Abstract
Primate lentiviruses are thought to use the chemokine receptor CCR5 as the major coreceptor for entry into cells. Here we show that some variants of simian immunodeficiency virus (SIV) replicate efficiently in peripheral blood mononuclear cells (PBMCs) lacking a functional CCR5. There were differences in the replication patterns of sequential variants that evolved during SIVMne infection; the late-stage pathogenic variants were unable to replicate in PBMCs lacking CCR5, whereas the early- and intermediate-stage viruses replicated as well in PBMCs lacking CCR5 as they did in cells with wild-type CCR5. The coreceptor specificities of these sequential variants were compared using indicator cell lines expressing known SIV coreceptors. Among the known SIV coreceptors, there were none that were functional for the early and intermediate variants but not the late-stage variants, suggesting that the coreceptor used for replication in PBMCs may be a coreceptor that has not yet been described. Because some variants replicate with high efficiency in peripheral blood cells using this as yet uncharacterized cellular receptor, this coreceptor may be important for viral entry of some target cell populations in the host.
The entry of primate lentiviruses into cells involves a series of interactions with host cell receptors, starting with binding of the viral envelope to the CD4 protein; this leads to a conformational change that allows binding of the envelope protein to a second receptor. This coreceptor can be one of a variety of seven transmembrane-spanning G-protein-coupled chemokine receptors. The chemokine receptor CCR5 is used by most isolates of human immunodeficiency virus type 1 (HIV-1) and is thought to be the coreceptor that is expressed on cells that are the earliest targets for virus replication after transmission. Some later-stage isolates of HIV-1 use CXCR4 as a coreceptor, and many of these variants also retain the ability to use CCR5 as a coreceptor, perhaps allowing some flexibility for later-stage viruses to infect a wider range of target cells. A minority of HIV-1 variants can use other G-protein-coupled receptors for entry, although the efficiency of infection is reduced relative to that for CCR5-mediated entry, and the importance of these alternate coreceptors in infection is unclear (reviewed in references 1, 11, and 18).
Simian immunodeficiency virus (SIV) also uses CCR5 as a coreceptor (3, 4, 17). In addition, several other cellular receptors can function as coreceptors for SIV, including GPR1, GPR15, CCR8, APJ, STRL33, and CHEMR23 (5, 6, 9, 20, 22; G. Alkhatib, F. Liao, E. A. Berger, J. M. Farber, and K. W. C. Peden, Letter, Nature 388:238, 1997). Many pathogenic SIVs can efficiently infect cells by using both CCR5 and GPR15 as a coreceptor with CD4 (6, 8, 9, 12). However, studies of SIV infection of macaques suggest that GPR15 may not be important for virus replication in vivo because mutations that abolish GPR15-mediated entry of SIVmac239 did not affect the levels of virus in the infected animal (19). In general, it remains unclear if coreceptors other than CCR5 play a major role in SIV or HIV replication at any stage of infection and disease in the host.
Previous studies of SIV infection of Macaca nemestrina demonstrated that the late-stage variants are more pathogenic than the cloned infecting virus, SIVMneCL8, from which they arose in the host (13). Viruses that evolved at intermediate (35-week-postinfection) and late (170-week-postinfection) stages in animals infected with SIVMneCL8 replicated 100- and 3,000-fold better, respectively, than the parental viral clone when transmitted to naïve monkeys (13). Some of the increased replication was attributable to the inability of these intermediate- and late-stage viruses to elicit neutralizing antibody responses. However, because neither the intermediate nor the late viruses could elicit detectable neutralizing antibodies, the ∼30-fold-higher replication of the two viruses may reflect an additional selective advantage of the late-stage variant (13). In our initial studies of the coreceptor specificities of these different SIVMne variants, we found no differences in the coreceptor preferences of these viruses; all of the SIVMne variants tested were able to infect cells in culture by using either CCR5 or GPR15, but not CXCR4 (12). To examine if coreceptors other than CCR5 were important for replication of these variants in relevant cell types such as T lymphocytes and macrophages, we examined the ability of the viruses to infect human peripheral blood mononuclear cells (PBMCs) from donors who were homozygous for a 32-bp deletion of CCR5 (Δ32 PBMCs). The viruses examined were chimeric viruses encoding envelope surface unit proteins that were obtained from intermediate [35-week-postinfection; SIVMneCL8(35wkSU)] and late [170-week-postinfection; SIVMneCL8(170wkSU)] stages of infection in animals inoculated with SIVMneCL8 (14). Thus, the only difference between viruses was in the envelope surface protein.
