Abstract
Objectives. We tested the efficacy of brief HIV/sexually transmitted disease (STD) risk-reduction interventions for African American women in primary care settings.
Methods. In a randomized controlled trial, 564 African American women recruited at a Newark, NJ, inner-city women’s health clinic were assigned to a 20-minute one-on-one HIV/STD behavioral skill-building intervention, 200-minute group HIV/STD behavioral skill-building intervention, 20-minute one-on-one HIV/STD information intervention, 200-minute group HIV/STD information intervention, or 200-minute health intervention control group. Primary outcomes were self-reported sexual behaviors in the previous 3 months; secondary outcome was STD incidence.
Results. At 12-month follow-up, participants in the skill-building interventions reported less unprotected sexual intercourse than did participants in the information interventions (Cohen’s d [d]=0.23, P=.02), reported a greater proportion of protected sexual intercourse than did information intervention participants (d=0.21, P=.05) and control participants (d=0.24, P=.03), and were less likely to test positive for an STD than were control participants (d=0.20, P=.03).
Conclusions. This study suggests that brief single-session, one-on-one or group skill-building interventions may reduce HIV/STD risk behaviors and STD morbidity among inner-city African American women in primary care settings.
There is growing concern about morbidity and mortality associated with sexually transmitted diseases (STDs) among African American women. Although STDs are widespread across racial and ethnic groups in the United States, reported rates of chlamydia are 10 times higher, and reported rates of gonorrhea and syphilis 25 times higher, among African Americans than among Whites.1,2 African American women are also disproportionately affected by HIV/AIDS, which is commonly transmitted through sexual behavior. Although only 12% of women in the United States are African Americans, 67% of US women diagnosed with AIDS in 2004 were African Americans,3 and AIDS is the leading cause of death among African American women aged 25 to 34 years.4
Interventions are needed in a variety of venues to comprehensively address African American women’s risk of STDs, including HIV. One important venue for such interventions is the primary health care setting. Nurses and other health care providers may be especially effective agents of behavior change. Because health care providers are generally unable to devote a great deal of time to primary prevention, brief single-session interventions may be especially practical in primary health care settings. Unfortunately, there is a paucity of evidence on the efficacy of such interventions.
Although there is considerable evidence of the efficacy of behavioral interventions in reducing self-reported HIV/STD sexual-risk behavior,5 few trials have demonstrated significant reductions in the rate of biologically confirmed STDs among women,6–8 and none have examined brief single-session interventions implemented by health care providers with African American women in a primary care setting. Moreover, in some of these studies,6,7 participants were selected on the basis of recent STD or HIV test results. Whether the findings of these trials would generalize to a less restricted population of African American women is unclear.
There is a growing consensus that merely providing information is not enough to induce sexual behavior change and that it is also necessary to instill behavioral skills, including condom use and condom-use negotiation skills. Both one-on-one counseling9 and small-group interventions6,9 are appropriate in primary care settings. Small-group interventions can allow participants to learn from each other, whereas one-on-one interventions can be shorter and more tailored to the individual.
Our randomized controlled trial was designed to identify effective single-session HIV/STD risk-reduction interventions for inner-city African American women that can be implemented by nurses and other health care providers in clinics and other primary care facilities. We tested 4 culture-sensitive, HIV/STD risk-reduction interventions involving 2 kinds of intervention content—information versus behavioral skills—and 2 methods of intervention delivery—group versus individual.
We randomly assigned African American women from an inner-city women’s health clinic to 1 of these 4 HIV/STD risk-reduction interventions or a general health-promotion intervention, which served as the control group. We hypothesized that the skill-building interventions would reduce self-reported sexual-risk behavior and the rate of STDs compared with the control group or information interventions. In addition, we tested whether the skill-building group intervention was more effective than the skill-building one-on-one intervention.
METHODS
Participants
The participants in this study, called “Sister-to-Sister: The Black Women’s Health Project,” were 564 African American women (mean age = 27.2 years) seeking care at the outpatient women’s health clinic of a large hospital in Newark, NJ. The participants were told that the study was designed to empower women to reduce their risk of developing devastating health problems, including cardiovascular diseases, cancer, and AIDS. The women were recruited during their initial or semiannual appointment. Women were offered a total of $130 for participating: $25 immediately after the intervention and $30, $35, and $40 for the 3-, 6-, and 12-month follow-ups, respectively.
