Abstract
The purpose of this article is to clarify the nutritional recommendations for pregnant women in light of the new Food Guide Pyramid, known as “MyPyramid,” along with the Dietary Guidelines for Americans 2005 and recommendations by the Institute of Medicine. The differences between the Food Guide Pyramid (introduced in 1992) and the more recent, color-coded MyPyramid (introduced in 2005) are discussed. A list of nutritional recommendations for pregnant women is presented, which may serve as a reference for practitioners when counseling pregnant women.
Keywords: nutrition, pregnancy, Food Guide Pyramid, dietary requirements
The quality of a woman's diet during pregnancy has a profound influence on positive fetal and maternal outcomes. Dietary quality, particularly during the first trimester of pregnancy, exerts a strong influence on fetal and placental development and on subsequent fetal growth and maternal well-being (Carmichael & Abrams, 1997; Siega-Riz, Adair, & Hobel, 1996; Smith, 2004). During the first two months of pregnancy, the embryo and placenta undergo a process of rapid cell differentiation and division and are particularly sensitive to excesses and deficiencies in micronutrients. Adequate maternal nutritional status is an essential component of the intrauterine environment during this critical time of fetal development. Additionally, recent research suggests that inadequate levels of maternal nutrients during this crucial period of fetal development may lead to “reprogramming” within the fetal tissues that predisposes the infant to chronic illnesses in adulthood (Godfrey & Barker, 2001).
Adequate maternal nutritional status is an essential component of the intrauterine environment during this critical time of fetal development.
FOOD GUIDE PYRAMID
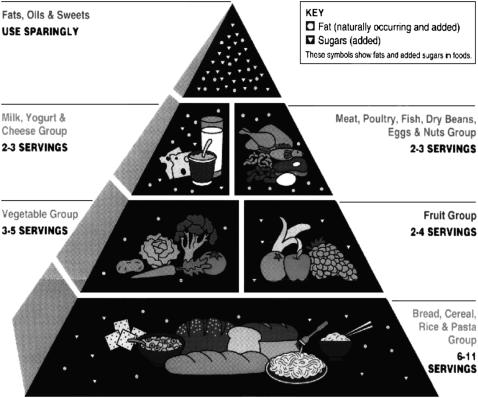
Providers of health care to pregnant women have traditionally relied on the U.S. Department of Agriculture's (USDA) Food Guide Pyramid to counsel and encourage their clients to consume foods that meet the nutritional requirements of pregnancy and, consequently, avoid developing obstetrical complications and low infant-birth weight. The original version of the Food Guide Pyramid (USDA, 1992) outlined an optimal number of servings for each of five food groups (see Figure 1), gained wide public recognition, and was used extensively in education materials on nutrition. Pregnant women were encouraged to consume the larger number of servings per day in each food group. For example, women were counseled to consume at least three servings of milk per day, instead of two, and at least three servings of fruits and four servings of vegetables per day in order to meet the nutritional requirements of pregnancy. Previous research reported that pregnant women readily consumed 6 to 12 servings per day from the bread group and at least three servings of meat per day (Fowles, 2000).
Original (1992) USDA Food Guide Pyramid
The original, visual version of the Food Guide Pyramid did not, however, specify the appropriate volume or weight that was equivalent to one serving within any food group. Some women considered one serving to be a 4- to 6-oz hamburger or 8-oz steak. The misconception often led to the consumption of too many calories and may have contributed to the rising obesity epidemic in postpartum women (Walker et al., 2004).
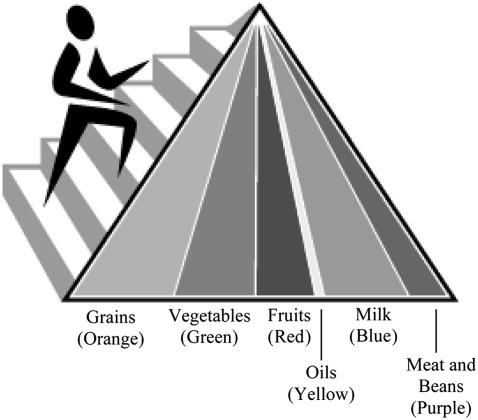
In 2005, the USDA released a new version of the Food Guide Pyramid, also known as “MyPyramid” (USDA, 2005b). The newer pyramid has colored, vertical stripes of varying widths with an outline of a person climbing stairs alongside the pyramid (see Figure 2). Each color represents a different food group: Orange represents the grains food group; green, the vegetables food group; red, the fruits food group; yellow, oils; blue, the milk food group; and purple, the meat-and-bean food group. The stripes also vary in width to signify the relative proportion of food that should be consumed from each food group on any one day. For example, the wide, orange stripe indicates that most of the food eaten in a day should come from the grain food group, while the narrow, yellow stripe indicates that oils and fats should be consumed sparingly. The outline of a person climbing stairs indicates the increased emphasis on exercise and suggests finding a balance between food and exercise, an initiative that is supported by the USDA.
