Abstract
Aims
To compare the effects of multiple dosing with St John's wort (Hypericum perforatum) extract and amitriptyline on heart rate variability, cognitive function and quantitative EEG (qEEG) with placebo in healthy humans.
Methods
A randomized, double-blind, cross over study of 12 healthy male volunteers. Subjects orally received capsules with 255–285 mg St John's wort extract (900 µg hypericin content), 25 mg amitriptyline and placebo three times daily for periods of 14 days each with at least 14 days between. The doses of amitriptyline and St John's wort extract are comparable with respect to their antidepressant activity. Compliance was confirmed by coadministration of 10 mg of riboflavin with each capsule and detection of urinary vitamin B2 on treatment day 11 with high performance liquid chromatography. Measurements of heart rate variability, psychometric tests and qEEG were performed before start of medication and repeatedly on the last treatment day.
Results
St John's wort extract did not affect heart rate variability (HRV) whereas amitripytline significantly decreased it: the difference in the percentage number of adjacent RR intervals > 50 ms (pNN50) was 8.6 (−2.6, 19.9; mean; 95% confidence interval) between St John's wort extract and placebo and −17.6 (−24.7, −10.4) between amitriptyline and placebo. Neither St John's wort extract nor amitriptyline had an influence on cognitive performance such as choice reaction, psychomotor coordination, short-term memory and responsiveness to distractive stimuli. Amitriptyline but not St John's wort extract decreased self rated activity (P < 0.05). Both drugs caused significant qEEG changes. St John's wort extract increased theta power density. Amitriptyline increased theta as well as fast alpha power density.
Conclusions
Multiple doses of St John's wort extract do not affect heart rate variability nor cognitive function. Chronic administration of amitriptyline causes a decrement of HRV and subjective sedation but it does not impair cognitive performance.
Keywords: amitriptyline, cognitive function, heart rate variability, quantitative EEG, St John's wort
Introduction
Treatment of depressive illness with tricyclic antidepressants may cause unwanted autonomic and cognitive effects which are due to anticholinergic, alpha-adrenolytic and antihistaminic properties of the drugs. Heart rate variability (HRV) depends on autonomic sympathovagal balance. A decrement of time-derived measurement of HRV such as the percentage number of adjacent RR intervals > 50 ms (PNN50) has been described in depressed patients who received amitriptyline chronically [1, 2]. Frequency derived parameters of HRV such as power in the very low frequency (VLF), low frequency (LF) and high frequency (HF) bands have also been noted to be decreased under treatment with amitryptyline [2, 3].
Cognitive impairment and psychomotor retardation are among the characteristic features of clinical depression. Thus, the sedative effects induced by antidepressant agents are somewhat countertherapeutic, since they may exacerbate these aspects of the clinical profile.
Treatment with amitriptyline is often associated with an impairment of cognitive and psychomotor skills [4]. On the other hand, attention and memory may also be improved in patients receiving multiple dosing with amitriptyline [5]. Increases of slow wave power in the quantitative EEG (qEEG) such as theta activity in humans receiving amitriptyline have been hypothesized to be due to drug induced impairment of vigilance [6].
St John's wort extract is widely promoted as a ‘natural antidepressant’ which lacks autonomic and cognitive side-effects. Patients often report that, compared with synthetic antidepressants, extracts of St John's wort leave them feeling more alert and more able to think clearly [7]. However the cognitive and cardiac autonomic effects of the phyto drug have not yet been evaluated in well defined clinical studies. The aim of the present study was therefore to compare the effects of chronic administration of St John's wort extract on cognitive functions and heart rate variabilitity with those of amitriptyline at equipotent doses [8] and placebo in healthy humans.
Methods
Subjects
Twelve healthy male subjects, aged 22–31 years (25 ± 3 years; mean ± s.d.), weighing between 61 and 89 kg (76 ± 9 kg) and 170–193 cm (181 ± 8 cm), in height were enrolled in the study. The subjects were included after a standard physical examination, routine clinical laboratory tests and a 12-lead ECG. The study was conducted according to the Declaration of Helsinki (Somerset West Amendment 1996) and German regulations. Written informed consent from the subjects and approval from the Hospital Ethics Committee (Dresden, Germany) were obtained.
