Abstract
Aims The use of medication and information discharge summaries (MIDS) has become a standard procedure in many hospitals. We have evaluated if these summaries, together with in-patient pharmaceutical counselling backed up with a simple medicine reminder card, may help with the delivery of seamless pharmaceutical care.
Methods Elderly patients prescribed more than four items discharged to their own home received the standard discharge policy including a recently introduced MIDS and medicine reminder card. Each patient's GP was sent a copy on discharge. Pre-discharge a pharmacist counselled study patients about their medicines and compliance. A research pharmacist visited patients in their home approximately 2–3 weeks and at 3 months post-discharge to determine their drug knowledge, compliance, home medicine stocks and any healthcare related events.
Results Forty-three study and 40 control patients completed both visits. Their mean (s.d.) ages were 80.2 (5,7) and 81.1 (5,8) years and they were prescribed 7.1 (1.8) and 7.1 (2.3) items, respectively. At visit 1 knowledge (P < 0.01) and compliance (P < 0.001) was better in the study group. At visit 2 compliance had improved in the study group (P < 0.001). Unplanned visits to the GP and readmission to hospital amongst the study group were 19 and 5, respectively, which were both significantly less (P < 0.05) than 27 and 13 in the control group. At visit 2 for the study group the 24 unplanned GP visits and three re-admissions were significantly (P < 0.05) less than the respective 32 and 15 in the control group. At visit 1, two study group patients had altered their own medication compared with 10 control patients. At visit 2 these reduced to 0 and 4, respectively.
Conclusions In-patient pharmaceutical counselling, linked to a medication and information discharge summary and a medicine reminder card, contributed to better drug knowledge and compliance together with reduced unplanned visits to the doctor and re-admissions. A pharmaceutical domiciliary visit consolidated the improved healthcare outcomes.
Keywords: compliance, discharge, pharmaceutical counselling, readmission
Introduction
Educating patients about their drugs could improve their understanding on the importance of continued therapy and compliance at home following discharge [1]. Research into hospital admissions suggests that many are drug-related [2] and that with appropriate patient education this incidence could be reduced [3]. The degree of knowledge that patients have improves compliance [4] and this is enhanced by a medicine reminder card [5].
Studies have shown differences between discharge medication and the next prescription due to a lack of good communication [6, 7]. Pharmaceutical care plans given to patients pre-discharge and posted to community pharmacists together with pre-discharge pharmacist counselling improved compliance but did not alter unintentional changes to therapy [7]. Community pharmacists generally ignored these care plans because during the dispensing process they were unaware that the patient had recently been discharged. In contrast a study has shown that giving the patient a discharge advice note with instructions to show to their Community Pharmacist, when dispensing their next prescription, decreased the number of unintentional changes [8]. However, the incidence of 32.2% for unintentional changes amongst the group with the discharge advice note is unsatisfactory and many patients post-discharge were unable to visit their community pharmacy. Other studies have highlighted how a pharmaceutical domiciliary visit is useful [7, 9 10] and can prevent an unnecessary hospital readmission [7, 10].
To improve the communication between secondary and primary care many hospitals have recently introduced a policy of providing a hand written summary when a patient is discharged. This is immediately posted to the patient's General Practitioner and a copy is given to the patient. This medication and information discharge summary (MIDS) includes the reason for admission, the major in-patient events and the discharge prescription. We have evaluated if pharmaceutical counselling pre-discharge in combination with the MIDS and a medicine reminder card can improve a patient's therapeutic management post-discharge and reduce unnecessary visits to their doctor or hospital readmission. We have also investigated if a pharmaceutical domiciliary visit can reinforce the in-patient counselling.
Methods
The Local Research Ethics Committee gave approval for the study and all patients gave signed informed consent. All patients admitted to two care of the elderly wards who were> 65 years, prescribed 4 or more regular items, were to be discharged to their own home and had an abbreviated mental score of greater than 7 out of 10 were eligible. Their first language was English and routine assessment by the clinical pharmacist was that they could have problems with their medicines when they were discharged to their home. Every patient who met the study criteria was invited to take part. The period of recruitment was 4 months. The same medical teams serviced the two care of the elderly wards. Of the two care of the elderly wards one was randomly chosen for the study group patients and the other for the control group patients.