New (2005) USDA Food Guide Pyramid: “MyPyramid”
The revised pyramid does not list the number of servings, nor does it include pictures of food that meet the recommended intake from a food group. The number of calories to be consumed each day varies with gender, age, and activity level (see Table 1). For example, a 20-year-old woman with a sedentary lifestyle should consume 2,000 calories per day, while an active, 28-year-old woman may consume 2,400 calories per day. A 40-year-old man with a low-active lifestyle should consume 2,400 to 2,600 calories per day (not shown in Table 1). In addition, the revised pyramid outlines portion sizes as a volume of food per day rather than a number of servings per food group that vary with the recommended number of calories to be consumed per day (see Table 2).
Table 1.
Levels of Target Energy Intake (Calories per Day) for Childbearing-Aged Women
| Age | Sedentarya | Low-Activeb | Activec |
|---|---|---|---|
| 14–18 years | 1,800 | 2,000 | 2,400 |
| 20–30 years | 2,000 | 2,000–2,200 | 2,400 |
| 35–50 years | 1,800 | 2,000 | 2,200 |
“Sedentary” means a lifestyle that includes only the physical activity of independent living.
“Low-Active” means a lifestyle that includes the equivalent to walking about 1.5–3 miles/day at a rate of 3–4 miles/hour, in addition to the activities of independent living.
“Active” means a lifestyle that includes physical activity equivalent to walking more than 3 miles/day at a rate of 3–4 miles/hour, in addition to the activities of independent living.
Table 2.
Volume of Food per Day From Each Food Group for Various Food Patterns*
| Food Group | 1,800 Calories | 2,000 Calories | 2,200 Calories | 2,400 Calories | 2,600 Calories |
|---|---|---|---|---|---|
| Fruits | 1 c | 1.5 c | 1.5 c | 1.5 c | 2 c |
| Vegetables | 2 c | 2 c | 2 c | 2.5 c | 3 c |
| Dark-green | .43 c | .43 c | .43 c | .50 c | .50 c |
| Deep-yellow | .29 c | .29 c | .29 c | .36 c | .43 c |
| Legumes | .43 c | .43 c | .43 c | .50 c | .50 c |
| Starchy | .36 c | .36 c | .36 c | .50 c | .64 c |
| Other | .50 c | .50 c | .50 c | .64 c | .93 c |
| Grains | 3.5 c | 4 c | 4.5 c | 5 c | 5 c |
| Whole grains | 1.75 c | 2 c | 2.25 c | 2.50 c | 2.50 c |
| Other grains | 1. 75 c | 2 c | 2.25 c | 2.50 c | 2.50 c |
| Meat and beans | 5 oz | 5.5 oz | 6 oz | 6.5 oz | 6.5 oz |
| Milk | 2 or 3 c | 2 or 3 c | 2 or 3 c | 2 or 3 c | 2 or 3 c |
| Additional fats | 36 g | 40 g | 44 g | 46 g | 50 g |
| Added sugar | 32 g (8 tsp) | 40 g (10 tsp) | 48 g (12 tsp) | 56 g (14 tsp) | 64 g (16 tsp) |
c = cup; oz = ounce; g = gram; tsp = teaspoon.
Adapted from the Proposed Daily Food Intake Patterns developed by the Center for Nutrition Policy and Promotion (retrieved April 2, 2006, from http://www.usda.gov/cnpp/pyramid-update/FGP%20docs/TABLE%201.pdf)
MyPyramid is a fresh look at providing guidance to help Americans make healthy food choices and be active every day; however, several problems exist that may confuse pregnant women and health-care providers. The lack of pictures depicting the types of foods and the recommended number of servings within each food group does not readily offer accessible information that can guide women's dietary choices during pregnancy. Ethnically diverse food choices should also be included. Furthermore, although it is relatively easy to navigate through the USDA's MyPyramid Web site to retrieve additional information, important facts and supporting data may not be readily available to some pregnant women, particularly low-income women who do not have access to a computer or the Internet. Additionally, MyPyramid does not offer specific dietary modifications that should be followed during pregnancy, which may be inadequate for health-care professionals seeking to advise pregnant women.
MyPyramid is a fresh look at providing food guidance to help Americans make healthy food choices and be active every day.
