Abstract
Background
The social inequalities in health have endured or even worsened comparatively throughout different social groups since the 1990s. Our objective was to identify the individual characteristics (socio-economic status, living conditions, individuals’ social integration, health beliefs, expectations and representation, and psychological characteristics) statistically associated with the fact of stating (or not) that healthcare had been forgone because of cost.
Methods
In this cross-sectional, multi-centre study we randomly selected a study sample from five underprivileged areas in the Paris region. A multiple logistic regression model was used to calculate the odds ratios (OR) and 95% CI. The validity of the model was assessed by goodness-of-fit tests (Pearson and deviance) and by the study of 100 bootstrap samples.
Results
After making adjustments for numerous individual socio-economic and health characteristics, we observed a higher occurrence of reported forgone healthcare among people who have had financial worries during adulthood (ORyes/no = 5.47 [1.44–20.75]), a life-course experience of physical, sexual or psychological abuse (ORyes/no = 2.86 [1.40–5.84]); who have experienced childhood difficulties (OR1/never difficulties = 5.28 [1.81–15.39], OR2–4/never = 7.62 [2.69–21.57], OR>4/never = 8.57 [2.39–30.80]); who have expressed a low degree of sickness orientation ORlows/high = 2.62 [1.33–5.14]), a high worry/concern about health (ORhigh/low = 2.71 [1.33–5.50]) and a low self-esteem (ORmedium/high = 8.28 [1.44–47.64], ORlow/high = 16.44 [2.81–96.24]).
Conclusion
Aside from purely financial hurdles, other factors play a role in the non-use of healthcare services. Health policies mainly promoting equal financial access to healthcare have little chance of abating health inequalities.
Keywords: Adolescent, Adult, Aged, Attitude to Health, Cross-Sectional Studies, Female, France, Health Expenditures, Health Services Accessibility, Health Services Needs and Demand, Humans, Male, Mental Health, Middle Aged, Poverty Areas, Socioeconomic Factors, Treatment Refusal, psychology
Key-points
In France, despite a universal health insurance system, a substantial share of the population repeatedly states that they have forgone healthcare because they could not afford it.
We aimed to identify individual characteristics associated with the fact of stating (or not) that healthcare has been forgone because of cost.
Our results shows that forgoing healthcare because of cost is associated with lifestyle, social integration, social disruption, and psychological characteristics.
Universal health insurance and fewer financial hurdles to healthcare are necessary but not sufficient requisites for achieving an equitable healthcare system.
Introduction
It has been established that the social conditions of an individual’s life affect his or her health. In most industrialised countries, numerous studies have identified the existence of a link between individuals’ health and their socio-economic situation.1–3 Despite ongoing biomedical and technological advances over the past fifty years, the social inequalities in health have endured or even worsened comparatively throughout different social groups since the 1990s.4 Merely describing the inequalities will not abate them. Importantly, they should be explained to gain a deeper insight into their underlying mechanisms. Most of the current research mainly addresses individuals’ socio-economic characteristics (income, occupational status, socio-economic group, educational level, composition of the family, type of housing, and so on)5–8 and socio-demographic characteristics (gender, age, race and/or migration status).9 The studies seldom explore the individual characteristics of integration and social disruptions (social support and social capital, personal disruptions during childhood or adulthood)10–14 although a growing number of authors underscore the value of studying new determinants.15–17 Some sociological and psychological study findings also highlight that considering characteristics such as self-esteem,18,19 sense of coherence,20,21 and self-efficacy22,23 (called ‘psychological’ characteristics in this paper although they also refer to social processes)24 would be of some avail. Finally, many studies of health-belief models25 show how health beliefs, expectations and perceptions differ from one social group to the next on the one hand, and how health beliefs have a decisive impact on health behaviours and the recourse to healthcare, on the other. Studies combining the different approaches for assessing the relative impact of the manifold determinants (socio-economic situation, living conditions, social integration, psychological characteristics, health beliefs and perceptions) and explaining the observed social differences in health outcomes (including the recourse to healthcare) are few in population-based studies.16,26 And though France may seem emblematic in this area, such studies are singularly non-existent in France. For instance, France – a country where access to medical and surgical care is affordable for everyone - shows one of highest inequalities in mortality by occupational class in Western Europe.4,27,28 In 2000, French public healthcare insurance was broadened to become the Couverture maladie universelle. The new system provides basic health insurance for everyone and free complementary insurance for the destitute. However, representative annual surveys of healthcare consumption show that a substantial share of the population states that, “they have forgone healthcare because they could not afford it.” In 2000, nearly 24% of the respondents stated that they had forgone healthcare because they could not afford it at least once in their lifetime, and 15% stated they had done so in the year preceding the survey. The proportions vary substantially depending on age, gender and household size but also on income levels, occupational status and welfare coverage (with or without complementary health insurance supplementing basic national health coverage).29 The proportions, which are constant over time (despite the gradual extension of the French national healthcare insurance), show that the mandatory, public French health insurance scheme (e.g. for dental care) does not enable people to clear the financial hurdles in full. This may also suggest that factors – i.e., the above-mentioned hurdles – other than purely financial hurdles underlie the statement (and perception) that healthcare has been forgone because of cost.
