Abstract
Objective
This study examined the association of trajectories of heavy episodic drinking (at least five alcoholic drinks on one occasion) during adolescence with health status and practices at age 24.
Method
Semi parametric group-based modeling and logistic regressions were used to analyze data from a longitudinal panel of 808 youths interviewed between 10 and 24 years of age.
Results
Four distinct trajectories of adolescent heavy episodic drinking were identified: nonheavy drinkers, late onsetters, escalators and chronic heavy drinkers. Overall, young adults who did not engage in heavy episodic drinking during adolescence had the lowest occurrence of health problems and were most likely to engage in safe health behaviors at age 24. Chronic and late-onset heavy episodic drinking during adolescence had negative effects on health status and practices at age 24. Adolescent chronic heavy drinkers were more likely 10 be overweight or obese and to have high blood pressure at age 24 than those who did not drink heavily in adolescence. Late-onset heavy drinkers were less likely to engage in safe driving practices at age 24 and were more likely to have been ill in the past year than adolescents who did not drink heavily. These health disparities remained even after current frequency of heavy episodic drinking at age 24, other adolescent drug use, ethnicity, gender and family poverty were controlled.
Conclusions
Heavy episodic alcohol use during adolescence has long-term, negative health consequences. Distinct patterns of adolescent heavy drinking affect health status and practices in young adulthood differently.
Drinking at least five alcoholic drinks on one occasion (called heavy episodic or binge drinking by some; Kandel, 1980; White, 1987; Zucker and Gomberg, 1986) is a relatively common behavior among adolescents in the United States. According to the most recent Monitoring the Future study (Johnston et al., 2002), 25% of 10th-grade and 30% of 12th-grade students had at least five drinks in a row during the 2 weeks before the survey. Certain patterns of drinking—particularly heavy, frequent and prolonged use of alcohol during adolescence—are especially detrimental to the health of adolescents and young adults (Aarons et al., 1999; Johnson and Richter, 2002), Some health effects of adolescent heavy episodic drinking are immediate and already observable in adolescence, including reduced nervous and cognitive functioning and reduced general physical well-being (e.g., fatigue, headaches and sleeping problems; Arria et al., 1995; Brook et al., 2002; Brook et al., 2000; Hansell et al., 1991; Hansell and White, 1999; Johnson and Richter, 2002; National Institute on Alcohol Abuse and Alcoholism, 2000). It is less clear, however, whether adolescent heavy drinking has long-term health consequences.
Some patterns of adolescent alcohol use may have long-term health consequences beyond the immediate effects in adolescence. For example, early-onset, heavy adolescent alcohol use has been linked with continued alcohol abuse and dependence in adulthood (Guo et al., 2000), which in turn have been associated with negative physical and mental health consequences (e.g., coronary heart disease, hypertension, mood and personality disorders and aggression; Brook et al., 2000; National Institute on Alcohol Abuse and Alcoholism, 2000).
Life-span developmental research suggests that adolescence (approximately ages 12–18) and emerging adulthood (approximately ages 12–25) are theoretically and empirically distinct developmental periods (see Arnett 1998, 2000; Furstenberg, 2000; Shanahan, 2000). Compared with alcohol use in young adulthood, drinking in adolescence is deemed age-inappropriate and precocious behavior and is illegal in the United Stales. The context and meaning of adolescent drinking, and probably its consequences, are, therefore, different from alcohol consumption in young adulthood, which is legal at age 21. Furthermore, trajectories of early heavy drinking are associated with later alcohol abuse and dependence in young adulthood as well as with numerous negative social and personal outcomes (Guo et al., 2002; Hill et al., 2000; Kandel et al., 1986; Newcomb and Bentler, 1987, 1988). Focusing an alcohol use during adolescence is important because it sets the stage for later alcohol misuse and health problems and, therefore, has unique implications for prevention. Thus, in the present study we chose to examine the impact of heavy episodic drinking trajectories during the junior high and high school years (ages 13–18) on health behaviors and statuses in emerging adulthood (age 24).
Our understanding of substance use consequences is enhanced by a person-centered approach, because different trajectories of substance use in adolescence may have different consequences in young adulthood (Guo et al., 2002; Hill et al., 2000; Labouvie et al., 1991), Prior analyses of our panel data have identified distinct trajectories of alcohol use in adolescence (Guo et al., 2000, 2002; Hill et al., 2000). As have others (Muthén and Shedden, 1999; Schulenberg et al., 1996), Hill et al., (2000) identified four types of adolescent heavy episodic drinkers: those who never or rarely drank heavily (nonheavy drinkers); those who increased their involvement in heavy episodic drinking in mid adolescence (escalators); those who began heavy drinking only in late adolescence (late onsetters); and those who engaged in high levels of heavy episodic drinking throughout the adolescent years (chronic heavy drinkers). Hill et al., (2000) showed that these four heavy episodic drinking trajectories had distinctly different patterns of prosocial (e.g., academic attainment and social involvement) and antisocial (e.g., depression and crime) functioning at age 21.
