Abstract
Background
Urogenital Chlamydia trachomatis infections are widespread, and each year many tests are performed in general practice.
Aim
First, to quantify the magnitude of stigmatisation, problems related to partner, and anxiety of infertility among men and women tested for C. trachomatis in general practice. Second, to investigate the effect of a C. trachomatis test result on planned future condom use.
Design of study
Comparative cross-sectional study.
Setting
General practices in Aarhus County, Denmark.
Method
Men and women tested for C. trachomatis in general practice were given a questionnaire about feelings of stigmatisation, fear of partner's reaction, fear of future infertility and other psychosocial side effects related to being infected or not infected with C. trachomatis.
Results
A total of 277 participated in the study. The response rates were 61% (82/135) and 54% (195/365) among infected and non-infected individuals, respectively. Among the infected individuals 32% (9/28) of the men's partners and 35% (19/54) of the women's partners were upset about the test result, 9% (5/54) of the women and 11% (3/28) of the men split with their partner, 59% (32/54) of the women and 54% (15/28) of the men expressed nervousness about infertility, and 91% (19/21) of the women but only 56% (5/9) of the men said that they would use a condom more often in the future. All these figures were significantly lower for both men and women having C. trachomatis negative test results.
Conclusion
A chlamydia test affects the individual in terms of sexuality, relation to partner, reproduction, and future contraceptive strategy. The influence is highest among women and individuals with a positive test result. These findings should be taken into account in screening programmes targeting young women and men.
Keywords: Chlamydia trachomatis, general practice, psychosocial factors, screening
INTRODUCTION
Chlamydia trachomatis is a sexually transmitted infection (STI), and the most common treatable venereal disease among adolescents1. Infection with C. trachomatis is the leading course of pelvic inflammatory disease (PID) and infertility among women1,2 and urethritis and epididymitis among men.
C. trachomatis infection remains asymptomatic in up to 75% of all patients and intervention aimed at testing asymptomatic individuals would not only serve to aid diagnosis and treatment of unrecognised infections before the onset of complications like PID, but would break the chain of transmission.
In general practice in Denmark patients are tested in four cases: patients with symptoms; as part of a partner notification programme; prior to transcervical procedure; and, furthermore, as part of opportunistic screening3. The total annual number of tests taken in Denmark exceeds 250 000 (total population 5 600 000). Nine out of ten tests are taken in general practice.
Intensive testing for C. trachomatis is performed without precise knowledge of its psychosocial consequences. A single qualitative British study4 of women diagnosed with C. trachomatis identified three main areas of concern: perception of stigma associated with STI; uncertainty about future reproductive health; and anxiety about the partner's reaction to the diagnosis. The size of this problem remains unknown even when the current level of testing is high and is expected to rise upon the introduction of future universal screening programmes.
How this fits in
Little is known about the psychosocial aspects of testing for chlamydia. One qualitative study identified three topics to be of concern for women tested positive for chlamydia. Women are more concerned with stigmatisation, partner's reaction and future reproductive health than men. Fewer men than women consider changing their condom use, regardless of the diagnosis. Screening young men and women for chlamydia must include non-stigmatising information and an offer to discuss the result with a healthcare worker.
To our knowledge, no data on the psychosocial impact of testing have been collected on men and chlamydia-negative women.
The aim of the study was therefore to quantify the concerns related to a test for C. trachomatis in general practice, and the reactions to a positive or a negative test result.
METHOD
Setting
The study took place in Aarhus County, Denmark. Aarhus County has 640 000 inhabitants and 274 general practices, with a total of 450 GPs.
Development of questionnaire
The questionnaire was developed on the basis of three topics identified to be of concern to women tested positive for C. trachomatis:4 stigmatisation, partner's reaction and future reproductive health. For these questions the individuals were asked if they fully agreed, somehow agreed, somehow disagreed, or fully disagreed with the statement. In addition, data were collected on demographics, sexual behaviour, reasons for contacting the GP, symptoms at the time of testing and knowledge of the chlamydia infection. A further 15 questions addressed issues related to partner status, use of contraception, and earlier venereal diseases. For these questions it was possible to answer yes or no. Same questionnaire was used for participants with a negative and a positive test result for C. trachomatis.