Accordingly, the purpose of our population-based study in some underprivileged areas in the Paris region was to identify the individual characteristics statistically associated with the fact of stating (or not) that healthcare had been forgone because of cost. We did so by studying socio-economic status and living conditions concurrently, as is usual, as well as the individuals’ social integration, health beliefs, expectations and representation, and some of their psychological characteristics.
Material and methods
Our study population was randomly selected from the general population living in five underprivileged areas. These areas are 5 of the 157 Zones urbaines sensibles, i.e., areas that French urban policy in Ile-de-France region has designated as sensitive urban areas based on 3 main criteria (ratio of inhabitants under 25 years of age, ratio of long-term unemployed people, and ratio of foreigners).30 We randomly selected households from the population and then randomly chose 1 individual (18 to 75 years old) per household to put together a sample of 525 individuals from a total population of 50,000. Every non-respondent was replaced by another individual randomly selected in the same way. All told, 836 households were contacted since 27% of the eligible respondents refused to answer, 8% did not speak French and 2% could not answer for health reasons. Seven persons were not included in our analysis because they did not answer the question about forgone healthcare. We ended up with an analysed sample of 518 people.
Our questionnaire including both factual and subjective questions was administered to the respondents during face-to-face interviews at home. Demographic information included age, gender, nationality (current and at birth), and respondent’s intra-national and international migration history. Socio-economic variables included household size and structure; level of education; socio-economic group coded into low (working class, unskilled employees), medium (skilled employees, technicians) or high (engineers, senior executives, company managers); occupational status (employees with a work contract, the unemployed with and without unemployment benefits, and other people); monthly income per household unit (HU);31 financial worries during adulthood, and health insurance status.
For self-reported health, we defined a ‘chronic disease status’, i.e., people were asked whether they suffered (at the time of the interview) from any of the chronic diseases on a 33-item list,32 and then further dichotomised as ‘yes’ (at least one positive answer) or ‘no’.
Social integration and social disruption variables included participation in social activities, religious affiliation and practices, feeling of loneliness, feeling of exclusion, experiences of discrimination, perceived stress, life-course experience of physical, sexual or psychological abuse, number of striking events during childhood and adulthood. The question on the feeling of isolation was graded according to a 10-point scale ranging from 1 (feeling of complete loneliness) to 10 (presence of many supportive people) and then dichotomised as ‘high’ (<5) versus ‘low’ (>= 5). Questions on striking events during childhood and adulthood were taken from a list of 20 and 12 items, respectively.33 For our analysis, we retained respondents’ money troubles, parents’ disputes, run-ins with the law, family alcoholism, or serious relational problems with the family occurring before the age of 18; and run-ins with the law, heavy debts, children in institutions, alcohol or drug problems, or serious marital fights occurring after the age of 18.
Health perceptions included 5 items from the French translation of one question per subscale from the 33 statements in the Health Perceptions Questionnaire.34 The question on resistance to illness was scored by the level of agreement with the following statement, “I seem to get sick a little easier than other people”; the question on prior health by, “I was so sick once that I thought I might die”; the question on health worry/concern by, “I worry about my health less than other people worry about their health” and by, “My health is a concern in my life"; and sickness orientation by, “I don’t accept that sometimes I’m just going to be sick". All these items were further dichotomised as ‘yes’ (strongly agree and agree) or ‘no’ (strongly disagree and disagree). The question on the person’s health outlook was assessed by, “In the future, I expect to have better health”; and dichotomised as ‘yes’ (strongly agree) or ‘no’ (agree, strongly disagree or disagree).