The hospital discharge policy, at the time of the study, was that all patients and their General Practitioner (GP) together with the district nurse and carer (where appropriate) received a copy of the patient's medication and information discharge summary sheet (MIDS). This hand written sheet included data on the date of admission and discharge, reason(s) for admission, diagnosis and other problems together with their major in-patient events and follow up procedure. Other information included the community services arranged, any procedures/operations/investigations and a contact number and name of the key nurse. In addition, patients were given a medicine reminder card [5]. On this card the generic name (as applicable) for each drug prescribed was stated together with other common names given to the drug and what it was prescribed for. The number of doses together with the times of day (tick in box for breakfast, lunchtime, teatime and bedtime as appropriate) were also included. All patients were given 14 days of medication on discharge and informed to show their GP and community pharmacist the MIDS and medicine card during their first visit post discharge.
Normal discharge was provided to control patients. At this point the nurse went through their discharge medicines and explained that a new supply (via their GP) should be arranged within 14 days. They used the medicine reminder card and each dispensed item when explaining the prescribed drugs and doses. They also went through the information in the MIDS.
Study group patients received pre-discharge counselling by the clinical pharmacist attached to that ward. During this counselling session (approximately 30 min per patient) patients received information about their medicines. This included why each item had been prescribed, other uses (if applicable) and side-effects. Doses and dosage times were stressed with the aid of the medicine reminder card together with instructions to keep this card with their medicines as a constant reminder. The importance of compliance was stressed together with the consequences of under and over use of their medicines. The pharmacist asked the patient appropriate questions to ensure that the patient had remembered the information. For these questions the patient was encouraged to use their medicine reminder card to provide the answers. This counselling session was planned for the 24 h period before the patient was planned to be discharged.
At discharge all control and study group patients were given two envelopes. One envelope was labelled ‘to be given to your doctor at your next visit’ and the other ‘to be given to your pharmacist when they dispense your next prescription’. They were all verbally instructed to whom to give the letter. Each envelope contained a questionnaire (and a stamp addressed envelope) to obtain feedback on the information discharge system that had been implemented. Also, on discharge all patients were informed that a research pharmacist would contact them within 7 days to arrange a visit at their home to ‘check how they were coping with their medicines’. This visit was planned between 15 and 22 days post-discharge. If applicable any patient carers (including friends, relatives or neighbours) who helped them with their medicines were invited to attend. At this visit using a simple structured questionnaire the research pharmacist first went through all the medicines the patient was taking/using (prescribed and self medicated) and if any were different to that on discharge the reason for the change was obtained. If the patient was administering any medicines that had not been prescribed at discharge or by their GP they were advised to visit their GP. Also if the patient had stopped any prescribed medication they were advised to see their GP. Each patient was asked for information about what each medicine was being used for, its dose and how often he or she administered their medication. These data, for each drug, were recorded as either correct or incorrect. Any information that the patient was unavailable to provide or wrong was corrected. The importance of compliance was stressed. All post-discharge visits with any healthcare personnel were recorded. The patient was asked to show the research pharmacist all the medicines they had at home. Their home medicine stocks were recorded and the patient was advised to take any out of date or unnecessary medicines to their local pharmacy for disposal. Another visit was arranged for 3 months post-discharge. During this second visit the information obtained and the advice given was the same as that of the first visit.
Percent scores were derived for correct answers (drug use, dose and dosage interval) of each item prescribed. From the patient's medicine stocks and prescription refills an assessment of their compliance was made. During the first visit an assessment of compliance was made from a count of dosage units in the container provided on discharge and their first prescription post discharge. The dosage units of each item dispensed were obtained from the label on the container and the actual amounts remaining were counted. The difference between the amount dispensed and the doses left would be the number of dosage units that had been removed. Percentage compliance was calculated by dividing this difference by the number of dosage units that (theoretically) should have been removed. Patients were asked if they had administered any units from containers obtained prior to discharge so that this could be taken into consideration and thus compliance would not be underestimated. Compliance was categorized as follows: (a) mixing – when the amount of dosage units exceed the stated number on the label of the container dispensed, (b) under use – < 85% compliance, (c) over usage – > 115% compliance and (d) compliant −85–115% compliance. For the second visit compliance was assessed using the home medicine stocks between visit 1 and 2 and the refill prescription(s). The deviation of 15% was used in accordance with that used in other studies [11, 12].