Blood samples from four HIV-1-seronegative donors, two with a wild-type CCR5 allele (35-9 and 53-5) and two with the homozygous Δ32 allele (07-5 and 43-1), were provided without indication of the CCR5 status. PBMCs were isolated from whole blood by Ficoll-Hypaque centrifugation and cultured by methods similar to those described previously (21). SIV particles were made by transfecting 293T cells with the proviral clones and then passaging cell-free virus harvested 2 days later for 1 to 2 weeks in CEMx174 cells. The infectious titer was determined using sMAGI cells (2). SIVmac239 and the SIV/HIV-1 chimera SHIV162 were also generated in CEMx174 cells; in the case of SHIV162, the virus titer was determined using MAGI-CCR5 cells (3). Phytohemagglutinin (PHA)-stimulated PBMCs were infected with each virus at a multiplicity of infection of 0.01. Every 2 to 3 days, medium was replaced, and the level of virus replication was assessed by assaying the filtered supernatant for SIV p27gag.
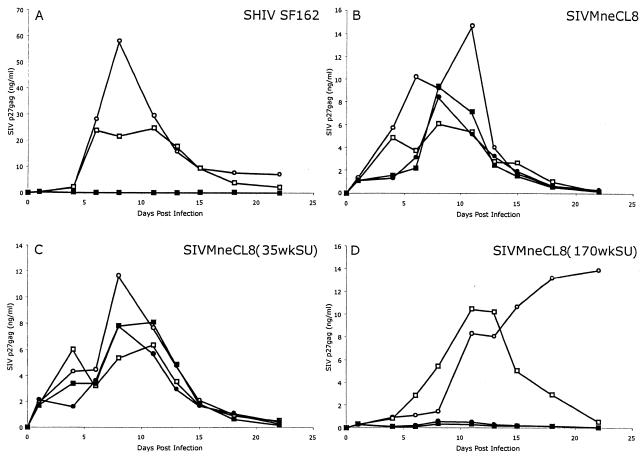
The results of the first infection study are shown in Fig. 1, and they represent the averages of results from duplicate infections. SHIV162 was used as a control for these experiments because it is dependent on CCR5 for entry (8, 10) and thus would not be expected to replicate in PBMCs lacking a functional CCR5 protein. As expected, SHIV162 replicated to high levels in the PBMCs from two donors and not in the PBMCs from two others. Upon unblinding of the experiment, the donors were shown to have the expected CCR5 genotype. SHIV162 replicated to high levels in PBMCs from each of the wild-type CCR5 donors, with peak levels of p27gag production of ∼19 to 58 ng/ml (Fig. 1A; Table 1). Somewhat lower peak levels of replication (∼6 to 15 ng/ml) were observed for each of the SIVs tested in PBMCs from the two donors with a wild-type CCR5 allele. In PBMCs from donors with a deletion in CCR5, the infection profile of SIVMne170SU followed a similar pattern as that observed with the CCR5-dependent SHIV162 control virus; there was a low level of virus replication (peak of ≤0.6 ng of p27gag/ml) of the chimera carrying the envelope gene from late-stage infection. Surprisingly, the parental, early-stage SIVMne clone, SIVMneCL8, replicated to high levels in the cells lacking CCR5. Similarly, the virus carrying the prototype envelope gene from intermediate stages of infection also replicated in PBMCs lacking CCR5. In both cases, the replication kinetics of these early- and/or intermediate-stage viruses were very similar in PBMCs from wild-type and Δ32 CCR5 donors (Fig. 1).