Finally, people were questioned about three psychological characteristics: self-efficacy, self-esteem, and sense of coherence. We scored self-efficacy by adding up the points matching the level of agreement with the 2 following statements taken from the Schwarzer General Self-efficacy Scale,35 “I can solve most problems if I invest the necessary effort” and “If I am in trouble, I can usually think of a solution”. The score was dichotomised as ‘low’ or ‘high’. Similarly, we scored self-esteem based on responses to the following statements taken from the Rosenberg Scale,18 “On the whole, I’m satisfied with myself”, “I feel that I have a number of good qualities”, “I am able to do things as well as most other people”, “I certainly feel useless at times” and “I feel I do not have much to be proud of”. The score was then broken down into ‘high’, ‘medium’ or ‘low’. Third, two questions were used for determining a sense of coherence36 additive score. They were, “Do you usually feel that your daily life is a source of personal satisfaction?” and “Do you usually feel that the things that happen to you in your daily life are hard to understand?” The score was broken down into ‘high’, ‘medium’, or ‘low’.
Throughout our analysis, our outcome variable is the response (yes/no) to the question: “During your life, have you ever forgone healthcare because you could not afford it?”, a question usually asked in the annual health consumption surveys conducted in France.29
We started by using logistic regression models to select potential covariates for forgone healthcare, after making adjustments for age, gender, household size, chronic disease status, health insurance status, income level, and occupation. We then included all the variables showing an univariate (adjusted) association with our dependant variable with a p value < 0.25 in the final multivariable regression model, and then we backward selected them. Decisions concerning potential covariates for the model (p <0.05) were based on the Hosmer and Lemeshow approach.37
We calculated the generalised coefficient of determination (R2) to assess the proportion of variance explained by the final model. We also calculated the Pearson chi-square (Χ2pearson) test statistic (for a correctly specified model, the test divided by its degrees of freedom should be equal to 1).37 To identify which observations did not fit the model, we calculated the degree to which the model increased when we withdrew individuals one after the other. Using this method, we were able to detect how many individuals (and with which characteristics) did contribute heavily to a disagreement between the observed data and the predicted values of the final fitted model.37 Furthermore, the area under the receiver operating characteristic curve (AUC) was calculated to provide an additional, more easily interpretable criterion of our modelassessment]. Finally, we assessed the stability of our model by studying 100 bootstrap samples from our study population. Each sample was the same size as the population under study.38 We did a backward selection of our covariates using logistic regression models fitted to each sample (adjusted systematically to the same 7 variables as above). We also calculated the frequency with which each co-variable was retained in the final 100 regression analysis.
Results
The breakdown of the study population was 44.2% men and 55.8% women; average age is at 36.7. In the study population, 51.3% were employed, 7.7% were unemployed welfare-recipients, 6.4% were unemployed non-welfare recipients, and 34.6% were in another situation (mainly students, retired workers, or female homemakers). The average monthly income was ¤624/HU: 42% were below the French poverty threshold (¤550/HU). Most of them (84.2%) had always had health insurance, 13.1% had health coverage at the time of the interview but stated not having any at least once in the past, and 2.7% had never been insured. At the time of interview, 39.4% stated they suffered from one or more chronic diseases. Finally, 13.7% reported having forgone healthcare because it was unaffordable (half of this number stated that the healthcare was for an emergency).
Table 1 shows a logistic regression model between our outcome variable and the usual socioeconomic factors observed in the general French population. Table 2 shows the association between our outcome and each of the studied covariables after they were adjusted to the variables in Table 1. Associations are significant with some lifestyle characteristics, some integration and disruption characteristics, some health perceptions, and some psychological characteristics.
Table 1.