Unless stated, an independent samples two tailed t-test was used for statistical comparisons.
Results
Forty-five study and 44 control group patients were recruited. From the study group, prior to visit 1, one died and one withdrew leaving 43 (16 females) in this group. Of the control group two died, one was admitted to a nursing home and one withdrew before visit 1, leaving 40 patients (20 females). All these remaining patients completed both visits. There was no statistical difference in gender (chi square) or abbreviated mental scores (Mann–Whitney) between the two groups. Sixteen patients in each group lived with their spouse whereas 20 study and 22 control group patients lived alone and the remainder with a relative. The normal procedure of 37 study and 36 control group patients was to ring the surgery when a repeat prescription was required and only one from each group collected the prescription form. Only nine study and six control group patients collected their own dispensed medicines. However 12 study and eight control patients had their dispensed items delivered by their local pharmacy.
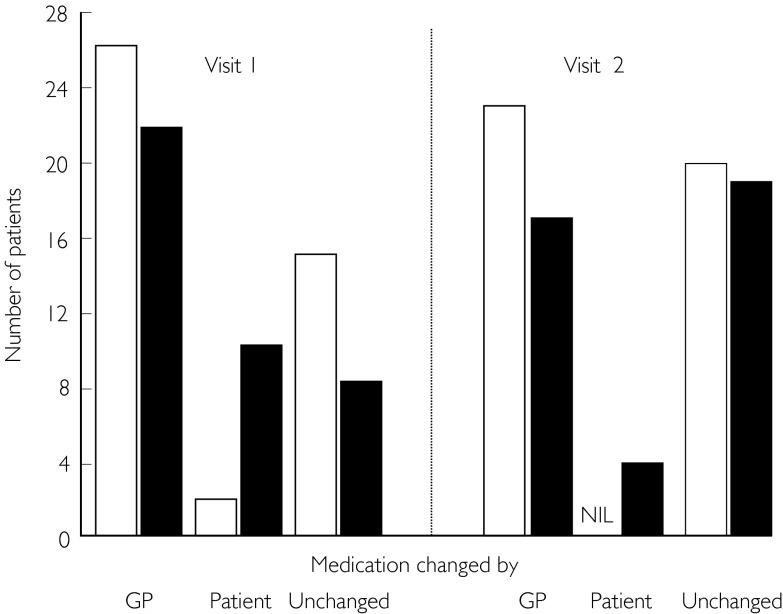
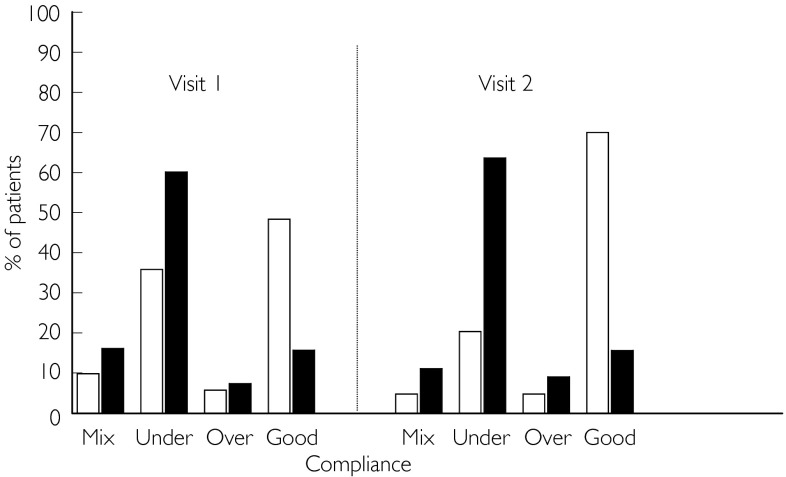
The mean (s.d.) age of the study (n = 43) group was 80.2 (5.7) years and this was statistically similar to the 81.1 (5.8) years of the control (n = 40) group patients. Table 1 reveals that there was no statistical difference for the drugs on admission between the two groups and those prescribed during their hospital stay and at discharge. A summary of the data collected during the two visits is shown in Table 2. Those in the study group tended not to hoard drugs for more than 3 months between the two visits (P < 0.01). Table 3 shows the change in the number of regular items prescribed for each patient and Figure 1 highlights who was responsible for the changes. Figure 2 differentiates their compliance into the four categories (mixing, over, under and good). Statistical analysis for each group between visit 1 and 2 revealed a highly significant (P < 0.001, chi2 test) improvement for compliance in the study group. All other comparisons between visits 1 and 2 for the study group and the control group were not statistically different. Figure 3 and Table 2 highlight that there were significantly (P < 0.05) more unplanned GP visits and hospital re-admission in the control group.