Study procedure
No concomitant drug therapy was allowed for 2 weeks before and during the study period. The subjects were not allowed to smoke or to consume alcoholic or caffeine-containing beverages for 10 h before and throughout the trial. Each subject received orally under randomized and double-blind crossover conditions capsules with 25 mg amitriptyline, 255–285 mg St John's wort extract (BNO 1385 with 900 µg hypericin content; Bionorica, Neumarkt, Germany) and placebo three times daily for 13 days each. On treatment day 14 the last dose of 25 mg amitriptyline, 255–285 mg St John's wort extract (900 µg hypericin content) and placebo was given at 09.00 h. Treatment phases were separated by a wash out period of at least 14 days. Compliance was confirmed by coadministration of 10 mg riboflavin with each capsule and detection of urinary vitamin B2 on treatment day 11 with high performance liquid chromatography according to Smith [9]. ECG recordings were performed before start of medication and at 0.5, 3 and 5 h after the last dose was given. Subsequently quantitative EEG was recorded. Thereafter cognitive performance was tested with a computerized version of the Vienna Testsystem® (Schuhfried, Mödling, Austria; see below). Systolic and diastolic blood pressure was monitored at 09.00 h on day 1, 11 and 14 at 09.00 h before dosing. All measurements were performed in a supine position.
Heart rate variability
Heart rate analysis was carried out with the computer program Chart® (AD Instruments, Castle Hill, Australia). Details have been described elsewhere [10]. In brief, the ECG signal was digitized at a sample rate of 400 s−1. Respiration was monitored by registration of chest movements. After a resting period of 10 min subjects were instructed to breath deeply at a frequency of 6 cycles min−1 (6 s inspiration, 4 s expiration) as deep respiration was demonstrated to produce maximal HRV in healthy volunteers [11]. The percentage number of adjacent RR intervals > 50 ms (PNN50) was calculated from 200 artefact free beats. A spectral power analysis was carried out over 3 min recording by means of a Fast Fourier Transformation (FFT). Absolute power values were calculated for three frequency bands: very low frequency (VLF) = 0.01–0.04 Hz, low frequency (LF) = 0.04–0.15 hz and high frequency (HF) = 0.15–0.4 Hz.
Quantitative EEG
The EEG signal (T3-A2 derivation) and electrooculogram were recorded for periods of 10 min each with the subjects keeping their eyes open. The electrophysiological variables (notch filter at 50 Hz, 0.3 Hz calibration: 50 µV, 10 Hz sinus wave) were digitized at 125 Hz and stored on tape. After visual screening and exclusion of artefacts the EEG recordings were submitted to a Fast Fourier Transform algorithm of 4 s epochs. Absolute spectral power density was assessed for six frequency ranges (delta 0.25–3.75 Hz, theta 4.00–7.75 Hz, alpha1 8.00–9.75 Hz, alpha2 10.00–12.75, beta1 13–17.75, beta2 18–32 Hz).
Psychometric tests
Prior to each test instructions were given to the subjects and subsequently a training session was perfomed. Subjects responded by touching fields on a computer screen with a light pen or turning knobs or pushing buttons on a panel. Subjective mood was assessed with a 35-item version of the Profile of Mood States (POMS; 12). The Stroop Color-Word-test was applied to test responsiveness to distractive stimuli. In the first part of this test volunteers had to name ink-colours (red, green, yellow or blue) used to print rectangular patches, in the second part they had to name the same colours used to print colour-name words. The words were written in a colour incongruent with their meaning, i.e. the name red appeared in blue ink. Each part consisted of 128 items, the first one served as a control. The differences in time (Δt) needed to give the answer to corresponding items and the number of correct answers were recorded. Visual memory span was assessed with a computerized version of the Block Board tapping test [13]. Subjects had to reproduce tapping-sequences by pointing on blocks which were presented on the screen and tapped in a randomized order. When a subject failed to reproduce three consecutive sequences the test was interupted. The maximum length of a sequence correctly replied (block span) was recorded. The choice reaction time was measured with the Viennese Reaction Device®. The subjects were presented yellow light, red light and a beep tone alone and in various combinations. They were instructed to react as fast as possible when yellow light and beep tone were presented simultaneously. The two-hand coordination test was used to assess psychomotor ability. Subjects had to move a light dot along a given path. They received an acoustic feed back when leaving the path. The time taken for the total path was recorded and the percentage error time was calculated as the ratio of total error time to total time.
