Abstract
Objectives. We assessed the epidemiology of primary and secondary syphilis in the United States and estimated the percentages of cases occurring among men who have sex with men (MSM).
Methods. We reviewed US syphilis surveillance data from 1990 through 2003. We estimated the number of cases occurring among MSM by modeling changes in the ratio of syphilis cases among men to cases among women.
Results. During 1990 through 2000, the rate of primary and secondary syphilis decreased 90% overall, declining 90% among men and 89% among women. The overall rate increased 19% between 2000 and 2003, reflecting a 62% increase among men and a 53% decrease among women. In 2003, an estimated 62% of reported cases occurred among MSM.
Conclusions. Increasing syphilis cases among MSM account for most of the recent overall increase in rates and may be a harbinger of increasing rates of HIV infection among MSM. National efforts are under way to improve monitoring of syphilis trends, better understand factors associated with the observed increases, and improve efforts to prevent syphilis transmission.
Syphilis is an ulcerative genital disease that facilitates transmission and acquisition of HIV infection and provides a marker of behaviors associated with HIV infection.1 Although syphilis is uncommon in much of the US population, several groups are disproportionately affected, including African Americans, Hispanics, and men who have sex with men (MSM).2–4 During the 1980s, the incidence of primary and secondary syphilis increased 54%, and racial/ethnic and regional disparities became more pronounced.3,5
However, the rapid decline in the rate of syphilis infection and the increasing concentration of cases in a small proportion of US counties during the early to mid-1990s led to optimism that syphilis could be eliminated in the United States. The National Plan to Eliminate Syphilis was announced in October 1999, with elimination defined as the absence of sustained transmission of syphilis.6 Healthy People 2010 objectives calling for decreases in rates and disparities in occurrence of disease among racial and ethnic groups were developed along with the syphilis elimination plan.7
During the 1990s, the overall incidence of syphilis and racial/ethnic disparities in the occurrence of disease declined; however, the rate of primary and secondary syphilis has increased each year since 2001. Although syphilis cases among MSM accounted for a small proportion of cases between the mid-1980s and the late 1990s, cases among MSM have been increasing in recent years. Increases in high-risk sexual behavior among MSM have been documented since the mid-1990s,8–10 and there have been reports of syphilis outbreaks among MSM in a number of US cities,11–20 Europe,21–28 and the United Kingdom29–32 since the late 1990s. We examined gender, racial/ethnic, and geographic trends in the incidence of primary syphilis and secondary syphilis (hereafter combined as “syphilis”) in the United States during 1990 through 2003, with particular attention to the reemergence of syphilis among MSM since the late 1990s.
METHODS
Between 1990 and 2003, the years examined in this study, state health departments submitted syphilis case report data to the Centers for Disease Control and Prevention (CDC) on monthly, quarterly, and annual reporting forms or weekly electronic case-specific records. Monthly reports included aggregate syphilis case data by county and state. Quarterly reports included aggregate case data by gender, stage, and source of report for each state and for the 63 large US cities in which cases and rates have been monitored by the US Public Health Service since 1941. Annual reports included aggregate data by age group, race/ethnicity, and gender for each state.
As of December 2002, all states were reporting case-specific syphilis data electronically. We analyzed data on reported cases of syphilis in the primary and secondary stages, which have been summarized in annual sexually transmitted disease (STD) surveillance reports,3,33,34 because these cases best represent the incidence of syphilis. Cases reported from public and private sources were combined.
We calculated incidence rates (new cases per 100 000 population) on an annual basis using US Census Bureau population estimates for 1990,35 US Census Bureau 1991 through 1999 postcensal population estimates based on the 1990 census, and 2000 census population estimates with race and ethnicity bridged to match 1990 through 1999 population race/ethnicity categories.36 Rates for 2000 through 2003 were postcensal population estimates based on the 2000 census. National, regional, and state incidence rates were determined from aggregate county age, gender, and race/ethnicity data. Incidence rates for cities were estimated from county-level data.
In the absence of national data on sexual orientation or gender of partners, we assumed that increases in male–female case ratios (MFCRs) of syphilis reflected, in part, increases in cases among MSM. We estimated the number of cases occurring among MSM each year during 2000 through 2003 using a model based on changes in the syphilis MFCR during 1998 through 2003. We estimated numbers of syphilis cases occurring annually among MSM during 2000 through 2003 using the following formula: MSM cases = ([annual MFCR − 1998 MFCR]/annual MFCR) × (annual number of cases among men). In this estimate, we assumed that (1) no cases of syphilis occurred among MSM when the MFCR was at or below the 1998 level of 1.26 and (2) any increase in the MFCR for nationally reported syphilis cases after 1998 could be attributed to cases occurring among MSM.