Table 1.
Mean (s.d.) in-patient prescribing.
| Items | Number | Study group | Mean (s.d.) | Number | Control group | Mean (s.d.) |
|---|---|---|---|---|---|---|
| All items on admission | 275 | 4–12 | 6.4 (1.9) | 274 | 3–15 | 6.8 (2.6) |
| Stopped on admission | 36 | 0–9 | 0.8 (1.6) | 59 | 0–6 | 1.5 (1.6) |
| Started on admission | 186 | 0–10 | 4.3 (2.8) | 200 | 0–13 | 5.0 (2.9) |
| Stopped whilst in-patient | 78 | 0–7 | 1.8 (1.80) | 83 | 0–5 | 2.1 (1.5) |
| Regular items on discharge | 303 | 4–11 | 7.1 (1.8) | 285 | 4–14 | 7.1 (2.3) |
| PRN items on discharge | 44 | 0–3′ | 1.0 (0.9) | 47 | 0–3 | 1.2 (1.0) |
Table 2.
Summary (with statistical analysis) of data collected during visit 1 and 2
| Visit 1 | Visit 2 | |||
|---|---|---|---|---|
| Study | Control | Study | Control | |
| Mean (s.d.) length of visit (min) | 32 (10) | 57 (18) | 31 (15) | 45 (18) |
| Number of regular items prescribed | 340 | 331 | 342 | 328 |
| Mean (s.d.) number of regular items prescribed | 7.9 (2.0) | 8.3 (2.6) | 8.0 (2.3) | 8.2 (2.4) |
| Patients (n) storing items no longer prescribed | 34 | 39 | 35 | 39 |
| Drug use (% correct of total items) | 95.3 | 63.1† | 97.4 | 69.5† |
| Dosage interval (% correct of total items) | 96.2 | 86.7† | 97.4 | 86.0† |
| Dose (% correct of total items) | 98.8 | 93.7† | 98.5 | 91.5† |
| Compliant (% of total items) | 48.4 | 15.9‡ | 70.0 | 15.8‡ |
| Patients with GP visits (n) | 19 | 27* | 24 | 32* |
| Patients readmitted (n) | 5 | 13* | 3 | 15* |
Study vs control group at each visit.
P < 05
P < 0.01
P < 0.001
otherwise non-significant independent paired t-test except Pearson's chi-squared test for GP visits and readmission.
Table 3.
The number of changes to the previous prescription of each patient
| Change in number of items | Between discharge and Visit 1 | Between visit 1 and visit 2 | ||
|---|---|---|---|---|
| Study | Control | Study | Control | |
| −4 | 1 | |||
| −3 | 1 | 1 | 1 | |
| −2 | 1 | 2 | 4 | 6 |
| −1 | 5 | 1 | 5 | 3 |
| 0 | 15 | 8 | 20 | 19 |
| 1 | 8 | 12 | 8 | 5 |
| 2 | 10 | 9 | 5 | 3 |
| 3 | 1 | 4 | 1 | |
| 4 | 2 | 3 | ||
| 5 | 1 | 1 | ||
Figure 1.
Person responsible for changing the prescribed medication. □ Study group; ▪ control group.
Figure 2.
Levels of compliance for all items by study and control groups at visit 1 (items = 340 and 331, respectively) and visit 2 (342 and 328, respectively). □ Study group; ▪ control group.
Figure 3.