Statistical analysis
The statistical analysis was performed with the Sigma Stat® software package (Jandel, San Rafael, CA, USA). Evaluation of heart rate and pNN50 was done with a one-way anova procedure for repeated measurements. Differences in means beween active treatments and placebo were calculated for values obtained at the last time point of measurement and the corresponding 95% confidence intervals are given. Friedman repeated measures anova on ranks was applied for VLF, LF, HF, blood pressure and parameters of cognitive function and qEEG as the values were not normaly distributed. If significant, Student-Newman-Keuls posthoc tests were used for comparisons of active treatment with placebo and baseline conditions. Statistical significance was accepted at P < 0.05.
Results
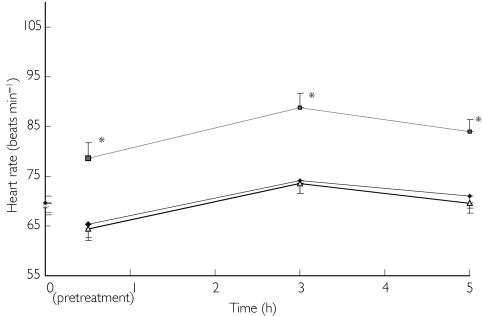
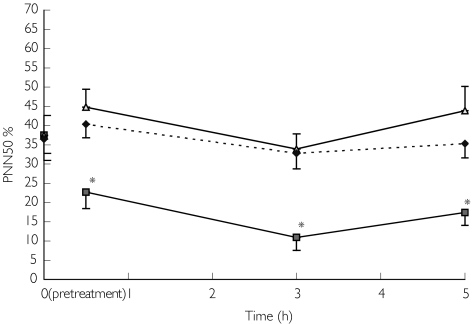
An increase in heart rate was seen after multiple dosing with amitriptyline (F ratio = 23.8, anovaP < 0.001). No significant changes of heart rate were noted after administration of St John's wort extract when compared post hoc with pretreatment and placebo conditions (Figure 1). The difference in heart rate was 13.2 beats min−1 (8.1, 18.3 beats min−1; mean; 95% confidence interval) between amitriptyline and placebo and −1.5 beats min−1 (−6.1, 3.1) between St John's wort and placebo. A decrease in pNN50 was seen after multiple dosing with amitriptyline (F ratio = 13.1, anovaP < 0.001). In contrast, no significant change of pNN50 was seen with St John's wort extract as compared post hoc with pretreatment and placebo conditions (Figure 1). The difference in pNN50 was −17.6 (−24.7, −10.4; mean; 95% confidence interval) between amitriptyline and placebo and 8.6 (−2.6, 19.9) between St John's wort extract and placebo. Post hoc comparisons with pretreatment and placebo conditions revealed decrements at all time points of measurement after administration of amitriptyline (Figure 2). Power in the LF and HF bands were also affected (anovaP < 0.001, Chi-Square = 57.9 and 70.4, respectively). Significant decrements were observed with amitriptyline at all time points of measurement but not with St John's wort extract when compared post hoc with pretreatment and placebo conditions (Table 1). Power in the VLF band was not influenced by any treatment. Neither amitriptyline nor St John's wort extract had an influence on diastolic and systolic blood pressure values. Self rated activity was found altered (anovaP < 0.0001, Chi-Square = 51.2). Decrements occurred at all time points of measurement during multiple dosing with amitriptyline, but no mood changes were noted with St John's wort extract (Table 2). None of the drugs had an influence on choice reaction time, short-term memory, psychomotor coordination and performance in the Stroop test. qEEG was altered in the theta and fast alpha (alpha2) bands (anovaP < 0.001, Chi-Square = 36.3 and 37.0, respectively). St John's wort increased theta activity whereas amitriptyline enhanced theta as well as fast alpha (alpha2) power density. Post hoc comparisons with pretreatment and placebo conditions were significant 0.5 and 3 h after last dosing (Table 3).