We selected the year 1998 as a baseline because surveillance data indicated that MFCRs had remained relatively constant for the previous 5 years. Although cases of syphilis occurred among MSM in 1998 and in other years during which the MFCR was at or below 1.26, we were not able to quantify them, and thus we made the conservative assumption that no cases occurred among MSM during these years. A study conducted to validate the model showed that the number of syphilis cases among MSM estimated using the model was similar to the number of cases among MSM determined with data, including partner gender, collected from 14 states or large cities during 1999 through 2002.37
RESULTS
Between 1990 and 2003, the incidence of syphilis in the United States declined 87.7%, reflecting decreases of 82% and 95% among men and women, respectively (Table 1 ▶). During these years, rates decreased in all racial/ethnic groups, declining 95% among African Americans, 81% among Hispanics, 53% among American Indians, 42% among Whites, and 38% among Asians. Rates also decreased in all US regions, declining 91% in the Northeast, 91% in the South, 79% in the Midwest, and 76% in the West. In 1990, cases of syphilis were reported by 42% of US counties, and 26 counties accounted for half of all reported cases; in 2003, only 19% of counties reported cases, and 18 counties and 1 independent city accounted for half of all reported cases.
TABLE 1—
Primary and Secondary Syphilis Cases and Incidence Rates (per 100 000 Population), by Gender, Race/Ethnicity, and Region: United States, 1990, 2000, and 2003
| 1990, No. (Rate) | 2000, No. (Rate) | 2003, No. (Rate) | |||||||
| Men | Women | Total | Men | Women | Total | Men | Women | Total | |
| Race/ethnicity | |||||||||
| White | 2 983 (3.3) | 1 910 (2.0) | 4 893 (2.6) | 698 (0.7) | 385 (0.4) | 1 083 (0.5) | 2 783 (2.8) | 227 (0.2) | 3 010 (1.5) |
| African American | 22 821 (165.8) | 18 791 (122.0) | 41 612 (142.8) | 2 369 (14.2) | 1 864 (10.1) | 4 233 (12.0) | 2 005 (11.5) | 805 (4.2) | 2 811 (7.7) |
| Hispanic | 2 366 (20.8) | 1 109 (10.1) | 3 475 (15.2) | 405 (2.2) | 162 (0.9) | 567 (1.6) | 1 001 (4.9) | 159 (0.8) | 1 160 (3.0) |
| Asian/Pacific Islander | 76 (2.1) | 37 (1.0) | 113 (1.6) | 29 (0.5) | 8 (0.1) | 37 (0.3) | 119 (1.9) | 8 (0.1) | 127 (1.0) |
| American Indian | 50 (5.2) | 57 (5.8) | 107 (6.0) | 26 (2.2) | 26 (2.2) | 52 (2.2) | 50 (4.2) | 19 (1.5) | 69 (2.8) |
| Regiona | |||||||||
| Northeast | 6 354 (25.9) | 5 014 (19.0) | 11 368 (22.3) | 278 (1.1) | 93 (0.3) | 371 (0.7) | 1 014 (3.8) | 122 (0.4) | 1 137 (2.1) |
| Midwest | 2 585 (8.9) | 1 875 (6.1) | 4 460 (7.5) | 682 (2.2) | 592 (1.8) | 1 274 (2.0) | 813 (2.5) | 232 (0.7) | 1 045 (1.6) |
| South | 15 844 (38.0) | 12 944 (29.3) | 28 788 (33.6) | 2 098 (4.3) | 1 606 (3.1) | 3 704 (3.7) | 2 514 (4.9) | 699 (1.3) | 3 214 (3.1) |
| West | 3 707 (14.0) | 2 255 (8.5) | 5 962 (11.2) | 474 (1.5) | 154 (0.5) | 630 (1.0) | 1 615 (4.9) | 164 (0.5) | 1 781 (2.7) |
| Total | 28 490 (23.4) | 22 088 (17.3) | 50 578 (20.3) | 3 532 (2.6) | 2 445 (1.7) | 5 979 (2.1) | 5 956 (4.2) | 1 217 (0.8) | 7 177 (2.5) |
aNortheast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
Between 1990 and 2003, the age groups with the highest rates of syphilis changed in the case of men but not women. In 1990, rates were highest among men aged 20 to 24 years (56.3 cases per 100 000 men) and 30 to 34 years (56.2 cases per 100 000 men) and among women aged 20 to 24 years (61.4 cases per 100 000 women). In 2003, rates were highest among men aged 35 to 39 years (12.0 cases per 100 000 men) and women aged 20 to 24 years (2.4 cases per 100 000 women).
Syphilis rates declined consistently during the 1990s. From 1990 to 2000, rates among both men and women declined each year, and the overall rate in 2000 was the lowest at that point since the initiation of national reporting in 1941. Also during that period, overall rates of infection declined in all racial/ethnic groups and all regions of the United States, and rates decreased each year among African Americans and in the South. Over these years, rates decreased in 49 states and the District of Columbia and increased in 1 state. However, between 2000 and 2003, the overall syphilis rate increased 19%, with rates growing among men but continuing to decline among women.
Between 2000 and 2003, the rate among men increased 62%, and rates increased across all racial and ethnic groups with the exception of African Americans. The rate among women declined 53%, and rates declined among all racial and ethnic groups other than Asian women, among whom the rate did not change. Rising cases among White men accounted for most of the rate increase among men, whereas declining cases among African American women accounted for most of the rate decrease among women. Over these years, the increase in cases among White men (2085 cases) accounted for 86% of the overall increase among men (2424 cases), and the decrease in cases among African American women (1059 cases) accounted for 86% of the overall decrease among women (1228 cases).
