Abstract
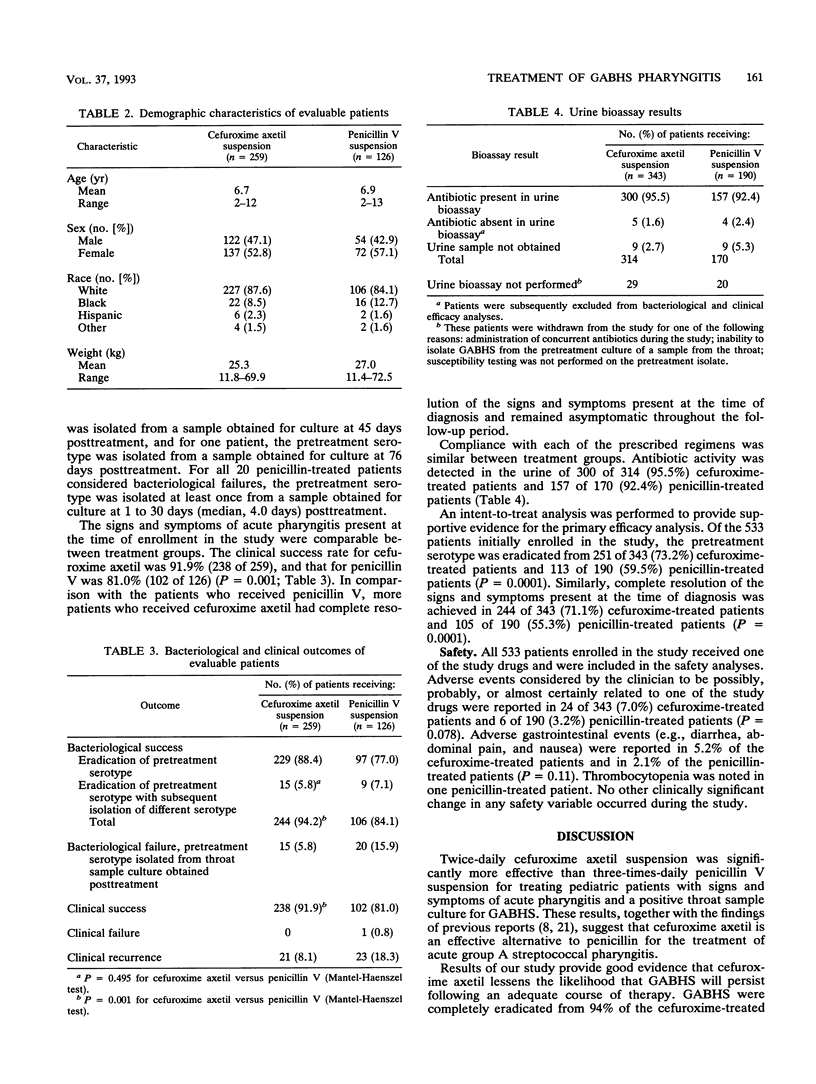
The bacteriological and clinical efficacies of cefuroxime axetil suspension (20 mg/kg of body weight per day in two divided doses) were compared with those of penicillin V suspension (50 mg/kg/day in three divided doses) in a multicenter, randomized, evaluator-blinded study. Children aged 2 to 13 years with clinical signs and symptoms of acute pharyngitis and a positive throat culture for group A beta-hemolytic streptococci (GABHS) were eligible. Patients were assessed and samples from the throat for culture were obtained at the time of diagnosis, 3 to 7 days after the initiation of treatment, and 4 to 8 days and 19 to 25 days after the completion of 10 days of therapy. Of the 385 evaluable patients, GABHS were eradicated from 244 of 259 (94.2%) cefuroxime-treated patients and 106 of 126 (84.1%) penicillin-treated patients (P = 0.001). Complete resolution of the signs and symptoms present at the time of diagnosis was achieved in 238 of 259 (91.9%) cefuroxime-treated patients and 102 of 126 (81.0%) penicillin-treated patients (P = 0.001). Potential drug-related adverse events were reported in 7.0 and 3.2% of the cefuroxime- and penicillin-treated patients, respectively (P = 0.078). In the present study, cefuroxime axetil suspension given twice daily resulted in significantly greater bacteriological and clinical efficacies than those of penicillin V suspension given three times daily to pediatric patients with acute pharyngitis and a positive throat culture for GABHS.