Figure 1.
Heart rate (beats min−1; mean ± s.e. mean) after placebo (♦), amitriptyline ( ) and St John's wort (
) and St John's wort ( ).
).
Figure 2.
Percentage number of adjacent RR intervals > 50 ms (PNN50%; mean ± s.e.mean) after placebo (♦), amitriptyline ( ) and St John's wort (
) and St John's wort ( ).
).
Table 1.
Absolute power in the low (LF) and high frequency (HF) bands (ms2; median; range).
| Time (h) | Parameter | Amitriptyline | St John's wort | Placebo |
|---|---|---|---|---|
| 0 | LF | 5626 (1138–12420) | 5325 (1138–17644) | 5137 (1119–20334) |
| HF | 573 (60–3069) | 642 (60–4480) | 437 (78–3893) | |
| 0.5 | LF | 3021 (742–10200)* | 6297 (2644–12294) | 5022 (2670–11295) |
| HF | 196 (65–1396)* | 761 (184–3964) | 650 (185–2396) | |
| 3 | LF | 1241 (384–7136)* | 4592 (2143–10697) | 4094 (2655–9748) |
| HF | 111 (29–2116)* | 531 (225–2612) | 554 (194–2411) | |
| 5 | LF | 2683 (945–8766)* | 6380 (2634–12545) | 4729 (2877–10420) |
| HF | 195 (36–1782)* | 938 (195–3237) | 615 (104–3262) |
P < 0.05 when compared post hoc with pretreatment (time 0) and with placebo.
Table 2.
Profile of mood states activity scores (all values are median; range).
| Time (h) | Amitriptyline | St John's wort | Placebo |
|---|---|---|---|
| 0 | 28.0 (19.0–36.0) | 30.5 (15.0–39.0) | 31.0 (24.0–37.0) |
| 0.5 | 24.5 (10.0–34.0)* | 31.0 (15.0–37.0) | 30.0 (21.0–35.0) |
| 3 | 22.5 (13.0–37.0)* | 30.5 (15.0–36.0) | 29.5 (20.0–35.0) |
| 5 | 25.5 (12.0–35.0)* | 28.5 (17.0–34.0) | 28.5 (19.0–34.0) |
P < 0.05 when compared post hoc with pretreatment (time 0) and with placebo.
Table 3.
EEG absolute power density (µV2 Hz−1; all values are median; range).
| Time (h) | Range | Amitriptyline | St John's wort | Placebo |
|---|---|---|---|---|
| 0 | theta | 2.7 (1.6–5.6) | 2.7 (1.7–6.0) | 2.7 (1.5–8.7) |
| alpha2 | 3.6 (1.2–8.3) | 3.1 (1.2–8.0) | 3.5 (1.1–8.3) | |
| 0.5 | theta | 3.2 (2.1–9.2)* | 3.0 (1.6–4.9)* | 2.8 (1.7–6.5) |
| alpha2 | 3.9 (1.7–10.2)* | 3.1 (1.6–6.7) | 3.1 (1.1–14.4) | |
| 3 | theta | 3.6 (2.1–8.6)* | 3.2 (1.7–6.3)* | 3.1 (1.7–8.1) |
| alpha2 | 4.9 (2.0–9.3)* | 3.8 (1.6–7.4) | 3.6 (1.3–12.1) | |
| 5 | theta | 3.0 (2.2–9.3) | 3.2 (1.6–6.7) | 3.2 (1.6–12.8) |
| alpha2 | 4.2 (1.9–8.8) | 4.3 (1.7–7.6) | 4.1 (1.0–13.3) |
P < 0.05 when compared post hoc with pretreatment (time 0) and with placebo.