Association of usual socioeconomic factors with forgone healthcare because of cost (multiple logistic regression)
| OR (95% CI) | p | |
|---|---|---|
| Gender | 0.14 | |
| Female | 1.00 (ref.) | |
| Male | 0.66 (0.67–1.15) | |
| Age (years) | 0.98 | |
| 18–24 | 1.00 (ref.) | |
| 25–34 | 0.97 (0.43–2.18) | |
| 35–54 | 1.02 (0.48–2.18) | |
| ≥ 55 | 0.85 (0.33–2.18) | |
| Household size | 0.04 | |
| ≥ 3 | 1.00 (ref.) | |
| 2–3 | 2.07 (1.10–3.91) | |
| Lives alone | 2.57 (0.93–7.10) | |
| Has a chronic disease | <10−3 | |
| No | 1.00 (ref.) | |
| Yes | 2.62 (1.52–4.53) | |
| Health insurance (HI) status | <10−2 | |
| Has always had HI | 1.00 (ref.) | |
| Has HI but didn’t have any at least once in the past | 1.43 (0.68–3.02) | |
| Has never had HI | 6.77 (1.98–23.16) | |
| Monthly income per household unit | <10−2 | |
| > €550 | 1.00 (ref.) | |
| ≤ €550 | 2.62 (1.41–4.85) | |
| Occupation | 0.03 | |
| Work contract | 1.00 (ref.) | |
| Unemployed (welfare-recipient) | 2.53 (1.13–5.66) | |
| Unemployed (non-welfare recipient) | 0.38 (0.10–1.38) | |
| Other | 0.81 (0.41–1.61) |
Table 2.
Variables associated with foregone healthcare because of cost
| OR (95% CI)a | p | |
|---|---|---|
| Lifestyle characteristics | ||
| Socioeconomic group | 0.24 | |
| Low | 1.00 (ref.) | |
| Medium | 0.85 (0.38–1.90) | |
| High | 0.72 (0.17–3.12) | |
| No socioeconomic group / missing | 0.23 (0.05–0.94) | |
| Has had financial worries in adulthood | <10−2 | |
| Never | 1.00 (ref.) | |
| At least once | 7.30 (2.11–25.23) | |
| Living with a child | 0.46 | |
| No | 1.00 (ref.) | |
| Yes | 0.78 (0.40–1.51) | |
| Has always lived in France | <10−2 | |
| Yes | 1.00 (ref.) | |
| No | 2.25 (1.23–4.12) | |
| Level of Education | 0.49 | |
| Primary | 1.00 (ref.) | |
| Lower secondary | 1.83 (0.68–4.89) | |
| Upper secondary | 2.09 (0.81–5.43) | |
| University | 2.47 (0.88–6.92) | |
| Student | 2.66 (0.68–10.45) | |
| Social integration and disruptions | OR (95% CI)a | p |
| Belongs to social community group(s) | 0.15 | |
| Yes | 1.00 (ref.) | |
| No | 1.57 (0.86–2.88) | |
| Religious affiliation | <10−2 | |
| Yes | 1.00 (ref.) | |
| No | 2.44 (1.34–4.44) | |
| Victim of discrimination | 0.01 | |
| No | 1.00 (ref.) | |
| Yes | 2.10 (1.19–3.7) | |
| Feeling of loneliness | 0.07 | |
| No | 1.00 (ref.) | |
| Yes | 1.89 (0.95–3.77) | |
| Feeling of exclusion | <10−2 | |
| No | 1.00 (ref.) | |
| Yes | 2.77 (1.23–5.93) | |
| Perceived stress | 0.04 | |
| Low | 1.00 (ref.) | |
| High | 1.89 (1.02–3.12) | |
| Life-course experience of physical, sexual or psychological abuse | <10−4 | |
| No | 1.00 (ref.) | |
| Yes | 4.99 (2.81–8.88) | |
| Number of striking events during childhood | <10−4 | |
| 0 | 1.00 (ref.) | |
| 1 | 5.49 (1.97–15.28) | |
| 2–4 | 10.71 (4.02–25.52) | |
| ≥5 | 25.81 (8.06–85.63) | |
| Number of striking events during adulthood | <10−2 | |
| 0 | 1.00 (ref.) | |
| 1 | 2.64 (1.42–4.91) | |
| ≥2 | 3.25 (1.45–7.28) | |
| Health perceptions | ||
| Seems to get sick a little easier than other people (resistance to illness) | <10−2 | |
| No | 1.00 (ref.) | |
| Yes | 2.88 (1.34–6.20) | |
| In the future, expects to have better health than other people (health outlook) | 0.04 | |
| No | 1.00 (ref.) | |
| Yes | 2.35 (1.04–5.30) | |
| Was so sick once he/she thought he/she might die (prior health) | 0.08 | |
| No | 1.00 (ref.) | |
| Yes | 1.58 (0.93–3.31) | |