There were substantial geographical changes in syphilis rates during 2000 through 2003. Rates tripled in the Northeast and increased 170% in the West but declined by 20% and 16% in the Midwest and South, respectively. Rates increased in 30 states, declined in 18 states, and remained unchanged in 2 states (Figure 1 ▶). Among men, rates increased in all regions and in 36 states, declined in 13 states, and remained unchanged in 1 state. Among women, however, rates increased in the Northeast and 14 states; declined in the Midwest, the South, and 24 states; and remained unchanged in the West and 12 states.
FIGURE 1—

Reported primary and secondary syphilis rates (per 100 000 population), by state, among (a) men in 2000, (b) men in 2003, (c) women in 2000, and (d) women in 2003: United States.
The ratio of syphilis cases reported among men to cases reported among women began to change in the late 1990s. The MFCR was low and relatively stable during the early to mid-1990s but increased more than 4-fold (from 1.2 to 4.9) between 1997 and 2003, growing most sharply after 2000. Between 2000 and 2003, MFCRs increased in all racial and ethnic groups and in all US regions. Ratios increased almost 7-fold among Whites, more than 4-fold among Asians, almost 3-fold among American Indians, almost 3-fold among Hispanics, and almost 2-fold among African Americans. Ratios increased approximately 3-fold (range: 2.7–3.2) in each of the 4 US regions.
Rapid and dramatic changes in syphilis profiles occurred in large US cities, as reflected by the increases in MFCRs that occurred during 2000 through 2003. MFCRs increased in 52 (82%) of the 63 large US cities in which cases and rates have been monitored for the past 6 decades. In these cities, the aggregate MFCR increased from 1.5 to 5.9. In 2000, only 26 cities had MFCRs of 2 or greater, and they accounted for 25% of the 3265 cases reported in large cities that year; only 2 cities had case ratios above 10. By 2003, 48 cities had MFCRs of 2 or greater, accounting for 85% of the 4334 cases reported in large cities; furthermore, 19 cities had case ratios greater than 10.
Nine large cities reported an increase of more than 50 cases between 2000 and 2003; these cities accounted for 11% of all cases reported in 2000 and 32% of all cases reported in 2003. During the same period, there were substantial and approximately simultaneous increases in cases among men in the 9 cities (Figure 2 ▶), and the aggregate MFCR in these cities increased from 3.3 to 14.1. Increases in MFCRs were not confined to large urban areas during these years, however. When cases from the 63 large cities were excluded, there was still an increase from 1.3 to 3.8 in the MFCR for the remainder of the nation.
FIGURE 2—
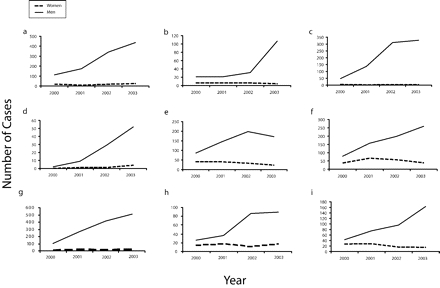
US cities with increases of more than 50 reported primary and secondary syphilis cases, by number of cases and gender, in (a) Los Angeles, Calif, (b) San Diego, Calif, (c) San Francisco, Calif, (d) San Jose, Calif, (e)Miami, Fla, (f) Atlanta, Ga, (g) New York, NY, (h) Columbus, Ohio, and (i) Houston, Tex: United States, 2000–2003.
As mentioned, we estimated the number of cases of syphilis occurring among MSM using a model based on changes in the MFCR over time. The model estimated that syphilis cases occurring among MSM increased from 441 in 2000 to 4387 in 2003 (Table 2 ▶); the estimated percentage of all reported cases occurring among MSM in 2003 was 62%. During 2000 through 2003, there was an estimated increase of 2298 cases among White MSM (data not shown). The model estimated that cases among heterosexual men and women (total number of cases minus number of cases occurring among MSM) decreased 50% (from 5532 to 2790) between 2000 and 2003.
TABLE 2—
Numbers of Primary and Secondary Syphilis Cases Among Different Groups, Along With Male–Female Case Ratios: United States, 2000–2003
| Year | Total No. of Cases | Cases Among Men | Cases Among Women | Male–Female Case Ratio | Cases Among MSMa | Cases Among Heterosexual Men and Womenb |
| 2000 | 5973 | 3528 | 2445 | 1.44 | 441 | 5532 |
| 2001 | 6100 | 4132 | 1968 | 2.10 | 1653 | 4447 |
| 2002 | 6862 | 5268 | 1594 | 3.30 | 3257 | 3605 |
| 2003 | 7177 | 5959 | 1218 | 4.89 | 4424 | 2753 |
Note. MSM = men who have sex with men.
aEstimated by assuming that a male–female case ratio at the 1998 level (1.26) indicates that no primary and secondary syphilis cases occurred among MSM and that the number of cases occurring among MSM can be calculated according to the formula described in the text.
bCalculated by subtracting estimated cases among MSM from the total number of cases.
