ABSTRACT
Radical surgery combined with postoperative radiation is recommended to achieve the best outcomes in patients suffering from malignant anterior skull base tumors. However, information on the impact of such treatment on the quality of life of these patients is sparse. This retrospective study evaluated quality of life in patients with anterior skull base malignancies after transdural resection and radiotherapy. At follow-up, 36% of the patients were alive (mean survival time, 39 months). Only 45% of the patients were able to work in their previous occupation a mean of 15 months after surgery. At follow-up, 58% of the patients had a recurrent tumor. The mean quality of life index was 42 points (range, 0 to 100). The lowest values were on the job item, and the highest mean value was on the family item. All patients, dependents, or both would agree to surgery in the future. Based on these findings, quality of life after transdural surgery for the treatment of anterior skull base malignancies seems to be low.
Keywords: Quality of life, malignancies, anterior skull base, tumor
Sekhar and Moller,1 among others,2,3,4,5 recommended radical surgery combined with postoperative radiation to maximize outcomes in patients suffering from malignant anterior skull base tumors. Advances in combined transcranial and transfacial approaches has improved survival for patients with these tumors. Despite modern techniques, surgery for these tumors is always challenging for both surgeon and patient. High recurrence rates (about 70%) and low survival rates (about 50%) 2 years after such surgery question whether surgical intervention can be justified. Data on the impact of surgery on quality of life after transdural resection of malignancies of the anterior skull base are sparse. Boyle and associates2 and Lang and others6,7,8 have discussed the need for more studies on this issue. Therefore, this study attempted to provide data on quality of life after skull base surgery.
METHODS
The clinical data and perioperative complications of all patients treated for malignancies of the anterior skull base in our department between 1995 and 2001 were reviewed retrospectively. Surgery was performed in collaboration with the Department of Ear, Nose, and Throat Surgery and the Department of Neurosurgery.
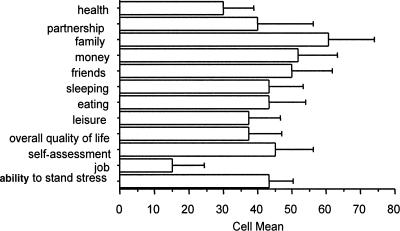
Postoperatively, outcome was assessed by sending patients a modified questionnaire following Blau.9 This questionnaire consists of 11 categories (job, leisure, eating, sleeping, friends, money, family, partnership, health, self-assessment, and the overall quality of life). Each item is rated on a scale ranging from 0 to 100, with 0 indicating nonexistent and 100 indicating best possible outcome. According to Blau, values above 70 indicate a fairly successful condition of living. A ranking between 70 and 50 indicates a painful situation but adequate coping. Values below 50 are reported by persons suffering considerably in their present situation.9
Finally, a quality of life index (QoLI) was calculated. Favorable outcomes were defined as a score above 49 points on the QoLI. An unfavorable outcome was a score below 50. Patients and relatives were asked whether they would agree to surgery in the future.
Follow-up was performed a mean of 40 months after surgery. In six cases relatives answered the questionnaires because the patients were no longer alive. Six patients were able to answer on their own. The remaining two patients died perioperatively.
RESULTS
Fourteen patients were identified from our data bank. There were 8 men and 6 women (mean age, 58 years; range, 42 to 74 years).
Seven patients (50%) suffered from a squamous epithelial carcinoma, six (43%) had an adenocarcinoma, and one patient (7%) suffered from an esthesioneuroblastoma. In nine cases (64%), the meninges had been infiltrated by tumor. In all patients bony infiltration of the skull base was observed, and 93% of the tumors infiltrated the paranasal sinus (Table 1). In 79% of the patients a frontal transdural resection was performed. Two patients underwent a combined temporal/transfacial and an orbital approach, respectively. Another patient underwent three subsequent operations via a frontal, transfacial, and endonasal approach. In 79% of the patients, gross total resection was achieved. All patients underwent postoperative radiation (30 to 64 Gray). One patient also received additional chemotherapy.
Table 1.
Frequency of Tumor Location and Infiltrated Structures
| Patient | Location and Infiltration |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Paranasal Sinus | Ethmoidal Labyrinth | Frontal Sinus | Dura Mater | Nasal Cavity | Frontobasal Bone | Sphenoid | Orbitonasal Bone | Maxillary Sinus | Lateral Wall and Floor of Orbita | Frontal Lobe | Temporobasal Bone | Temporal Lobe | Nervus Maxillaris | Rectus Muscle | |
| 1 | x | x | x | x | |||||||||||
| 2 | x | x | x | x | x | x | x | ||||||||
| 3 | x | x | x | x | x | x | x | ||||||||
| 4 | x | x | x | x | x | x | |||||||||
| 5 | x | x | x | x | x | x | x | x | x | x | |||||
| 6 | x | x | x | x | x | x | |||||||||
| 7 | x | x | x | x | x | ||||||||||
| 8 | x | x | x | x | x | x | x | ||||||||
| 9 | x | x | x | x | x | x | |||||||||
| 10 | x | x | x | x | x | x | x | ||||||||
| 11 | x | x | x | x | x | x | x | x | x | ||||||
| 12 | x | x | x | x | x | x | x | x | |||||||
| 13 | x | x | x | x | x | ||||||||||
| 14 | x | x | x | x | x | x | x | ||||||||
| % | 92.9 | 71.4 | 71.4 | 64.3 | 64.3 | 57.1 | 57.1 | 57.1 | 50 | 35.7 | 14.2 | 7.1 | 7.1 | 7.1 | 7.1 |
Anterior cranial fossa cerebrospinal fluid rhinorrhea was treated by lumbar drainage in 21% of the patients without further consequences. Two patients (14%) died perioperatively; both suffered from early postoperative intracranial bleeding.