The questionnaire was piloted on the first 20 people selected for the study. The pilot revealed no concerns with the questionnaire, which was subsequently used throughout the study.
Design
All samples for C. trachomatis testing in general practice in Aarhus are analysed at the Department of Clinical Microbiology, Aarhus University Hospital. Potential participants were therefore identified from all samples submitted to the Department of Clinical Microbiology. Criteria for inclusion were aged above 18 years and the acceptance of the GP performing the testing for C. trachomatis to recruit individuals for the study.
Tested individuals were included from 18 March to 31 May 2002. All individuals tested positive for C. trachomatis in the study period were considered for inclusion in the study, and for each individual with a C. trachomatis-positive test result, four individuals with a negative test result for C. trachomatis were identified. Matching was done for sex.
Two weeks before initiation of the study, all GPs in Aarhus County received a letter with information on the study. GPs were given the opportunity not to take part in the study and 25 general practices refused.
When a tested individual was considered for inclusion in the study, the GP was requested to ask the tested man or women if they could send them further information about the study. No reminder was sent to GPs who did not respond. If the patient accepted enrolment, they gave permission that the GP could fax their address to the study centre, and a questionnaire, information about the study and a pre-stamped, pre-addressed envelope was then sent to the participants. The time from performing the test at the practice to the time the patient received the questionnaire was 1 week (maximum). The participants who did not return the questionnaire after 2 weeks were sent a reminder.
Outcome measures
The main outcome measures were proportion of chlamydia tested individuals reporting stigmatisation, fear of partner's reaction, anxiety of infertility, and contraceptive strategy before and after the test.
Statistical methods
Data were manually extracted from the questionnaire, and entered in to EpiData 2.0. The answers to each question were categorised into two groups. Individuals answering that they fully agreed or somehow agreed were categorised as ‘agreeing’, whereas individuals answering that they somehow disagreed or fully disagreed were categorised as ‘disagreeing’.
The statistical analyses were performed with Fisher's exact test (two-tailed) and χ2 test with Yates correction. The significance level was set to P<0.01 to account for multiple testing of the questionnaire items.
Mantel–Haenszel analysis was made to adjust the P-value for age-associated differences and in this analysis the participants were divided into two age groups: individuals aged 18–25 years (n = 183) and individuals aged 26–43 years (n = 94).
Principal component factor analyses with Varimax rotation procedures were performed in order to summarise the relationship between psychosocial items and produce an orthogonal solution.5 SPSS 10.0 and STATA SE 8.0 was used for analysing data.
RESULTS
Participants
A total of 277 individuals were included in the study. Of these 54 (20%) were chlamydia-infected women, 122 (44%) non-infected women, 28 (10%) chlamydia-infected men, and 73 (26%) non-infected men. The response rate among those with chlamydia infection was 61% (82/135) and 53% (195/365) among those not infected, corresponding to a relative response rate of 1.14.
Figure 1 shows the drop outs during the study. The age range was 18–43 years (mean age = 25 years, and median age = 24 years). Symptoms were reported by 40% (40/101) of men and 48% (84/176) of women participating in the study. Among those infected 50% (14/28) of men and 65% (35/54) of women reported symptoms before diagnosis and treatment.
Figure 1.