Different adolescent heavy episodic drinking trajectories also may have different consequences for health outcomes in young adulthood. Different patterns of alcohol use may influence health directly and indirectly (Aarons et al., 1999; Brook et al., 2002). On the one hand, alcohol has a direct physiological effect due to its toxicity to the body, Based on their long-term heavy use of alcohol, we would expect to see physical health problems in young adulthood, especially among chronic heavy drinkers. Negative health effects also could be expected for escalators, who delayed their frequent involvement in heavy drinking until mid adolescence but rapidly increased the frequency of heavy drinking subsequently. By age 18, escalators had the highest frequency of heavy episodic drinking of all groups. Despite this rapid increase, however, physical health problems may not yet be observable in the escalator group at age 24, because they lack chronic or long-term exposure to alcohol and their heavy drinking occurs during a time when the body’s ability to recover from the physical effects of alcohol consumption may be high (Schulenberg et al., 2002).
Alcohol use also may affect health indirectly as a result of its association with such behaviors as risk taking, delinquency and violence, as well as other substance use, including smoking. We observed such behavioral patterns in late onsetters and escalators, who were more likely to participate in risky sex at age 21 and to continue using alcohol and drugs during young adulthood (Guo et al., 2002; Hill et al., 2000). These findings suggest that their risk-taking behavior also may extend to health-related practices. In comparison, nonheavy drinkers should have the lowest occurrence of health problems and should be most likely to engage in safe health practices.
Because clinical or chronic diseases still tend to be rare in young adulthood, health consequences of adolescent alcohol misuse in the early 20s are most likely to be observable in general health-related practices and in health conditions that may foreshadow later, more serious adult health problems and diseases (Arria et al., 1995; Johnson and Richter, 2002; Newcomb and Bentler, 1987), In the present study, we focused on common health behaviors (seat belt use, safe driving and physical activity) and general health conditions (overweight and obesity, hypertension and illness), which increase the risk for illness, injury or disease, including cardiovascular disease, diabetes and coronary heart disease (National Heart, Lung, and Blood Institute [NHLBI], 1997, 1998a, 2000). Using the previously identified developmental trajectories of adolescent heavy episodic drinking in our panel data (Hill et al., 2000), we examined the association of heavy drinking during adolescence with health status and practices at age 24.
Method
Sample
We used prospective data from the Seattle Social Development Project (SSDP), a longitudinal study of the development of prosocial and antisocial behaviors. In 1985, 18 Seattle, Washington, elementary schools that served students from high crime neighborhoods were identified. The study population included all fifth graders in these schools (N = 1,053). A total of 808 students (77% of the identified population) and their families agreed to participate in the longitudinal study. This acceptance rate is comparable to that in other studies that have recruited children and adolescents (Ellickson and Bell, 1990; Elliott et al., 1981; Thornberry et al., 1990).
In Grades 5 and 6, questionnaires were group administered in project schools and completed in class. Youths who left project schools were interviewed individually. All students were interviewed individually in person, starting in 1988 at age 13, in the spring of each succeeding year through age 16 in 1991 and again at age 18 in 1993. In young adulthood, participants were interviewed in person at age 21 (1996) and at age 24 (1999), Respondents were tracked and interviewed wherever they moved. Retention rates for the sample have remained above 93% since 1989, when participants were 14 years old. In the 1999 assessment at age 24, 752 respondents (95% of the 793 still-living panel members) participated in the study. In this analysis, we used heavy episodic drinking trajectories from ages 13 through 18 to predict health status and practices at age 24.
The sample comprised approximately equal numbers of males (n = 412) and females (n = 396). A substantial proportion of the participants were from low-income families. Forty-six percent of parents reported a maximum family income under $20,000 per year. More than 52% of the panel members were from families in poverty, as evidenced by participation in the National School Lunch/School Breakfast Program between the ages of 10 and 12. Forty-two percent of the sample reported only one parent present in the home when the participants were in fifth grade. About 44% were European American, 26% were African American, 22% were Asian American, 5% were Native American and 3% were from other racial/ethnic groups.
Measures
Health statuses and behaviors
We measured several health statuses and behaviors at age 24. In order to model nontrivial differences in health outcomes measured on a continuous scale, we used established cutoff points that define clinically significant thresholds for health risks. For example, body mass index (BMI) and waist circumference are indicators of health risks associated with overweight and obesity (NHLBI, 2000), According to NHLBI standards (2000), a BMI between 25 and 30 indicates overweight, and a BMI of 30 or greater indicates obesity, We calculated the participants’ BMI based on their self-reported height and weight and created a binary variable indicating whether respondents were overweight or obese (coded 1 if BMI ≥25) or not (coded 0).
The risk of disease (such as diabetes and hypertension) is increased for waist sizes that are greater than 35 inches for women and greater than 40 inches for men (NHLBI, 2000). Using these sex-specific cutoff points, we categorized male and female respondents, based on their self-reported waist circumference, into high-risk (coded 1) and low-risk (coded 0).
