Full Text
The Full Text of this article is available as a PDF (285.5 KB).
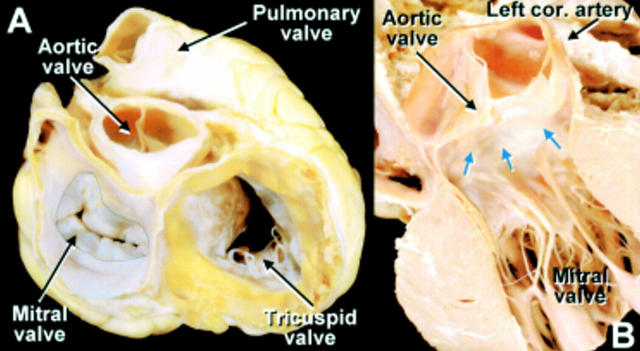
Figure 1 .
(A) View of the base of the heart in anatomical orientation shows the spatial relations of the four cardiac valves. The left heart valves are close together whereas the right heart valves are separated by myocardium. Dotted line marks the limit of atrial myocardium around the mitral orifice. (B) This dissection of the heart viewed from the anterior aspect shows the close relation between aortic and mitral valves in situ. Fibrous continuity between the valves (blue arrows) is related to the non- and left coronary sinuses of the aorta.
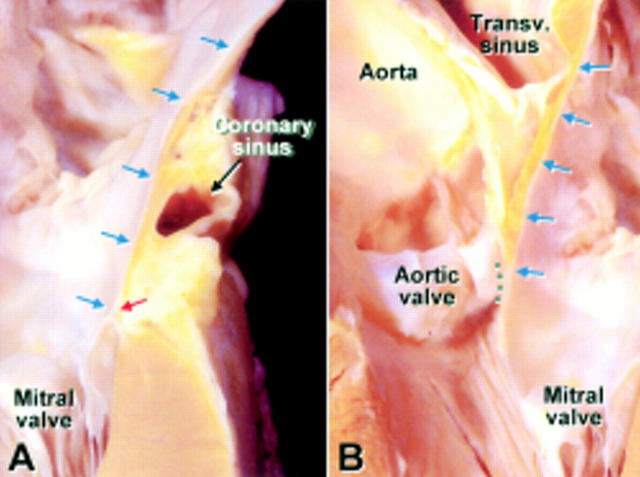
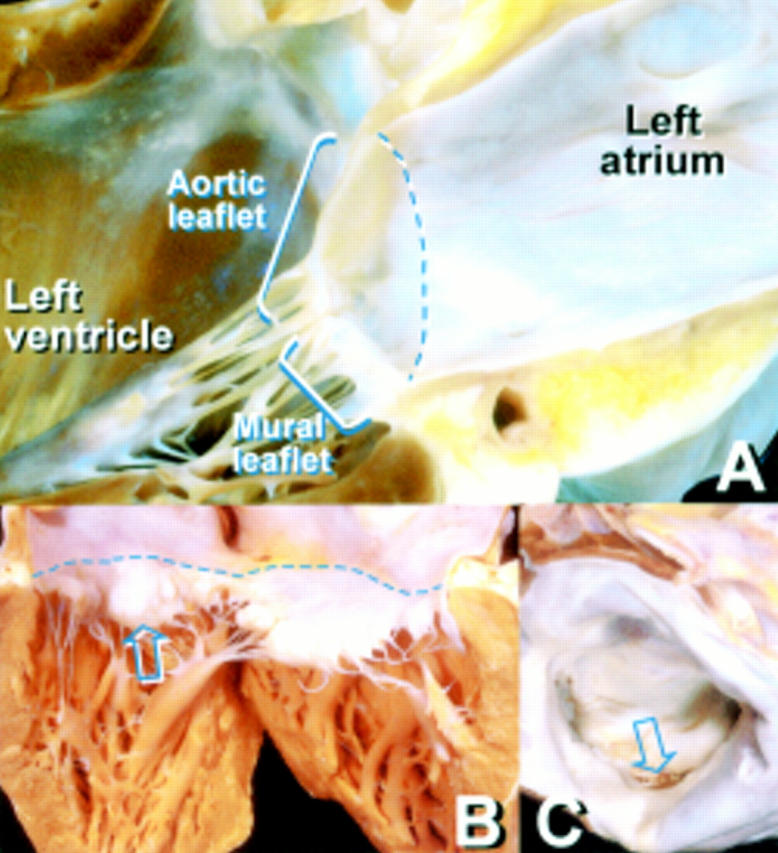
Figure 2 .
