Abstract
Background:
Effective combat trauma management strategies depend upon an understanding of the epidemiology of death on the battlefield.
Methods:
A panel of military medical experts reviewed photographs and autopsy and treatment records for all Special Operations Forces (SOF) who died between October 2001 and November 2004 (n = 82). Fatal wounds were classified as nonsurvivable or potentially survivable. Training and equipment available at the time of injury were taken into consideration. A structured analysis was conducted to identify equipment, training, or research requirements for improved future outcomes.
Results:
Five (6%) of 82 casualties had died in an aircraft crash, and their bodies were lost at sea; autopsies had been performed on all other 77 soldiers. Nineteen deaths, including the deaths at sea were noncombat; all others were combat related. Deaths were caused by explosions (43%), gunshot wounds (28%), aircraft accidents (23%), and blunt trauma (6%). Seventy of 82 deaths (85%) were classified as nonsurvivable; 12 deaths (15%) were classified as potentially survivable. Of those with potentially survivable injuries, 16 causes of death were identified: 8 (50%) truncal hemorrhage, 3 (19%) compressible hemorrhage, 2 (13%) hemorrhage amenable to tourniquet, and 1 (6%) each from tension pneumothorax, airway obstruction, and sepsis. The population with nonsurvivable injuries was more severely injured than the population with potentially survivable injuries. Structured analysis identified improved methods of truncal hemorrhage control as a principal research requirement.
Conclusions:
The majority of deaths on the modern battlefield are nonsurvivable. Improved methods of intravenous or intracavitary, noncompressible hemostasis combined with rapid evacuation to surgery may increase survival.
Effective combat trauma management strategies depend on an understanding of the epidemiology of death on the battlefield. A review of photographs and autopsy and treatment records of 82 combat deaths classified the majority as nonsurvivable. Twelve (15%) deaths identified as potentially survivable led us to conclude that improved methods of intravenous or intracavitary, noncompressible hemostasis, and rapid evacuation may increase survival.
Analyzing combat mortality data determines new strategies for treatment, equipment, and training and focuses research agendas to meet contemporary goals and needs. In civilian systems of trauma care, analysis of deaths from injury has long been a cornerstone of trauma system development and is essential to ongoing evaluation.1,2 Equivalent studies have been conducted on several military data sets,3–5 most recently from Vietnam casualties described by the Wound Data and Munitions Effectiveness Team (WEDMET) database. WEDMET has directed military medical research, logistics, and medical tactics since that time, but it is now 40 years old. Changes in body armor, improved medical care, equipment, and training since Vietnam raise the question of the applicability of the WEDMET data in the current experience. Additionally, and perhaps more importantly, 30 years of experience in maturing trauma systems research have transformed methods of death analysis.6 The reliability of this study type has been analyzed in the past.7 In 1992, the Preventable Death Study Group determined that a multidisciplinary group, using a panel consensus rule, with autopsy reports, adequate medical records, and a standardized approach, can approximate the upper bound for potentially preventable deaths.
Tactical Combat Casualty Care (TCCC) is designed to provide all Special Operations Forces (SOF) operators (medical and nonmedical) in deploying units with sufficient medical skills to sustain casualties until evacuation and if necessary, while under fire.8,9
TCCC training emphasizes:
Tourniquets for extremity wounds with life-threatening bleeding to gain initial control of hemorrhage.
Sustained direct pressure for severe external bleeding in an anatomic location where a tourniquet cannot be applied.
Proper casualty positioning and cricothyroidotomy instead of intubation for maxillofacial trauma associated with airway trauma.
Needle decompression of tension pneumothorax.
The goal of this review was to identify which fatal injuries in the SOF between 2001 and 2004 were potentially survivable and would have been amenable to TCCC prevention and treatment modalities. The resulting data was compared with previously published data from civilian and military trauma autopsy studies. The second focus of this study was to use these findings to identify potential areas of improvement for future treatment, training, or equipment and to direct future research initiatives.
METHODS
All U.S. combatants whose remains are recovered are transported to Dover, Delaware where complete identification and forensic examination are performed by the Office of the Armed Forces Medical Examiner. This unique resource formed the basis for this report. Institutional Review Board approval for the study was provided by the U.S. Army Institute of Surgical Research and the Armed Forces Institute of Pathology.