FIG. 1.
Levels of virus production, as measured by p27gag antigen capture assay, in PBMCs infected with SIV and SHIV. For these experiments, PBMCs were isolated from the whole blood of four HIV-1-seronegative donors, two with wild-type CCR5 (○, 53-3; □, 35-9) and two with CCR5 with a 32-bp-deletion (•, 43-1; ▪, 07-5). After Ficoll-Hypaque centrifugation, the cells were cultured with 1 μg of PHA/ml in RPMI 1640 supplemented with 10% fetal bovine serum (RPMI complete) and 10 U of human recombinant interleukin-2/ml for 3 days. The cells were pelleted by centrifugation at 300 × g, washed with RPMI complete to remove the PHA, and cultured for an additional 24 h in RPMI complete with interleukin-2. Duplicate cultures of 2 × 106 cells/ml were infected with each virus at a multiplicity of infection of 0.01 in 1 ml of RPMI complete plus 10 U of interleukin-2/ml. The infectious titers of the viruses were determined by sMAGI assay (2) for SIV or MAGI-CCR5 assay (3) for SHIV162 (16). Fourteen hours later, the cells were pelleted at 300 × g, washed three times with RPMI complete to remove any residual cell-free virions, and resuspended in 5 ml of RPMI complete plus interleukin-2 (10 U/ml). Every 2 to 3 days, 2 ml of cell-free supernatant was removed and replaced with fresh RPMI complete supplemented with 10 U of interleukin-2/ml. Cell-free supernatant that was collected was stored at −80°C and used to monitor viral replication by assaying for p27gag antigen with an enzyme-linked immunosorbent assay kit (Coulter).
TABLE 1.
Peak p27gag levels in PBMCs infected with different SIVs and SHIV
| Virus | Peak p27gag level (ng/ml) (day of peak virus) for CCR5, expt, and donora
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Wild-type CCR5
|
Δ32 CCR5
|
|||||||
| Expt 1
|
Expt 2
|
Expt 1
|
Expt 2
|
|||||
| 35-9 | 53-5 | 35-9 | 53-5 | 07-5 | 43-1 | 07-5 | 43-1 | |
| SHIV162 | 24.6 (11) | 58.2 (8) | 21.5 (12) | 19.0 (14) | 0.4 (1) | 0.3 (1) | 0.4 (14) | 0.4 (17) |
| SIVMneCL8 | 6.0 (8) | 14.7 (11) | 11.1 (12) | 9.2 (14) | 9.3 (8) | 8.4 (8) | 3.7 (14) | 12.9 (14) |
| SIV35wkSU | 6.4 (11) | 11.7 (8) | 15.0 (12) | 10.1 (12) | 8.1 (11) | 7.8 (8) | 3.0 (12) | 2.5 (17) |
| SIV170wkSU | 10.5 (11) | 13.9 (22) | 5.9 (17) | 7.6 (14) | 0.3 (8) | 0.6 (8) | 0.5 (14) | 0.4 (14) |
| SIV170 | NT | NT | 9.6 (12) | 14.4 (12) | NT | NT | 1.1 (14) | 0.1 (5) |
| SIVmac239 | NT | NT | 11.9 (12) | 12.9 (14) | NT | NT | 3.5 (12) | 2.5 (12) |
Experiment 1 was monitored through 22 days, with peak virus production typically observed at 8 or 11 days. Experiment 2 was monitored through day 17, with peak virus production typically observed at 12 or 14 days. NT, not tested.
