral vascular disease. Br J Med. 1969;I:614–615. doi: 10.1136/bmj.1.5644.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.ESPS Group. The European Stroke Prevention Study: Principal Endpoints. Lancet. 1987;ii:1351–1354. [PubMed] [Google Scholar]
- 51.Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996;143:1–13. doi: 10.1016/s0022-510x(96)00308-5. [DOI] [PubMed] [Google Scholar]
- 52.Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy-III: Reduction in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients. Br Med J. 1994;308:235–246. [PMC free article] [PubMed] [Google Scholar]
- 53.Ranhosky A, Rawson J. The safety of intravenous dipyridamole thallium myocardial perfusion imaging. Circulation. 1990;81:1205. doi: 10.1161/01.cir.81.4.1205. [DOI] [PubMed] [Google Scholar]
- 54.Varma SK, Watson DD, Beller GA. Quantitative comparison of thallium-201 scintigraphy after exercise and dipyridamole in coronary artery disease. Am J Cardiol. 1989;64:871. doi: 10.1016/0002-9149(89)90834-5. [DOI] [PubMed] [Google Scholar]