Procedures
Sexually experienced African American women aged 18 to 45 years who were not pregnant were eligible to participate. The study was conducted between March 1993 and November 1996. The women were stratified by age and randomly assigned to interventions on the basis of computer-generated random number sequences. One researcher conducted the computer-generated random assignments; others executed the assignments. In year 1 of the study, women (n = 168) were randomly assigned to a one-on-one HIV/STD information intervention, a one-on-one HIV/STD behavioral skill-building intervention, a small-group HIV/STD information intervention, or a small-group HIV/STD skill-building intervention. In years 2 and 3, women (n = 396) were randomly assigned to 1 of the 4 HIV/STD interventions or a small-group health promotion intervention that served as the control group. (The results based on all women enrolled in the study compared with those enrolled in years 2 and 3 did not differ statistically.) Figure 1 ▶ shows the number of women randomized to each group.
FIGURE 1—
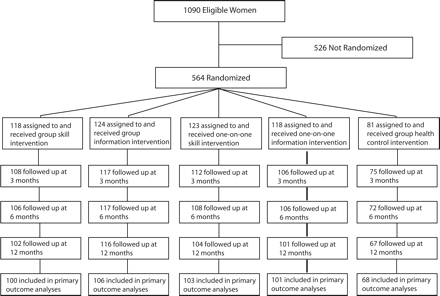
Progress of participants in brief HIV/STD risk-reduction interventions for African American women: “Sister-to-Sister: The Black Women’s Health Project,” Newark, NJ, 1993–1996.
Note. STD = sexually transmitted disease. Women who were not randomized failed to appear at the study site to be randomized and enrolled in the study for unknown reasons.
Intervention Methods
The interventions were based on social cognitive theory,10 which we adapted for this study using preliminary research, including quantitative surveys, elicitation surveys, and focus groups, with women from the study population. In addition, each intervention was pilot tested on women from the study population.
Designed to be educational but entertaining, culture sensitive, and gender appropriate, each intervention incorporated the “Sister to Sister! Respect Yourself! Protect Yourself! Because You Are Worth It!” theme that encouraged the participants to respect and protect themselves, not only for their own sake, but also for their family and community.
The one-on-one interventions involved a 20-minute session that the facilitator tailored to the specific needs of each participant after conducting an HIV/STD risk assessment interview. The one-on-one HIV/STD skill-building intervention was designed to increase skills regarding condom use. It involved a review of the “Sister to Sister” HIV/STD prevention behavioral skill brochure, video clips, condom demonstration, practice with an anatomical model, and role playing to increase self-efficacy and skills related to correct use of condoms and negotiation of condom use with a sexual partner.
The one-on-one HIV/STD information intervention was designed to increase knowledge about HIV/STD transmission and prevention and personal vulnerability to HIV/STDs. It involved a review of the “Sister to Sister” HIV/STD prevention information brochure and a discussion of basic HIV/STD risk-reduction information. It did not provide behavioral skill demonstrations or practice.
The group interventions consisted of a 200-minute session with 3 to 5 participants. The group HIV/STD behavioral skill-building intervention was designed to increase skills regarding condom use and to allay participants’ concerns about the adverse effects of condom use on sexual enjoyment. Group discussions, brainstorming, videos, interactive exercises, games, condom demonstrations, practice with anatomical models, and role playing were used to increase self-efficacy and skills related to correct use of condoms and negotiation of condom use with a sexual partner.
The group HIV/STD information intervention was designed to increase the perception of vulnerability to HIV/STDs and increase knowledge about HIV/STD transmission and prevention. Similar to the group skill-building intervention, this intervention involved group discussions, brainstorming, videos, interactive exercises, and games. However, it did not provide behavioral skill demonstrations or practice or address participants’ beliefs about the adverse effects of condom use on sexual enjoyment.
To reduce the likelihood that effects of the HIV/STD interventions could be attributed to nonspecific features,11 the control group received a general health promotion intervention. It focused not on HIV/STD risk behavior but on behaviors (diet, physical exercise, alcohol and tobacco use) associated with risk of heart disease, stroke, and cancer.
Facilitators and Facilitator Training
The facilitators who implemented the interventions were 28 African American female nurses (mean age = 38.0 years) from the Newark, NJ, area. Their median education was an undergraduate degree. They had a median of 14 years of experience as a nurse and 10 years of experience working with African American women. They all had the skills to implement any of the interventions. After stratifying them by age, we randomly assigned them to receive 8 hours of training to implement 1 of the 5 interventions. The training stressed the importance of implementing the intervention strictly according to the intervention manual.