| Worries about his/her health less than other people do (health worry/concern) | <10−2 | |
| No | 1.00 (ref.) | |
| Yes | 2.12 (1.22–3.69) | |
| Doesn’t accept that sometimes he/she is just going to be sick (sickness orientation) | <10−2 | |
| No | 1.00 (ref.) | |
| Yes | 2.23 (1.31–3.80) | |
| Her/his health is a concern in her/his life (health worry/concern) | 0.04 | |
| No | 1.00 (ref.) | |
| Yes | 1.78 (1.03–3.03) | |
| Psychological characteristics | ||
| Perceived self-efficacy | 0.81 | |
| High | 1.00 (ref.) | |
| Low | 0.90 (0.37–2.19) | |
| Perceived self-esteem | <10−3 | |
| High | 1.00 (ref.) | |
| Medium | 7.32 (1.32–39.81) | |
| Low | 16.00 (2.91–88.00) | |
| Perceived sense of coherence | <10−3 | |
| High | 1.00 (ref.) | |
| Medium | 1.61 (0.70–3.70) | |
| Low | 3.72 (1.77–7.81) | |
adjusted to age, gender, income level, household size, chronic disease status, health insurance status and occupation
Figure 1 presents the result of the multivariable analysis. Among the adjustment variables, only the income level was associated with our outcome (OR<€550/>€550 = 2.58 [1.23–5.43]). Our final model retained 6 individual variables statistically associated with our outcome. The variables were financial worries during adulthood, life-course experience of physical, sexual or psychological abuse, the number of striking events during childhood (with a dose-effect relationship), the sickness orientation, health worry/concern and finally one psychological characteristic (self-esteem). For this final model, R2 was equal to 0.23. This figure is much higher than the R2 computed for the model containing only adjustment variables (Table 1), which was 0.08. For the final model, the AUC was equal to 0.84 (which expresses a very good discrimination), 73.4% of our study population was well predicted by our model and Χ2pearson was equal to 1.00. Figure 1 shows that very few individuals contributed heavily to a disagreement between the observed data and the predicted values of the final fitted model. In our 100 bootstrap samples, the 6 variables in our final model showed a frequency higher than 70% among the first seven that were the most frequently selected in the models. The 7 variables were in order of decreasing frequency: sickness orientation (96%), life-course experience of physical, sexual or psychological abuse (94%), number of striking events during childhood (93%), self-esteem (86%), lifelong residents of France (82%), health concern (81%), and financial worries during adulthood (70%).
Figure 1.
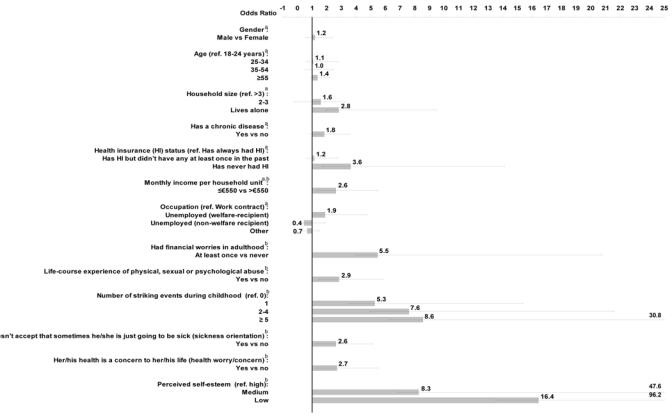
Factors associated with forgone healthcare because of cost (multiple logistic regression)
a adjustment variables, b significant variables
Discussion
Our results suggest that, at least in underprivileged areas in Paris region, forgoing healthcare because of cost is associated with lifestyle, social integration, social disruption characteristics, and psychological characteristics as well. After making adjustments for many individual demographic, health, and socio-economic characteristics, we found that the occurrence of reported forgone healthcare is higher among people who have had financial worries in adulthood, who have had a life course experience of physical, sexual or psychological abuse, who have experienced childhood difficulties, and who express a low degree of sickness orientation, a low self-esteem and/or a high worry/concern about health.