Hypertension in adults is defined as systolic blood pressure of 140 mm Hg or greater and diastolic pressure of 90 mm Hg or greater (NHLBI, 1997). Interviewers look two consecutive readings of the respondent’s blood pressure at the time of the age-24 interview, using an automatic blood pressure monitor. We computed the average of the two measurements for the systolic and diastolic blood pressure and, based on the NHLBI criteria, created a binary variable that indicates whether respondents had hypertension (1 = yes) or not (0 = no).
In addition, we asked participants whether they had had any of 18 illnesses and conditions in the past year. In order of prevalence, these illnesses included asthma or emphysema (14%), high blood pressure (8%), arthritis (6%), high cholesterol (3%), diabetes (3%), thyroid condition (2%), peptic ulcer (2%), radiation (2%), tuberculosis (1%), cancer (other than breast or colon cancer, 1%), heart disease (1%), hepatitis (1%), seizures (1%), stroke (1%), glaucoma (1%), hysterectomy (<1%), breast cancer (<1%) and colon cancer (<1%). Ninety percent of the respondents reported a total number of one or two illnesses or conditions. To assess hardiness and overall health, we coded respondents as having been ill in the past year equal to 1 (0 otherwise) if they checked any of the listed conditions. Because health conditions other than asthma, high blood pressure and arthritis were rare at this age, each illness was weighted equally.
Health behavior data were available for driving-related behaviors (seat belt use and safe driving) and regular exercise. We grouped participants into those who reported always or nearly always wearing their seat belt when in a car (coded 1) and those who did not (coded 0). Respondents who practiced safe driving were defined as not driving when they had had too much alcohol or drugs and not riding in a car with a driver who had had too much alcohol or drugs (coded 1, 0 otherwise). Finally, participants who exercised at least three times per week for at least 30 minutes with at least moderate intensity were coded as being physically active (coded 1, 0 otherwise). This classification corresponds to guidelines set by the NHLBI (1998b) for physical activity necessary to achieve weight loss and reduce risks of cardiovascular disease and diabetes.
Adolescent heavy episodic drinking
We measured heavy episodic use of alcohol by using the participants’ report of the number of times they drank at least live alcoholic drinks in a row in the last month. We used repeated measures of frequency of heavy episodic drinking at each of five measurement occasions (i.e., ages 13, 14, 15, 16 and 18). We did not use a gender-specific cutoff (e.g., four drinks in a row for girls and five drinks in a row for boys) when measuring heavy episodic drinking, because only the question about five drinks or more was available for the entire period used to define the adolescent drinking trajectories (ages 13–18). Based on semiparametric group-based modeling (SGM; Nagin, 1999), participants were assigned to one of four trajectories of adolescent heavy episodic drinking as previously identified in this sample (see Hill et al., 2000), Seventy percent of the panel members were most likely to never, or rarely, drink heavily during adolescence (nonheavy drinkers; n = 568); 23% began heavy use of alcohol more frequently late in adolescence, after age 16 (late onsetters; n = 167); 4% sharply and continuously increased the frequency of their heavy drinking during mid adolescence, starting around age 15 (escalators; n = 31); and 3% engaged in heavy episodic drinking at high levels throughout adolescence (chronic heavy drinkers; n 26). Figure 1 shows the observed heavy episodic drinking trajectories.
Figure 1.
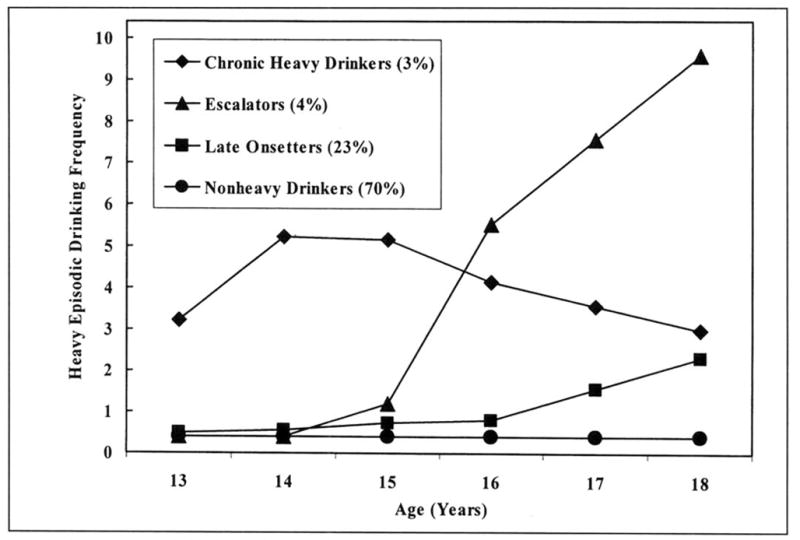
Adolescent heavy episodic drinking trajectories in the SSDP sample
Gender, ethnicity and socioeconomic status
Health status and behaviors are associated with gender, ethnicity and socioeconomic status (Aarons et al., 1999; Goodman et al., 1997; Johnson and Richter, 2002; Johnston et al., 2002; Newcomb and Bentler, 1987; Schulenberg et al., 1996). Therefore, we controlled these factors to estimate the unique effect that heavy episodic drinking trajectories may have on health in young adulthood. We included self-reported sex (1 = male, 0 = female) and ethnicity (dummy variables for African American, Asian American, Native American and other ethnicity, with European American as the reference category). Participation in the National School Lunch/School Breakfast Program (available from school records) defined respondents’ poverty status in adolescence (1 = eligible for free school lunch in Grades 5 or 6, 0 = not eligible).