REVISED EDITION OF DIETARY GUIDELINES FOR AMERICANS
In 2005, the USDA also released a revised edition of Dietary Guidelines for Americans (USDA, 2005a). The revision emerged as an attempt to stem the increased rate of obesity by encouraging consumers to eat more healthfully and control their weight. The guidelines “encourage Americans to eat fewer calories, be more active and make wiser food choices” (p. vi). Key recommendations in the new guidelines focus on adequate nutrients within calorie needs; weight management; physical activity; food groups to encourage; fats; carbohydrates; sodium and potassium; alcoholic beverages; and, for the first time, food safety. In addition to these key recommendations, the document outlines important recommendations for specific populations, when warranted, such as children, people over 50 years old, and pregnant or breastfeeding women (see Table 3).
Table 3.
Pregnancy-Specific Guidelines from the Dietary Guidelines for Americans 2005*
| Adequate Nutrients Within Calorie Needs |
|---|
| • Women of childbearing age who may become pregnant. Eat foods high in heme-iron and/or consume iron-rich plant foods or iron-fortified foods with an enhancer of iron absorption, such as vitamin C-rich foods. |
| • Women of childbearing age who may become pregnant and those in the first trimester of pregnancy. Consume adequate synthetic folic acid daily (from fortified foods or supplements) in addition to food forms of folate from a varied diet. |
| Weight Management |
| • Pregnant women. Ensure appropriate weight gain as specified by a health-care provider. |
| • Breastfeeding women. Moderate weight reduction is safe and does not compromise weight gain of the nursing infant. |
| Physical Activity |
| • Pregnant women. In the absence of medical or obstetric complications, incorporate 30 minutes or more of moderate-intensity physical activity on most, if not all, days of the week. Avoid activities with a high risk of falling or abdominal trauma. |
| • Breastfeeding women. Be aware that neither acute nor regular exercise adversely affects the mother's ability to successfully breastfeed. |
| Food Groups to Encourage; Fats; Carbohydrates; and Sodium and Potassium |
| • No specific recommendation for pregnant or breastfeeding women. |
| Alcoholic Beverages |
| • Alcoholic beverages should not be consumed by some individuals, including those who cannot restrict their alcohol intake, women of childbearing age who may become pregnant, pregnant and lactating women, children and adolescents, individuals taking medications that can interact with alcohol, and those with specific medical conditions. |
| Food Safety |
| • Pregnant women. Only eat certain deli meats and frankfurters that have been reheated to steaming hot. |
Source: U.S. Department of Agriculture. (2005). Dietary guidelines for Americans 2005. Retrieved March 21, 2006, from http://www.healthierus.gov/dietaryguidelines
INSTITUTE OF MEDICINE GUIDELINES
In 1992, the Institute of Medicine (IOM) published Nutrition during Pregnancy and Lactation: An Implementation Guide, which provides guidelines to counsel pregnant women regarding appropriate dietary intake (see page 45 of the document for specific recommendations for pregnant women). Although the document has served as the “gold standard” for nutritional assessment and dietary counseling, the recommendations do not take into account the results of more recent nutritional research, nor do they synthesize the recommendations within the recent series of Dietary Reference Intakes publications produced by the IOM.
From 1997 through 2005, the IOM published a series of books that offers revisions to the Recommended Dietary Allowances for many of the macronutrients (carbohydrates, proteins, and fats) and micronutrients (sodium, potassium, calcium, iron, etc.) and referred to these recommendations as “Dietary Reference Intakes” or DRIs (IOM, 1997, 1998, 2000, 2001, 2005). The DRIs were developed after extensive review of the nutritional science literature. The reference values, collectively called the DRIs, include the Recommended Dietary Allowance, Adequate Intake, Tolerable Upper Intake Level, and Estimated Average Requirement (see Box 1 for a definition of each parameter). Recommended intake of each nutrient varies with the age, gender, and metabolic state of each individual. For example, recommended levels of nutrient intake are different for healthy adults, children of various ages, elderly adults, and women who are pregnant or breastfeeding (IOM, 2005).
Box 1. Definitions of Dietary Reference Intakes.
Recommended Dietary Allowance (RDA)
The average daily dietary nutrient intake level sufficient to meet the nutrient requirement of nearly all (97–98%) healthy individuals in a particular life stage and gender group.
Adequate Intake (AI)
The recommended average daily intake level based on observed or experimentally determined approximations or estimates of nutrient intake by a group (or groups) of apparently healthy people that are assumed to be adequate—used when an RDA cannot be determined.
Tolerable Upper Intake Level (UL)
The highest average daily nutrient intake level that is likely to pose no risk of adverse health effects to almost all individuals in the general population. As intake increases above the UL, the potential risk of adverse effects may increase.
