ABSTRACT
Objective: Retrospectively assess the efficacy of lumbar cerebrospinal fluid (CSF) drainage placed preoperatively in skull base operations in decreasing the incidence of postoperative CSF fistula. Methods: A retrospective review of 150 patients undergoing a posterior fossa craniotomy from 1989 to 2000 was conducted. Patients were divided into those receiving preoperative lumbar drains and those that did not. The rates of postoperative CSF leakage were compared between the two groups. Patient data were analyzed to determine if there were other comorbidities affecting the postoperative incidence of CSF leakage such as smoking, diabetes, or hypertension. Results: Between 1989 and 1994, 25/72 (35%) patients with no preoperative lumbar drain had a postoperative CSF leak. From 1995 to 2000, 9/78 (12%) patients with a preoperative lumbar drain had a CSF leak. This was a 23% decreased incidence of postoperative CSF leakage and a significant decrease in the probability (p < 0.001) of CSF leakage in patients treated with a preoperative lumbar drain. The comorbidities of diabetes, smoking, or hypertension did not increase the probability of a CSF leak (p = 0.43). Conclusions: A preoperatively placed lumbar drain can significantly lower the rate of postoperative CSF leakage after skull base surgery. The drain is a well-tolerated adjunct to dural closure and helps increase surgical exposure of the posterior fossa. The comorbidities of diabetes, smoking, or hypertension do not contribute to an increased rate of CSF leakage.
Keywords: Cerebrospinal fluid fistula, lumbar drain, retrosigmoid, translabyrinthine
Skull base surgery is commonly used to approach cerebellopontine angle (CPA) lesions such as vestibular schwannomas and to access the lower cranial nerves for pain and vascular compression syndromes. Cerebrospinal fluid (CSF) leaks are one of the most frequent postoperative complications1,2 reported for posterior cranial fossa surgery with potentially life-threatening complications.3 Depending on the surgical approach, the rate of CSF leakage reported in the literature ranges between 5% and 15%, but rates as high as 30% have been reported.4
Multiple strategies have been employed to reduce the incidence of CSF fistula after skull base surgery. However, the rates of CSF leakage have remained stable. The purpose of this article is to look at our experience with the use of preoperative lumbar drains and their efficacy in reducing the rate of CSF fistula in three different approaches to the skull base: retrosigmoid, middle cranial fossa, and translabyrinthine. The effect of patient comorbidities on the rate of CSF fistula is also addressed. Elucidating a reliable method to minimize CSF fistula is pertinent to skull base surgery.
METHODS
Subjects
Between 1989 and 2000, 150 patients were studied retrospectively for spinal fluid leak. At the start of the study dates, patients did not have a lumbar drain placed. Due to an unacceptable incidence of CSF fistula, all patients began receiving preoperative lumbar drains, thereby dividing the study population. All patients in the study were followed for a minimum of 2 years. Seventy-two patients did not have a drain placed. The remaining 78 patients had a prophylactic lumbar drain inserted preoperatively in the subarachnoid space. There were 58 males and 92 females included in the study, and of these, 11 were younger than 35 years old, 49 were between the ages of 36 and 50, and 90 patients were 51 years of age or older (Table 1).
Table 1.
Patient Characteristics
| Number of Patients | |
|---|---|
| Age (y) | |
| ≤ 35 | 11 |
| 36–50 | 49 |
| ≥ 51 | 90 |
| Sex | |
| Male | 58 |
| Female | 92 |
Diagnostic Criteria
The definition of a CSF leak was drainage of clear fluid at any time in the postoperative period, after the lumbar drain had been removed. The type of leak was listed as otorrhea, rhinorrhea, incisional, or a subcutaneous accumulation. All cases were followed for a minimum of 2 years.