Primary Outcome Measures
The primary outcomes were self-reported sexual behaviors in the previous 3 months, including proportion of protected sexual intercourse, frequency of unprotected sexual intercourse, and condom use during most recent intercourse. Participants completed confidential self-administered measures of these behaviors at baseline and 3, 6, and 12 months after the intervention. Proportion of protected sexual intercourse was the number of days on which the participants had sexual intercourse using a condom divided by the number of days on which they had sexual intercourse. Frequency of unprotected sexual intercourse was the number of days on which the participants had sexual intercourse without using a condom.
We took several steps to increase the validity of self-reported sexual behavior. To reduce potential memory problems, we asked women to report their behaviors over a brief period (i.e., 3 months),12 wrote the dates comprising the period on a chalkboard, and gave participants calendars clearly highlighting the period. To reduce the likelihood that demand characteristics would influence participants’ responses, proctors blind to the participants’ intervention—not the facilitators—collected the data. Participants signed an “agreement” pledging to answer the questions honestly, a procedure that has been shown to yield more valid self-reports on sensitive issues.13
Secondary Outcome Measure
The secondary outcome measure was STD rate. At baseline and 6- and 12-month follow-up, participants were screened for Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomonas vaginalis. The Gen-probe Pace–2 System (Gen-Probe Inc, San Diego, Calif) was used to detect N gonorrhoeae and C trachomatis in cervical specimens. Specimens were collected and then analyzed in the hospital-based laboratory according to the manufacturer’s instructions. Direct microscopic examination of saline wet mounts of vaginal secretions was used to detect T vaginalis. The wet mounts were immediately examined after collection at both 4 × and 10 × magnification. Wet mounts were considered positive if motile trichomonads were identified. The same clinician collected all the specimens and performed all the wet mount examinations. All identified STDs were treated according to Centers for Disease Control and Prevention treatment guidelines.14
The Marlowe–Crowne Social Desirability Scale,15 used extensively in studies of African American populations,16–18 assessed participants’ social desirability response bias—that is, the tendency to exaggerate the social acceptability of one’s behavior.
Statistical Analyses and Sample Size
We used the t test and the χ 2 test to analyze differences between participants and eligible nonparticipants. We used logistic repeated measures models to test whether attrition was related to intervention group or to any of the baseline measures of outcome variables. Three binary variables indicating participants’ attrition status at 3-, 6-, or 12-month follow-up were regressed on intervention groups, time, intervention by time interactions, and the baseline measure of each of the outcome measures. We used analyses of variance, the Kruskal–Wallis test, and the χ 2 test to determine whether there were baseline differences between groups despite randomization.
Generalized estimating equations (GEEs) with an unstructured working correlation matrix19 were used to fit repeated measures models to test hypotheses regarding sexual behaviors and STD rate. We analyzed binary data, including condom use during last intercourse and STD rate, using binomial-error models with logit-link functions. We analyzed count data—frequency of unprotected sexual intercourse—using Poisson error models with log-link functions.
The statistical significance of 3 orthogonal planned contrasts20 of prespecified hypotheses adjusted for baseline scores was evaluated using the Wald χ 2 test. Contrast 1 compared the one-on-one and group skill-building interventions with the control group. Contrast 2 compared the one-on-one and group skill-building interventions with the one-on-one and group information interventions. Contrast 3 compared the one-on-one skill-building intervention with the group skill-building intervention. With α =.05 (2-tailed), a total sample size of 470 participants completing the trial provided power of 80% to detect an estimated effect of d=0.32 standard deviation units in self-reported sexual behavior for contrast 1, power of 80% to detect an estimated effect of d=0.28 for contrast 2, and power of 80% to detect an estimated effect of d=0.40 for contrast 3. We tested interactions hierarchically; that is, we controlled for the main effects of all variables involved in the interaction.
The estimated effect size in standard deviation units (Cohen’s d, d) is presented for each significant contrast. Models evaluating intervention effects included the baseline measure of the outcome measures, intervention groups, time effects, and the intervention-by-time interaction. Tests of the effects of the interventions used an intention-to-treat approach in which data from all participants were analyzed regardless of the number of follow-up sessions they attended.