DISCUSSION
Although syphilis rates in the United States declined steeply between 1990 and 2003, syphilis cases among MSM rose sharply after 2000, accounting for the overall increase in syphilis during 2000 through 2003. National case report data do not contain information on partner gender or other behavioral factors; however, according to investigations of syphilis infections conducted in the early to mid-1990s38–40 (and consistent with the low MFCRs over that period), heterosexual transmission was responsible for most of the cases that occurred during these years. In contrast, by 2003, it appears that the majority of syphilis cases reported annually were occurring among MSM, as evidenced by declines in rates among women, increasing rates among men, estimates of cases among MSM derived from our study’s modeling of changes in MFCRs, and recent reports of syphilis outbreaks among MSM.11–20
During the syphilis epidemic that occurred between the late 1980s and early 1990s, the rate of syphilis peaked in 1990, with a rate higher than that in any year since 1949.4 This epidemic, which predominantly involved heterosexual men and women, is thought to have been fueled by the use of crack cocaine and the exchange of sex for drugs or money.6,41–45 The reasons for the rapid decline in the syphilis rate after 1990 are unclear but may reflect a refocusing of prevention efforts to address syphilis and increased resources provided to STD-control programs after recognition of the epidemic.45 During this period, STD-control programs used a combination of traditional (e.g., partner notification) and new (e.g., counseling and education to promote risk reduction and targeted screening and prevention efforts) approaches.43,45–47 A decrease in the number of people using crack cocaine in the late 1980s and early 1990s48,49 may also explain some of the decline in syphilis rates after 1990.
Throughout the 1990s, rates of syphilis declined in all regions of the United States, and cases became concentrated in a small percentage of counties. Although the rate of decline was steepest in the Northeast during these years, the reduction in numbers of cases was largest in the South. Rates of disease declined among all racial and ethnic groups during the 1990s, particularly African Americans and Hispanics, but rates remained substantially higher among members of racial and ethnic minority groups than among Whites at the end of the decade. In the mid-1990s, in part because of the large racial disparity in syphilis rates, initial syphilis elimination efforts focused on syphilis among minority populations and in the South.4
The disparity in rates of syphilis infection between African Americans and Whites has decreased because of the continued decline in the rate of infection among African Americans, particularly African American women, and the increased rate of infection among White men. Rates of syphilis remain higher among African Americans than among Whites; however, in 2003, for the first time since the initiation of race/ethnicity-specific case reporting in 1981, more cases were reported among Whites than among African Americans.3,33,34,50
The geographic pattern of syphilis infection has also shifted. Although the rate of syphilis and the number of cases reported annually have been consistently higher in the South than in other US regions, the South has accounted for a declining proportion of overall annual cases each year since 1997.3,51 During 2000 through 2003, syphilis rates increased substantially in the Northeast and West but declined in the South and Midwest; large increases in cases among men accounted for most of the growth in rates in the Northeast and West, whereas decreasing numbers of cases among African American women accounted for most of the decline in rates in the South and Midwest.
Between 2000 and 2003, the largest increase in cases, by gender and race/ethnicity, occurred among White men. The substantial increases in cases among White men and estimates of MSM cases based on the steep rise in the MFCR among Whites suggest that cases among White MSM account for most of the recent national increase in syphilis cases among men. However, cases have been increasing among men from all racial/ethnic groups other than African Americans, and MFCRs have been increasing among all racial and ethnic groups, indicating that cases have been increasing among MSM in each of these groups.
The dramatic increases since 2000 among men and MFCRs in US cities, along with evidence that the current syphilis epidemic is not confined to the largest urban centers, indicate that the occurrence of syphilis among MSM is increasing throughout the United States. Since the late 1990s, there have also been widespread outbreaks of syphilis in the United Kingdom and many European countries, and as in the United States, a high proportion of involved men have been coinfected with HIV.21–32 These coincident outbreaks among MSM suggest that substantial and concurrent changes in sexual behavior have facilitated syphilis transmission among MSM in many industrialized nations.
Increases in high-risk sexual behavior among some MSM may be related to (1) diminished concerns about the risk of acquiring and transmitting HIV as a result of optimism regarding highly active antiretroviral therapy (and its recent availability in many industrialized nations), (2) beliefs inferred from partners’ physical appearance that they are unlikely to be infected with HIV, (3) use of nitrate inhalants and other drugs, and (4) an increased inclination to ignore messages promoting safe sex.10,52–59 One study focusing on MSM showed that use of methamphetamine, with and without the concomitant use of sildenafil (Viagra), increased the risk of acquisition of syphilis infection.60
In recent years, the Internet has emerged as an important venue for MSM to meet sexual partners.61,62 The Internet may facilitate MSM meeting sexual partners when they travel, which may in part explain the rapid dissemination of syphilis among MSM both within and outside the United States.63 Several studies have revealed an association among MSM between location of partners through the Internet and acquisition of syphilis.14,60,63,64 Transmission of syphilis from contact with anorectal chancres that are difficult to detect, inadequate medical screening for STDs, and increased susceptibility to infection with syphilis mediated by HIV coinfection may also be contributing to the increased incidence of syphilis among MSM.