Surgical Approach and Technique
The surgical approaches were as follows: 107 retrosigmoid, 19 translabyrinthine, 20 middle cranial fossa, and 4 combined. The surgical procedures indicated for a preoperative CSF drain were: (1) posterior fossa approach to vestibular schwannomas; (2) vestibular nerve sections; (3) vascular loop syndromes such as trigeminal neuralgia and hemifacial spasm; and (4) miscellaneous skull base tumors.
The posterior fossa approach utilized has been well described by Silverstein and Rosenberg5 and Nadol and Schuknecht.6 A craniectomy is completed using the sigmoid sinus and transverse sinus as the anterior and superior borders of the dissection that creates a bony window, 3 × 3 cm in size, down to the posterior fossa dura.
Prophylactic CSF drains were placed in the operating room by the neurosurgical service after the patients had been intubated. The patients were placed in the lateral decubitus position and after obtaining clear fluid return, the catheter was threaded into the CSF space and a Tegaderm™ (3M, St. Paul, MN) occlusive dressing was placed over the skin-catheter interface. The catheter system was a standard lumbar drainage kit that included a 14-gauge Touhy needle. After the catheter was placed in the subarachnoid space it was clamped until the craniectomy had been completed. The CSF was allowed to have an outflow rate set by gravity and fluid accumulated in a drip chamber and then into a sterile collection system. Initially, 30 to 70 cc of CSF was drained prior to dural incision depending on the turgidity of the posterior cranial fossa dura. The drain was kept at bed level during craniectomy, and after the CSF had been allowed to drain it was reclamped for the remainder of the operative procedure.
Wound Closure
In all patients, a watertight dural closure was obtained whether closed primarily or with a dural graft. Bone wax or muscle graft was placed in the internal auditory canal if this bone was removed. All dural suture lines were covered with CoStasis (Cohesion Technologies, Palo Alto, CA) fibrin glue. Hydroxyapatite paste was used to obliterate the mastoid air cells.7 A cranioplasty was used to reconstruct the normal contours of the skull with hydroxyapatite paste over titanium mesh (Fig. 1). A multiple-layer soft-tissue closure utilizing 3–0 Vicryl sutures subcutaneously and either skin staples or 3–0 Prolene suture was used for skin approximation. A snug craniotomy dressing was placed over the wound for 3 to 5 days postoperatively.
Figure 1.
(A) Titanium mesh covering dural defect. (B) Hydroxyapatite paste applied over titanium mesh to complete cranioplasty.
Postoperative Care
The head of the bed was elevated to 30 degrees and the CSF drip chamber was placed at the top of the patient's shoulder in a level position. The lumbar drain was kept open for 72 hours after insertion and was clamped on postoperative day 3. The drain was clamped for 24 hours and if no leak occurred and the wound was flat, the drain was removed. If a CSF percutaneuous leak or collection persisted, this technique was repeated at 24-hour intervals.
Statistical Analysis
All statistical data were recorded in a Microsoft Access® database. The frequency and percent for each of the variables were calculated in a standard fashion. After calculating the cumulative frequency and cumulative percent, p-values were obtained by comparing the proportions between groups using the Fisher exact test.
RESULTS
Data
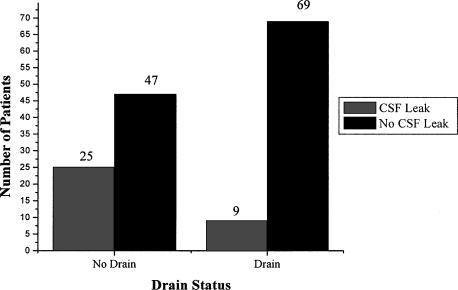
In the 72 patients with no preoperative CSF drain, 25 developed a postoperative CSF leak. This was an incidence of 35% CSF leakage between 1989 and 1994. In patients treated with a preoperatively placed CSF drain, 9 of 78 patients had a CSF leak between the years of 1995 and 2000 for an incidence of 12% (Fig. 2). The result was a 23% lower incidence of postoperative CSF leakage in patients treated with a prophylactic lumbar drain compared with those without a drain. The use of a lumbar drain significantly decreased the probability of a CSF leak (p < 0.001).