The infection experiments were repeated on a second occasion, and similar results were obtained. Table 1 shows the peak viral levels observed in both infection experiments in which we used PBMCs from the same four donors, two with wild-type CCR5 and two with Δ32 CCR5. In summary, the control virus SHIV162 replicated to ∼100-fold-higher peak levels in each of the four experiments with PBMCs carrying a wild-type CCR5 gene than in experiments with PBMCs carrying Δ32 CCR5. A similar difference (10- to 100-fold) between peak levels of p27gag in Δ32 PBMCs and those in wild-type PBMCs was observed for both the full-length proviral clone from 170 weeks postinfection, SIVMne170, and the chimera encoding the envelope from this provirus, SIVMneCL8(170wkSU). In contrast, both SIVMneCL8 and SIVMneCL8(35wkSU) replicated to similar levels in PBMCs from wild-type and Δ32 CCR5 donors (approximately one- to threefold differences in peak viral levels). In the second experiment, SIVmac239 was also examined because previous studies have shown that this virus can replicate in PBMCs lacking CCR5 from some donors but not others (4, 24). Replication of SIVmac239 was only three- to fourfold lower in Δ32 CCR5 PBMCs; the replication pattern was very similar to that of the intermediate-stage SIVMne variant in the second experiment, where it was tested in parallel (Table 1). Thus, the major novel finding is that the early- and intermediate-stage SIVMne variants can replicate in PBMCs in the absence of CCR5, whereas late-stage SIVMne variants are much more CCR5 dependent.
To determine whether the coreceptor that is used by early- and intermediate-stage SIVMne variants is among those that have been described, we examined the ability of the viral variants to infect a set of HOS-CD4+ (GHOST) cell lines that express various coreceptors known to support infection by different strains of SIV. It was previously shown that all SIVMne variants use CCR5 and GPR15 for entry into target cells (12). None of the SIVMne variants was able to use STRL33 (now called CXCR6) or CXCR4 as a coreceptor for entry, at least at the levels expressed on GHOST cells that permit HIV-1 infection (12). To examine other potential coreceptors, we infected a panel of GHOST4 cells expressing the following coreceptors: CCR8, GPR1, APJ, and CHEMR23. We compared infection of these cells with infection of GHOST cells expressing CCR5 (12) (GHOST cells expressing CCR8, GPR1, and CCR5 were kindly provided by Dan Littman). In the case of APJ and CHEMR23, the cells were constructed by transducing the parental indicator cells (GHOST4), which are HOS cells modified to stably express the human CD4 gene and humanized green fluorescent protein (GFP) under the control of the HIV-2 long terminal repeat, with retroviral particles carrying a pBabe-puromycin vector containing the coreceptor gene of interest (APJ or CHEMR23). The results of infection of GHOST cells expressing various coreceptors with the different SIVMne variants and relevant control viruses are shown in Table 2. As expected, all viruses tested were able to use CCR5. However, neither the early-stage variant SIVMneCL8 nor the intermediate-stage variant SIVMneCL8(35wkSU) was able to use any of these additional coreceptors. The late-stage variant SIVMneCL8(170wkSU) was able to use CCR8 and GPR1 in addition to CCR5 and GPR15, although the efficiency of alternative coreceptor usage was reduced compared to CCR5 usage.
TABLE 2.
Infection of GHOST4 indicator cells with variants of SIVMnea
| Virus | Coreceptor expressed
|
||||
|---|---|---|---|---|---|
| CCR5 | CCR8 | GPR1 | APJ | CHEMR23 | |
| Mock | − | − | − | − | − |
| SIVMneCL8 | +++ | − | − | − | − |
| 35wkSU | +++ | − | − | − | − |
| 170wkSU | +++ | ++ | ++ | +/− | +/− |
| SIVmac239/316b | +++ | +++ | +++ | +++ | +++ |
Cells were infected at a multiplicity of infection of 0.1 or 1, and the number of GFP-positive cells was visually inspected in relation to the number of GFP-positive cells observed when the same virus dose was used to infect GHOST-CCR5 cells (defined as +++). Thus, the designation of ++ is somewhat arbitrary, indicating only that the number of GFP-positive cells was reduced versus that for GHOST-CCR5 cells. A result of +/− indicates that, in one of the four experiments that were performed, the infected culture could not be distinguished from the negative control.
One of two SIVmac clones was used as a positive control as appropriate for the indicated coreceptor.
Summary and conclusions.