All adverse events were mild to moderate in nature and transient. Dry mouth was seen in nine cases with amitriptyline and in two cases with placebo but was not reported during treatment with St John's wort extract. Each of the 12 subjects complained about tiredness when receiving amitriptyline whereas only one volunteer reported sedation during treatment with St John's wort extract. Dizziness, emotional irritability, lack of concentration, elevation of serum transaminases (ALAT 0.81 µkat l−1, ASAT 0.63 µkat l−1) and excessive appetite were further adverse events observed with amitriptyline. Elevation of transaminases was asymptomatic. Lack of concentration and headaches were seen in one case each during treatment with St John's wort extract (Table 4).
Table 4.
Adverse events.
| Adverse event | Amitriptyline | St John's wort extract | Placebo |
|---|---|---|---|
| Dry mouth | 9 | – | 2 |
| Sedation | 12 | 1 | – |
| Dizziness | 7 | – | 1 |
| Emotional irritability | 4 | – | – |
| Lack of concentration | 4 | 1 | – |
| Nausea | – | – | 1 |
| Headaches | – | 1 | – |
| Elevation of serum transaminases | 1 | – | – |
| Excessive appetite | 1 | – | – |
Discussion
In the present study it was demonstrated that amitriptyline decreases heart rate variability (HRV). This is consistent with previous studies [4, 14, 15]. In contrast, St John's wort extract had no influence on HRV. The decrease in heart variability after chronic adminstration of amitriptyline appears to result from its anticholinergic properties as a reduction of spectral power was noted in the high and low frequency ranges but not in the very low frequency band. A decrease in HRV was previously observed with tricyclic antidepressants (TCAs) with similar anticholinergic properties such as imipramine [16] and doxepine [17]. HRV depends on autonomic parasympathetic and on sympathetic balance. St John's wort extract inhibits the synaptic reuptake of noradrenaline. It exerts central cholinergic and dopaminergic actions [18, 19]. Therefore, an influence on HRV parameters could have been expected for both active treatments. It has not yet been established what impairment of HRV means with regard to drug safety. Patients with a decrement of HRV after myocardial infarction have an increased mortality risk when compared to patients who have an intact cardiac autonomic function [20].
The present study indicates that St John's wort extract does not impair cognitive functions. Amitriptyline was not found to influence objective measures of cognitive functions such as choice reaction time, memory span, psychomotor performance and responsiveness to distractive stimuli (Stroop performance) to a significant extent but it was noted to lower the levels of self rated activity when administered at multiple daily doses of 75 mg. Our results are consistent with previous trials in healthy volunteers who received multiple dosing with amitriptyline up to 150 mg day−1[21–23]. It may be noted, that our present findings contradict some other findings in the literature. Saarial-ho-Kere and coworkers reported a slight but statistically significant impairment of psychomotor coordination in healthy subjects after 8 days treatment with 75 mg amitriptyline per day [24]. Seppälä and coworkers found impaired psychomotor coordination and reaction ability after 8 days treatment with amitriptyline at daily doses of 100 mg [25]. These discrepancies may be due either to shorter treatment duration or differences in the test paradigms.
Amitriptyline as well as St John's wort extract were found by us to induce increases of theta activity in the qEEG. St John's wort extract standardized on hypericin content was used by us. Rises in theta power have also been described for other chemical antidepressants and for St John's wort extract standardized on hyperforin [26, 27]. They have been suggested to reflect changes in the catecholaminergic transmitter system of the brain. In contrast, an increase in alpha power which we observed with amitriptyline but not with St John's wort extract has been attributed to changes in the serotonergic transmitter system [28].
Taken together, St John's wort extract as well as amitriptyline do not interfere with cognitive and psychomotor abilities. St John's wort extract does not influence HRV wheras amitriptyline decreases HRV. Both drugs produce changes in the qEEG.
This work was part of a thesis. The authors are sincerely thankful to Mrs T. Urban and Mrs E. Hempel for their assistance in conducting the study.