Figure 2.
Comparison of CSF leak with and without drain.
Treatment of patients with a CSF leak that did not receive a preoperative drain was accomplished by lumbar catheter insertion and lumbar puncture. Of those 25 patients, 4 required surgery to correct the underlying CSF leak and 1 patient responded with a pressure dressing alone (Table 2). The management of the CSF leak in those 9 patients who did receive a preoperative lumbar drain was replacement of the lumbar catheter drainage system (5) or multiple lumbar punctures (4). No patient who received a preoperative lumbar drain required surgical intervention to correct the underlying CSF leak (Table 3).
Table 2.
Treatment of Postoperative CSF Leaks in Patients without Preoperative Lumbar Drains (N = 25)
| Treatment | Number |
|---|---|
| Lumbar drain | 20 |
| Operation | 4 |
| Pressure dressing | 1 |
Table 3.
Treatment of Postoperative CSF Leaks in Patients with Preoperative Lumbar Drains (N = 9)
| Treatment | Number |
|---|---|
| Replacement of lumbar drain | 5 |
| Multiple lumbar punctures | 4 |
The comorbidities evaluated during the study included diabetes, smoking, hypertension, and sleep apnea. Sixty-nine (46%) patients had comorbidities. The presence of comorbidities was similar for patients with and without lumbar drains. For all patients combined, there was no association between presence of comorbidities and wound complications (p = 0.43). There was no apparent association between the presence of comorbidities and wound complications when analyzed separately for patients with (p = 0.73) and without (p = 0.32) preoperative lumbar drain.
Complications
Two patients had postural headaches. No patients had any nerve root injuries, major infections, or other complications as a result of placement of the lumbar catheter drain.
DISCUSSION
CSF fistulas occur as the result of an abnormal communication between the subarachnoid space and bone of the skull base along with the underlying mucosa. CSF fistulas remain one of the most common complications of the various skull base approaches.
A wide range of CSF leakage rates have been reported for posterior fossa surgery. Magliulo and associates8 reported a 17.6% CSF leak following CPA tumor surgery, while Nutick and Korol1 reported a 13% incidence following acoustic tumor removal. Fishman et al,9 as well as Ruiz-Fornells and colleagues,10 reported 17% and 15% CSF leakage, respectively. At the opposite end of the spectrum, Falcioni and coworkers11 reported a series of 200 translabyrinthine approaches and several CPA tumor removals with a zero incidence of CSF leaks. This type of success has not been reported elsewhere in the literature.
Many factors have been identified as potentially increasing the rate of postoperative CSF leakage. Two commonly established concepts currently accepted as contributing factors to the pathophysiology of CSF leakage are poor dural closure and advanced patient age.12,13 Other factors that may contribute to an increased CSF leakage rate include increased intracranial pressure either from transient postoperative hydrocephalus, intraoperative bone dust accumulation in the subarachnoid space, size of the dural opening, aseptic meningitis, abnormal CSF dynamics,14 or other comorbidities such as patient nutritional status, smoking, diabetes, or vascular disease.15 Surgical approaches that remove the internal auditory canal versus leaving it intact may contribute to CSF leakage,1 but Becker and colleagues4found the rates of CSF leakage after translabyrinthine, middle fossa, and retrosigmoid approaches not to be statistically significant.
Hoffman16 compared the surgical approach used in CPA tumor removals and found there was no significant difference in the rate of CSF leakage when comparing the translabyrinthine and retrosigmoid approaches (21% versus 16%, respectively). Becker and associates4 reported that neither the tumor size nor the surgical approach had an effect on the rate of CSF leaks. The results showed a 10% postoperative CSF leakage rate when using a translabyrinthine, middle cranial fossa, or retrosigmoid craniotomy approach. They placed lumbar drains in nearly half of their study patients and included lumbar drains as an integral step in their proposed algorithms for both early and late postoperative CSF leaks.