All SOF fatalities were identified by the personnel office of the U.S Special Operations Command. These included both noncombat and combat fatalities, including those killed in action (ie, died prior to arrival at a facility with surgical capability), as well as those who died of wounds (ie, died after arrival at a facility with surgical capability).10 Treatment records and files from the Joint Theater Trauma Registry and the Office of the Armed Forces Medical Examiner were compiled. Unique identifiers were removed for this review. All autopsies had been coded independent of this study for Abbreviated Injury Score (AIS) and Injury Severity Score (ISS), the standard injury scoring systems used in trauma.7,11 The intent of this study was to identify the upper bound of potentially survivable injuries and to err on the side of inclusion. By narrowly defining too many injuries as nonsurvivable, opportunities for improvement in the delivery of medical care would have been missed.
A panel of forensic pathologists, military and civilian trauma surgeons, a trauma nurse, and a SOF combat medic was convened for this study. Prior to the initiation of the study, a panel consensus rule format12 was selected to determine whether, based on TCCC standards, an injury could be classified as potentially survivable or was nonsurvivable. All panel members were thoroughly familiarized with the standardized format prior to the initiation of the study. In the initial review, all cases were examined for mechanism of injury, ISS, age, medical examiner reports, and care received at the point of wounding. Unfortunately, the documentation of the in-hospital care, at any level, was frequently very limited. At the time of this review, there were no CT scans or plain x-rays available from the deployed setting. While CT autopsy has been described and is a very useful modality, these data were not available for this study. These findings determined which cases merited further in-depth review. Cases that required DNA identification or whose cause of death was “total body disruption” were recorded as nonsurvivable injuries and were not reviewed further.
In-depth review of the selected cases was conducted in a format similar to a morbidity and mortality conference. After action reviews, medical examiner cause of death, detailed autopsy results, including toxicology, AIS and ISS scores, photos, and x-rays, were used to determine which cases sustained potentially survivable injuries. In the analysis, patients were assumed to be within the domain of the deployed U.S. level III medical treatment facilities in theater. These level III facilities are the highest standard of medical care available in the deployed setting with advanced surgical abilities, blood bank service, radiology, and laboratory support. These facilities do not have cardiopulmonary bypass capabilities and neurosurgical support is limited.
The classic terminology encountered in the civilian literature when conducting a similar analysis is “preventable death,” “potentially preventable death,” and “nonpreventable death.” However, delivery of care on the battlefield is dictated as much by the tactical situation as by traditional medical necessity. While a casualty may sustain an injury that is considered treatable and from which the soldier should not have died, if this same injury occurs during a fire fight that prohibits a medic or soldier from reaching the casualty, then to categorize the death as “preventable” is erroneous. The term “preventable” implies that something could have or should have been done to alter the final outcome of the patient. Therefore, the panel decided that terminology that describes the injury sustained would better achieve the goals of this study and selected the terms “potentially survivable” and “nonsurvivable.” No separate distinction of “definitely survivable” or “potentially survivable” was made. A completed questionnaire for each casualty summarized a consensus of the panel’s findings and identified changes in training, treatment, or equipment that could have influenced the outcome of the casualty. These findings were then reviewed to identify possible areas for future research.
RESULTS
Between October 2001 and November 2004, there were 82 SOF fatalities: 35 (42%) from explosions, 23 (28%) gunshot wounds, 19 (23%) aircraft crashes, 4 (5%) motor vehicle crashes, and 1 (2%) fall (Table 1). Autopsies were performed for all except 5 SOF soldiers who died in an airplane crash and whose bodies were lost at sea. These 5 deaths were included in the count of clearly nonsurvivable injuries (n = 70). Twenty-four of the 82 cases were selected for detailed review by the panel. Eighty-five percent (n = 70) of the fatal injuries were considered nonsurvivable (ISS = 58 ± 35), while 15% (n = 12) were regarded as potentially survivable (ISS = 35 ± 9, P < 0.05). The 16 mechanisms ofinjury in these 12 deaths are shown in Table 1. Four (33%) of the potentially survivable injured were identified as died of wounds, of which 1 death occurred 56 days after injury in a medical center in the United States. The 3 other casualties all died within 24 hours of hospital admission from exsanguination: 2 from noncompressible truncal hemorrhage and 1 from cervical hemorrhage, potentially amenable to direct compression. The remaining 8 (66%) potentially survivable injured were identified as killed in action and died on the battlefield.