Adolescent substance use and age-24 heavy episodic drinking
Heavy episodic drinking typically occurs in conjunction with the use of other drugs, such as tobacco and marijuana (Johnson et al., 2000; Kandel, 1980; White, 1987). To control the possibly confounding effect of other substance use during adolescence on health outcomes at age 24, we included a summary measure of drug use between ages 13 and 18. We standardized and summed the average frequency of cigarette smoking, marijuana use and other illicit drug use between ages 13 and 18.
We also included a variable indicating the frequency of heavy episodic drinking at age 24 to assess the possibility that the effect of adolescent heavy drinking trajectories on young adult health outcomes is mediated through current levels of heavy use at age 24 and other processes that might be associated with current heavy drinking. Heavy episodic drinking at age 24 was measured us the number of times participants reported having five or more drinks on one occasion during the past month.
Missing data and analysis procedures
SGM makes full use of available data in determining parameter estimates and their standard errors, and it includes all subjects who have at least two data points (Jones et al., 2002), Therefore, heavy episodic drinking trajectory variables contained missing data when no, or only one, wave of data was available. Heavy episodic drinking trajectories could be estimated for 792 (98%) of the 808 study participants.
Other missing data in the final data set were imputed using the multiple imputation procedure in the SAS/STAT software, version 8.2. (aSAS Institute, 2002a). This approach results in less bias than alternative procedures, such as list-wise deletion (Graham et al., 1997; Little and Rubin, 1987; Schafer 1997), and it provides less biased parameter estimates than other methods even if the missing-at-random assumption is not fully met (Collins et al., 2001; Schafer and Graham, 2002). All regression results reported here are the averages of 20 imputed data sets using the MIANALYZE procedure (bSAS Institute, 2002b) in the SAS/STAT software, version 8.2.
All young adult health outcomes were measured as binary variables and were analyzed using cross-tabulations and logistic regressions. We report overall chi-square values for differences in proportions from the bivariate cross-tabulation and odds ratios from the multiple logistic regressions for the heavy episodic drinking trajectory groups (with nonheavy drinkers us the reference category), adjusted for gender, ethnicity, poverty, adolescent substance use and age-24 heavy use of alcohol.
Results
Table 1 shows the prevalence of health practices and statuses at age 24 for the total sample and by adolescent heavy episodic drinking trajectory group. Overall, the heavy episodic drinking trajectory groups differed significantly on seat belt use, safe driving and overweight/obesity. Note that high-risk waist size, hypertension and illness in the past year were more prevalent among chronic heavy drinkers than in the other groups.
Table 1.
Prevalence of health practices and statuses at age 24 by adolescent heavy episodic drinking trajectories
| Health practices and statuses at age 24
|
|||||||
|---|---|---|---|---|---|---|---|
| Use seat belt (%) | Practice safe driving (%) | Physically active (%) | Overweight or obese (%) | High-risk waist size (%) | Hypertension (%) | Had been ill (%) | |
| Total sample (N = 792) | 82.2 | 63.8 | 38.1 | 50.8 | 14.0 | 16.7 | 29.7 |
| Nonheavy drinkers (n = 568) | 85.2 | 70.1 | 37.8 | 47.8 | 14.1 | 15.5 | 27.9 |
| Late onsetters (n = 167) | 78.1 | 47.5 | 37.1 | 513 | 11.7 | 17.5 | 35.0 |
| Escalators (n = 31) | 67.9 | 42.9 | 50.0 | 60.7 | 12.5 | 13.6 | 17.9 |
| Chronic heavy drinkers (n = 26) | 70.8 | 62.5 | 39.1 | 78.3 | 25.0 | 35.0 | 37.5 |
| χ2 | 11.3* | 32.8‡ | 1.8 | 9.9* | 2.7 | 5.5 | 5.5 |
p < .05;
p < .001.
Table 1 shows that chronic heavy drinkers had the most negative health profile of the four groups at age 24, with elevated risk for overweight and obesity, high-risk waist size, hypertension and illness. They also engaged less in safe health behaviors. In contrast, nonheavy drinkers exhibited a more positive pattern of health behaviors and statuses. Escalators and late onsetters generally fell between the chronic heavy drinkers and nonheavy drinkers. Escalators were the least likely to use seat belts and to engage in safe driving practices and showed a higher prevalence of overweight and obesity. Late onsetters also were less likely to participate in safe driving behavior and had a higher occurrence of illness in the past year.