RESULTS
Participants
Of the participants, 12.1% were married, 76.4% had never married, and 11.5% were separated, divorced, or widowed. About 30.5% were employed. At baseline, 20.3% tested positive for N gonorrhoeae, C trachomatis, or T vaginalis. More specifically, 8.9% had C trachomatis, 11.3% had T vaginalis, and 2.6% had N gonorrhoeae. About 88.9% reported sexual intercourse during the previous 3 months. Only 23.5% of respondents who had intercourse in the previous 3 months reported always using condoms on those occasions. Few reported ever using injection drugs (2.4%) or having same-gender sexual relationships (1.3%).
As shown in Figure 1 ▶, 51.7% of the eligible women patients (i.e., 564 of 1090) participated in the study. Inspection of data culled from charts at the time of recruitment revealed that participants and eligible non-participants did not differ significantly in history of pregnancy, history of STDs, education, or type of payment for health care services. Three differences were significant: compared with nonparticipants, participants were more likely to be married (14.2% vs 9.6%, P = .02) and unemployed (66.1% vs 57.5%, P = .004) and were older (mean age = 27.06 [SD = 6.71] vs mean age = 25.60 [SD = 6.00], P < .001).
Baseline Comparability and Attrition
As shown in Table 1 ▶, analyses revealed no significant differences among the intervention groups on the baseline measures of demographic characteristics, self-reported sexual behavior, or STD prevalence.
TABLE 1—
Demographic Characteristics, Self-Reported Sexual Behavior, and Sexually Transmitted Disease (STD) Status at Baseline of Participants in Brief HIV/STD Risk-Reduction Interventions, by Intervention Group: “Sister-to-Sister: The Black Women’s Health Project,” Newark, NJ, 1993–1996
| Demographic Characteristic | Group Skill Intervention (n = 118) | One-on-One Skill Intervention (n = 123) | Group Information Intervention (n = 124) | Information One-on-One Intervention (n = 118) | Group Health Intervention (n = 81) | P |
| Age, y, mean (SE) | 27.0 (0.59) | 27.0 (0.59) | 27.3 (0.60) | 27.3 (0.63) | 27.3 (0.82) | .99b |
| Never married, % | 79.3 | 71.9 | 80.2 | 77.8 | 71.2 | .39c |
| Employed, %c | 28.7 | 27.7 | 33.6 | 30.5 | 32.5 | .86c |
| Sexually active in past 3 mo, % | 91.3 | 90.0 | 86.1 | 89.6 | 87.5 | .73c |
| Proportion of protected sexual intercourse occasions in past 3 mo, mean (SE) | 0.51 (0.04) | 0.55 (0.04) | 0.52 (0.05) | 0.58 (0.04) | 0.51 (0.05) | .80b |
| Used condom during last sexual intercourse , % | 43.0 | 38.3 | 34.2 | 40.7 | 37.3 | .70c |
| No. days of unprotected sexual intercourse in past 3 mo, mean (SE) | 9.67 (1.90) | 7.52 (1.59) | 8.00 (1.42) | 6.36 (1.08) | 11.15 (2.35) | .94d |
| No. sexual partners in past 3 mo, mean (SE) | 1.32 (0.11) | 1.26 (0.09) | 1.07 (0.07) | 1.28 (0.18) | 1.05 (0.06) | .55d |
| STD positive, %e | 20.4 | 21.6 | 21.1 | 16.5 | 22.7 | .85c |
Note. The group health intervention was the control group. All group interventions lasted 200 minustes; all one-on-one interventions lasted 20 minutes.
aSkill-building interventions were aimed at increasing skill related to the correct use of condoms and the negotiation of condom use with a sexual partner; information interventions were designed to increase knowledge about HIV/STD transmission and prevention and personal vulnerability to HIV/STDs. The control group received a general health promotion intervention focused not on HIV/STD risk behavior but on behaviors (diet, physical exercise, alcohol and tobacco use) associated with risk of heart disease, stroke, and cancer.
bUsing analysis of variance (ANOVA).
cUsing the χ2 test.
dUsing the Kruskal—Wallis test.
ePercentage STD positive is the percentage that tested positive for Neisseria gonorrhoeae, Chlamydia trachomatis, or Trichomonas vaginalis.
The return rates were 91.8%, 90.2%, and 86.9% at the 3-, 6-, and 12-month follow-ups, respectively, with 96.3% of participants attending at least 1 follow-up. Baseline measures of outcome variables were the same for women who attended at least 1 follow-up and for those who did not. Figure 1 ▶ presents the follow-up return rates by intervention group. None of the differences were statistically significant.