Full text
PDF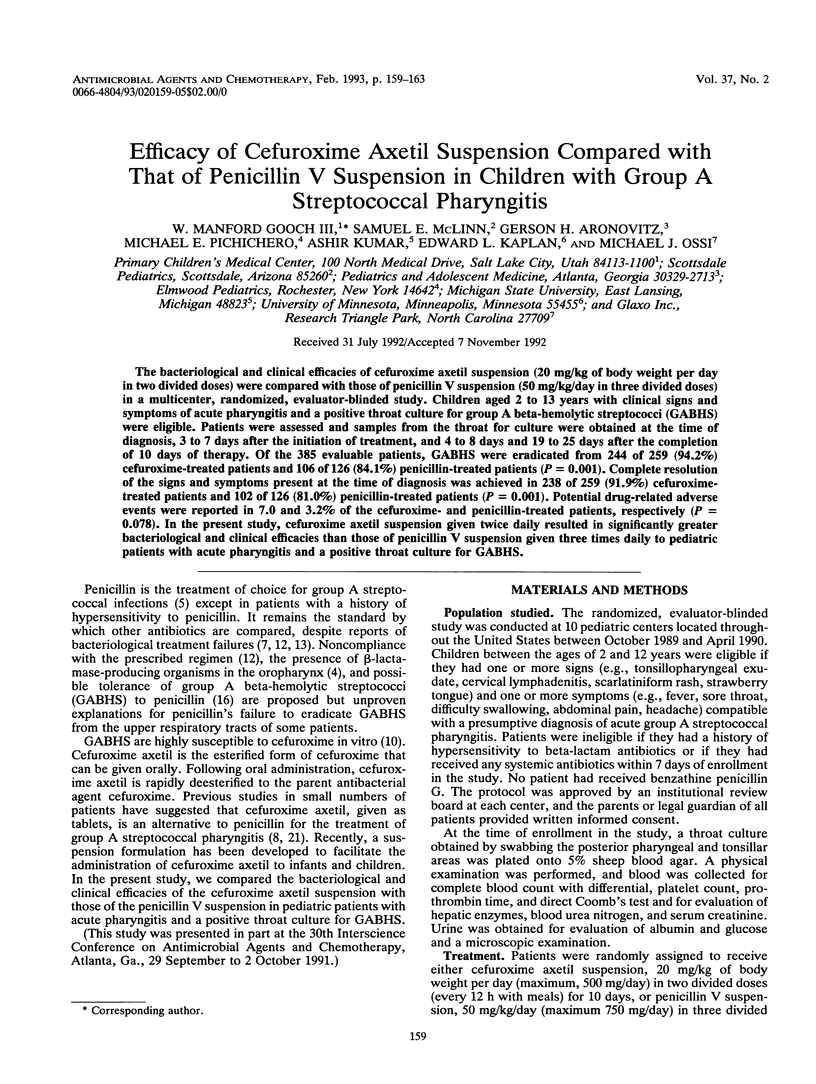


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alvarez S., Jones M., Holtsclaw-Berk S., Guarderas J., Berk S. L. In vitro susceptibilities and beta-lactamase production of 53 clinical isolates of Branhamella catarrhalis. Antimicrob Agents Chemother. 1985 Apr;27(4):646–647. doi: 10.1128/aac.27.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BREESE B. B., DISNEY F. A. The successful treatment of beta hemolytic streptococcal infections in children with a single injection of repository penicillin (benzathine penicillin G). Pediatrics. 1955 May;15(5):516–521. [PubMed] [Google Scholar]
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Brook I. The role of beta-lactamase-producing bacteria in the persistence of streptococcal tonsillar infection. Rev Infect Dis. 1984 Sep-Oct;6(5):601–607. doi: 10.1093/clinids/6.5.601. [DOI] [PubMed] [Google Scholar]
- Dajani A. S., Bisno A. L., Chung K. J., Durack D. T., Gerber M. A., Kaplan E. L., Millard H. D., Randolph M. F., Shulman S. T., Watanakunakorn C. Prevention of rheumatic fever: a statement for health professionals by the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease of the Council on Cardiovascular Disease in the young, the American Heart Association. Pediatr Infect Dis J. 1989 May;8(5):263–266. [PubMed] [Google Scholar]
- Gastanaduy A. S., Kaplan E. L., Huwe B. B., McKay C., Wannamaker L. W. Failure of penicillin to eradicate group A streptococci during an outbreak of pharyngitis. Lancet. 1980 Sep 6;2(8193):498–502. doi: 10.1016/s0140-6736(80)91832-2. [DOI] [PubMed] [Google Scholar]
- Gooch W. M., 3rd, Swenson E., Higbee M. D., Cocchetto D. M., Evans E. C. Cefuroxime axetil and penicillin V compared in the treatment of group A beta-hemolytic streptococcal pharyngitis. Clin Ther. 1987;9(6):670–677. [PubMed] [Google Scholar]
- Johnson D. R., Kaplan E. L. Microtechnique for serum opacity factor characterization of group A streptococci adaptable to the use of human sera. J Clin Microbiol. 1988 Oct;26(10):2025–2030. doi: 10.1128/jcm.26.10.2025-2030.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R. N., Fuchs P. C., Gavan T. L., Gerlach E. H., Barry A. L., Thornsberry C. Cefuroxime, a new parenteral cephalosporin: collaborative in vitro susceptibility comparison with cephalothin against 5,887 clinical bacterial isolates. Antimicrob Agents Chemother. 1977 Jul;12(1):47–50. doi: 10.1128/aac.12.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan E. L. Benzathine penicillin G for treatment of group A streptococcal pharyngitis: a reappraisal in 1985. Pediatr Infect Dis. 1985 Sep-Oct;4(5):592–596. doi: 10.1097/00006454-198509000-00060. [DOI] [PubMed] [Google Scholar]
- Kaplan E. L., Gastanaduy A. S., Huwe B. B. The role of the carrier in treatment failures after antibiotic for group A streptococci in the upper respiratory tract. J Lab Clin Med. 1981 Sep;98(3):326–335. [PubMed] [Google Scholar]