Prophylactic CSF drainage may decrease the postoperative CSF leakage rate by several factors. It can reduce the effect of a transient postoperative hydrocephalus and also improve surgical exposure by decompressing the posterior fossa, which allows less cerebellar retraction to be used, thereby decreasing rebound swelling of the cerebellum in the posterior fossa.
There is a minimal risk associated with the use of CSF lumbar drains. Roland and coworkers17 reported a minimal complication rate from the placement of the lumbar drain and alleviation of all complications with removal of the drain. This finding was confirmed by Grady et al,18 who demonstrated that of 530 anesthetized patients with lumbar drains, there were no neurologic deficits and a 2.5% incidence of postpuncture headache. There is minimal risk associated with the placement of a lumbar drain, and this was further confirmed in the present study.
One of the limitations of the current study is that it is retrospective. The retrospective nature of this study allows for author bias and the lack of prospective randomization. These weaknesses of a retrospective review are lessened, and selection bias eliminated, in the current analysis because the two study arms were divided based on unacceptable CSF leak rates. The two populations were divided based on a given point in time rather than on operative approach, age, or comorbidity. Finally, this study does not account for those patients lost to follow-up.
CONCLUSIONS
Routine implementation of lumbar drainage is not commonly agreed upon as a means to reduce postoperative CSF leakage rates.19 This study shows that lumbar catheters are well tolerated when performed preoperatively with no complications from the placement of the lumbar drain. Lumbar drains are a safe and well-tolerated adjunct to the various watertight dural closures advocated.20,21 In this study, there was a statistically significant lower rate of postoperative CSF leakage in patients with a preoperatively placed lumbar drain. The various comorbidities investigated did not contribute to an increased incidence of CSF leak. The only variable identified to avoid the development of a postoperative CSF leak was placement of a preoperative lumbar catheter.
IN MEMORIAM
We would like to honor the life and career of Lyal Leibrock, M.D., F.A.C.S., with the publishing of this paper. He was a friend to all and a mentor to many. His presence will be greatly missed, but his influence will continue.
ACKNOWLEDGMENT
Thank you to Jane Meza, Ph.D., for her timely and insightful assistance with the statistical portions of this manuscript.
REFERENCES
- Nutik S L, Korol H W. Cerebrospinal fluid leak after acoustic neuroma surgery. Surg Neurol. 1995;43:553–557. doi: 10.1016/0090-3019(95)00016-x. [DOI] [PubMed] [Google Scholar]
- Lebowitz R A, Hoffman R A, Roland R A, Jr, et al. Autologous fibrin glue in the prevention of cerebral spinal fluid leak following acoustic neuroma surgery. Am J Otol. 1995;16:172–174. [PubMed] [Google Scholar]
- Bryce G E, Nedzelski J M, Rowed D W, Rappaport J M. Cerebrospinal fluid leaks and meningitis in acoustic neuroma surgery. Otolaryngol Head Neck Surg. 1991;104:81–87. doi: 10.1177/019459989110400115. [DOI] [PubMed] [Google Scholar]
- Becker S S, Jackler R K, Pitts L H. Cerebral spinal fluid leak after acoustic neuroma surgery: a comparison of the translabyrinthine, middle fossa, and retrosigmoid approaches. Otol Neurotol. 2003;24:107–112. doi: 10.1097/00129492-200301000-00021. [DOI] [PubMed] [Google Scholar]
- Silverstein H, Rosenberg S. Surgical Techniques of the Temporal Bone and Skull Base. Malvern, PA: Lea & Febiger; 1992. pp. 145–170.
- Nadol J B, Schuknecht H F. Surgery of the Ear and Temporal Bone. New York, NY: Raven Press; 1993. pp. 391–413.