Effects of Behavioral Interventions on Sexual Behaviors and STD Rate
As shown in Table 2 ▶, at the 3-month follow-up, women who received the skill-building interventions reported using condoms a greater proportion of the time during sexual intercourse in the previous 3 months than women who received the information interventions (d = 0.24, P = .02). At the 12-month follow-up, women in the skill-building interventions reported higher rates of condom use than women who received either the information interventions (d = 0.21, P = .051) or the control group (d = 0.24, P = .03). In addition, the group skill-building intervention participants reported a greater proportion of protected sexual intercourse at the 12-month follow-up than did the one-on-one skill-building intervention participants (d=0.21, P=.049).
TABLE 2—
Self-Reported Sexual Behavior in the Previous 3 Months and Sexually Transmitted Disease (STD) Status of Participants in Brief HIV/STD Risk-Reduction Interventions, by Intervention Group and Follow-Up Period: “Sister-to-Sister: The Black Women’s Health Project,” Newark, NJ, 1993–1996
| Intervention Groupa | P for Contrasts | |||||||
| Behavior and STD Status | Group Skill (n = 118) | One-on- One Skill (n = 123) | Group Information (n = 124) | One-on-One Information (n = 118) | Group Health (n = 81) | Skill Groups vs Control | Skill Groups vs Information Groups | Group Skill vs One-on-One Skill |
| Protected sexual intercourse, adjusted mean proportion (SE) | ||||||||
| At 3-mo follow-up | 0.75 (0.02) | 0.74 (0.02) | 0.69 (0.02) | 0.67 (0.02) | 0.68 (0.02) | .10 | .02 | .89 |
| At 6-mo follow-up | 0.73 (0.02) | 0.70 (0.02) | 0.68 (0.02) | 0.67 (0.02) | 0.72 (0.02) | .85 | .07 | .68 |
| At 12-mo follow-up | 0.79 (0.02) | 0.70 (0.02) | 0.69 (0.02) | 0.69 (0.02) | 0.62 (0.03) | .03 | .05 | .05 |
| Condom use at last sexual intercourse, adjusted proportion (SE) | ||||||||
| At 3-mo follow-up | 0.52 (0.02) | 0.52 (0.02) | 0.51 (0.02) | 0.51 (0.02) | 0.39 (0.03) | .05 | .92 | .48 |
| At 6-mo follow-up | 0.60 (0.02) | 0.46 (0.02) | 0.46 (0.02) | 0.59 (0.02) | 0.51 (0.03) | .89 | .69 | .13 |
| At 12-mo follow-up | 0.59 (0.02) | 0.55 (0.02) | 0.36 (0.02) | 0.52 (0.02) | 0.40 (0.03) | .03 | .01 | .80 |
| Unprotected sexual intercourse, adjusted mean frequency (SE) | ||||||||
| At 3-mo follow-up | 4.49 (0.73) | 3.08 (0.46) | 5.32 (0.54) | 5.40 (0.42) | 8.20 (1.62) | .02 | .01 | .69 |
| At 6-mo follow-up | 4.93 (0.73) | 3.38 (0.51) | 3.77 (0.34) | 5.58 (0.34) | 6.90 (1.47) | .59 | .16 | .67 |
| At 12-mo follow-up | 5.14 (0.89) | 3.60 (0.64) | 5.94 (0.62) | 5.12 (0.24) | 8.34 (1.90) | .18 | .02 | .58 |
| Tested positive for STD, adjusted % (SE) | ||||||||
| At 6-mo follow-up | 0.18 (0.003) | 0.22 (0.004) | 0.16 (0.003) | 0.17 (0.003) | 0.15 (0.004) | .35 | .38 | .45 |
| At 12-mo follow-up | 0.15 (0.003) | 0.14 (0.003) | 0.19 (0.003) | 0.22 (0.004) | 0.27 (0.006) | .03 | .13 | .82 |
Note. The adjusted means and proportions are the follow-up measure partialling out (removing the effect of the baseline measure) the effect of the baseline measure. P values were derived using the Wald χ2 test of the generalized estimating equation (GEE) models. The model for intervention effects at each follow-up includes baseline behavior, intervention group, time, and time-by-intervention interaction. STD is a positive test for Neisseria gonorrhoeae, Chlamydia trachomatis, or Trichomonas vaginalis. Proportion of protected sexual intercourse was analyzed through use of identity link by specifying the normal distribution in the GEE. STD results and condom use at last sexual intercourse were analyzed through logit link by specifying the binomial distribution in the GEE. Frequency of unprotected intercourse was analyzed through log link by specifying the Poisson distribution in the GEE. The group health intervention was the control group.
aSkill-building interventions were aimed at increasing skill related to the correct use of condoms and the negotiation of condom use with a sexual partner; information interventions were designed to increase knowledge about HIV/STD transmission and prevention and personal vulnerability to HIV/STDs. The control group received a general health promotion intervention focused not on HIV/STD risk behavior but on behaviors (diet, physical exercise, alcohol and tobacco use) associated with risk of heart disease, stroke, and cancer.