Risk of HIV transmission is a particular concern in the current syphilis epidemic because infection with syphilis increases transmission of HIV 3- to 5-fold,1 and a high percentage of MSM who have been involved in recent outbreaks are coinfected with HIV.11,15,17,18,20 The impact of increases in syphilis rates among MSM on the incidence of HIV is unclear. Although the number of new HIV diagnoses among MSM reported from 29 states increased 17% between 1999 and 2002,65 the incidence of HIV (determined with the serologic testing algorithm for recent HIV seroconversion [STAHRS]) did not increase among MSM in 2 cities (Los Angeles and San Francisco) that reported outbreaks of syphilis during those years.66
However, additional research in Los Angeles County involving STAHRS revealed that the annual incidence of HIV infection among MSM with early syphilis (primary and secondary syphilis in combination with early latent syphilis) between January 2002 and April 2004 (26%) was higher than the rate of newly diagnosed HIV infection among MSM tested for HIV at publicly funded clinics in 2002 (4.1%).67 One possible explanation for why the current syphilis epidemic has not been accompanied by a definitive increase in HIV incidence among MSM is that some MSM, in an attempt to prevent acquisition or transmission of HIV, choose partners who have the same HIV infection status as they do.9,68 Another possibility is that risk of HIV transmission is reduced among infected individuals who are on antiretroviral therapy and have low or undetectable viral loads.69,70
Limitations
Limitations of this study include incomplete reporting of syphilis cases, variations in data collection and recording within and between STD control programs, and the absence of information about sexual orientation and gender of partners. In recent years, with the increasing rates of syphilis among MSM, incomplete reporting of cases has been a particular problem. One reason is that the number of cases detected through contact tracing has been low owing to high numbers of anonymous sexual partners,71 which might result in underreporting of cases among MSM. In addition, some cases occurring among MSM are not identified and reported.
Because syphilis elimination efforts in the United States were not directed toward MSM until increased rates had been identified, it is unlikely that a substantial proportion of the increase in syphilis cases among MSM can be explained by enhanced case detection resulting from syphilis elimination activities. Also, simultaneous outbreaks of syphilis among MSM in many industrialized countries argue against increased case ascertainment being the primary explanation for the increase in cases among MSM in the United States.
Because national case report data do not include information about partner gender, we relied on a model that estimated the annual number of cases occurring among MSM during 2000 through 2003 on the basis of increases in the syphilis MFCR between 1998 and 2003. These estimates must be interpreted with caution because MFCRs may be elevated for a variety of reasons in addition to increases in cases among MSM (e.g., increased case ascertainment among men relative to women and outbreaks involving transmission of syphilis between women who are commercial sex workers and men).
However, the model also underestimated the number of cases occurring among MSM because it conservatively assumed that no cases occurred among MSM in 1998. In 2005, CDC asked STD programs to begin including gender of sexual partners in all STD morbidity data reported through state and local health departments. The magnitude of our model’s underestimations cannot be quantified because CDC did not receive information about gender of partners during the study period with which to compare estimates from the model.
Conclusions
The rate of syphilis declined to a historic low in 2000. However, increasing syphilis cases among MSM have reversed the decade-long trend of declines in overall rates. We estimate that MSM accounted for more than 60% of reported syphilis cases in 2003. The primary challenges for syphilis elimination are to continue to reduce the incidence of syphilis in populations among whom efforts have been successful and to prevent and control syphilis among MSM. Interventions that have been relied on in previous epidemics, such as notification and treatment of partners, have not proved as effective in preventing syphilis among MSM.71,72
Local, state, and federal health officials and other partners are working together to develop, evaluate, and support new intervention strategies directed toward MSM that will be effective in reducing the incidence of syphilis. The updated National Syphilis Elimination Plan, published in 2006, included MSM among affected populations for whom specific interventions should be tailored. Key activities for controlling syphilis in MSM recommended in the 2006 syphilis elimination plan included (1) collecting and reporting data on the gender of sexual partners and the sexual preference of persons diagnosed with syphilis, (2) developing and using Internet-based interventions to engage MSM with syphilis and facilitate partner notification activities, (3) enhancing syphilis education and sexual health promotion with MSM within STD clinics and the community, (4) using provider outreach, education and mobilization to raise awareness of syphilis infection among MSM and improve the quality of clinical management, and (5) expanding access to syphilis screening for MSM at STD care facilities and in outreach settings.73 Raising awareness about the current syphilis epidemic and its implications for transmission and acquisition of HIV infection, promoting efforts to reduce high-risk sexual behaviors, and educating MSM to recognize symptoms and signs of syphilis and understand the importance of seeking medical care early in the course of infection may help minimize transmission of the disease.
Mobilizing the MSM community to take an active role in these efforts is crucial for their success. Training providers to improve their skills in diagnosing and treating syphilis, to screen sexually active MSM routinely for syphilis and other STDs, and to screen for STDs in conjunction with HIV counseling and testing is also critical for controlling syphilis among MSM.
Peer Reviewed
Contributors J. D. Heffelfinger originated the study, completed the analyses, and led the writing. E. B. Swint assisted with the study and analyses. S. M. Berman assisted in the conception and implementation of the study. H. S. Weinstock assisted in the conception of the study and supervised all aspects of its implementation. All of the authors contributed to conceptualizing ideas, interpreting findings, and reviewing drafts of the article.
Human Participant Protection No protocol approval was needed for this study.