- Kaplan E. L., Johnson D. R. Eradication of group A streptococci from the upper respiratory tract by amoxicillin with clavulanate after oral penicillin V treatment failure. J Pediatr. 1988 Aug;113(2):400–403. doi: 10.1016/s0022-3476(88)80291-9. [DOI] [PubMed] [Google Scholar]
- Kaplan E. L. The group A streptococcal upper respiratory tract carrier state: an enigma. J Pediatr. 1980 Sep;97(3):337–345. doi: 10.1016/s0022-3476(80)80178-8. [DOI] [PubMed] [Google Scholar]
- Kaplan E. L., Top F. H., Jr, Dudding B. A., Wannamaker L. W. Diagnosis of streptococcal pharyngitis: differentiation of active infection from the carrier state in the symptomatic child. J Infect Dis. 1971 May;123(5):490–501. doi: 10.1093/infdis/123.5.490. [DOI] [PubMed] [Google Scholar]
- Kim K. S. Clinical perspectives on penicillin tolerance. J Pediatr. 1988 Apr;112(4):509–514. doi: 10.1016/s0022-3476(88)80160-4. [DOI] [PubMed] [Google Scholar]
- Kumar A., Nankervis G. A. Patient compliance to antibiotic regimens. A simple method of evaluation. Postgrad Med. 1979 Mar;65(3):165–167. doi: 10.1080/00325481.1979.11715090. [DOI] [PubMed] [Google Scholar]
- Neu H. C., Fu K. P. Cefuroxime, a beta-lactamase-resistant cephalosporin with a broad spectrum of gram-positive and -negative activity. Antimicrob Agents Chemother. 1978 Apr;13(4):657–664. doi: 10.1128/aac.13.4.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pichichero M. E., Disney F. A., Aronovitz G. H., Ginsburg C., Stillerman M. A multicenter, randomized, single-blind evaluation of cefuroxime axetil and phenoxymethyl penicillin in the treatment of streptococcal pharyngitis. Clin Pediatr (Phila) 1987 Sep;26(9):453–458. doi: 10.1177/000992288702600904. [DOI] [PubMed] [Google Scholar]
- Pichichero M. E., Margolis P. A. A comparison of cephalosporins and penicillins in the treatment of group A beta-hemolytic streptococcal pharyngitis: a meta-analysis supporting the concept of microbial copathogenicity. Pediatr Infect Dis J. 1991 Apr;10(4):275–281. doi: 10.1097/00006454-199104000-00002. [DOI] [PubMed] [Google Scholar]
- Powell D. A., James N. C., Ossi M. J., Nahata M. C., Donn K. H. Pharmacokinetics of cefuroxime axetil suspension in infants and children. Antimicrob Agents Chemother. 1991 Oct;35(10):2042–2045. doi: 10.1128/aac.35.10.2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T. D., Huskins W. C., Kim K. S., Kaplan E. L. Efficacy of beta-lactamase-resistant penicillin and influence of penicillin tolerance in eradicating streptococci from the pharynx after failure of penicillin therapy for group A streptococcal pharyngitis. J Pediatr. 1987 May;110(5):777–782. doi: 10.1016/s0022-3476(87)80023-9. [DOI] [PubMed] [Google Scholar]
- Tanz R. R., Shulman S. T., Sroka P. A., Marubio S., Brook I., Yogev R. Lack of influence of beta-lactamase-producing flora on recovery of group A streptococci after treatment of acute pharyngitis. J Pediatr. 1990 Dec;117(6):859–863. doi: 10.1016/s0022-3476(05)80122-2. [DOI] [PubMed] [Google Scholar]