When asked specifically about the last time they had sexual intercourse, women who received the skill-building interventions were more likely to report using a condom than those who received the health control intervention (d = 0.18, P = .050) at the 3-month follow-up and than those receiving either the health control intervention (d = 0.20, P = .034) or the information intervention (d = 0.23, P = .014) at the 12-month follow-up.
Skill-building intervention participants also reported less unprotected sexual intercourse than did information intervention participants (d = 0.25, P = .012) or control group participants (d = 0.23, P = .019) at the 3-month follow-up and information intervention participants at 12-month follow-up (d = 0.23, P = .024). None of the contrasts was statistically significant at the 6-month follow-up.
GEE analyses revealed that although there were no differences at 6-month follow-up (P = .353), women who had received the skill-building interventions were significantly less likely to test positive for a new STD at the 12-month follow-up than were those in the control group (d = 0.20, P = .032).
Social Desirability Response Bias
Multiple regression analyses revealed that Marlowe-Crowne Social Desirability Scale scores did not interact with intervention group to influence sexual behavior reported at any of the follow-ups. Analyses restricted to women in the 4 HIV/STD interventions also revealed that social desirability scores were unrelated to self-reported sexual behavior at the follow-ups.
DISCUSSION
The results of this study suggest that brief culture-sensitive, cognitive-behavioral, skill-building interventions can reduce self-reported HIV/STD risk behavior among African American women and that the intervention effects can be sustained at relatively long-term follow-up, 12 months after the intervention’s implementation. These findings are consonant with a few other randomized controlled trials in supporting the view that cognitive behavioral skill-building interventions can reduce sexual-risk behavior among women.6,8,9,21–24
We also found that the skill-building interventions modestly reduced the rate of STD at the 12-month follow-up compared with the control group. Although other randomized controlled trials have demonstrated that sexual risk-reduction interventions can reduce the biologically confirmed STD rate among women, our trial differed from those studies in important respects. For instance, the one-on-one intervention employed here involved one 20-minute session, whereas the interventions in the study by Kamb et al. involved two 40-min sessions.7 Moreover, the small-group intervention employed in this study involved only 1 session and was much shorter than the multisession interventions used in the other studies.6,8
This trial is the first to compare the efficacy of one-on-one and small-group skill-building interventions to reduce sexual risk. The only significant difference was that the group skill-building intervention caused a greater increase in the proportion of protected sexual intercourse acts at the 12-month follow-up than did the one-on-one skill-building intervention. It is surprising that there were not more differences inasmuch as the group skill-building intervention was substantially longer and participants might have benefited from modeling and feedback from other group members. It may well be that the individually delivered skill-building intervention elicited more personal disclosure; hence, skill building in that intervention may have been more tailored to individual women’s life situation. In any event, our results suggest that those who seek to reduce sexual risk behavior among African American women can fruitfully employ either type of intervention.
This study has several strengths. It used a randomized controlled trial. It examined biologically confirmed STDs as an outcome25 and thus provided data on the interventions’ impact on disease prevention. The attrition rates were low and, most importantly, did not differ between groups. Moreover, the study imposed few limitations on inclusion. The participants were women who attended a health clinic for various health issues, including infertility, pregnancy, and annual screenings. By not excluding women who tested negative for STD at baseline, who were in long-term relationships, who were married, or who had not engaged in unprotected sexual intercourse recently, the study maintained the ability to generalize to the diverse population served in women’s health clinics.