Estimated Average Requirement (EAR)
The average daily nutrient intake level estimated to meet the requirement of half the healthy individuals in a particular life stage and gender group.a
Retrieved April 2, 2006, from http://fermat.nap.edu/books/0309085373/html/22.html#p2000dc1a8940022001
Permission to reprint received from The National Academies Press.
In the case of energy, an Estimated Energy Requirement (EER) is provided. The EER is the average dietary energy intake that is predicted to maintain energy balance in a healthy adult of a defined age, gender, weight, height, and level of physical activity consistent with good health. In children and pregnant and lactating women, the EER is taken to include the needs associated with the deposition of tissues or the secretion of milk at rates consistent with good health.
Box 2. Suggested Dietary Guidelines for Pregnant Women.
Prior to Pregnancy
Eat iron-rich or iron-fortified foods (meat or meat alternatives, breads, and cereals). Include vitamin C-rich foods (e.g., orange juice, broccoli, or strawberries) to enhance iron absorption.
Take folic acid supplements (400 micrograms), daily.
Eat a well-balanced diet, including 3 to 3.5 cups of fruits and vegetables per day, with a focus on a variety of different colors of these foods.
Eat/Drink 3 cups of milk or calcium-rich foods per day, with a focus on low-fat or skimmed milk products.
Do not consume alcoholic beverages.
During Pregnancy
Continue to follow the recommendations listed above.
Eat enough food to gain weight at the rate recommended by health-care provider, as shown on the Institute of Medicine's weight-gain chart (IOM, 1992, p. 44).
No need exists to increase food intake in the first trimester; however, continue to eat well-balanced meals. Increase food intake by only 340 calories per day during the second trimester and 450 calories per day during the third trimester.
Do not skip meals. Eat three small- to moderate-sized meals at regular intervals and two to three nutritious snacks (fruits/vegetables) per day.
If no medical or obstetrical complications exist, exercise 30 minutes or more, employing a moderate intensity of physical activity, on most, if not all, days of the week. Examples include walking briskly (about 3.5 miles per hour); hiking; gardening or yard work; dancing; golf (walking and carrying clubs); bicycling (less than 10 miles per hour); weight training (general, light workout).
Only eat hot dogs and deli meats that have been reheated to steaming hot.
Breastfeeding
Losing weight after giving birth does not affect the nursing newborn's weight gain.
Exercise does not affect the ability to successfully breastfeed.
Adapted from the following sources:
Institute of Medicine. (1992). Nutrition during pregnancy and lactation: An implementation guide. Washington, DC: The National Academies Press.
Institute of Medicine. (2005). Dietary Reference Intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids (macronutrients). Washington, DC: The National Academies Press.
U.S. Department of Agriculture. (2005a). Dietary guidelines for Americans 2005. Retrieved March 21, 2006, from http://www.healthierus.gov/dietaryguidelines/
U.S. Department of Agriculture. (2005b). MyPyramid.gov. Retrieved March 21, 2006, from http://www.mypyramid.gov/
In 2005, the IOM also outlined the number of additional calories that pregnant women should consume. During pregnancy, the pattern of weight gain is more influential in contributing to a positive birth outcome than the total amount of weight gain alone. Women with slow weight gain during the second and third trimesters of pregnancy are more likely to develop preterm labor and, subsequently, give birth to preterm infants (Carmichael & Abrams, 1997; Carmichael, Abrams, & Selvin, 1997; Hickey, Cliver, McNeal, Hoffman, & Goldenberg, 1995; Muscati, Gray-Donald, & Koski, 1996; Siega-Riz et al., 1996). The recently released Dietary Reference Intakes for energy (IOM, 2005) recommends that pregnant women from 14 to 50 years old consume no additional calories in the first trimester of pregnancy over the level recommended in the USDA MyPyramid. However, an additional 340 kilocalories per day in the second trimester and 450 kilocalories per day in the third trimester are needed to meet the energy requirements to support the increased maternal-metabolic rate and to foster adequate fetal growth (IOM, 2005).
IMPLICATIONS FOR PRACTICE AND NUTRITIONAL RECOMMENDATIONS
Assessing pregnant women's nutritional knowledge may be more difficult because the health-care provider may be unfamiliar with the varying volumes of intake recommended for the different age groups and activity levels. The public's lack of familiarity with specific recommendations presented in the new pyramid and limited access to educational materials also may hinder perinatal educators' ability to provide nutritional guidance to pregnant women. No governmental agency has synthesized the recommendations from the various sources into an easy-to-use guide to assist health-care providers and perinatal educators with dietary counseling for pregnant women. The recommendations outlined in Box 2 represent an initial attempt to provide such a guide.