References
- 1.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999; 75:3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fichtner RR, Aral SO, Blount JH, Zaidi AA, Reynolds GH, Darrow WW. Syphilis in the United States: 1967–1979. Sex Transm Dis. 1983;10:77–80. [DOI] [PubMed] [Google Scholar]
- 3.Sexually Transmitted Disease Surveillance 2002. Atlanta, Ga: Centers for Disease Control and Prevention; 2003.
- 4.Centers for Disease Control and Prevention. Primary and secondary syphilis—United States, 2002. MMWR Morb Mortal Wkly Rep. 2003;52:1117–1120. [PubMed] [Google Scholar]
- 5.Rolfs RT, Nakashima AK. Epidemiology of primary and secondary syphilis in the United States, 1981 through 1989. JAMA. 1990;264:1432–1437. [PubMed] [Google Scholar]
- 6.The National Plan to Eliminate Syphilis From the United States. Atlanta, Ga: National Center for HIV, STD, and TB Prevention, Centers for Disease Control and Prevention; 1999.
- 7.Healthy People 2010, With Understanding and Improving Health and Objectives for Improving Health. 2nd ed., 2 vols. Washington, DC: US Dept of Health and Human Services; 2000.
- 8.Ekstrand ML, Stall RD, Paul JP, Osmond DH, Coates TJ. Gay men report high rates of unprotected anal sex with partners of unknown or discordant HIV status. AIDS. 1999;13:1525–1533. [DOI] [PubMed] [Google Scholar]
- 9.Stall RD, Hays RB, Waldo CR, Ekstrand M, McFarland W. The gay ’90s: a review of research in the 1990s on sexual behavior and HIV risk among men who have sex with men. AIDS. 2000;14(suppl 3): S1–S14. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Increases in unsafe sex and rectal gonorrhea among men who have sex with men—San Francisco, California, 1994–1997. MMWR Morb Mortal Wkly Rep. 1999; 48:45–48. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Resurgent bacterial sexually transmitted disease among men who have sex with men—King County, Washington, 1997–1999. MMWR Morb Mortal Wkly Rep. 1999;48:773–777. [PubMed] [Google Scholar]
- 12.Williams LA, Klausner JD, Whittington WL, Handsfield HH, Celum C, Holmes KK. Elimination and reintroduction of primary and secondary syphilis. Am J Public Health. 1999;89:1093–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ciesielski C, Beiinger H. Emergence of primary and secondary syphilis among men who have sex with men in Chicago and relationship to HIV infection. In: Program and abstracts of the 7th Conference on Retroviruses and Opportunistic Infections, January–February 2000, Chicago, Ill. Abstract 470.
- 14.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284:447–449. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men—Southern California, 2000. MMWR Morb Mortal Wkly Rep. 2001;50:117–120. [PubMed] [Google Scholar]
- 16.Bronzan R, Echavarria L, Hermida J, Trepka M, Burns T, Fox K. Syphilis among men who have sex with men (MSM) in Miami-Dade County, Florida. In: Program and abstracts of the National STD Prevention Conference, March 2002, San Diego, Calif.
- 17.Centers for Disease Control and Prevention. Primary and secondary syphilis among men who have sex with men—New York City, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:853–856. [PubMed] [Google Scholar]
- 18.D’Souza G, Lee JH, Paffel JM. Outbreak of syphilis among men who have sex with men in Houston, Texas. Sex Transm Dis. 2003;30:872–873. [DOI] [PubMed] [Google Scholar]
- 19.Robinson BC, Chiliade PA, Lee C, Bautista J, Saenz G. Redirecting elimination efforts in response to the changing epidemiology of syphilis. In: Program and abstracts of the National STD Prevention Conference, March 2004, Philadelphia, Pa. Abstract 167.
- 20.Niccolai L, Jenkins H, Oyervides O, Lane P, Richardson W. Infectious syphilis in Connecticut: trends and epidemiologic characteristics. In: Program and abstracts of the National STD Prevention Conference, March 2004, Philadelphia, Pa. Abstract 171.