Percentage of patients with unplanned GP visits and hospital re-admission. □ Study group; ▪ control group.
Of the 83 questionnaires (study and control) the GPs returned nine uncompleted, six partially completed because they had already filled one for another patient and 46 were completed. Community pharmacists returned three uncompleted, 11 partially completed because they had already filled one in and 35 completed. Thus 61 forms were returned by GPs and 49 from community pharmacists and the mean (s.d.) time between patient discharge and receiving a returned form in the post was 12.9 (1.7) and 13.0 (1.8) days post-discharge. There was no difference between the number of returned forms via the patients in the study and control groups. Thirty (57.7%) of the 52 (6 + 46) GPs stated that they were aware that their copy of the MIDS had been received and 18 (34.6%) had been shown a copy by their patient. In contrast only two (4.4%) patients showed a copy of their MIDS to their community pharmacist (n = 11 + 35). A summary of their comments is shown in Table 4. 58.7% of GPs and 97.1% of community pharmacists agreed that the community pharmacist, that had been nominated by the patient, should be sent a copy
Table 4.
Summary of GP (n = 46) and Community Pharmacist (n = 35) feedback in the questionnaires about the MIDS (number and percentage in parenthesis)
| General practitioners | Community pharmacists | |
|---|---|---|
| Useful for | ||
| Transfer of information | 41 (89.1%) | 32 (91.4%) |
| GP | 45 (97.8%) | 33 (94.3%) |
| Community pharmacist | 31 (67.4%) | 34 (97.1%) |
| Nurse | 41 (89.1%) | 32 (91.4%) |
| Social worker | 11 (23.9%) | 14 (40.0%) |
| Not useful at all | 4 (8.7%) | 0 (0%) |
| Information required | ||
| Name of drug | 46 (100%) | 35 (100%) |
| When to take each drug | 35 (76.1%) | 33 (94.3%) |
| Why each drug prescribed | 18 (39.1%) | 24 (68.6%) |
| How long to prescribe | 44 (95.7%) | 34 (97.1%) |
| Side-effects | 15 (32.6%) | 6 (17.1%) |
| Correct storage of item | 14 (30.4%) | 25 (71.4%) |
| Reason for admission | 45 (97.8%) | 19 (54.3%) |
| Main diagnosis | 46 (100%) | 31 (88.6%) |
| Other clinical problems | 45 (97.8%) | 30 (85.7%) |
| Follow-up information | 44 (95.7%) | 29 (82.9%) |
| Potential problems with MIDS | ||
| Patients may lose their MIDS | 44 (95.7%) | 35 (100%) |
| Confidentiality | 25 (54.3%) | 14 (40%) |
| Diagnosis given to patient | 28 (60.9%) | 10 (28.6%) |
| Diagnosis given to pharmacist | 30 (65.2%) | 2 (5.7%) |
| Diagnosis given to other healthcare | 14 (30.4%) | 1 (2.9%) |
| Not all patients use same pharmacy | 42 (91.3%) | 23 (65.7%) |
| Legibility of hand-written form | 46 (100%) | 34 (97.1%) |
Discussion
The results indicate the healthcare benefits of in-patient pharmaceutical counselling to elderly patients, prior to discharge, coupled with the MIDS and a medicine reminder card. Overall the study group patients’ knowledge of their prescribed medicines was better, they had higher compliance rates, less self prescribed from their home medicine stocks, they visited their GPs less often and there were fewer hospital admissions. A previous study, published in abstract form, has shown how short-term self reported adherence was improved by pharmaceutical counselling to elderly patients prescribed at least one medication [13]. The healthcare benefits were not assessed and there was no change in the drug knowledge of the patients. This earlier study was carried out prior to the implementation of prompt discharge summarizes, also given to the patient, and the use of medicine reminder cards.