- Kveton J F, Goravalingappa R. Elimination of temporal bone cerebrospinal fluid otorrhea using hydroxapatite cement. Laryngoscope. 2000;110:1655–1659. doi: 10.1097/00005537-200010000-00016. [DOI] [PubMed] [Google Scholar]
- Magliulo G, Sepe C, Varacalli S, et al. Cerebrospinal fluid leak management following cerebellopontine angle surgery. J Otolaryngol. 1998;27:258–262. [PubMed] [Google Scholar]
- Fishman A J, Hoffman R A, Roland J T, Jr, et al. Cerebrospinal fluid drainage in the management of CSF leak following acoustic neuroma surgery. Laryngoscope. 1996;106:1002–1004. doi: 10.1097/00005537-199608000-00017. [DOI] [PubMed] [Google Scholar]
- Ruiz-Fornells A, Monux A, Cabra J, et al. Our experience in neuroma surgery. Acta Otorrinolaringol Esp. 1996;47:205–207. [PubMed] [Google Scholar]
- Falcioni M, Mulder J JS, Taibah A, et al. No cerebral spinal fluid leaks in translabyrinthine vestibular schwannoma removal. Am J Otol. 1999;20:660–666. [PubMed] [Google Scholar]
- Oghalai J S, Buxbaum J L, Pitts L H, et al. The effect of age on acoustic neuroma surgery outcomes. Otol Neurotol. 2003;24:473–477. doi: 10.1097/00129492-200305000-00020. [DOI] [PubMed] [Google Scholar]
- Rodgers G K, Luxford W M. Factors affecting the development of cerebrospinal fluid leak and meningitis after translabyrinthine acoustic tumor surgery. Laryngoscope. 1993;103:959–962. doi: 10.1288/00005537-199309000-00003. [DOI] [PubMed] [Google Scholar]
- Spetzler R F, Wilson C B. Management of recurrent CSF rhinorrhea of the middle and posterior fossa. J Neurosurg. 1978;49:393–397. doi: 10.3171/jns.1978.49.3.0393. [DOI] [PubMed] [Google Scholar]
- Kwartler J A, Schulder M, Baredes S, et al. Endoscopic closure of the eustachian tube for repair of cerebral spinal fluid leak. Am J Otol. 1996;17:470–472. [PubMed] [Google Scholar]
- Hoffman R A. Cerebrospinal fluid leak following acoustic neuroma removal. Laryngoscope. 1994;104:40–58. doi: 10.1288/00005537-199401000-00009. [DOI] [PubMed] [Google Scholar]
- Roland P S, Marple B F, Meyerhoff W L, et al. Complications of lumbar spinal fluid drainage. Otolaryngol Head Neck Surg. 1992;107:564–569. doi: 10.1177/019459989210700409. [DOI] [PubMed] [Google Scholar]
- Grady R E, Horlocker T T, Brown R D, et al. Neurologic complications after placement of cerebrospinal fluid drainage catheters and needles in anesthetized patients: implication for regional anesthesia. Anesth Analg. 1999;88:388–392. [PubMed] [Google Scholar]
- Leonetti J, Anderson D, Marzo S, et al. Cerebrospinal fluid fistula after transtemporal skull base surgery. Otolaryngol Head Neck Surg. 2001;124:511–514. doi: 10.1067/mhn.2001.115089. [DOI] [PubMed] [Google Scholar]
- Savva A, Taylor M J, Beatty C W. Management of cerebrospinal fluid leaks involving the temporal bone: report on 92 patients. Laryngoscope. 2003;113:50–56. doi: 10.1097/00005537-200301000-00010. [DOI] [PubMed] [Google Scholar]
- Lundy L B, Graham M D, Kartush J M, et al. Temporal bone encephalocele and cerebrospinal fluid leaks. Am J Otol. 1996;17:461–469. [PubMed] [Google Scholar]