At follow-up, 36% of the patients were still alive (mean survival time, 39 months). Survival time was influenced by tumor type. Patients with a squamous epithelial carcinoma survived a mean of 35.5 months. Patients suffering from adenocarcinoma survived only 23.2 months. The survival of patients with tumor infiltrating the meninges was shorter than the survival time of patients with no evidence of such infiltration (mean, 39.8 months versus 49.5 months). The 3-year survival rate for patients with meningeal infiltration was 60% compared with 100% in patients without infiltration. A mean of 15 months after surgery, 58% of the patients showed a tumor recurrence.
At follow-up only 42% of the patients were free of symptoms. Most patients suffered from headache (25%), and 17% complained of nasal secretions. Two patients developed postoperative seizures. Five patients complained of visual deficits, three of whom underwent unilateral enucleation. Seventy-three percent of the patients experienced postoperative anosmia, and 18% were aphasic and hemiparetic. All patients and dependents stated that they would agree to surgery in the future.
In our study population, only 45% of the individuals were able to return to their previous job. The mean QoLI was 42 points, the lowest values were found on the job item (15 points, mean), and the highest mean value was found in the family item with 61 points. See also Figure 1 and Table 2.
Figure 1.
Results of the questionnaire regarding quality of life.
Table 2.
Quality of Life for Different Items According to Different Patient Subgroups
| Quality of Life | All Patients Mean | Still Alive after Hospital Stay Mean | P Mean | R Mean | Min P/R | Max P/R |
|---|---|---|---|---|---|---|
| P, estimation by patients; R, estimation by relatives; Min, minimum; Max, maximum. | ||||||
| Job | 15 | 21.4 | 18 | 15 | 0/0 | 80/60 |
| Self-assessment | 45 | 60 | 82 | 32.5 | 50/10 | 100/60 |
| Leisure | 37.5 | 50 | 64 | 46 | 10/30 | 70/100 |
| Eating | 43.3 | 57.8 | 72 | 40 | 40/0 | 100/80 |
| Sleeping | 43.3 | 57.8 | 60 | 55 | 10/40 | 100/80 |
| Friendship | 50 | 66.7 | 72 | 60 | 10/20 | 100/90 |
| Money | 51.7 | 68.9 | 70 | 67.5 | 40/20 | 100/100 |
| Family | 60.8 | 81.1 | 90 | 70 | 50/10 | 100/100 |
| Partnership | 40 | 57.1 | 60 | 25 | 0/0 | 100/100 |
| Health | 30 | 40 | 48 | 30 | 10/0 | 100/50 |
DISCUSSION
In this series only 36% of our patients were still alive by follow-up. This rate is at the lower limit of the reported survival rates in the literature (44 to 74%).2,10 It is well known that histopathological diagnosis and grade are significant prognostic factors. Consistent with the literature, we found that patients suffering from adenocarcinomas had a shorter survival time than patients treated for squamous epithelial carcinomas.4
As a predictor of survival, meningeal infiltration is controversial. Kraus et al11 reported a survival rate of only 14% in patients with dural infiltration compared with 83% in patients without evidence of such infiltration. Clayman and coworkers12 reported no long-time survivor in their group of patients with dural infiltration. In our study the 3-year survival rate in patients with dural infiltration was 60% and 100% in patients without such infiltration. Long-time survival rate seems to be significantly influenced by dural infiltration, but it seems better than previously reported.
The recurrence rate of 58% in our study seems to be high, but it is within the range reported in the literature. Despite radical surgery, Pitman and colleagues3 and Naficy and associates13 achieved recurrence rates of 71 and 76%, respectively.
Most studies in the literature dealing with malignant tumors of the anterior skull base discuss the survival rates, perioperative complications, recurrence rates, and surgical procedures employed for treatment of these lesions.2 The literature describing overall outcome, especially quality of life after these procedures, is sparse. Lang et al6 reported 14 patients suffering from a mixture of deep-seated lesions in the central skull base region using parts of the SF 36 to measure quality of life. They found that only 50% of the patients were scored as having normal values postoperatively, indicating an adequate quality of life.
Considering the QoLI of all patients according to Blau,9 we found that only 50% of the patients scored above 50. Among the survivors 66.7% of the patients were above this limit. The worst mean values were found on the items on job (21.4), health (40), and leisure (50). The best quality of life was reached on the items family (81.1), money (68.9), and friendship (66.7).