This study has four main limitations. First, our sample size was quite small, but our final model seems to be adequately fitted and robust, as shown by our complementary bootstrap analysis. Second, our random sample is only representative of the 5 areas where the study was conducted and further studies are needed to estimate the role of psychological characteristics in the general (and more socially mixed) population. Third, non-French speakers could not be interviewed due to a lack of translators. So, a small proportion of the study population was not included. Finally, our multivariable model explains only a limited fraction of the variance (R2=0.23), but this limitation is not uncommon when modelling social and behavioural variables.39,40
Our outcome variable – forgoing healthcare because it is unaffordable – is a standard question in the annual health consumption studies in France.29 When there is only one question on this subject, respondents’ answer is very global encompassing both temporality (since the question pertained to the whole life course of the individuals, we adjusted our model to the respondents’ ages) and meaning. Indeed, we did not have any data on the detailed occasions when healthcare was forgone (e.g. medications, dental care, medical consultations, etc.). We only knew that 50% of the respondents felt that the care they had forgone was for an emergency”. Actually, the question on forgoing healthcare because of cost may measure more than a mere perceived financial hurdle. It may also assess a feeling of frustration stemming from the medical care the individuals would like to receive and the care they actually get. Accordingly, among people with similar incomes and health statuses, some think they have forgone healthcare and others do not, depending on their level of expectation of care and treatments.
Indeed, our results show that perceptions of financial worries seem to have a greater impact (ORfinancial worries/never = 5.47[1.44–20.75]) than income level. Thus, our study reveals that beyond the objective socio-economic gradient (income), it is important to consider the perceived socio-economic gradient. Furthermore, people who can’t stand illness, albeit benign, stated more often than others that they forgo healthcare because of cost. One would assume that these people’s sickness orientation incurs behaviours of (high) healthcare consumption. Once could further assume that, with the same income and health coverage, they would be more likely to experience frustration (as per the above-mentioned meaning we ascribed to the studied outcome).
The observed association between forgone healthcare and self-esteem may be interpreted in several different ways. One the one hand, the loss of self-esteem may be associated with a disregard for one’s own welfare in general and hence a neglect to devote any resources (including funds) to medical care. On the other hand, the loss of self-esteem may bring on other cognitive disorders, apathy or even depressive disorders, and a deterioration of mental health,41 hence an increased feeling of a need for healthcare concurrent with a certain ‘inertia’ that might be expressed – or reinterpreted – as forgoing healthcare because of cost. Lastly, the association may also work in reverse, i.e., forgoing healthcare because it is unaffordable may be a significant stage (the impossibility of coping with certain basic needs) for an individual in his/her process of social precariousness or even social disaffiliation; a stage that entails a loss of self-esteem.42,43
As for the descriptions found in the literature, our results show that a broader approach to health determinants may be particularly useful for a better understanding of the social inequalities of healthcare observed in industrialised countries, including in the Western Europe countries, which provide their populations with universal health coverage. Following other authors, our results suggest that the observed socio-economic gradients in healthcare utilisation are more the results than the causes of other social inequalities in health. Although our study (because of its both observational and cross sectional design) does not allow us to conclude in terms of causality, it does suggest that events during childhood and life-course experiences as well as health beliefs and expectations (which are also socially constructed and determined) may be among the many causal pathways for the gradients observed.44
From the standpoint of both public health and health policies, our results show that universal health insurance and fewer financial hurdles to healthcare are necessary but not sufficient requisites for achieving an equitable healthcare system.45–48 Our results expressly suggest that health is a concern that varies according to the social group and that it does so to a greater extent than usually expected and considered by health policy decision-makers and health professionals. Consequently, health policies mainly promoting equal financial access to healthcare have little chance of abating health inequalities if they are not supplemented by programmes (e.g. outreach care services) and discretionary local policies tailored to the needs of those with poor health concern.
Acknowledgments
This study was supported by grants from the ‘Avenir’ program of the French National Institute of Health and Medical Research. It was based on a survey funded by the French National Observatory of Poverty and Social Exclusion.