Tables 2 and 3 show the results from the logistic regression analyses for the three health practices and the four health status outcomes, respectively. We estimated two models for each outcome. Model 1 comprised the heavy episodic drinking trajectory groups and the adolescent control variables. In Model 2, we added age-24 heavy episodic drinking frequency to test whether the more proximal measure of young adult heavy drinking mediates the influence of adolescent drinking patterns. Because heavy episodic drinking tends to co-occur with smoking, we also estimated a model that included age-24 smoking (during the past month) as an additional covariate. We found that smoking does not act as a mediator of the association between adolescent heavy drinking and young adult health; nor does its inclusion affect any of the other coefficients in the model. Thus, we excluded agc-24 smoking from the analysis presented here.
Table 2.
Logistic regression of health practices at age 24 on adolescent heavy episodic drinking (odds ratios)
| Seat belt use
|
Safe driving
|
Physically active
|
||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Heavy episodic drinking (ages 13–18) | ||||||
| Late onsettersa | 0.67 | 0.76 | 0.50‡ | 0.65* | 0.73 | 0.74 |
| Escalatorsa | 0.47 | 0.51 | 0.57 | 0.77 | 1.15 | 1.16 |
| Chronic heavy drinkersa | 0.46 | 0.44 | 1.14 | 1.40 | 0.79 | 0.79 |
| Frequency of heavy drinking (age 24) | – | 0.90† | – | 0.63‡ | – | 0.98 |
| Gender | ||||||
| Male vs female | 0.33‡ | 0.38‡ | 0.45‡ | 0.66* | 2.75‡ | 2.80‡ |
| Ethnicity | ||||||
| African Americanb | 0.64§ | 0.63§ | 1.39 | 1.42 | 1.02 | 1.02 |
| Asian Americanb | 0.70 | 0.68 | 1.90† | 1.79* | 0.63* | 0.63* |
| Native Americanb | 0.98 | 1.27 | 1.54 | 2.05§ | 1.49 | 1.52 |
| Otherb 0.92 | 0.90 | 0.92 | 0.91 | 1.06 | 1.06 | |
| Poverty (ages 10–12) | ||||||
| Eligible for free lunch vs not | 0.92 | 0.89 | 1.16 | 1.05 | 0.81 | 0.80 |
| Other drug use (ages 13–18) | 0.92 | 1.01 | 0.76* | 0.80 | 1.07 | 1.08 |
| Δ (−2 log likelihood) | – | 10.97‡ | – | 66.24‡ | – | 0.32 |
| Δ (degrees of freedom) | – | 1 | – | 1 | – | 1 |
Notes: Reported estimates are odds ratios; Models 1 and 2 are equivalent, except for the addition of heavy episodic drinking at age 24 in Model 2.
Reference group is nonheavy drinkers.
Reference group is European American.
p<.10;
p<.05;
p<.01;
p<.001.
Table 3.
Logistic regression of health statuses at age 24 on adolescent heavy episodic drinking (odds ratios)
| Overweight/obese
|
High-risk waist size
|
Hypertension
|
Had been ill
|
|||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Heavy episodic drinking (ages 13–18) | ||||||||
| Late onsettersa | 1.21 | 1.19 | 1.31 | 1,30 | 0.98 | 0.86 | 1.54* | 1.51§ |
| Escalatorsa | 1.49 | 1.48 | 1.51 | 1.51 | 0.79 | 0.74 | 0.57 | 0.54 |
| Chronic heavy drinkersa | 3.71* | 3.71* | 2.39 | 2.39 | 3.29* | 3.60* | 1.22 | 1.23 |
| Frequency of heavy drinking (age 24) | – | 1.02 | – | 1.01 | – | 1.12† | – | 1.02 |
| Gender | ||||||||
| Male vs female | 1.52† | 1.49* | 0.15‡ | 0.15‡ | 2.86‡ | 2.51‡ | 0.55‡ | 0.54‡ |
| Ethnicity | ||||||||
| African Americanb | 3.19‡ | 3.19‡ | 2.16† | 2.16† | 1.08 | 1.09 | 1.46§ | 1.46§ |
| Asian Americanb | 0.87 | 0.87 | 0.52§ | 0.52§ | 0.82 | 0.84 | 1.07 | 1.07 |
| Native Americanb | 1.60 | 1.57 | 0.87 | 0.86 | 1.08 | 0.86 | 0.64 | 0.63 |
| Otherb 1.77 | 1.77 | 0.53* | 0.53* | 1.09 | 1.12 | 0.84 | 0.84 | |
| Poverty (ages 10–12) | ||||||||
| Eligible for free lunch vs not | 0.99 | 1.00 | 1.70 | 1.70 | 1.12 | 1.16 | 1.40§ | 1.42§ |
| Other drug use (ages 13–18) | 0.93 | 0.93 | 0.76 | 0.76 | 0.90 | 0.79 | 1.19 | 1.17 |
| Δ (−2 log likelihood) | – | 0.41 | – | 0.09 | – | 11.39‡ | – | 0.73 |
| Δ (degrees of freedom) | – | 1 | – | 1 | – | 1 | – | 1 |
Notes: Reported estimates are odds ratios; Models 1 and 2 are equivalent, except for the addition of heavy episodic drinking at age 24 in Model 2.
Reference group is nonheavy drinkers.