(A) The left parietal atrioventricular junction in profile shows the left atrial wall (blue arrows) running to the hinge (red arrow) of the mural leaflet of the mitral valve. (B) The aortic leaflet of the mitral valve cut in profile shows the atrial wall (blue arrows) reaching the leaflet. Grey dots mark the region of fibrous continuity between aortic and mitral valves.
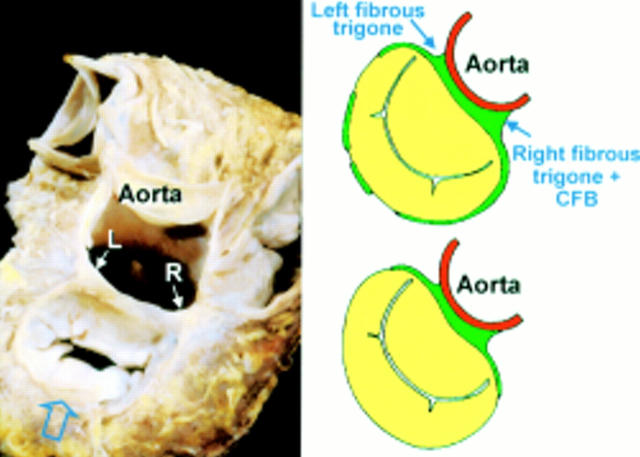
Figure 3 .
A dissection showing the left (L) and right (R) fibrous trigones revealed by removing the left and non-coronary aortic sinuses. The trigones are expansions of fibrous tissue at either end of the area of aortic–mitral valvar continuity. The right fibrous trigone together with the membranous septum forms the central fibrous body. The diagrams represent two of the cases reported in the work by Angelini and colleagues.5 They show the variation in completeness of the so-called valvar annulus (green areas).
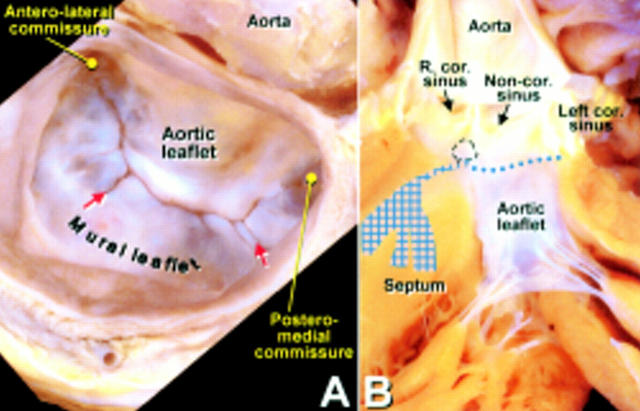
Figure 4 .
(A) The atrial aspect of the mitral valve shows the arrangement of the two leaflets between the commissures. The free edge of the mural leaflet has two clefts (red arrows) giving this leaflet the appearance of three scallops. Note the wider middle scallop. (B) The aortic leaflet of the mitral valve hangs between inflow and outflow tracts of the left ventricle. Aortic–mitral fibrous continuity (dotted line) extends between the membranous septum (dotted circle) and the left fibrous trigone.
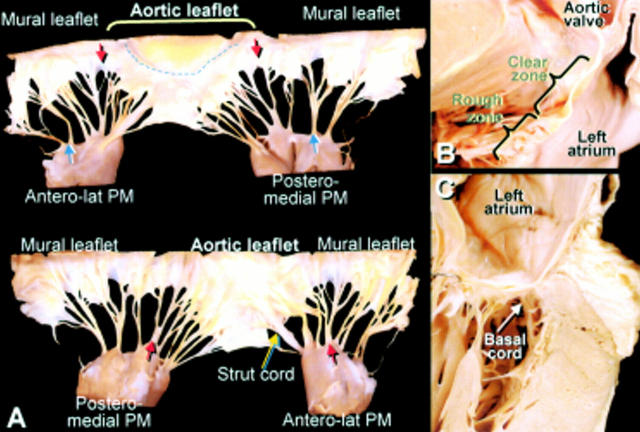
Figure 5 .