References
- 1.Whitehead M, Townsend P, Davidson N, Davidsen N, editors. Inequalities in Health: Black Report. London: Penguin Books; 1992. [Google Scholar]
- 2.Davey Smith G, editor. Health inequalities. Bristol: The Policy Press; 2003. [Google Scholar]
- 3.Leclerc A, Fassin D, Grandjean H, Kaminski M, Lang T, editors. Les inégalités sociales de santé. Paris: La Découverte; 2000. [Google Scholar]
- 4.Mackenbach JP, Kunst AE, Cavelaars AE, Groenhof F, Geurts JJ. Socioeconomic inequalities in morbidity and mortality in western Europe. The EU Working Group on Socioeconomic Inequalities in Health. Lancet. 1997;349:1655–9. doi: 10.1016/s0140-6736(96)07226-1. [DOI] [PubMed] [Google Scholar]
- 5.Houweling TA, Kunst AE, Mackenbach JP. World Health Report 2000: inequality index and socioeconomic inequalities in mortality. Lancet. 2001;357:1671–2. doi: 10.1016/S0140-6736(00)04829-7. [DOI] [PubMed] [Google Scholar]
- 6.Bartley M, Owen C. Relation between socioeconomic status, employment, and health during economic change, 1973–93. BMJ. 1996;313:445–9. doi: 10.1136/bmj.313.7055.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn JR. Housing and inequalities in health: a study of socioeconomic dimensions of housing and self reported health from a survey of Vancouver residents. J Epidemiol Community Health. 2002;56:671–81. doi: 10.1136/jech.56.9.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92:758–68. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper H. Investigating socio-economic explanations for gender and ethnic inequalities in health. Soc Sci Med. 2002;54:693–706. doi: 10.1016/s0277-9536(01)00118-6. [DOI] [PubMed] [Google Scholar]
- 10.Berkman L, Glass T. Social networks as predictors of ischemic heart disease, cancer, stroke and hypertension: incidence, survival and mortality. In: Berkman L, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 137–173. [Google Scholar]
- 11.Vogt TM, Mullooly JP, Ernst D, Pope CR, Hollis JF. Social networks as predictors of ischemic heart disease, cancer, stroke and hypertension: incidence, survival and mortality. J Clin Epidemiol. 1992;45:659–66. doi: 10.1016/0895-4356(92)90138-d. [DOI] [PubMed] [Google Scholar]
- 12.Franks P, Campbell TL, Shields CG. Social relationships and health: the relative roles of family functioning and social support. Soc Sci Med. 1992;34:779–88. doi: 10.1016/0277-9536(92)90365-w. [DOI] [PubMed] [Google Scholar]
- 13.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol. 2002;155:507–15. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- 14.Marmot MG, Bosma H, Hemingway H, Brunner E, Stansfeld S. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350:235–9. doi: 10.1016/s0140-6736(97)04244-x. [DOI] [PubMed] [Google Scholar]
- 15.Krieger N. Commentary: Society, biology and the logic of social epidemiology. Int J Epidemiol. 2001;30:44–6. doi: 10.1093/ije/30.1.44. [DOI] [PubMed] [Google Scholar]
- 16.Marmot M, Ryff CD, Bumpass LL, Shipley M, Marks NF. Social inequalities in health: next questions and converging evidence. Soc Sci Med. 1997;44:901–10. doi: 10.1016/s0277-9536(96)00194-3. [DOI] [PubMed] [Google Scholar]
- 17.Macdonald K. Commentary: Social epidemiology. A way? Int J Epidemiol. 2002;30:46–47. doi: 10.1093/ije/30.1.46. [DOI] [PubMed] [Google Scholar]
- 18.Rosenberg M. Society and the Adolescent Self-Image. New Jersey: Princeton University Press; 1965. [Google Scholar]
- 19.Blascovich J, Tomaka J. Measures of self-esteem. In: Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of personality and social psychological attitudes. Ann Arbor: Institute for Social Research; 1993. pp. 115–160. [Google Scholar]
- 20.Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993;36:725–33. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- 21.Lundberg O. Childhood conditions, sense of coherence, social class and adult ill health: exploring their theoretical and empirical relations. Soc Sci Med. 1997;44:821–31. doi: 10.1016/s0277-9536(96)00184-0. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Self-efficacy: toward a unifying theory of behavioural change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 23.Schwarzer R, Fuchs R. Self-efficacy and health behaviour. In: Conner M, Norman P, editors. Predicting health behaviour: Research and practice with social cognition models. Buckingham: Open University Health; 1996. pp. 163–196. [Google Scholar]