Reference group is European American.
p<.10;
p<.05;
p<.01;
p<.001.
Table 2 shows that safe driving was the only health practice measured here that had a significant relationship with adolescent heavy episodic drinking independent of young adult heavy episodic drinking and the other control variables. Consistent with the bivariate findings presented in Table 1, the multiple regression results in Table 2 show that late onsetters had a significantly lower odds ratio (OR = 0.65) of practicing safe driving than nonheavy drinkers, but they had odds similar to those of chronic heavy drinkers (analysis not shown). None of the other groups were different from each other in their driving practices. Adolescent heavy episodic drinking did not have a significant independent association with seal belt use and physical activity at age 24 in this sample. Frequent heavy episodic drinking at age 24, however, decreased the contemporaneous likelihood of using a seat belt and practicing safe driving (Model 2).
Table 3 shows that young adults who were chronic heavy drinkers during adolescence were more than three and a half times as likely to he overweight or obese (OR = 3.71) and to have hypertension (OR = 3.60) at age 24, compared with nonheavy drinkers, even when we controlled for age-24 frequency of heavy episodic drinking, poverty, gender, ethnicity and other drug use. Their odds of overweight or obesity (OR = 3.25) and hypertension (OR = 4.01) also were significantly greater than those of the late onsetters (analysis not shown). High-risk waist size at age 24 was not associated with adolescent or young adult heavy episodic drinking. Young adults who began drinking heavily late in adolescence (late onsetters) had significantly greater odds of having been ill in the past year, compared with nonheavy drinkers (OR = 1.54). This relationship was reduced to marginal significance when we controlled for age-24 frequency of heavy episodic drinking. The likelihood of late onsetters having been ill was similar to that of chronic heavy drinkers (OR = 1.22; analysis not shown).
Tables 2 and 3 also show that poverty, ethnicity and other drug use during adolescence were not consistently associated with health outcomes at age 24, although African Americans were at significantly greater risk than European Americans for overweight/obesity and high-risk waist size. Asian Americans in this sample were significantly more likely to practice safe driving but significantly less likely to be physically active than European Americans. These differences by ethnicity are found even after controlling for poverty, gender, adolescent other drug use and current heavy drinking.
In contrast, gender was associated with all the health practices and statuses in young adulthood measured here, independent of alcohol and other substance use, ethnicity and socioeconomic background. When compared with young women, young men in this sample were less likely to engage in safe health behaviors, such as seat belt use and safe driving, but were more likely to be physically active. Young men in the sample were more likely than young women to be overweight or obese and to have hypertension at age 24, but they were less likely than young women to have been ill in the past year.
Discussion
This study examined the relationship between adolescent heavy episodic drinking trajectories and young adult health outcomes at age 24. As expected, young adults in this sample who did not engage in heavy episodic drinking during adolescence had the lowest occurrence of health problems and were most likely to engage in safe health behaviors at age 24. Patterns of chronic and late-onset heavy drinking in adolescence had negative consequences for later health. Compared with young adults who did not drink heavily during adolescence, chronic heavy drinkers during adolescence showed signs at age 24 of increased risk for poor health and serious disease. They were three and a half to four times as likely to be overweight or obese and to have high blood pressure as those who did not drink heavily in adolescence. This finding is consistent with our expectation that adolescent chronic heavy drinkers would have poorer health in young adulthood based on their long-term exposure to heavy alcohol use.
Also consistent with our prediction, young adults who began heavy episodic drinking late in adolescence (late onsetters) but increased the frequency to levels similar to the chronic heavy drinkers by age 18 were less likely than were adolescents who did not drink heavily to engage in safe health-related behaviors and to have good health at age 24. Late onsetters were less likely to practice safe driving and were one and a half times as likely to have been ill in the past year as adolescents who did not drink heavily. The reduced hardiness in young adulthood of adolescents who began drinking late in adolescence may be an indication of more serious health consequences later on in life. It is important to emphasize that, because our analyses controlled for confounding factors, these health disparities among types of adolescent heavy episodic drinkers occur independent of young adult heavy episodic drinking (at age 24) and cannot be attributed to other adolescent drug use, ethnicity, gender or family poverty.
Contrary to our expectation that the accelerated increase in heavy drinking of the escalators group would be accompanied by a greater tendency to engage in risky health practices at age 24 (but not necessarily show any physical health problems at this age), escalators in this sample did not differ in their health status and behaviors at age 24 from the other three groups. It is noteworthy, however, that the bivariate results suggested a tendency toward unsafe health practices. The main effects in Table 1 indicate that escalators were less likely to use their seat belt and to practice safe driving, compared with young adults who did not drink heavily as adolescents. This difference is marginally significant (p < .10) even when we controlled for poverty, ethnicity and gender, yet it becomes insignificant when we accounted for other drug use during adolescence. Examination of a broader range of health practices with a larger sample of escalators and, in particular, following them over a longer period of time may reveal evidence of adverse health outcomes for this group.