References
- 1.Ziegler VE, Co BT, Biggs JT. Electrocardiographic findings in patients undergoing amitriptyline treatment. Dis Nerv Syst. 1977;38:697–699. [PubMed] [Google Scholar]
- 2.Rechlin T, Claus D, Weis M. Heart rate analysis in 24 patients treated with 150 mg amitriptyline per day. Psychopharmacology. 1994;116:110–114. doi: 10.1007/BF02244880. [DOI] [PubMed] [Google Scholar]
- 3.Rechlin T, Weis M, Claus D. Heart rate variability in depressed patients and differential effects of paroxetine and amitripytline on cardiovascular autonomic functions. Pharmacopsychiat. 1994;27:124–128. doi: 10.1055/s-2007-1014291. [DOI] [PubMed] [Google Scholar]
- 4.Fairweather DB, Kerr JS, Harrison DA, Moon CA, Hindmarch I. A double blind comparison of the effects of fluoxetine and amitriptyline on cognitive function in elderly depressed outpatients.
- 5.McNair DM, Kahn RJ, Frankenthaler LM, Faldetta LL. Amoxapine and amitriptyline. II. Specifity of cognitive effects during brief treatment of depression. Psychopharmacology. 1984;83:134–139. doi: 10.1007/BF00429721. [DOI] [PubMed] [Google Scholar]
- 6.Herrmann WM, Schärer E, Delini-Stula A. Predictive value of pharmaco-electroencephalography in early human–pharmacological evaluations of psychoactive drugs. First example: savoxepine. Pharmacopsychiatry. 1991;24:196–205. doi: 10.1055/s-2007-1014469. [DOI] [PubMed] [Google Scholar]
- 7.Mueller BM. St. John's wort for depressive disorders: result of an outpatient study with the hypericum preparation HYP 811. Adv Ther. 1998;15:109–116. [PubMed] [Google Scholar]
- 8.Wheatley D. LI 160, an extract of St. John's wort, versus amitriptyline in mildly to moderately depressed outpatients: a controlled 6-week clinical trial. Pharmacopsychiatry. 1997;30:S77–S80. doi: 10.1055/s-2007-979523. [DOI] [PubMed] [Google Scholar]
- 9.Smith MD. Rapid method for determination of riboflavin in urine by high-performance liquid chromatography. J Chromatogr. 1980;182:285–291. doi: 10.1016/s0378-4347(00)81476-0. [DOI] [PubMed] [Google Scholar]
- 10.Mück-Weymann M. Methoden und Technik [Methods and Techniques] In: Mück-Weymann M, editor. Autonome Funktionskreise in Psychosomatik und PsychiatrieNicht-Invasives Biomonitoring in der Psychopharmakotherapie[Autonomic Functions in Psychosomatic Medicine and PsychiatryNon-Invasive Monitoring of Psychopharmacological Therapy] Lage: Hans Jacobs; 2000. pp. 28–38. [Google Scholar]
- 11.Anonymous. Special report of the Task Force of the European Society of Cardiology and North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 12.Gibson SJ. The measurement of mood states in older adults. J Gerontol: Psychol Sci. 1997;52B:P167–P174. doi: 10.1093/geronb/52b.4.p167. [DOI] [PubMed] [Google Scholar]
- 13.Smirni P, Villardita C, Tappala G. Influence of different paths on spatial memory performance in the block-tapping test. Clin Neuropsychol. 1983;5:355–359. doi: 10.1080/01688638308401184. [DOI] [PubMed] [Google Scholar]
- 14.Low PA, Opfer-Gehrking TL. Differential effects of amitriptyline on sudomotor, cardiovagal, and adrenergic function in human subjects. Muscle Nerve. 1992;15:1340–1344. doi: 10.1002/mus.880151208. [DOI] [PubMed] [Google Scholar]