(A) Atrial surface (upper panel) and ventricular surface (lower panel) of a mitral valve spread open by cutting through the mural leaflet. The red arrows indicate the commissures supported by fan shaped commissural cords that are difficult to distinguish from cleft cords (blue arrows). Note the attachment of the cords to the edge and the rough zone of the leaflets. The broken line on the aortic leaflet marks the border between clear and rough zones. (B) This dissection profiling the aortic leaflet shows cordal attachments to the rough zone. (C) A basal cord inserts to the basal zone on the ventricular surface of the mural leaflet, close to its hinge.
Figure 6 .
(A) The closure line of the mitral valve is seen in this simulated two chamber section through the long axis of the left ventricle. The closure line is below the level of the atrioventricular junction (broken line). (B) A case of prolapse of the middle scallop (arrow) in the mural leaflet overshooting above the level of the atrioventricular junction (broken line) when the valve closes. Note also the dome-like protrusions on the aortic leaflet. (C) Rupture of the tip of a papillary muscle affecting the aortic leaflet.
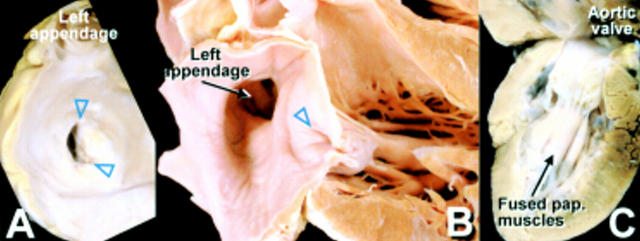
Figure 7 .
(A) Rheumatic mitral valve viewed from the atrium showing the stenotic crescent shaped orifice owing to fusion of the leaflets at the commissures (▿). (B) This longitudinal section through a rheumatic mitral valve shows fusion at the commissures (▿) and thickening of the leaflets. (C) A single group of papillary muscles supports this parachute mitral valve. Note the short cords and loss of intercordal spaces exacerbating valvar stenosis.
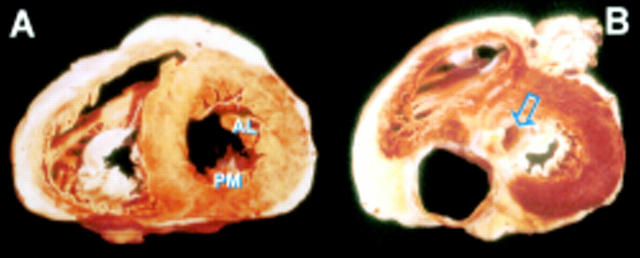
Figure 8 .
(A) Short axis section through the ventricles showing the oblique arrangement of the anterolateral (AL) and posteromedial (PM) papillary muscles. (B) This section nearer to the base shows the aortic outlet (arrow) sandwiched between the mitral valve and the septum.
Figure 9 .
The diagram shows the planes of longitudinal sections through the mitral valve. The parasternal two chamber plane (P2) passes through the middle of both leaflets along the minor axis of the valve whereas the apical two chamber plane (A2) is at an angle to it. The apical four chamber plane (A4) is nearly parallel to the zone of apposition. (A) This simulated parasternal long axis section profiles the two leaflets nicely. (B) This simulated four chamber plane cuts the leaflets obliquely. It shows the aortic leaflet toward the posteromedial commissure and the mural leaflet toward the anterolateral commissure.