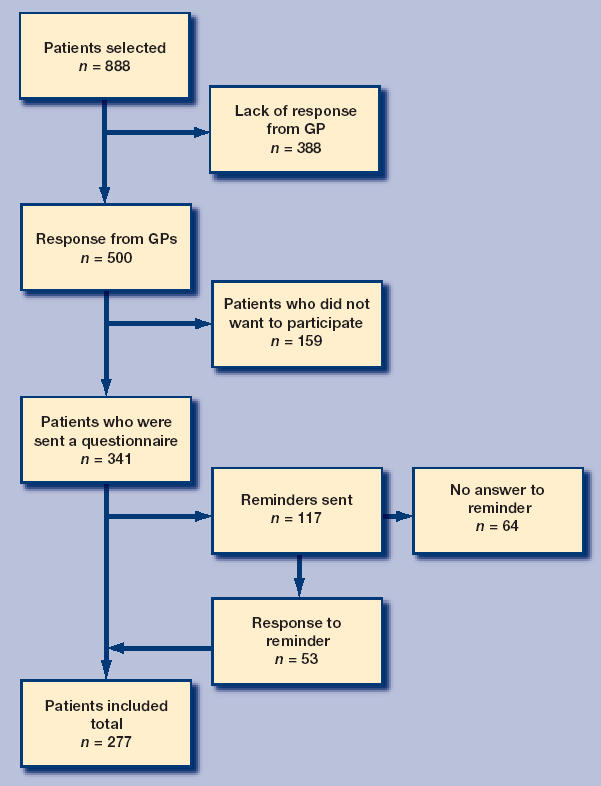
Flowchart for the study showing the amount of participants and non-participants and reasons for not being included in the study.
A regular partner was reported by 64%(113/176) of the women and 70% (71/101) of the men. A total of 45% (126/277) of the participants were students, 33% (91/277) were workers, 8% (22/277) were apprentices, 4% (12/277) were unemployed and 8% (21/277) were in non-replaceable categories. Fiftyeight per cent (160/277) had two or less sexual partners during the previous year while 42% (117/277) had three or more. Both men and women had a high degree of general knowledge of chlamydia infection (Table 1).
Table 1.
Knowledge about chlamydia. General knowledge of Chlamydia trachomatis infections among participating individuals.
| Yes n (%) | No n (%) | Do not know n (%) | |
|---|---|---|---|
| Is chlamydia sexually transmitted? | 270 (97.4) | 0 (0.0) | 4 (1.4) |
| Can you infect other people without knowing it? | 252 (91.0) | 8 (2.9) | 14 (5.1) |
| Can chlamydia be cured? | 266 (96.0) | 2 (0.7) | 5 (1.8) |
| Can you have chlamydia more than once? | 258 (93.0) | 1 (0.4) | 14 (5.1) |
| Can chlamydia cause female infertility? | 256 (92.4) | 3 (1.1) | 15 (5.4) |
| Will you always have symptoms when you are infected? | 7 (2.6) | 227 (81.9) | 39 (14.1) |
| Are condoms protective against chlamydia? | 260 (93.9) | 5 (1.8) | 9(3.2) |
Data are merged for men and women as no difference was observed between the two sexes. (n = 277). Missing data in all rows as not all the questions were answered by the participants.
Having the test offered by the GP
In the questionnaire it was possible for the participants to mark more than one reason for having a C. trachomatis test. All 277 participants answered the question regarding reason for testing and they gave a total of 323 reasons for the test.
Twenty-two per cent (71/323) of the participants were not aware that they could be infected, but were tested because the GP proposed a chlamydia test (Table 2). Seventeen per cent (55/323) were tested because they thought they had been exposed to chlamydia, 9% (27/323) because their partner was infected, 5% (17/323) because they had previously had chlamydia and had a follow-up appointment, 16% (51/323) because they had a new partner and wanted to be tested, 20% (66/323) because they had symptoms that they related to chlamydia, 6% (19/323) because their partner had suggested a test and 5% (17/323) because a friend had suggested a test.
Table 2.
Reaction to being offered a test for Chlamydia trachomatis by the GP.