The results of these studies suggest that some SIV variants can replicate to high levels in PBMCs lacking CCR5. To our surprise, this was true for early- and intermediate-stage variants but not for later-stage variants that evolved from them. This result was unexpected because the late-stage virus SIVMne170 replicated to much higher levels in the animal, as judged by both plasma and lymph node viral RNA levels, and the late-stage virus was more pathogenic (13). This suggests that the alternative coreceptor used by early-stage viruses may not be important for high levels of virus replication per se. Thus, entry with the use of this coreceptor, if relevant in vivo, may be for a select subset of targets, perhaps cells important early in infection and/or with viruses that cause a more prolonged disease course. Additional studies with sequential viruses from monkeys infected with other SIV or simian/human immunodeficiency virus (SHIV) strains may provide insights as to whether there is a relationship between CCR5-independent replication and stage of infection for primate lentiviruses. One might assume that the opposite is the case for HIV-1 infection in humans, because in some individuals, the late-stage HIV-1 variants acquire the ability to use the CXCR4 coreceptor to infect PBMCs. However, there is no evidence that well-characterized sequential variants from the same source have been tested for replication in PBMCs that lack CCR5.
Both GPR15 and STRL33 are expressed on activated PBMCs (6-9, 15). However, there was not a correlation between the use of these coreceptors and the ability of the SIV variant tested to replicate in PBMCs lacking CCR5. The coreceptors tested were of human origin, so species-specific differences in the GHOST cell and the PBMC experiments cannot account for the findings. None of the SIVMne variants efficiently infect GHOST cells expressing STRL33, whereas GPR15 is used by all of the SIVs tested, including the late-stage variants (12); thus, infection via one of these coreceptors would not appear to explain the observed differences in replication of the SIV variants in Δ32 PBMCs. However, we cannot completely rule out that the differences we observed between viruses reflect a difference between their abilities to use a given coreceptor when expressed on PBMCs and those when expressed on GHOST cells. This could occur if PBMCs express much higher levels of the coreceptor in question than do the GHOST cell lines, because it has been noted that, for some coreceptors such as STRL33, the levels of expression have a major impact on viral replication (23). Thus, we cannot rule out that early- and late-stage variants differ in their abilities to infect PBMCs via STRL33. Coreceptor-independent entry is not a likely explanation for these findings because these SIVs are dependent on a coreceptor for entry; SIVMneCL8 did not infect HeLa cells expressing CD4 alone, but it could infect HeLa cells expressing CD4 and CCR5 (3).
In GHOST cells, we did observe low-level infection of the late-stage variants with various alternative coreceptors such as CCR8 and GPR1, suggesting that the late-stage viruses may have more flexibility in the coreceptors that they use for entry. However, we found no evidence that a known SIV coreceptor can be used for entry by the early- and intermediate-stage SIVMne variants, but not the late-stage variant. There were no coreceptors that distinguished SIVmac239 from the early- and/or intermediate-stage SIVMne variants, and previous results (4, 24), which were confirmed here, indicate that SIVmac239 can infect PBMCs from some donors lacking CCR5. The earlier studies by Zhang et al. (24), which included studies with inhibitor molecules that block CCR5 entry, suggested that a coreceptor other than CCR5 may be used by SIVmac239 for replication in PBMCs, although the specific coreceptor could not be identified (24). Our studies indicate that the same is true for some variants of SIVMne. Collectively, these studies suggest that the coreceptor that facilitates high-level replication of some SIVs in PBMCs lacking CCR5 may be a protein that has not yet been identified as a coreceptor for primate lentiviruses. Because this coreceptor permits entry in peripheral blood cells, this suggests that the as yet unidentified coreceptor may be important for replication in relevant cell types.
Acknowledgments
We thank Jason Kimata for helpful discussion and comments on the manuscript; Connie Celum and her team for providing PBMCs from CCR5-deletion donors; Dan Littman for providing GHOST cells; Dan Littman, Joe Sodroski, and Bob Doms for providing coreceptor clones; Cecelia Cheng-Mayer for providing SHIV162; and Ron Desrosiers for providing SIVmac239. The CEMx174 cell line was obtained from the AIDS Research and Reference Reagent Program.