Health-care providers and perinatal educators need to become familiar with newer dietary recommendations for pregnant women to ensure that mothers eat foods that contribute to adequate birth weight, prevent obstetrical complications, and promote a woman's postnatal health.
Health-care providers and perinatal educators need to become familiar with newer dietary recommendations for pregnant women.
Footnotes

Source: The U.S. Department of Agriculture and the U.S. Department of Health and Human Services.

Image retrieved April 2, 2006, from the following link on the U.S. Department of Agriculture Web site: http://www.mypyramid.gov
Editor's note: Subheadings that identify colors are added here to the original image, due to this journal's black-and-white reproduction.

References
- Carmichael S, Abrams B. A critical review of the relationship between gestational weight gain and preterm delivery. Obstetrics & Gynecology. 1997;89(5):865–873. doi: 10.1016/s0029-7844(97)00047-1. [DOI] [PubMed] [Google Scholar]
- Carmichael S, Abrams B, Selvin S. The association of pattern of maternal weight gain with length of gestation and risk of spontaneous preterm delivery. Paediatric and Perinatal Epidemiology. 1997;11:392–406. doi: 10.1046/j.1365-3016.1997.d01-28.x. [DOI] [PubMed] [Google Scholar]
- Fowles E. Comparing pregnant women's nutritional knowledge to their actual dietary intake. MCN: The American Journal of Maternal/Child Nursing. 2000;27:171–177. doi: 10.1097/00005721-200205000-00009. [DOI] [PubMed] [Google Scholar]
- Godfrey K. M, Barker D. J. Fetal programming and adult health. Public Health Nutrition. 2001;4(2b):611–624. doi: 10.1079/phn2001145. [DOI] [PubMed] [Google Scholar]
- Hickey C, Cliver S, McNeal S, Hoffman H, Goldenberg R. Prenatal weight gain patterns and spontaneous preterm birth among non-obese black and white women. Obstetrics & Gynecology. 1995;85(6):909–914. doi: 10.1016/0029-7844(95)00067-2. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. 1992. Nutrition during pregnancy and lactation: An implementation guide. Washington, DC: The National Academies Press.
- Institute of Medicine. 1997. Dietary Reference Intakes for calcium, phosphorus, magnesium, vitamin D and fluoride. Washington, DC: The National Academies Press.
- Institute of Medicine. 1998. Dietary Reference Intakes for thiamine, riboflavin, niacin, vitamin B6, vitamin B12, pantothenic acid, biotin, and choline. Washington, DC: The National Academies Press.
- Institute of Medicine. 2000. Dietary Reference Intakes for vitamin C, vitamin E, selenium, and carotenoids. Washington, DC: The National Academies Press.
- Institute of Medicine. 2001. Dietary Reference Intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, manganese, molybydenium, nickel, silicon, vanadium, and zinc. Washington, DC: The National Academies Press.
- Institute of Medicine. 2005. Dietary Reference Intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids (macronutrients). Washington, DC: The National Academies Press.
- Muscati S, Gray-Donald K, Koski K. Timing of weight gain during pregnancy: Promoting fetal growth and minimizing maternal weight retention. International Journal of Obesity. 1996;20:526–532. [PubMed] [Google Scholar]
- Siega-Riz A, Adair L, Hobel C. Maternal underweight status and inadequate rate of weight gain during the third trimester of pregnancy increases the risk of preterm delivery. Journal of Nutrition. 1996;126:146–153. doi: 10.1093/jn/126.1.146. [DOI] [PubMed] [Google Scholar]
- Smith G. First trimester origins of fetal growth impairment. Seminars in Perinatology. 2004;28:41–50. doi: 10.1053/j.semperi.2003.10.012. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture [USDA]. 1992. The Food Guide Pyramid. Retrieved April 2, 2006, from http://www.nal.usda.gov/fnic/Fpyr/pmap.htm.
- U.S. Department of Agriculture [USDA]. 2005a. Dietary guidelines for Americans 2005. Retrieved March 21, 2006, from http://www.healthierus.gov/dietaryguidelines/
- U.S. Department of Agriculture [USDA]. 2005b. MyPyramid.gov. Retrieved March 21, 2006, from http://www.mypyramid.gov/
- Walker L. O, Freeland-Graves J. H, Milani T, George G, Hanss-Nuss H, Kim M. Weight and behavioral and psychosocial factors among ethnically diverse, low-income women after childbirth: II. Trends and correlates. Women and Health. 2004;40:19–34. doi: 10.1300/J013v40n02_02. et al. [DOI] [PubMed] [Google Scholar]