Each in-patient counselling procedure took approximately 30 min of contact time. Thus to counsel the 43 study patients would have involved approximately 24 h of staff time. There were eight fewer re-admissions amongst the study group during the first few weeks post-discharge. Over the next 3 months (between the first and second domiciliary visit by the research pharmacist) there was also 12 fewer re-admissions in the study group. The improvements indicate that it is cost effective for a pharmacist to counsel each elderly patient prior to discharge. The overall time of the first domiciliary visit was approximately 30 min for study patients and 1 h per control patient but this did not include travel time. The data suggest that the improved healthcare events were maintained between the two visits with compliance significantly increasing in the study group, from 48 to 70%. These positive effects highlight the potential of a pharmacist to counsel each elderly patient during a domiciliary visit post-discharge. The home medicine stocks can be checked at this visit to ensure that out of date medication is disposed of together with any that are no longer prescribed. We appreciate that the results obtained may reflect differences between the two wards. Hospital data did not indicate any difference in admission or re-admissions rates for these two wards. To use the same ward for control and study group patients may have influenced the discharge counselling given by nurses to the control group.
Previous research has shown that problems are caused by prolonged delays in GPs receiving discharge information [1, 14, 15] and that the content is usually inadequate [14]. The turnover time in receiving the completed questionnaires indicates that delays have been substantially shortened. This could have been responsible for the absence of unintentional prescribing changes. Although GPs and community pharmacists indicated that there was some room for improving the MIDS overall they were satisfied. The impact of the introduction of the MIDS and the medicine reminder card, prior to the study, has not been studied. GPs welcomed providing the community pharmacist with a copy of the MIDS although they did have some reservations about the confidentiality of the information. A previous study has shown that less than 10% of 403 GPs were in favour of such information being sent to a community pharmacist [16]. The positive response, in our study, is welcomed as it will provide community pharmacists with the information they require to ensure the continuity of care to the discharged patient [17]. The questionnaire section of this study highlights that both doctors and pharmacists were happy with the amount of information. The doctors wanted more information on the clinical events whilst community pharmacists wanted more to ensure a continuity of supply.
A review suggests that patient compliance is approximately 50% [18]. Measuring compliance is difficult and the method we have used may have contributed to the low compliance levels obtained at visit 1. The assessment of compliance at visit 2 should be accurate because baseline home stocks were available (from visit 1) and detailed prescribing and dispensing data were available. This may account for the improvement to 70% in the study group but does not explain the lack of a change in the control group. Thus, despite the lack of baseline data, the assessment of compliance at visit 1 may have been more accurate than expected and the improvement in the study group may be due to re-enforcing the counselling given pre-discharge. Higher compliance rates have been reported for the medicine reminder card with either counselling [5] or self medication [15]. These higher compliance rates could be influenced by the design of these studies. Overall these two studies used younger patients, they were prescribed fewer items, all their old medicine stocks were taken away and compliance was assessed before patients obtained a prescription refill [5].
The medication knowledge of younger patients discharged from an acute medical ward 2 weeks post-discharge has been reported to be poor [12]. Coupled to this observation the number of changes to the medication of both the study and control group patients at admission, during their hospital stay and at discharge highlight the potential for confusion. The higher compliance in the study group is likely to be associated with better knowledge as previously reported by others [1, 4, 5, 19, 20]. These five studies have not involved discharge information that is immediately posted to the GP and given to the patient. The retention of knowledge in the study group maybe related to age being a predominant factor associated with desired information [21]. No improvement in the medication knowledge of the control group patients between visit 1 and 2 could be due to many factors. The research pharmacist providing the counselling during visit 1 had very limited experience. In contrast the hospital clinical pharmacist had several years of experience providing pharmaceutical care to the elderly patients on the study ward we used. Despite the limited experience of the research pharmacist it could be argued that they were able to maintain the study group patients’ knowledge and improve compliance.
Discrepancies between the discharge prescription and the next prescription issued are caused by either poor communication from the hospital to the GP or the patient self medicating from their home stocks. Discharged patients are frequently confused whether their new treatment is a replacement for or in addition to previous therapy. A study of discharged patients reported that 32% of patients had initiated or deleted a drug from their discharge prescription and that a further 18% had altered the dose [22]. The prescription changes initiated by the patients in the control group (10 out of 40 at visit 1 – see Figure 1) highlights this potentially serious problem and the lower incidence in the study group (2 out of 43) indicates the value of the counselling.