TABLE 1. Mechanisms of Injury: 82 SOF Deaths Versus All Combat Injuries
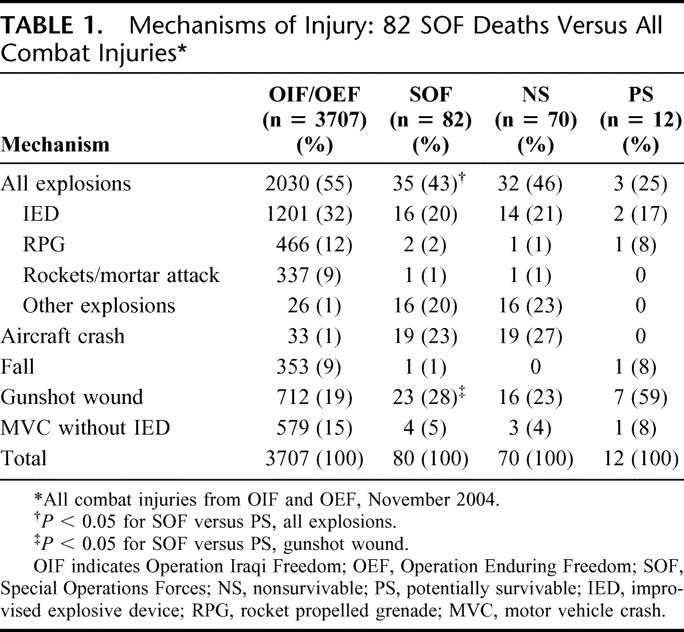
Cause of SOF deaths differed somewhat from what has been observed in conventional military personnel throughout Operation Iraqi Freedom and Operation Enduring Freedom.13 The SOF fatalities had a higher incidence of death secondary to gunshot wounds (28% vs. 19%; P < 0.05) and a lower incidence of death secondary to explosions (55% vs. 43%; P < 0.05; logit case control odds ratio, 95% confidence interval of 1.42–4.03).
Among nonsurvivable injuries, there were 40 AIS 6 injuries in 31 patients (P = 0.001), and 104 AIS 5 injuries in 53 patients (Table 2). Among the 12 potentially survivable injuries, there were only 8 AIS 5 injuries and 18 AIS 4 injuries. The distribution of ISS is shown in Figure 1. Figure 2 shows the distribution of ISS by quartiles. Nearly one half of the nonsurvivable casualties had an ISS of 60 to 75. Using Fisher exact test, a significantly greater percentage of potentially survivable casualties were in the ISS 20 to 40 quartile (P < 0.03).
TABLE 2. Abbreviated Injury Score (AIS) Distribution
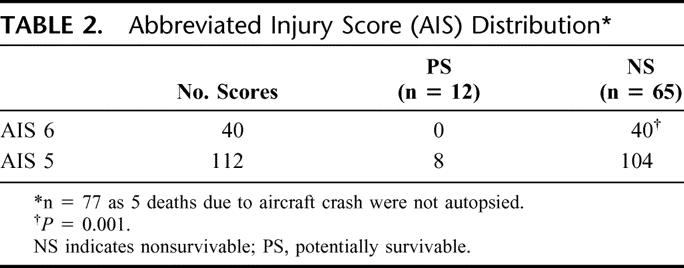
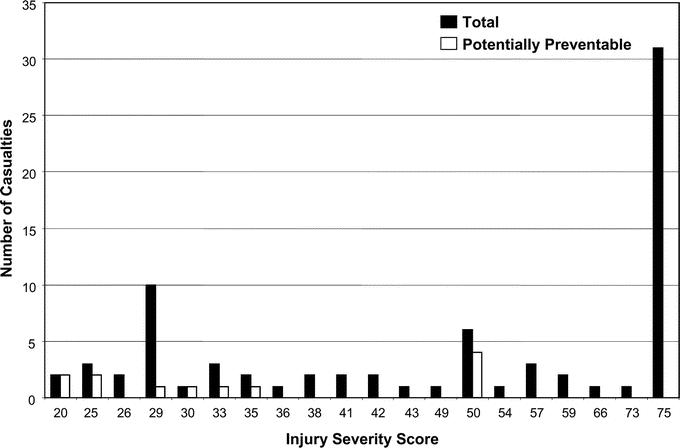
FIGURE 1. Injury Severity Score (ISS) ranges for Special Operations deaths in Operation Iraqi Freedom and Operation Enduring Freedom.