| Women (n = 53) | Men (n = 18) | ||||
|---|---|---|---|---|---|
| Agree n (%) | Agree n (%) | P-valuea | OR | 95% CI | |
| I do not think that I am the ‘type of person’ who has chlamydia | 32 (60) | 14 (77.8) | 0.470 | 0.61 | 0.17 to 2.27 |
| I felt satisfied with the test offer | 42 (79) | 16 (88.9) | 0.360 | 0.42 | 0.07 to 2.56 |
| I felt astonished by having the test offer | 28 (53) | 13 (72.2) | 0.475 | 0.64 | 0.18 to 2.18 |
| I felt stigmatised by having the test offer | 7 (13.2) | 1 (5.6) | 0.308 | 3.45 | 0.32 to 36.80 |
| It had no emotional impact on me | 7 (13.2) | 1 (5.6) | 0.298 | 3.45 | 0.32 to 36.80 |
Among all participants, 22% (71/323) were not aware that they could be infected with C. trachomatis and were only tested upon the GP's suggestion. The table shows the reaction to the test offer in this subgroup of participants and participants were allowed to report more than one reaction. P-values and odds ratios reflect the difference between tested women and men. Data are adjusted for age by a Mantel–Haenszel analysis.
Adjusted for age. OR = odds ratio.
A total of 55% (28/53) of the women and 72% (13/18) of the men were astonished to receive the test offer (P = 0.475), but most of them (four out of five) were also satisfied with the offer. Only 13% (7/53) of the women and 6% (1/18) of the men felt stigmatised by being offered the test.
Psychosocial impact of test result
Table 3 shows the psychosocial impact of having a C. trachomatis positive test result versus having a C. trachomatis negative test result.
Table 3.
Psychosocial impact of having a positive test result for Chlamydia trachomatis.
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Infected Agree (n = 54) n (%) | Non-infected Agree (n = 122) n (%) | P-valuea | Infected Agree (n = 28) n (%) | Non-infected Agree (n = 73) n (%) | P-valuea | |
| Stigmatisation | ||||||
| • It is a private affair so I will not tell anyone | 29 (54) | 57 (47) | 0.448 | 14 (50) | 41 (56) | 0.549 |
| • I feel stigmatised talking about it | 17 (32) | 17 (14) | 0.012 | 8 (29) | 13 (18) | 0.326 |
| • I think it is embarrassing to talk about the test | 18 (33) | 17 (14) | 0.009 | 13(46) | 13 (18) | 0.005 |
| • I have a need for someone to talk to | 33 (61) | 50 (41) | 0.082 | 7 (25) | 18 (25) | 0.883 |
| Reaction to test answer | ||||||
| • I felt upset | 31 (57) | 9 (7) | <0.001 | 4 (14) | 0 (0) | 0.007 |
| • I felt despair | 32 (59) | 6 (5) | <0.001 | 6 (21) | 3 (4) | 0.022 |
| • I felt embarrassed | 23 (43) | 4 (3) | <0.001 | 8 (29) | 2 (3) | <0.001 |
| • It had no emotional impact on me | 10 (19) | 39 (32) | 0.047 | 9 (32) | 25 (34) | 0.708 |
| Relation to partner | ||||||
| • I feel ‘dirty’ | 16 (30) | 8 (7) | <0.001 | 7 (25) | 0 (0) | <0.001 |
| • I do not feel sexually attractive | 20 (37) | 8 (7) | <0.001 | 5 (18) | 7 (10) | 0.450 |
| • I feel relieved | 21 (40) | 84 (70) | <0.001 | 12 (43) | 56 (77) | <0.001 |
| • My partner was upset | 19 (35) | 6 (5) | <0.001 | 9 (32) | 3 (4) | <0.001 |
| • My partner was disappointed | 5 (9) | 2 (2) | 0.032 | 5 (18) | 3 (4) | 0.017 |
| •My partner was understanding | 42 (78) | 74 (61) | 0.598 | 21 (75) | 55 (75) | 0.891 |
| • My partner and I split up | 5 (9) | 1 (1) | 0.003 | 3 (11) | 0 (0) | 0.006 |
| Anxiety of infertility | ||||||
| • I do not think it will be a problem for me/my partner to become pregnant | 29 (54) | 74 (61) | 0.220 | 16 (57) | 53 (73) | 0.199 |
| • I do not consider my/my partner's chances of becoming pregnant different now compared with before | 29 (54) | 88 (72) | 0.005 | 19 (68) | 59 (81) | 0.146 |
| • I am nervous that my/my partner's chances of becoming pregnant are reduced | 32 (59) | 24 (20) | <0.001 | 15 (54) | 14 (19) | 0.002 |
| • My wish to become pregnant is more intense after the test than before | 10 (19) | 12 (10) | 0.191 | 4 (14) | 13 (18) | 0.489 |
All participants (C. trachomatis positive and C. trachomatis negative) were asked about their feelings and reaction to the C. trachomatis test result. They were given certain statements related to stigmatisation, reaction to test result, relation to partner and anxiety of infertility and were asked to mark if they fully agreed, somehow agreed, somehow disagreed or fully disagreed to the statement. The table shows the proportion of individuals who agreed (fully or somehow) to the statements. P-values reflect the difference between the infected and non-infected groups.