This study contributes to the understanding of the developmental links between heavy episodic drinking in adolescence and long-term health consequences. Although our analyses do not allow causal conclusions, the longitudinal character of our data and the inclusion of major confounding factors provide strong evidence for a connection between patterns of heavy episodic drinking in adolescence and young adult health above and beyond young adult heavy episodic drinking. Future research needs to examine the direct and indirect mechanisms that link adolescent heavy episodic drinking and young adult health. Future investigations also may consider whether our findings are replicated when a gender-specific measure of heavy episodic drinking is used and when the research is extended to a broader range of health-related behaviors.
The present findings indicate that heavy episodic drinking in adolescence has long-term health consequences beyond adolescence. Furthermore, distinct patterns of heavy episodic drinking have different consequences. Late-onset heavy episodic drinking in high school has some health consequences by age 24, but chronic heavy episodic drinking during adolescence is especially detrimental to young adult health and health-related behaviors.
Footnotes
This research was supported by National Institute on Drug Abuse grants R01DA09679 and P50DA10075, National Institute on Alcohol Abuse and Alcoholism grant R21AA10989-01 and a gram from the Robert Wood Johnson Foundation. Points of view expressed are those of the authors and are not the official positions of the funding agencies. This article was presented in a poster session at the 10th Annual Meeting of the Society for Prevention Research, Seattle, Washington, May 29-June 1 2002.
References
- Aarons GA, Brown SA, Coe MT, Myers MG, Garland AF, Ezzet-Lofstram R, Hazen AL, Hough RL. Adolescent alcohol and drug abuse and health. J Adolesc Hlth. 1999;24:412–421. doi: 10.1016/s1054-139x(99)00006-3. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Learning to stand alone: The contemporary American transition to adulthood in cultural and historical context. Human Devel. 1998;41:295–315. [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Amer Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- Arria AM, Dohey MA, Mezzich AC, Bukstein OG, Van Thiel DH. Self-reported health problems and physical symptomatology in adolescent alcohol abusers. J Adolesc, Hlth. 1995;16:226–231. doi: 10.1016/1054-139X(94)00066-N. [DOI] [PubMed] [Google Scholar]
- Brook JS, Finch SJ, Whiteman M, Brook DW. Drug use and neurobehavioral, respiratory, and cognitive problems: precursors and mediators. J Adolesc Hlth. 2002;30:433–441. doi: 10.1016/s1054-139x(01)00395-0. [DOI] [PubMed] [Google Scholar]
- Brook JS, Richter L, Rubenstone E. Consequences of adolescent drug use on psychiatric disorders in early adulthood. Ann Med. 2000;32:401–407. doi: 10.3109/07853890008995947. [DOI] [PubMed] [Google Scholar]
- Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Meth. 2001;6:330–351. [PubMed] [Google Scholar]
- Ellickson PL, Bell RM. Drug prevention in junior high: A multisite longitudinal test. Science. 1990;247:1299–1305. doi: 10.1126/science.2180065. [DOI] [PubMed] [Google Scholar]
- Elliott DS, Knowles BA, Canter RJ. National Youth Survey Project Report No 14. Vol. 1. Boulder. CO: Behavioral Research Institute; 1981. The epidemiology of Delinquent Behavior and Drug Use among American Adolescents. [Google Scholar]
- Furstenberg FF. The sociology of adolescence and youth in the 1990s: A critical commentary. J Marr Fam. 2000;62:869–910. [Google Scholar]
- Goodman E, Amick BC, Rezendes MO, Tarlov AR, Rogers WH, Kagan J. Influences of gender and social class on adolescents’ perceptions of health. Arch Pediat Adolesc Med. 1997;151:899–904. doi: 10.1001/archpedi.1997.02170460037006. [DOI] [PubMed] [Google Scholar]
- Graham JW, Hofer SM, Donaldson SI, MacKinnon DP, Schafer JL. Analysis with missing data in prevention research. In: Bryant KJ, Windle M, West SG, editors. The Science of Prevention: Methodological Advances from Alcohol and Substance Abuse Research. 1. Washington. DC: American Psychological Association; 1997. pp. 325–366. [Google Scholar]
- Guo J, Chung IJ, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adolesc Hlth. 2002;31:354–362. doi: 10.1016/s1054-139x(02)00402-0. [DOI] [PubMed] [Google Scholar]
- Guo J, Collins LM, Hill KG, Hawkins JD. Developmental pathways to alcohol abuse and dependence in young adulthood. J Stud Alcohol . 2000;61:799–808. doi: 10.15288/jsa.2000.61.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansell S, White HR. Adolescent drug use, psychological distress, and physical symptoms. J Hlth Social Behav. 1991;32:288–301. [PubMed] [Google Scholar]
- Hansell S, White HR, Vali FM. Specific alcoholic beverages and physical and mental health among adolescents. J Stud Alcohol. 1999;60:209–218. doi: 10.15288/jsa.1999.60.209. [DOI] [PubMed] [Google Scholar]
- Hill KG, White HR, Chung IJ, Hawkins JD, Catalano RF. Early adult outcomes of adolescent binge drinking: Person- and variable-centered analyses of binge drinking trajectories. Alcsm Clin Exp Res. 2000;24:892–901. [PMC free article] [PubMed] [Google Scholar]
- Johnson PB, Boles SM, Vaughan R, Kleber HD. The co-occurrence of smoking and binge drinking in adolescence. Addict Behav. 2000;25:779–783. doi: 10.1016/s0306-4603(99)00066-0. [DOI] [PubMed] [Google Scholar]
- Johnson PB, Richter L. The relationship between smoking, drinking and adolescents’ self-perceived health and frequency of hospitalization: Analyses from the 1997 National Household Survey on Drug Abuse. J Adolesc Hlth. 2002;30:175–183. doi: 10.1016/s1054-139x(01)00317-2. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. NIH Publication No. 02-5105. Bethesda, MD: National Institute on Drug Abuse; 2002. Monitoring the Future National Survey Results on Adolescent Drug Use: Overview of Key Findings, 2001. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. [accessed November l, 2002];A SAS Procedure Based on Mixture Models for Estimating Developmental Trajectories. 2002 http://www.scat.cmu.edu/cmu-stats/tr/tr684/tr684.html.