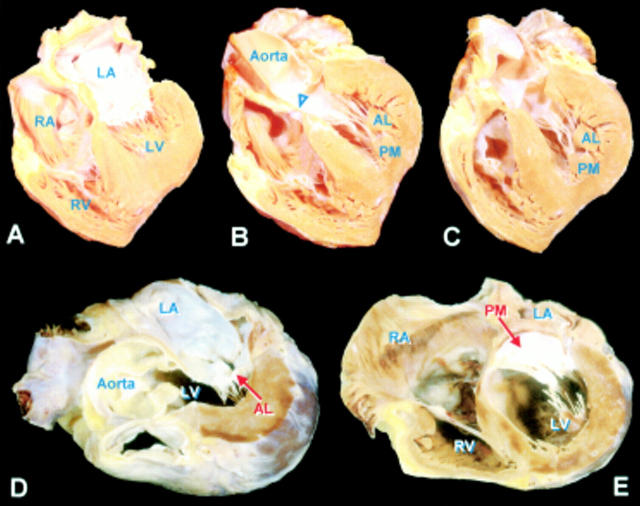
Figure 10 .
Sections A, B, and C are a series of heart sections replicating transgastric echocardiographic cuts of four chamber views foreshortened at the cardiac apex that allow visualisation of the tendinous cords and papillary muscles. Section A shows the off-set arrangement between tricuspid and mitral valves at the septum. Section B is a cut through the membranous septum (▿) and shows the papillary muscles. Sections D and E replicate transgastric cuts through the closure line of the mitral leaflets that allow examination of the anterolateral (AL) and posteromedial (PM) commissures. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Angelini A., Ho S. Y., Anderson R. H., Davies M. J., Becker A. E. A histological study of the atrioventricular junction in hearts with normal and prolapsed leaflets of the mitral valve. Br Heart J. 1988 Jun;59(6):712–716. doi: 10.1136/hrt.59.6.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BROCK R. C. The surgical and pathological anatomy of the mitral valve. Br Heart J. 1952 Oct;14(4):489–513. doi: 10.1136/hrt.14.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker A. E., De Wit A. P. Mitral valve apparatus. A spectrum of normality relevant to mitral valve prolapse. Br Heart J. 1979 Dec;42(6):680–689. doi: 10.1136/hrt.42.6.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulkley B. H., Roberts W. C. Dilatation of the mitral anulus. A rare cause of mitral regurgitation. Am J Med. 1975 Oct;59(4):457–463. doi: 10.1016/0002-9343(75)90252-1. [DOI] [PubMed] [Google Scholar]
- Burch G. E., Giles T. D. Angle of traction of the papillary muscle in normal and dilated hearts: a theoretic analysis of its importnace in mitral valve dynamics. Am Heart J. 1972 Jul;84(1):141–144. doi: 10.1016/0002-8703(72)90319-5. [DOI] [PubMed] [Google Scholar]
- Carpentier A., Deloche A., Dauptain J., Soyer R., Blondeau P., Piwnica A., Dubost C., McGoon D. C. A new reconstructive operation for correction of mitral and tricuspid insufficiency. J Thorac Cardiovasc Surg. 1971 Jan;61(1):1–13. [PubMed] [Google Scholar]
- Cheng T. O., Xie M. X., Wang X. F., Li Z. A., Hu G. Evaluation of mitral valve prolapse by four-dimensional echocardiography. Am Heart J. 1997 Jan;133(1):120–129. doi: 10.1016/s0002-8703(97)70257-6. [DOI] [PubMed] [Google Scholar]
- Davies M. J., Moore B. P., Braimbridge M. V. The floppy mitral valve. Study of incidence, pathology, and complications in surgical, necropsy, and forensic material. Br Heart J. 1978 May;40(5):468–481. doi: 10.1136/hrt.40.5.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert B. W., Schatz R. A., VonRamm O. T., Behar V. S., Kisslo J. A. Mitral valve prolapse. Two-dimensional echocardiographic and angiographic correlation. Circulation. 1976 Nov;54(5):716–723. doi: 10.1161/01.cir.54.5.716. [DOI] [PubMed] [Google Scholar]
- Hutchins G. M., Moore G. W., Skoog D. K. The association of floppy mitral valve with disjunction of the mitral annulus fibrosus. N Engl J Med. 1986 Feb 27;314(9):535–540. doi: 10.1056/NEJM198602273140902. [DOI] [PubMed] [Google Scholar]
- LEVY M. J., EDWARDS J. E. Anatomy of mitral insufficiency. Prog Cardiovasc Dis. 1962 Sep;5:119–144. doi: 10.1016/s0033-0620(62)80025-5. [DOI] [PubMed] [Google Scholar]