This work was supported by NIH grant RO1 AI34251. S.F. and M.-E.H. were supported in part by NIH training grant T32 CA09229. M.J.P. was supported in part by a Poncin Fellowship.
REFERENCES
- 1.Berger, E. A., P. M. Murphy, and J. M. Farber. 1999. Chemokine receptors as HIV-1 coreceptors: roles in viral entry, tropism, and disease. Annu. Rev. Immunol. 17:657-700. [DOI] [PubMed] [Google Scholar]
- 2.Chackerian, B., N. L. Haigwood, and J. Overbaugh. 1995. Characterization of a CD4-expressing macaque cell line that can detect virus after a single replication cycle and can be infected by diverse simian immunodeficiency virus isolates. Virology 213:386-394. [DOI] [PubMed] [Google Scholar]
- 3.Chackerian, B., E. M. Long, P. A. Luciw, and J. Overbaugh. 1997. Human immunodeficiency virus type 1 coreceptors participate in postentry stages in the virus replication cycle and function in simian immunodeficiency virus infection. J. Virol. 71:3932-3939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen, Z., P. Zhou, D. D. Ho, N. T. Landau, and P. A. Marx. 1997. Genetically divergent strains of simian immunodeficiency virus use CCR5 as a coreceptor for entry. J. Virol. 71:2705-2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choe, H., M. Farzan, M. Konkel, K. Martin, Y. Sun, L. Marcon, M. Cayabyab, M. Berman, M. E. Dorf, N. Gerard, C. Gerard, and J. Sodroski. 1998. The orphan seven-transmembrane receptor Apj supports the entry of primary T-cell-line-tropic and dualtropic human immunodeficiency virus type 1. J. Virol. 72:6113-6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deng, H. K., D. Unutmaz, V. N. KewalRamani, and D. R. Littman. 1997. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature 388:296-300. [DOI] [PubMed] [Google Scholar]
- 7.Edinger, A. L., A. Amedee, K. Miller, B. J. Doranz, M. Endres, M. Sharron, M. Samson, Z. H. Lu, J. E. Clements, M. Murphey-Corb, S. C. Peiper, M. Parmentier, C. C. Broder, and R. W. Doms. 1997. Differential utilization of CCR5 by macrophage and T cell tropic simian immunodeficiency virus strains. Proc. Natl. Acad. Sci. USA 94:4005-4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edinger, A. L., T. L. Hoffman, M. Sharron, B. Lee, B. O'Dowd, and R. W. Doms. 1998. Use of GPR1, GPR15 and STRL33 as coreceptors by diverse human immunodeficiency virus type 1 and simian immunodeficiency virus envelope proteins. Virology 249:367-378. [DOI] [PubMed] [Google Scholar]
- 9.Farzan, M., H. Choe, K. Martin, L. Marcon, W. Hofmann, G. Karlsson, Y. Sun, P. Barrett, N. Marchand, N. Sullivan, N. Gerard, C. Gerard, and J. Sodroski. 1997. Two orphan seven-transmembrane segment receptors which are expressed in CD4-positive cells support simian immunodeficiency virus infection. J. Exp. Med. 186:405-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harouse, J. M., A. Gettie, R. C. Tan, J. Blanchard, and C. Cheng-Mayer. 1999. Distinct pathogenic sequela in rhesus macaques infected with CCR5 or CXCR4 utilizing SHIVs. Science 284:816-819. [DOI] [PubMed] [Google Scholar]
- 11.Hoffman, T. L., and R. W. Doms. 1998. Chemokines and coreceptors in HIV/SIV-host interactions. AIDS 12:S17-S26. [PubMed] [Google Scholar]
- 12.Kimata, J. T., J. J. Gosink, V. N. KewalRamani, L. M. Rudensey, D. R. Littman, and J. Overbaugh. 1999. Coreceptor specificity of temporal variants of simian immunodeficiency virus Mne. J. Virol. 73:1655-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kimata, J. T., L. Kuller, D. B. Anderson, P. Dailey, and J. Overbaugh. 1999. Emerging cytopathic and antigenic simian immunodeficiency virus variants influence AIDS progression. Nat. Med. 5:535-541. [DOI] [PubMed] [Google Scholar]