P-value is adjusted for age by a Mantel–Haenszel analysis.
Stigmatisation
Half of the tested individuals, regardless of infectious state, felt that the test was a private affair and they would not tell anyone about it. More infected women than infected men felt a need for someone with whom they could discuss the test result (61 versus 25%, P = 0.003). Thus, although more women than men had a need to talk to someone, the presence of a trusted other was something that mattered to both participants with a positive and a negative test result. One-third of both infected women (17/54 = 32%) and men (8/28 = 29%) agreed that they felt stigmatised telling their friends about the test. This proportion was almost equal to the proportion of women (18/54 =33%) and men (13/28 = 46%) who felt embarrassed telling about the test.
Reaction to test result
Lack of emotional impact was only reported by 19% (10/54) of the infected women and 32% (9/28) of the infected men. In contrast, there was no difference between the emotional impact for infected and uninfected men (32 versus 34%, P = 0.708). Having a positive test result was related to a high degree of being upset (57.4%), despair (59.3%), and embarrassed (42.6%) among women, but among infected men these reactions were less outspoken (14.3, 21.4 and 28.6%, respectively).
Relation to partner
Five of the infected women (5/54 = 9%) and three of the infected men (3/28 = 11%) left their partner, or were left by their partner, as a consequence of the test result.
Considering partner-related reactions associated with a positive chlamydia test, 30% (16/54) of the women and 25% (7/28) of the men felt ‘dirty’ by knowing that they were infected. In total, 37% of the infected women felt sexually unattractive compared with 18% of the men (P = 0.08).
Partners of the infected individuals were upset in 34% of the cases (28/82), but at the same time 77% (63/82) of infected participants reported their partner to be supportive.
Anxiety of infertility
Fifty-nine percent (32/54) of the infected women were more anxious about infertility after the test result than before. This was significantly more than the 20% (24/122) of uninfected women who reported being more anxious of infertility after being aware of the test result (P<0.001). The corresponding figures for men were 54 and 19%, respectively (P = 0.002). One in seven (39/277) agreed that they had an intensified wish for pregnancy after the C. trachomatis test result, but it was neither related to being infected or uninfected nor to being women or man.
Future contraceptive use
Table 4 shows that among individuals with no regular partner, 56% (5/9) of the infected men compared with 91% (19/21) of the infected women reported that they would use condom more often now than before the test result (P = 0.053). For uninfected individuals the corresponding figures were 50% (9/18) for men and 60% (24/40) for women, respectively.
Table 4.
Considerations on future condom use among individuals with no regular partner.
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Infected Agree (n = 21) n (%) | Non-infected Agree (n = 40) n (%) | P-valuea | Infected Agree (n = 9) n (%) | Non-infected Agree (n = 18) n (%) | P-valuea | |
| My partner or I will use a condom more often | 19 (91) | 24 (60) | 0.053 | 5 (56) | 9 (50) | 0.802 |
| I will only use a condom with a new partner | 13 (62) | 26 (65) | 0.609 | 5 (56) | 15 (83) | 0.134 |
| My use of contraceptive choice will probably not change | 6 (29) | 24 (60) | 0.007 | 5 (56) | 12 (67) | 0.508 |
Among all participants, 32% (88/277) had no regular partner and this subgroup of the population was asked how they would consider their future use of condom. P-values reflect the difference between infected and non-infected.
P-value is adjusted for age by a Mantel–Haenszel analysis.