Amongst those who were not re-admitted there were less than three changes made to the discharge prescription. The effect of a readmission accounted for the large alterations in the patient's prescription (shown in Table 3). Previously we [7). Previously we [7] and others [6, 8, 23] have highlighted the effect of poor communication when the first prescription post-discharge has been issued. As far as could be ascertained all the changes between the discharge prescription and the first visit by the GPs were intentional thereby highlighting the value of the MIDS and, judging from the questionnaires, its quick delivery. A different method has advocated the use of a letter for the patient to give to their community pharmacist to improve communication [8]. However the questionnaire results indicate that the patients were not very good at showing information to their community pharmacist although they did hand in the envelopes so that the questionnaires could be completed.
Twenty-one of the 43 study and 14 of the 40 control group patients would have had some contact with their community pharmacist either by collecting the medication at the pharmacy or during delivery. The remainder would not have had any direct contact with a pharmacist. A study by Hawksworth & Chrystyn [10] has highlighted the value of a pharmaceutical domiciliary visit to the housebound patient. These were 50 patients that had not recently been discharged and the total time to complete all the domiciliary visits and follow up all the pharmaceutical issues was 125 h. The study concluded that the visits prevented five out of the 50 patients from potential admission to hospital. The domiciliary visits to the 40 control patients, in our study, took approximately 40 h (about 1 h per patient) but this did not include travel or following up interventions. The patient was advised to see their GP when it was discovered that they had decided to self medicate from their home stocks or had stopped a prescribed medicine. More time was spent educating the control group patients during the domiciliary visits because they gave more wrong answers and it would have been unethical not to correct wrong or missing information.
Pharmaceutical interventions during the dispensing process [24] and during a domiciliary visit [10] have been reported to prevent interventions. These studies did not include many recently discharged patients. This study, of in-patient counselling by pharmacists, highlights its potential to reduce a readmission and hence healthcare costs with improved patient outcomes. The recently published programme for pharmacy in the National Health Service [25] recommends that patients should receive more support about their medicines from pharmacy. The results from this study strongly suggest that in-patient counselling of elderly patients prior to discharge, by a pharmacist, is a positive step to achieve this aim. We combined this counselling with the immediate issue of discharge information (MIDS) to GPs and patients together with a medicine reminder card. The results also suggest the potential of a pharmaceutical domiciliary visit during the first few weeks post-discharge to re-enforce the in-patient counselling. Furthermore, the results highlight how the medicine management objectives of the Government's National Health Service Framework for Older People [26] can be achieved for the discharged patient. These objectives of getting the maximum benefit from medication and minimizing unnecessary illness caused by excessive, inappropriate or inadequate consumption of medicines [27] were met, for the discharged patients, by providing pharmaceutical counselling prior to discharge and by a pharmaceutical domiciliary visit. Funding of these proactive duties for the in-patient counselling of elderly patients before discharge to their own home should be available from hospital budgets. However it is not clear who would be responsible for funding the pharmaceutical domiciliary visit.
References
- 1.Oborne A, Dodds LJ. Seamless pharmaceutical care: the needs of community pharmacists. Pharm J. 1994;253:502–506. [Google Scholar]
- 2.Hallas J, Gram LF, Goodrum E, et al. Drug related admissions to medical wards: a population based survey. Br J Clin Pharmacol. 1992;33:61–68. doi: 10.1111/j.1365-2125.1992.tb04001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Col N, Fanale JER, Kronholm P. The role of medication non-compliance and adverse reactions in the hospitalisation of the elderly. Arch Intern Med. 1990;150:841–845. [PubMed] [Google Scholar]