- 14.Kimata, J. T., and J. Overbaugh. 1997. The cytopathicity of a simian immunodeficiency virus Mne variant is determined by mutations in Gag and Env. J. Virol. 71:7629-7639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liao, F., G. Alkhatib, K. W. Peden, G. Sharma, E. A. Berger, and J. M. Farber. 1997. STRL33, a novel chemokine receptor-like protein, functions as a fusion cofactor for both macrophage-tropic and T cell line-tropic HIV-1. J. Exp. Med. 185:2015-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luciw, P. A., E. Pratt-Lowe, K. E. S. Shaw, J. A. Levy, and C. Cheng-Mayer. 1995. Persistent infection of rhesus macaque with T-cell-line-tropic and macrophage-tropic clones of simian/human immunodeficiency viruses (SHIV). Proc. Natl. Acad. Sci. USA 92:7490-7494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marcon, L., H. Choe, K. A. Martin, M. Farzan, P. D. Ponath, L. Wu, W. Newman, N. Gerard, C. Gerard, and J. Sodroski. 1997. Utilization of C-C chemokine receptor 5 by the envelope glycoproteins of a pathogenic simian immunodeficiency virus, SIVmac239. J. Virol. 71:2522-2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Overbaugh, J., A. D. Miller, and M. V. Eiden. 2001. Receptors and entry cofactors for retroviruses include single and multiple transmembrane-spanning proteins as well as newly described glycophosphatidylinositol-anchored and secreted proteins. Microbiol. Mol. Biol. Rev. 65:371-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pohlmann, S., N. Stolte, J. Munch, P. Ten Haaft, J. L. Heeney, C. Stahl-Hennig, and F. Kirchhoff. 1999. Co-receptor usage of BOB/GPR15 in addition to CCR5 has no significant effect on replication of simian immunodeficiency virus in vivo. J. Infect. Dis. 180:1494-1502. [DOI] [PubMed] [Google Scholar]
- 20.Rucker, J., A. Edinger, M. Sharron, M. Samson, B. Lee, J. Berson, Y. Yi, B. Margulies, R. Collman, B. Doranz, M. Parmentier, and R. Doms. 1997. Utilization of chemokine receptors, orphan receptors, and herpesvirus-encoded receptors by diverse human and simian immunodeficiency viruses. J. Virol. 71:8999-9007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rudensey, L. M., J. T. Kimata, R. E. Benveniste, and J. Overbaugh. 1995. Progression to AIDS in macaques is associated with changes in the replication, tropism, and cytopathic properties of the simian immunodeficiency virus variant population. Virology 207:528-542. [DOI] [PubMed] [Google Scholar]
- 22.Samson, M., A. L. Edinger, P. Stordeur, J. Rucker, V. Verhasselt, M. Sharron, C. Govaerts, C. Mollereau, G. Vassart, R. W. Doms, and M. Parmentier. 1998. ChemR23, a putative chemoattractant receptor, is expressed in monocyte-derived dendritic cells and macrophages and is a coreceptor for SIV and some primary HIV-1 strains. Eur. J. Immunol. 28:1689-1700. [DOI] [PubMed] [Google Scholar]
- 23.Sharron, M., S. Pohlmann, K. Price, E. Lolis, M. Tsang, F. Kirchoff, R. W. Doms, and B. Lee. 2000. Expression and coreceptor activity of STRL33/bonzo on primary peripheral blood lymphocytes. Blood 96:41-49. [PubMed] [Google Scholar]
- 24.Zhang, Y., B. Lou, R. B. Lal, A. Gettie, P. A. Marx, and J. P. Moore. 2000. Use of inhibitors to evaluate coreceptor usage by simian and simian/human immunodeficiency viruses and human immunodeficiency virus type 2 in primary cells. J. Virol. 74:6893-6910. [DOI] [PMC free article] [PubMed] [Google Scholar]