- Lam J. H., Ranganathan N., Wigle E. D., Silver M. D. Morphology of the human mitral valve. I. Chordae tendineae: a new classification. Circulation. 1970 Mar;41(3):449–458. doi: 10.1161/01.cir.41.3.449. [DOI] [PubMed] [Google Scholar]
- Louie E. K., Langholz D., Mackin W. J., Wallis D. E., Jacobs W. R., Scanlon P. J. Transesophageal echocardiographic assessment of the contribution of intrinsic tissue thickness to the appearance of a thick mitral valve in patients with mitral valve prolapse. J Am Coll Cardiol. 1996 Aug;28(2):465–471. doi: 10.1016/0735-1097(96)00160-X. [DOI] [PubMed] [Google Scholar]
- Malkowski M. J., Boudoulas H., Wooley C. F., Guo R., Pearson A. C., Gray P. G. Spectrum of structural abnormalities in floppy mitral valve echocardiographic evaluation. Am Heart J. 1996 Jul;132(1 Pt 1):145–151. doi: 10.1016/s0002-8703(96)90403-2. [DOI] [PubMed] [Google Scholar]
- Perloff J. K., Roberts W. C. The mitral apparatus. Functional anatomy of mitral regurgitation. Circulation. 1972 Aug;46(2):227–239. doi: 10.1161/01.cir.46.2.227. [DOI] [PubMed] [Google Scholar]
- RUSTED I. E., SCHEIFLEY C. H., EDWARDS J. E., KIRKLIN J. W. Guides to the commissures in operations upon the mitral valve. Proc Staff Meet Mayo Clin. 1951 Aug 1;26(16):297–305. [PubMed] [Google Scholar]
- RUSTED I. E., SCHEIFLEY C. H., EDWARDS J. E. Studies of the mitral valve. I. Anatomic features of the normal mitral valve and associated structures. Circulation. 1952 Dec;6(6):825–831. doi: 10.1161/01.cir.6.6.825. [DOI] [PubMed] [Google Scholar]
- Ranganathan N., Lam J. H., Wigle E. D., Silver M. D. Morphology of the human mitral valve. II. The value leaflets. Circulation. 1970 Mar;41(3):459–467. doi: 10.1161/01.cir.41.3.459. [DOI] [PubMed] [Google Scholar]
- Roberts W. C., Perloff J. K. Mitral valvular disease. A clinicopathologic survey of the conditions causing the mitral valve to function abnormally. Ann Intern Med. 1972 Dec;77(6):939–975. doi: 10.7326/0003-4819-77-6-939. [DOI] [PubMed] [Google Scholar]
- Seward J. B., Khandheria B. K., Oh J. K., Abel M. D., Hughes R. W., Jr, Edwards W. D., Nichols B. A., Freeman W. K., Tajik A. J. Transesophageal echocardiography: technique, anatomic correlations, implementation, and clinical applications. Mayo Clin Proc. 1988 Jul;63(7):649–680. doi: 10.1016/s0025-6196(12)65529-3. [DOI] [PubMed] [Google Scholar]
- Stümper O., Fraser A. G., Ho S. Y., Anderson R. H., Chow L., Davies M. J., Roelandt J. R., Sutherland G. R. Transoesophageal echocardiography in the longitudinal axis: correlation between anatomy and images and its clinical implications. Br Heart J. 1990 Oct;64(4):282–288. doi: 10.1136/hrt.64.4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman J. The functional and surgical anatomy of the heart. Ann R Coll Surg Engl. 1966 Dec;39(6):348–366. [PMC free article] [PubMed] [Google Scholar]
- van der Bel-Kahn J., Becker A. E. The surgical pathology of rheumatic and floppy mitral valves. Distinctive morphologic features upon gross examination. Am J Surg Pathol. 1986 Apr;10(4):282–292. doi: 10.1097/00000478-198604000-00007. [DOI] [PubMed] [Google Scholar]