- 4.Binyon D. Pharmaceutical care: its pact on patient care and the hospital community interface. Pharm J. 1994;253:344–349. [Google Scholar]
- 5.Raynor DK, Booth TG, Blenkinsopp A. Effects of computer generated reminder cards on patient's compliance with drug regimes. Br Med J. 1993;306:1158–1162. doi: 10.1136/bmj.306.6886.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cochrane RA, Mandal AR, Ledger-Scott M, Walker R. Charges in drug treatment after discharge from hospital in geriatric patients. Br Med J. 1993;306:694–696. doi: 10.1136/bmj.305.6855.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith L, McGowan L, Moss-Barclay C, Wheater J, Knass D, Chrystyn H. An investigation of hospital generated pharmaceutical care when patients are discharged home from hospital. Br J Clin Pharmacol. 1997;44:163–165. doi: 10.1046/j.1365-2125.1997.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duggan C, Feldman R, Hough J, Bates I. Reducing adverse prescribing discrepancies following hospital discharge. Int J Pharm Pract. 1998;6:77–82. [Google Scholar]
- 9.Schneider J, Barber N. Provision of a domiciliary service by community pharmacists. Int J Pharm Pract. 1996;4:19–24. [Google Scholar]
- 10.Hawksworth GM, Chrystyn H. Clinical pharmacy domiciliary service – an extended role of the community pharmacist. J Appl Ther. 1997;1:325–329. [Google Scholar]
- 11.Wood SI, Calvert RT, Acomb C, Kay EA. A self-medication scheme for elderly patients improves compliance with their medication regimens. Int J Pharm Prac. 1992;1:240–241. [Google Scholar]
- 12.Eagleton JM, Walker FS, Barber ND. An investigation into patient compliance with hospital discharge medication in a local population. Int J Pharm Pract. 1993;2:107–110. [Google Scholar]
- 13.Horne R, Coombes J, Weinman J. Impact of a hospital-based programme of pharmaceutical care on elderly patients’ adherence (compliance) to medication following discharge into the community. Pharm J. 1995;255(Suppl):R10. [Google Scholar]
- 14.Williams E, Fitton F. General practitioner response to elderly patients discharged from hospital. Br Med J. 1990;300:159–161. doi: 10.1136/bmj.300.6718.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Slater S, West P, Mottram DR. A study into the correspondence between hospitals and GPs on patient discharge. Pharm J. 1993;251(Suppl):R40. [Google Scholar]
- 16.Al-Rashid A, Wcenter DJ, Reeves JA, Chrystyn H. Opinions about hospital discharge information in the UK. Part 1: General practitioners. J Soc Admin Pharm. 2001;18:91–96. [Google Scholar]
- 17.Oborne CA, Dodds L. The quality and quantity of drug-related information provided to hospital in-patients and its effects on seamless care. Pharm J. 1993;251(Suppl):R5. [Google Scholar]
- 18.Wcenter EC. Non-compliance – or how many aunts has Matilda. Lancet. 1993;342:900–903. doi: 10.1016/0140-6736(93)91951-h. [DOI] [PubMed] [Google Scholar]
- 19.Lowe CJ, Raynor DK, Courtney EA, Purvis J, Teale C. Effects of self medication programme on knowledge of drugs and compliance with treatment in elderly patients. Br Med J. 1995;310:1229–1331. doi: 10.1136/bmj.310.6989.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dhillon S, Duggan C, Joshua AE. What part pharmacists should play in providing medicines-related information. Pharm J. 2001;266:364–366. [Google Scholar]
- 21.Astrom K, Carlsson J, Bates I, et al. Desire for information about drugs. A multi-method study in general medical in-patients. Pharm World Sci. 2000;22:159–164. doi: 10.1023/a:1008783115420. [DOI] [PubMed] [Google Scholar]
- 22.Omori DM, Potyk RP, Kroenke MD. The adverse effects of hospitalisation on drug regimens. Arch Intern Med. 1991;151:1562–1564. [PubMed] [Google Scholar]
- 23.Duggan C, Bates I, Hough J. Discrepancies in prescribing – where do they occur. Pharm J. 1996;256:65–67. [Google Scholar]
- 24.Hawksworth GM, Corlett AJ, Wcenter DJ, Chrystyn H. Clinical pharmacy interventions by community pharmacists during the dispensing process. Br J Clin Pharmacol. 1999;47:695–700. doi: 10.1046/j.1365-2125.1999.00964.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Department of Health. Pharmacy in the Future – Implementing the NHS Plan. A Programme for Pharmacy in the National Health Service. London: Department of Health; 2000. [Google Scholar]
- 26.Department of Health. National Service Framework for Older People. London: Department of Health; 2001. [Google Scholar]
- 27.Department of Health. National Service Framework – Medicines and Older People. London: Department of Health; 2001. [Google Scholar]