- 21.Stolte IG, Dukers NH, de Wit JB, Fennema JS, Coutinho RA. Increase in sexually transmitted infections among homosexual men in Amsterdam in relation to HAART. Sex Transm Infect. 2001;77:184–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halsos AM, Edgardh K. An outbreak of syphilis in Oslo. Int J STD AIDS. 2002;13:370–372. [DOI] [PubMed] [Google Scholar]
- 23.Giard M, Queyron PC, Ritter J, et al. The recent increase of syphilis cases in Lyon University hospitals is mainly observed in HIV-infected patients: descriptive data from a laboratory-based surveillance system. J Acquir Immune Defic Syndr. 2003;34:441–443. [DOI] [PubMed] [Google Scholar]
- 24.Couturier E, Michel A, Janier M, Dupin N, Semaille C, Syphilis Surveillance Network. Syphilis surveillance in France, 2000–2003. Euro Surveill. 2004; 9:7–8. [DOI] [PubMed] [Google Scholar]
- 25.Marcus U, Bremer V, Hamouda O. Syphilis surveillance and trends of the syphilis epidemic in Germany since the mid-90s. Euro Surveill. 2004;9:9–10. [PubMed] [Google Scholar]
- 26.Sasse A, Defraye A, Ducoffre G. Recent syphilis trends in Belgium and enhancement of STI surveillance systems. Euro Surveill. 2004;9:5–6. [DOI] [PubMed] [Google Scholar]
- 27.Fenton KA. A multilevel approach to understanding the resurgence and evolution of infectious syphilis in Western Europe. Euro Surveill. 2004;9:3–4. [DOI] [PubMed] [Google Scholar]
- 28.Van der Bij AK, Stolte IG, Coutinho RA, Dukers NH. Increase of sexually transmitted infections, but not HIV, among young homosexual men in Amsterdam: are STIs still reliable markers for HIV transmission? Sex Transm Infect. 2005;81:34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown AE, Sadler KE, Tomkins SE, et al. Recent trends in HIV and other STIs in the United Kingdom: data to the end of 2002. Sex Transm Infect. 2004;80: 159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hopkins S, Lyons F, Coleman C, Courtney G, Bergin C, Mulcahy F. Resurgence in infectious syphilis in Ireland: an epidemiological study. Sex Transm Dis. 2004;31:317–321. [DOI] [PubMed] [Google Scholar]
- 31.Macdonald N, Dougan S, McGarrigle CA, et al. Recent trends in diagnoses of HIV and other sexually transmitted infections in England and Wales among men who have sex with men. Sex Transm Infect. 2004; 80:492–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simms I, Fenton KA, Ashton M, et al. The re-emergence of syphilis in the United Kingdom: the new epidemic phases. Sex Transm Dis. 2005;32:220–226. [DOI] [PubMed] [Google Scholar]
- 33.Sexually Transmitted Disease Surveillance 1994. Atlanta, Ga: Centers for Disease Control and Prevention; 1995.
- 34.Sexually Transmitted Disease Surveillance 1999. Atlanta, Ga: Centers for Disease Control and Prevention; 2000.
- 35.Census of Population and Housing, 1990: Summary Tape File 1 (All States) [machine-readable file]. Washington, DC: US Census Bureau; 1991.
- 36.Nakashima AK, Rolfs RT, Flock ML, Kilmarx P, Greenspan JR. Epidemiology of syphilis in the United States, 1941–1993. Sex Transm Dis. 1996;23:16–23. [DOI] [PubMed] [Google Scholar]
- 37.Heffelfinger JD, Patel SM, Zaidi A, Weinstock HS. Validating a model that estimates the proportion of primary and secondary (P&S) syphilis cases occurring among men who have sex with men (MSM). In: Program and abstracts of the 43rd Infectious Diseases Society of America Conference, October 2005, San Francisco, Calif. Abstract 906.
- 38.Centers for Disease Control and Prevention. Outbreak of primary and secondary syphilis—Baltimore City, Maryland, 1995. MMWR Morb Mortal Wkly Rep. 1996;45:166–169. [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Outbreak of primary and secondary syphilis—Guilford County, North Carolina, 1996–1997. MMWR Morb Mortal Wkly Rep. 1998;47:1070–1073. [PubMed] [Google Scholar]
- 40.Estimates of the Population of Counties by Age, Sex and Race/Hispanic Origin: 1990 to 2000 [machine-readable file]. Washington, DC: US Census Bureau; 2000.
- 41.Centers for Disease Control and Prevention. Relationship of syphilis to drug use and prostitution—Connecticut and Philadelphia, Pennsylvania. MMWR Morb Mortal Wkly Rep. 1988;37:755–758, 764. [PubMed] [Google Scholar]
- 42.Rolfs RT, Goldberg M, Sharrar RG. Risk factors for syphilis: cocaine use and prostitution. Am J Public Health. 1990;80:853–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Alternative case-finding methods in a crack-related syphilis epidemic—Philadelphia. MMWR Morb Mortal Wkly Rep. 1991;40:77–81, 87. [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Current trends in primary and secondary syphilis—United States, 1981–1990. MMWR Morb Mortal Wkly Rep. 1991;40:314, 321–323. [PubMed] [Google Scholar]
- 45.Webster LA, Rolfs RT. Surveillance for primary and secondary syphilis—United States, 1991. MMWR Morb Mortal Wkly Rep. 1993;42(SS-3):13–19. [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. Epidemic early syphilis—Escambia County, Florida, 1987 and July 1989–June 1990. MMWR Morb Mortal Wkly Rep. 1991;40:323–325. [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. Epidemic early syphilis—Alabama, 1990–1991. MMWR Morb Mortal Wkly Rep. 1992;41:790–794. [PubMed] [Google Scholar]
- 48.Kandel DB, Davies M. Decline in the use of illicit drugs by high school students in New York State: a comparison with national data. Am J Public Health. 1991;81:1064–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Golub A, Johnson BD. A recent decline in cocaine use among youthful arrestees in Manhattan, 1987 through 1993. Am J Public Health. 1994;84: 1250–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sexually Transmitted Disease Surveillance, 1989. Atlanta, Ga: Centers for Disease Control and Prevention; 1990.
- 51.Sexually Transmitted Disease Surveillance 2001. Atlanta, Ga: Centers for Disease Control and Prevention; 2002.