Lang and colleagues6 also found a decline in quality of life regarding energy and vitality of their patients. Comparing quality of life in patients who underwent decompressive craniectomy after supratentorial ischemia and in patients who suffered from severe head injury, patients who underwent surgery for malignancies of the anterior skull base (42 points, mean, QoLI) scored in the same range as patients suffering from severe head injury (36.3 points, mean, QoLI).14 Patients treated for severe ischemia were reported to have a better quality of life (60 points, mean, QoLI).15
CONCLUSION
Quality of life after surgery of skull base tumors seems to be quite low. The perioperative morbidity and mortality of rates associated with surgery of these tumors is relatively high. Furthermore, the mean survival time of about 39 months in this study is relatively low. Thus, it appears that these kinds of tumors remain a challenge despite contemporary surgical techniques.
REFERENCES
- Sekhar L N, Moller A R. Operative management of tumors involving the cavernous sinus. J Neurosurg. 1986;64:879–889. doi: 10.3171/jns.1986.64.6.0879. [DOI] [PubMed] [Google Scholar]
- Boyle J O, Shah K C, Shah J P. Craniofacial resection for malignant neoplasms of the skull base: an overview. J Surg Oncol. 1998;69:275–284. doi: 10.1002/(sici)1096-9098(199812)69:4<275::aid-jso13>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pitman K T, Prokopakis E P, Aydogan B, et al. The role of skull base surgery for the treatment of adenoid cystic carcinoma of the sinonasal tract. Head Neck. 1999;21:402–407. doi: 10.1002/(sici)1097-0347(199908)21:5<402::aid-hed4>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Joos U, Mann W, Gilsbach J. Microsurgical treatment of midfacial tumors involving the skull base. J Craniomaxillofac Surg. 1998;26:226–234. doi: 10.1016/s1010-5182(98)80018-8. [DOI] [PubMed] [Google Scholar]
- Hendryk S, Czecior E, Misiolek M, Namyslowski G, Mrowka R. Surgical strategies in the removal of malignant tumors and benign lesions of the anterior skull base. Neurosurg Rev. 2004;27:205–213. doi: 10.1007/s10143-004-0323-z. [DOI] [PubMed] [Google Scholar]
- Lang D A, Honeybul S, Neil-Dwyer G, Evans R T, Weller R O, Gill J. The extended transbasal approach: clinical applications and complications. Acta Neurochir (Wien) 1999;141:579–585. doi: 10.1007/s007010050346. [DOI] [PubMed] [Google Scholar]
- Fukuda K, Saeki N, Mine S, et al. Evaluation of outcome and QOL in patients with craniofacial resection for malignant tumors involving the anterior skull base. Neurol Res. 2000;22:545–550. doi: 10.1080/01616412.2000.11740716. [DOI] [PubMed] [Google Scholar]
- Neil-Dwyer G, Lang D A, Davis A. Outcome from complex neurosurgery: an evidence based approach. Acta Neurochir (Wien) 2000;142:367–371. doi: 10.1007/s007010050444. [DOI] [PubMed] [Google Scholar]
- Blau T. Quality of life, social indicators, and criteria of change. Prof Psychol. 1977;11:464–473. [Google Scholar]
- Richtsmeier W J, Briggs R J, Koch W M, et al. Complications and early outcome of anterior craniofacial resection. Arch Otolaryngol Head Neck Surg. 1992;118:913–917. doi: 10.1001/archotol.1992.01880090029010. [DOI] [PubMed] [Google Scholar]
- Kraus D H, Sterman B M, Levine H L, Wood B G, Tucker H M, Lavertu P. Factors influencing survival in ethmoid sinus cancer. Arch Otolaryngol Head Neck Surg. 1992;118:367–372. doi: 10.1001/archotol.1992.01880040025005. [DOI] [PubMed] [Google Scholar]
- Clayman G L, DeMonte F, Jaffe D, et al. Outcome and complications of extended cranial-base resection requiring microvascular free-tissue transfer. Arch Otolaryngol Head Neck Surg. 1995;121:1253–1257. doi: 10.1001/archotol.1995.01890110031006. [DOI] [PubMed] [Google Scholar]
- Naficy S, Disher M J, Esclamado R M. Adenoid cystic carcinoma of the paranasal sinuses. Am J Rhinol. 1999;4:311–314. doi: 10.2500/105065899782102872. [DOI] [PubMed] [Google Scholar]
- Woertgen C, Rothoerl R D, Brawanski A. Early S-100 serum values correlate to quality of life after severe head injury. Brain Inj. 2002;16:807–816. doi: 10.1080/02699050210128933. [DOI] [PubMed] [Google Scholar]
- Woertgen C, Erban P, Rothoerl R D, Bein T, Horn M, Brawanski A. Quality of life after decompressive craniectomy in patients suffering from supratentorial brain ischemia. Acta Neurochir (Wien) 2004;146:691–695. doi: 10.1007/s00701-004-0280-x. [DOI] [PubMed] [Google Scholar]