- 24.Martikainen P, Bartley M, Lahelma E. Psychosocial determinants of health in social epidemiology. Int J Epidemiol. 2002;31:1091–3. doi: 10.1093/ije/31.6.1091. [DOI] [PubMed] [Google Scholar]
- 25.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 26.Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health. No easy solution JAMA. 1993;269:3140–5. [PubMed] [Google Scholar]
- 27.Kunst AE, Mackenbach JP. International variation in the size of mortality differences associated with occupational status. Int J Epidemiol. 1994;23:742–50. doi: 10.1093/ije/23.4.742. [DOI] [PubMed] [Google Scholar]
- 28.Marmot M, Bobak M. International comparators and poverty and health in Europe. BMJ. 2000;321:1124–8. doi: 10.1136/bmj.321.7269.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Auvray L, Dumesnil S, Le Fur P. Renoncement à des soins pour motifs financiers. In: Auvray L, Dumesnil S, Le Fur P, editors. Santé, soins et protection sociale en 2000. Paris: CREDES; 2001. pp. 147–153. [Google Scholar]
- 30.Estebe P. Instruments et fondements de la géographie prioritaire de la politique de la ville (1982–1996) Rev Fr Aff Soc. 2001;3:2–13. [Google Scholar]
- 31.Principles and Recommendations for Population and Housing Censuses, revision 1. New York: United Nations; 1998. [Google Scholar]
- 32.Auvray L, Dumesnil S, Le Fur P. Les maladies et les troubles de santé déclarés en 2000. In: Auvray L, Dumesnil S, Le Fur P, editors. Santé, soins, et protection sociale en 2000. Paris: CREDES; 2001. pp. 49–86. [Google Scholar]
- 33.Menahem G, Bantman P. Evenements de la jeunesse, trajectoires de vie et troubles de l'existence à l'âge adulte. In: Bouchayer F, editor. Trajectoires sociales et inégalités : Recherches sur les conditions de vie. Ramonville Saint-Agne: Erès; 1994. pp. 65–90. [Google Scholar]
- 34.Ware JE. The Health Perceptions Questionnaire. In: McDowell I, Newell C, editors. Measuring Health. Oxford: Oxford University press; 1976. pp. 219–225. [Google Scholar]
- 35.Schwarzer R. Self-efficacy: Through control of action. Washington: Hemisphere; 1992. [Google Scholar]
- 36.Lundberg O, Nyström-Peck M. A simplified way of measuring sense of coherence. Eur J Public Health. 1995;5:56–59. [Google Scholar]
- 37.Hosmer D, Lemeshow S. Applied logistic regression. New York: Wiley Interscience; 1990. [Google Scholar]
- 38.Efron B, Tibshirani R. An introduction to the bootstrap. New York: Chapman and Hall; 1993. [Google Scholar]
- 39.Mechanic D. Correlates of physician utilization: why do major multivariate studies of physician utilization find trivial psychosocial and organization effects? J Health Soc Behav. 1979;20:387–396. [PubMed] [Google Scholar]
- 40.Monge-Rojas R, Nunez HP, Garita C, Chen-Mok M. Psychosocial aspects of Costa Rican adolescents' eating and physical activity patterns. J Adolesc Health. 2002;31:212–9. doi: 10.1016/s1054-139x(02)00376-2. [DOI] [PubMed] [Google Scholar]
- 41.Schroevers MJ, Ranchor AV, Sanderman R. The role of social support and self-esteem in the presence and course of depressive symptoms: a comparison of cancer patients and individuals from the general population. Soc Sci Med. 2003;57:375–85. doi: 10.1016/s0277-9536(02)00366-0. [DOI] [PubMed] [Google Scholar]
- 42.Bartley M. Unemployment and ill health: understanding the relationship. J Epidemiol Community Health. 1994;48:333–7. doi: 10.1136/jech.48.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siegrist J. Place, social exchange and health: proposed sociological framework. Soc Sci Med. 2000;51:1283–93. doi: 10.1016/s0277-9536(00)00092-7. [DOI] [PubMed] [Google Scholar]
- 44.Wadsworth ME. Health inequalities in the life course perspective. Soc Sci Med. 1997;44:859–69. doi: 10.1016/s0277-9536(96)00187-6. [DOI] [PubMed] [Google Scholar]
- 45.Calman KC. Equity, poverty and health for all. BMJ. 1997;314:1187–91. doi: 10.1136/bmj.314.7088.1187a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bloom G, McIntyre D. Towards equity in health in an unequal society. Soc Sci Med. 1998;47:1529–38. doi: 10.1016/s0277-9536(98)00233-0. [DOI] [PubMed] [Google Scholar]
- 47.Andrulis DP. Access to care is the centrepiece in the elimination of socioeconomic disparities in health. Ann Intern Med. 1998;129:412–6. doi: 10.7326/0003-4819-129-5-199809010-00012. [DOI] [PubMed] [Google Scholar]
- 48.Navarro V. Health and Equity in the World in the Era of Globalization. In: Navarro V, editor. The political economy of social inequalities: Consequences for Health and Quality of life. New York: Baywood; 2002. pp. 149–73. [Google Scholar]