- 52.Gold RS, Skinner MJ. Situational factors and thought processes associated with unprotected intercourse in young gay men. AIDS. 1992;6:1021–1030. [DOI] [PubMed] [Google Scholar]
- 53.Ekstrand ML, Stall RD, Paul JP, Osmond DH, Coates TJ. Gay men report high rates of unprotected anal sex with partners of unknown or discordant HIV status. AIDS. 1999;13:1525–1533. [DOI] [PubMed] [Google Scholar]
- 54.Ekstrand ML, Stall RD, Bein E, Coates TJ. HIV treatment optimism is associated with sexual risk taking among gay men in San Francisco. Paper presented at: 4th International Conference on Biopsychosocial Aspects of HIV Infection, July 1999, Ottawa, Ontario, Canada.
- 55.Waldo CR, McFarland W, Katz MH, MacKellar D, Valleroy LA. Very young gay and bisexual men are at risk for HIV infection: the San Francisco Bay Area Young Men’s Survey II. J Acquir Immune Defic Syndr. 2000;24:168–174. [DOI] [PubMed] [Google Scholar]
- 56.Ostrow DG, Fox K, Chmiel JS, et al. Attitudes toward highly active retroviral therapy predict sexual risk-taking among HIV-infected gay men in the Multicenter AIDS Cohort Study (MACS). In: Program and abstracts of the XIII International Conference on AIDS, July 2000, Durban, South Africa. Abstract THPeD5812.
- 57.Wolitski RJ, Validserri RO, Denning PH, Levine WC. Are we headed for a resurgence of the HIV epidemic among men who have sex with men? Am J Public Health. 2001;91:883–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mitchell SJ, Wong W, Kent CK, Chaw JK, Klausner JD. Methamphetamine use, sexual behavior, and sexually transmitted diseases among men who have sex with men seen in an STD clinic, San Francisco, 2000–2003. In: Program and abstracts of the National STD Prevention Conference, March 2004, Philadelphia, Pa. Abstract D04C.
- 59.Paz-Bailey G, Meyers A, Blank S, et al. A case-control study of syphilis among men who have sex with men in New York City: association with HIV infection. Sex Transm Dis. 2004;31:581–587. [DOI] [PubMed] [Google Scholar]
- 60.Wong W, Chaw JK, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sex Transm Dis. 2005;32:458–463. [DOI] [PubMed] [Google Scholar]
- 61.Kim AA, Kent C, McFarland W, Klausner JD. Cruising on the Internet highway. J Acquir Immune Defic Syndr. 2001;28:89–93. [DOI] [PubMed] [Google Scholar]
- 62.Mettey A, Crosby R, DiClemente RJ, Holtgrave DR. Associations between Internet sex seeking and STI associated risk behaviours among men who have sex with men. Sex Transm Infect. 2003;79:466–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention. Internet use and early syphilis infection among men who have sex with men—San Francisco, California, 1999–2003. MMWR Morb Mortal Wkly Rep. 2003;52: 1229–1232. [PubMed] [Google Scholar]
- 64.Taylor M, Aynalem G, Smith L, Bemis C, Kenney K, Kerndt P. Correlates of Internet use to meet sex partners among men who have sex with men diagnosed with early syphilis in Los Angeles County. Sex Transm Dis. 2004;31:552–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Centers for Disease Control and Prevention. Increases in HIV diagnoses—29 states, 1999–2002. MMWR Morb Mortal Wkly Rep. 2003;52:1145–1148. [PubMed] [Google Scholar]
- 66.Centers for Disease Control and Prevention. Trends in primary and secondary syphilis and HIV infections in men who have sex with men—San Francisco and Los Angeles, California, 1998—2002. MMWR Morb Mortal Wkly Rep. 2004;53:575–578. [PMC free article] [PubMed] [Google Scholar]
- 67.Taylor MM, Hawkins K, Gonzalez A, et al. Use of the serologic testing algorithm for recent HIV seroconversion (STARHS) to identify recently acquired HIV infections in men with early syphilis in Los Angeles County. J Acquir Immune Defic Syndr. 2005;38: 505–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Parsons JT, Schrimshaw EW, Wolitski RJ, et al. Sexual harm reduction practices of HIV-seropositive gay and bisexual men: serosorting, strategic positioning, and withdrawal before ejaculation. AIDS. 2005; 19:S13–S25. [DOI] [PubMed] [Google Scholar]
- 69.Quinn TC, Wawer MJ, Sewankambo N, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. N Engl J Med. 2000;342: 921–929. [DOI] [PubMed] [Google Scholar]
- 70.Porco TC, Martin JN, Page-Shafer KA, et al. Decline in HIV infectivity following the introduction of highly active antiretroviral therapy. AIDS. 2004;18: 81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gorbach PM, Aral SO, Celum C, et al. To notify or not to notify: STD patients’ perspectives of partner notification in Seattle. Sex Transm Dis. 2000;27: 193–200. [DOI] [PubMed] [Google Scholar]
- 72.Gunn RA, Maroufi A, Peterman TA. Syphilis among men who have sex with men: limitations of traditional case and partner services, San Diego County, CA. In: Program and abstracts of the National STD Prevention Conference, March 2004, Philadelphia, Pa.
- 73.Together we can. The National Plan to Eliminate Syphilis from the United States. Atlanta, Ga: Centers for Disease Control and Prevention; 2006.