- 15.Burgess CD, Montgomery S, Wadsworth J, Turner P. Cardiovascular effects of amitriptyline, mianserin, zimelidine and nomifensine in depressed patients. Postgrad Med J. 1979;55:704–708. doi: 10.1136/pgmj.55.648.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeragani VK, Pohl R, Balon R, et al. Effect of imipramine tretament on heart rate variability measures. Neuropsychobiol. 1992;26:27–32. doi: 10.1159/000118892. [DOI] [PubMed] [Google Scholar]
- 17.Rechlin T. Decreased RR-variation. a criterium for overdosage of tricyclic psychotropic drugs. Intensive Care Med. 1995;21:598–601. doi: 10.1007/BF01700167. [DOI] [PubMed] [Google Scholar]
- 18.Nathan PJ. The experimental and clinical pharmacology of St. John's wort (Hypericum perforatum L.) Mol Psychiatry. 1999;4:333–338. doi: 10.1038/sj.mp.4000557. [DOI] [PubMed] [Google Scholar]
- 19.Dimpfel W, Schombert L. Central action of hypericum flore extractum siccum in freely moving rats. Eur J Med Res. 1997;28:491–496. [PubMed] [Google Scholar]
- 20.Zuanetti G, Neilson JM, Latini R, Santoro E, Maggioni AP, Ewing DJ. Prognostic significance of heart rate variability in post-myocardial infarction patients in the fibrinolytic era. The GISSI-2 results. Circulation. 1996;94:432–436. doi: 10.1161/01.cir.94.3.432. [DOI] [PubMed] [Google Scholar]
- 21.Lader M, Melhuish A, Frcka G, Fredricson Overo K, Christensen V. The effects of citalopram in single and repeated doses and with alcohol on physiological and psychological measures in healthy subjects. Eur J Clin Pharmacol. 1986;31:183–190. doi: 10.1007/BF00606656. [DOI] [PubMed] [Google Scholar]
- 22.Warrington SJ, Dana-Haeri J, Sinclair AJ. Cardiovascular and psychomotor effects of repeated doses of paroxetine: a comparison with amitriptyline and placebo in healthy men. Acta Psychiatr Scand. 1989;350(Suppl):42–44. doi: 10.1111/j.1600-0447.1989.tb07169.x. [DOI] [PubMed] [Google Scholar]
- 23.Robbe HWJ, O'Hanlon JF. Acute and subchronic effects of paroxetine 20 and 40 mg on actual driving, psychomotor performance and subjective assessments in healthy volunteers. Eur Neuropsychopharm. 1995;5:35–42. doi: 10.1016/0924-977x(94)00130-4. [DOI] [PubMed] [Google Scholar]
- 24.Saarialho-Kere U, Mattila MJ, Paloheimo M, Seppälä T. Psychomotor, respiratory and neuroendocrinological effects of buprenorphine and amitriptyline in healthy volunteers. Eur J Clin Pharmacol. 1987;33:139–146. doi: 10.1007/BF00544557. [DOI] [PubMed] [Google Scholar]
- 25.Seppälä T, Strömberg C, Bergman I. Effects of zimeldine, mianserin and amitriptyline on psychomotor skills and their interaction with ethanol – a placebo controlled cross-over study. Eur J Clin Pharmacol. 1984;27:181–189. doi: 10.1007/BF00544043. [DOI] [PubMed] [Google Scholar]
- 26.Saletu B, Grünberger J, Rajna P. Pharmaco-EEG profiles of antidepressants. Pharmacodynamic studies with fluvoxamine. Br J Clin Pharmacol. 1983;15:369S–384S. doi: 10.1111/j.1365-2125.1983.tb02128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schellenberg R, Sauer S, Dimpfel W. Pharmacodynamic effects of two different hypericum extracts in healthy volunteers measured by quantitative EEG. Pharmacopsychiatry. 1998;31(Suppl):44–53. doi: 10.1055/s-2007-979345. [DOI] [PubMed] [Google Scholar]
- 28.Dimpfel W, Spüler M, Nichols DE. Hallucinogenic and stimulatory amphetamine derivatives: fingerprinting DOM, DOS, DOB, MDMA, and MDBB by spectral analysis of brain field potentials in the freely moving rat (Tele-Stereo-EEG) Psychopharmacol. 1989;98:297–303. doi: 10.1007/BF00451678. [DOI] [PubMed] [Google Scholar]