Principal component factor analysis
We performed an exploratory principal component factor analysis summarising the 19 items regarding psychosocial consequences of C. trachomatis testing (shown in Table 3). The Kaiser Criterion (eigenvalue >1.0) indicated a five-factor solution. One of the items (‘My wish to become pregnant is more intense after the test than before’) did not fit with any of the categories and was removed. After repeated principal component factor analysis the five factors had eigenvalue >1.0 and accounted for 62.3% of the total variance (28.7, 10.1, 8.9, 8.3 and 6.2, respectively). The results of the factor analysis including main factor loadings are shown in Table 5.
Table 5.
Principal component factor-based subscales with respective items and item loadings.
| Factor | Label | Item | Loading |
|---|---|---|---|
| I | Stigmatisation | It is a private affair so I will not tell anyone | 0.67 |
| I feel stigmatised talking about it | 0.74 | ||
| I think it is embarrassing to talk about the test | 0.79 | ||
| II | Reaction to test answer | I felt upset | 0.77 |
| I felt despair | 0.72 | ||
| I felt embarrassed | 0.68 | ||
| I felt ‘dirty’ | 0.49 | ||
| I do not feel sexually attractive | 0.61 | ||
| I feel relieved | −0.58 | ||
| My partner was upset | 0.62 | ||
| III | Relation to partner | My partner was disappointed | 0.70 |
| My partner was understanding | −0.68 | ||
| My partner and I split up | −0.72 | ||
| IV | Anxiety of infertility | I do not think it will be a problem for me/my partner to become pregnant | 0.80 |
| I do not consider my/my partner's chances of becoming pregnant different now compared with before | 0.88 | ||
| I am nervous that my/my partner's chances of becoming pregnant are reduced | −0.62 | ||
| V | Emotional impact | I have a need for someone to talk to | 0.69 |
| It had no emotional impact on me | −0.68 | ||
Factor I includes variables related to thoughts about the test. We named it ‘stigmatisation’.
Factor II includes variables related to the test answer. We named it ‘reaction to test answer’. Item ‘my partner was upset’ was thought to belong to the factor ‘relation to partner’, but was correlated with items from category ‘reaction to test answer’ and thus kept there.
Factor III includes variables related to the partner of the tested. We named it ‘relation to partner’.
Factor IV includes variables related to thoughts about infertility. We named it ‘anxiety of infertility’.
Factor V includes variables related to emotional impact. We named it ‘emotional impact’.
DISCUSSION
Summary of main findings
In this study, we quantified the psychosocial impact related to C. trachomatis testing in general practice. In general the participants were satisfied with being offered a chlamydia test. A positive test result had an emotional impact on four out of five individuals, and women in particular needed someone with whom they could discuss the test result. One in ten patients infected with C. trachomatis split with their partner due to the test, and more than half of the infected participants were anxious about infertility after the test result. Only half of the uninfected individuals with no regular partner would intensify their use of condoms as a result of the test.
Strengths and limitations of the study
Problems defined in qualitative studies must be quantified in order to define to which extent the issue addressed has implications for clinical practice. To our knowledge, this study is the first to quantify the psychosocial impact on C. trachomatis testing and, indeed, the first study on the psychosocial consequences of testing men. Our study enjoys the major advantage that we had the possibility to develop a questionnaire based on an earlier published qualitative study4 among individuals tested positive for C. trachomatis.
However, since the British qualitative study only included interviews among women tested positive for C. trachomatis, men and women may think differently about these issues, as may the British and the Danish population in general. Another limitation in our study might lie in the high number of dropouts. However, the dropouts were mainly due to GPs who refused or forgot to inform their patients about the study, and these dropouts will only have caused limited bias in our study. A bias may, however, have been introduced because of the tested individuals who did not want to participate in the study, and it could have been interesting to be able to compare relevant parameters between participants and non-participants. Unfortunately we are not able to do so in our present study design.