Limitations
A limitation of this study is that the primary outcome, sexual behavior, was measured with self-reports, which might have been unintentionally or intentionally inaccurate.26 Several aspects of our methods and findings weaken the plausibility of inaccurate self-reports as an explanation for our results. We have described the strategies that we employed to increase participants’ ability to recall their behavior accurately and to motivate them to respond honestly. The results also revealed that self-reported sexual behavior and changes in sexual behavior were unrelated to a standard measure of social desirability response bias. Moreover, the results for STD rate, a biological outcome measure that was not based on self-reports, dovetailed with those for self-reported behavior. There were fewer significant effects of the skill-building interventions on self-reported behavior at the 6-month follow-up than at the 12-month follow-up. Similarly, at the 6-month follow-up, there were no significant intervention effects on STDs, but at the 12-month follow-up, skill-building intervention participants were less likely to have an STD than were control group participants.
The delayed effect of the intervention observed in this trial has been observed in other studies.27,28 One possible explanation for such a delayed effect is that women have difficulty introducing safer-sex practices into existing relationships.29–31 As they become involved with new sexual partners over time, they are able to implement those practices; hence, intervention effects are larger at longer-term follow-up.
Conclusions
The results of our study support several tentative conclusions. They suggest that brief, culture-sensitive, cognitive-behavioral, skill-building interventions can reduce the HIV/STD risk behavior of African American women and that intervention-induced changes in such behavior can be sustained at relatively long-term follow-up, 12 months after implementation. The finding that the effects of the skill-building interventions in modestly reducing the rate of STDs paralleled the interventions’ effects on self-reported behavior increases confidence in the results. This study, with its excellent retention rates, lends credence to the notion that, to achieve desired outcomes, HIV/STD behavioral interventions may not have to be long in duration and implemented over multiple sessions—characteristics that diminish their practicality in primary health care settings. The single-session interventions in this study are feasible in primary health care settings. Nurses and other primary care providers can implement them.
The current results must be replicated with other populations of women in other settings, particularly women at higher risk. Research along these lines may contribute to efforts to reduce the spread of sexually transmitted HIV infection, which has already killed too many African American women and orphaned too many children.
Acknowledgments
This research was supported by the National Institute for Nursing Research (grant R01 NR03123).
The authors gratefully acknowledge the contributions to this research of Jane Bliss-Holtz, Felecia Briggs, Veronica Catan, Monique Howard, Kathleen Jennings-Dossier, Cornelia Nichols, Sonia O’Leary, Vivian Steinmetz, Luretna Stribling, Beverly Whipple; the nurse facilitators, nurse practitioners, lab technicians, unit clerks, babysitters, and clinic nursing staff; and the helpful suggestions of Linda H. Aiken, Paula K. Braverman, Geoffrey T. Fong, Lorraine Tulman, and Antonia M. Villarruel, regarding an earlier version of this article.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Human Participant Protection The institutional review boards of the University of Pennsylvania and Rutgers University approved the study.
Peer Reviewed
Contributors L. S. Jemmott oversaw all aspects of the study, led the development of the intervention procedures and training of facilitators, and was the lead author. J. B. Jemmott III assisted in all aspects of the study and led development of the design, measures, and data analysis. A. O’Leary assisted in the development of the intervention procedures and measures and the application of social cognitive theory. All authors helped to secure funding, conceptualize ideas, interpret findings, and review drafts of the article.
References
- 1.Eng TR, Butler W. The Hidden Epidemic: Confronting Sexually Transmitted Diseases. Washington, DC: National Academies Press; 1997. [PubMed]
- 2.Centers for Disease Control and Prevention. Summary of notifiable diseases—United States, 2000. MMWR Morb Mortal Wkly Rep. 2002;49(53):1–101. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV AIDS Surveill Rep. 2005;16:1–46. [Google Scholar]
- 4.Anderson RN, Smith BL. Deaths: leading causes for 2002. Natl Vital Stat Rep. March 7, 2005;53: 1–92. [PubMed] [Google Scholar]
- 5.Interventions to prevent HIV risk behaviors. NIH Consens Statement. 1997;15:1–41. [PubMed] [Google Scholar]
- 6.Shain RN, Piper JM, Newton ER, et al. A randomized, controlled trial of a behavioral intervention to prevent sexually transmitted disease among minority women. N Engl J Med. 1999;340:93–100. [DOI] [PubMed] [Google Scholar]
- 7.Kamb ML, Fishbein M, Douglas JM, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA. 1998;280:1161–1167. [DOI] [PubMed] [Google Scholar]
- 8.Wingood GM, DiClemente RJ, Mikhail I, et al. A randomized controlled trial to reduce HIV transmission risk behaviors and sexually transmitted diseases among women living with HIV: The WiLLOW Program. J Acquir Immune Defic Syndr. 2004;37(Suppl 2): S58–S67. [DOI] [PubMed] [Google Scholar]
- 9.Kelly JA, Murphy DA, Washington CD, et al. The effects of HIV/AIDS intervention groups for high-risk women in urban clinics. Am J Public Health. 1994;84: 1918–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
- 11.Cook TD, Campbell DT. Quasi-Experimentation: Design and Analysis Issues for Field Settings. Chicago, Ill: Rand McNally; 1979.