- Kandel DB. Drug and drinking behavior among youth. Annual Rev Sociol. 1980;6:235–285. [Google Scholar]
- Kandel DB, Davies M, Karus D, Yamaguchi K. The consequences in young adulthood of adolescent drug involvement: An overview. Arch Gen Psychiat. 1986;43:746–754. doi: 10.1001/archpsyc.1986.01800080032005. [DOI] [PubMed] [Google Scholar]
- Labouvie EW, Pandina RJ, Johnson V. Developmental trajectories of substance use in adolescence: Differences and predictors. Int J Behav Devel. 1991;14:305–328. [Google Scholar]
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: John Wiley & Sons; 1987. [Google Scholar]
- Muthen BO, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach, Psychol. Meth. 1999;4:139–157. [Google Scholar]
- National Heart, Lung, and Blood Institute. The Sixth Report of the Joint National Committee on Prevention, Detection. [accessed February 5, 2002];Evaluation, and Treatment of High Blood Pressure. 1997 http://www.nhlbi.nih.gov/guidelines/hypertension/jnc6.pdf. [PubMed]
- National Heart, Lung, and Blood Institute. [accessed February 5, 2002];Behavioral Research in Cardiovascular, Lung, and Blood Health and Disease. 1998a http://www.nhlbi.nih.gov/resources/docs/taskforc.pdf.
- National Heart, Lung, and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. [accessed December 11, 2002];NIH Publication No. 98-4083. 1998b http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. [PubMed]
- National Heart, Lung, and Blood Institute. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. [accessed February 5, 2002];NIH Publication No. 00-4084. 2000 http://www.nhlbi.nih.gov/guidelines/obesity/prctgd_b.pdf.
- National Institute on Alcohol Abuse and Alcoholism. Tenth Special Report to the U.S. Congress on Alcohol and Health: Highlights from Current Research. [accessed December 5, 2002];NIH Publication No. 00-1583. 2000 http://www.niaa.nih.gov/publications/10report/intro.pdf.
- Newcomb MD, Bentler PM. The impact of late adolescent substance use on young adult health status and utilization of health services: A structural-equation model over four years. Social Sci Med. 1987;24:71–82. doi: 10.1016/0277-9536(87)90141-9. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Bentler PM. Consequences of Adolescent Drug Use: Impact on the Lives of Young Adults. Thousand Oaks, CA: Sage; 1988. [Google Scholar]
- SAS Institute. [accessed December 12, 2002];SAS/STAT Software, Version 8.2: The MI Procedure. 2002a http://www.sas.com/rnd/app/papers/miv802.pdf.
- SAS Institute. [accessed December 12, 2002];SAS/STAT Software, Version 8.2: The MIANALYZE Procedure. 2002b http://www.sas.com/rnd/app/papers/miv802.pdf.
- Schafer JL. Analysis of Incomplete Multivariate Data. 1. New York: Chapman and Hall; 1997. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Meth. 2002;7:147–177. [PubMed] [Google Scholar]
- Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J Stud Alcohol. 2002;(Supplement No 14):54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, O’Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: Trajectories of frequent binge drinking during the transition to young adulthood. J Stud Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Shanahan MJ. Pathways to adulthood in changing societies: Variability and mechanisms in life course perspective. Annual Rev Sociol. 2000;26:667–692. [Google Scholar]
- Thornberry TP, Lizotte AJ, Krohn MD, Farnworth M. Working Paper Series, No. 6. Albany, NY: Univ. at Albany Press; 1990. The Role of Delinquent Peers in the Initiation of Delinquent Behavior. [Google Scholar]
- White HR. Longitudinal stability and dimensional structure of problem drinking in adolescence. J Stud Alcohol. 1987;48:541–550. doi: 10.15288/jsa.1987.48.541. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Gomberg ES. Etiology of alcoholism reconsidered: The case for a biopsychosocial process. Amer Psychol. 1986;41:783–793. doi: 10.1037//0003-066x.41.7.783. [DOI] [PubMed] [Google Scholar]