Comparison with existing literature
Overall, the population tested had good knowledge about C. trachomatis infections as also reported for other populations.6,7 Earlier studies have shown that knowledge of STIs and sexual behaviour is not necessarily correlated,8–10 but since the large majority of participants in our study were well informed about STIs, we made no similar analysis of the correlation between knowledge and sexual behaviour.
In two qualitative studies from Britain,4,1 it was found that the C. trachomatis diagnosis was associated with thoughts about sexual behaviour, partner's reaction, and contraceptive use. Our findings support this, but we were also able to show that the vast majority of tested women, whether positive or negative, had such thoughts. In light of the many tests being performed each year, chlamydia testing, therefore, has a substantial psychosocial impact on the community.
Studies has also been conducted among people who were diagnosed with an STI at sexual health clinics.12 In these studies, anxiety, stigma and isolation were the major topics and having an STI was associated with feeling ‘dirty’. In our study, we found that more than a quarter of the individuals who had a diagnosis of C. trachomatis felt ‘dirty’ or felt sexually unattractive and this was a lot different from what was felt by individuals who were tested negative. Thus stigmatisation is, indeed, a problem in relation to a C. trachomatis diagnosis like in other STIs. It is important to note that screening for STIs including C. trachomatis makes the connection between infection and sex, and therefore demands a careful approach to the patients.13
Men reacted differently from women. In general, they were less influenced by having a test offer and a positive test result. In particular, the need for someone to talk to was lower among men than among women. Of particular interest is the high proportion of men who reported that they would not use condom more often after than before they were diagnosed with a chlamydia infection. This could reflect that men's major reason for choice of contraception was guided more by a wish to avoid pregnancy rather than by a wish to be protected from an STI.14 The finding should lead to a re-evaluation of the counselling procedure for infected men. There seems to be a need for a stronger focusing on education of men with regard to the responsibility they have in connection with an STI that mainly has complications for women.15,16
Despite the reactions to a positive, as well as a negative, test result, a remarkable 90% of the participants in this study were actually satisfied with being offered a test. This reflects the results from many other studies assessing participation rates in universal screening programmes.17 Universal screening programmes have shown to be instrumental in lowering the complication rated for the individuals2 and the prevalence of disease in the community,18 and it may therefore be speculated that universal screening programmes may become part of future public health measures to combat the problems of C. trachomatis infections. If such universal screening programmes are to be introduced, it is important to consider the findings of this study. Individuals will feel stigmatised by having a test offer, there will be a need for someone to talk to regardless of the test result, and there will still be a substantial need for counselling, in particular of infected men.
Implications for clinical practice
The findings of our study should be taken into account when counselling individuals tested for C. trachomatis in general practice, and for each patient it seems important to identify the individuals who need help to deal with the situation. In areas where major screening programmes are considered, the possible benefits of the programme in preventing especially fertility complications should be weighted against the psychosocial consequences of more widespread testing as they are defined in our study.
Acknowledgments
With thanks to statistician Ineta Sokolowski for her superior work with some of the analysis. We are grateful to the GPs in Aarhus County who were willing to include patients in this study. We are grateful for the staff at the Department of Clinical Microbiology, Aarhus University Hospital, Aarhus for their great help.