- 12.Kauth MR, St. Lawrence JS, Kelly JA. Reliability of retrospective assessments of sexual HIV risk behavior: a comparison of biweekly, three-month, and twelvemonth self-reports. AIDS Educ Prev. 1991;3:207–214. [PubMed] [Google Scholar]
- 13.Sudman S, Bradburn NM. Response Effects in Surveys. Chicago, Ill: Aldine; 1974.
- 14.Centers for Disease Control and Prevention. 1993 sexually transmitted diseases treatment guidelines. MMWR Morb Mortal Wkly Rep. 1993;42(RR-14): 1–102. [PubMed] [Google Scholar]
- 15.Crowne D, Marlowe D. The Approval Motive. New York, NY: Wiley; 1964.
- 16.Carr JG, Gilroy FD, Sherman MF. Silencing the self and depression among women: the moderating role of race. Psychol Women Q. 1996;20:375–392. [Google Scholar]
- 17.Jensen BJ, Witcher DB, Lane ME. Cognitive and social desirability factors in marital adjustment for black subjects: a preliminary report. South Psychol. 1987;3:51–55. [Google Scholar]
- 18.McFarland SG, Sparks CM. Age, education, and the internal consistency of personality scales. J Pers Soc Psychol. 1985;49:1692–1702. [Google Scholar]
- 19.Diggle PJ, Liang KY, Zeger S. Analysis of Longitudinal Data. New York, NY: Oxford University Press; 1994.
- 20.Rosenthal R, Rosnow RL. Contrast Analysis: Focused Comparisons in the Analysis of Variance. New York, NY: Cambridge University Press; 1985.
- 21.El-Bassel N, Witte S, Gilbert L, Wu E, Hill J, Steinglass P. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am J Public Health. 2003;93:963–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sikkema KJ, Kelly JA, Winett RA, et al. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. Am J Public Health. 2000;90:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wyatt GE, Longshore D, Chin D, et al. The efficacy of an integrated risk reduction intervention for HIV-positive women with child sexual abuse histories. AIDS Behav. 2004;8:453–462. [DOI] [PubMed] [Google Scholar]
- 24.Ehrhardt A, Exner T, Hoffman S, et al. A gender-specific HIV/STD risk reduction intervention for women in a health care setting: short- and long-term results of a randomized clinical trial. AIDS Care. 2002; 14:147–161. [DOI] [PubMed] [Google Scholar]
- 25.O’Leary A, DiClemente RJ, Aral SO. Reflections on the design and reporting of STD/HIV behavioral intervention research. AIDS Educ Prev. 1997;9(1 suppl): 1–14. [PubMed] [Google Scholar]
- 26.Catania J, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108: 339–362. [DOI] [PubMed] [Google Scholar]
- 27.Jemmott JB III, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: a randomized controlled trial. Arch Pediatr Adolesc Med. 2005;159:440–449. [DOI] [PubMed] [Google Scholar]
- 28.Johnson WD, Hedges LV, Ramirez G, et al. HIV prevention research for men who have sex with men: a systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2002;30(Suppl 1):S118–S129. [PubMed] [Google Scholar]
- 29.Morrill AC, Ickovics JR, Golubchikov VV, Beren SE, Rodin J. Safer sex: social and psychological predictors of behavioral maintenance and change among heterosexual women. J Consult Clin Psychol. 1996;64: 819–828. [DOI] [PubMed] [Google Scholar]
- 30.Sanderson CA, Jemmott JB III. Moderation and mediation of HIV prevention interventions: relationship status, intentions, and condom use among college students. J Appl Soc Psychol. 1996;26:2076–2099. [Google Scholar]
- 31.St Lawrence JS, Wilson TE, Eldridge GD, Brasfield TL, O’Bannon RE 3rd. Community-based interventions to reduce low income, African American women’s risk of sexually transmitted diseases: a randomized controlled trial of three theoretical models. Am J Community Psychol. 2001;29:937–964. [DOI] [PubMed] [Google Scholar]