Funding body
Institute of Experimental Clinical Research, Skejby Hospital, Aarhus University Hospital. The Danish National Research Foundation for Primary Care
Ethics committee
Scientific Ethics Committee in the County of Aarhus approved the study (20020013)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Cates W, Jr, Wasserheit JN. Genital chlamydial infections: epidemiology and reproductive sequelae. Am J Obstet Gynecol. 1991;164:1771–1781. doi: 10.1016/0002-9378(91)90559-a. [DOI] [PubMed] [Google Scholar]
- 2.Scholes D, Stergachis A, Heidrich FE, et al. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. N Engl J Med. 1996;334:1362–1366. doi: 10.1056/NEJM199605233342103. [DOI] [PubMed] [Google Scholar]
- 3.Moller JK, Andersen B, Olesen F, Ostergaard L. Reasons for Chlamydia trachomatis testing and the associated age-specific prevalences. Scand J Clin Lab Invest. 2003;63:339–345. doi: 10.1080/00365510310002031. [DOI] [PubMed] [Google Scholar]
- 4.Duncan B, Hart G, Scoular A, Bigrigg A. Qualitative analysis of psychosocial impact of diagnosis of Chlamydia trachomatis: implications for screening. BMJ. 2001;322:195–199. doi: 10.1136/bmj.322.7280.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mainous AG., III Factor analysis as a tool in primary care research. Fam Pract. 1993;10:330–336. doi: 10.1093/fampra/10.3.330. [DOI] [PubMed] [Google Scholar]
- 6.Persson E. The sexual behaviour of young people. Br J Obstet Gynaecol. 1993;100:1074–1076. doi: 10.1111/j.1471-0528.1993.tb15168.x. [DOI] [PubMed] [Google Scholar]
- 7.Zimmer JC, Thurston WE. Attitudes, beliefs, and practices of nursing students concerning HIV/AIDS: implications for prevention in women. Health CareWomen Int. 1998;19:327–342. doi: 10.1080/073993398246304. [DOI] [PubMed] [Google Scholar]
- 8.Fouchard JR, Worm AM. Viden, holdning og adfaerd blandt chlamydia-patienter. Perspektiver for forebyggelsen. [Knowledge, attitude and behavior among patients with chlamydia. Perspectives for prevention] Ugeskr Laeger. 1997;159:5085–5088. [PubMed] [Google Scholar]
- 9.Johnson LS, Rozmus C, Edmisson K. Adolescent sexuality and sexually transmitted diseases: attitudes, beliefs, knowledge, and values. J Pediatr Nurs. 1999;14:177–185. doi: 10.1016/S0882-5963(99)80006-2. [DOI] [PubMed] [Google Scholar]
- 10.Andersson-Ellstrom A, Forssman L, Milsom I. The relationship between knowledge about sexually transmitted diseases and actual sexual behaviour in a group of teenage girls. Genitourin Med. 1996;72:32–36. doi: 10.1136/sti.72.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.France C, Thomas K, Slack R, James N. Psychosocial impacts of chlamydia testing are important. BMJ. 2001;322:1245. [PMC free article] [PubMed] [Google Scholar]
- 12.Holgate HS, Longman C. Some peoples' psychological experiences of attending a sexual health clinic and having a sexually transmitted infection. J R Soc Health. 1998;118:94–96. doi: 10.1177/146642409811800210. [DOI] [PubMed] [Google Scholar]
- 13.Duncan B, Hart G. A social science perspective on screening for Chlamydia trachomatis. Sex Transm Infect. 1999;75:239–241. doi: 10.1136/sti.75.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper ML, Agocha VB. Powers AM. Motivations for condom use: do pregnancy prevention goals undermine disease prevention among heterosexual young adults? Health Psychol. 1999;18:464–474. doi: 10.1037//0278-6133.18.5.464. [DOI] [PubMed] [Google Scholar]
- 15.Duncan B, Hart G. Sexuality and health: the hidden costs of screening for Chlamydia trachomatis. BMJ. 1999;318:931–933. doi: 10.1136/bmj.318.7188.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christianson M, Johansson E, Emmelin M, Westman G. ‘One-night stands’ — risky trips between lust and trust: qualitative interviews with Chlamydia trachomatis infected youth in North Sweden. Scand J Public Health. 2003;31:44–50. doi: 10.1080/14034940210134158. [DOI] [PubMed] [Google Scholar]
- 17.Andersen B, Olesen F, Moller JK, Ostergaard L. Population-based strategies for outreach screening of urogenital Chlamydia trachomatis infections: a randomised, controlled trial. J Infect Dis. 2002;185:252–258. doi: 10.1086/338268. [DOI] [PubMed] [Google Scholar]
- 18.Ostergaard L, Andersen B, Moller JK, Olesen F. Home sampling versus conventional swab sampling for screening of Chlamydia trachomatis in women: a cluster-randomised 1-year follow-up study. Clin Infect Dis. 2000;31:951–957. doi: 10.1086/318139. [DOI] [PubMed] [Google Scholar]