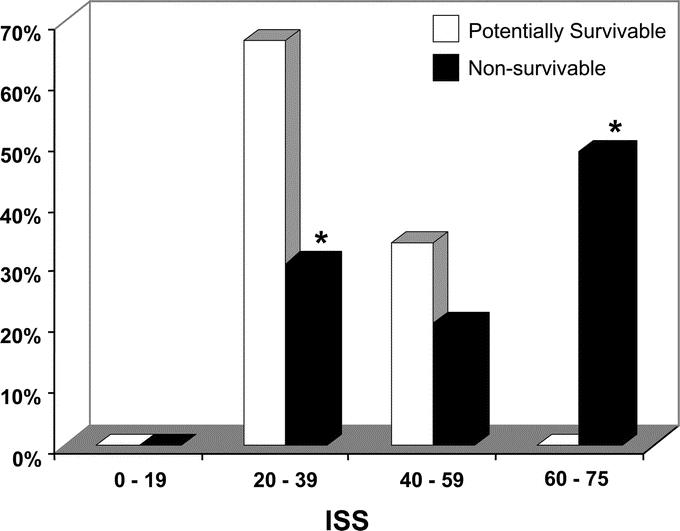
FIGURE 2. Injury Severity Scores (ISS) for potentially survivable casualties compared with nonsurvivable casualties. *P < 0.03 (Fisher exact test).
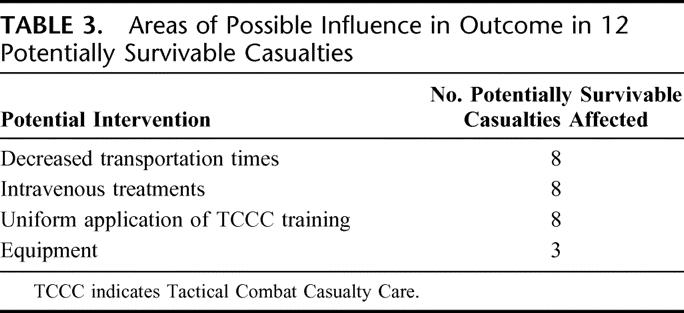
The most common potentially survivable injuries were noncompressible (truncal) hemorrhage (8), followed by hemorrhage amenable to tourniquet (3), hemorrhage not amenable to tourniquet yet compressible (2), obstructed airway (1), tension pneumothorax (1), and sepsis (1) (Fig. 3). Panel members identified 4 main areas, treatment, training, equipment, or transport, which may have altered outcomes for these 12 patients (Table 3). Some injuries fell within more than one area. Potential treatment included methods for hemostasis, including hemorrhage control with tourniquet (3) and pressure with hemostatic dressings (2). Other potential treatment included adequate airway (1) and needle thoracostomy (1). These interventions are taught to all SOF combat medics and are covered in chapter 17 on TCCC in the Pre-Hospital Trauma Life Support Manual.14 More expeditious casualty evacuation to a facility capable of surgical intervention may have improved patient outcome in 8 casualties. In 3 casualties, improved equipment that has since become available, the Combat Application Tourniquet (1) and the HemCon hemostatic dressing (2) may have altered outcome.
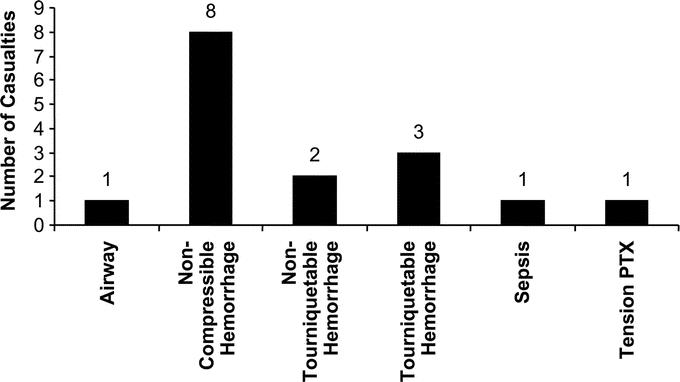
FIGURE 3. Sixteen potential causes of death in the 12 potentially survivable casualties.
TABLE 3. Areas of Possible Influence in Outcome in 12 Potentially Survivable Casualties
Whether or not these soldiers were wearing body armor at the time of injury was not recorded at any time prior to our evaluation. However, knowing the capabilities of armor systems and the mechanism of injury, the assumption was made that the potentially survivable injuries in 3 casualties may have been avoided had they worn their body armor. Of the 82 SOF deaths, only 1 soldier sustained a potentially survivable wound to the chest in an area that is not covered by body armor.
Consensus was reached on 23 of the 24 (96%) reviewed cases. The 1 case for which no consensus was reached was a casualty who on autopsy, in addition to multiple sites of internal injury and rib fractures, was found to have a large tension pneumothorax (Fig. 4). It was unclear whether the tension pneumothorax was postmortem artifact or a clinically relevant finding. Given the stated goals of this study, this death was considered by some to be a clinically relevant finding and the result of potentially survivable injuries.
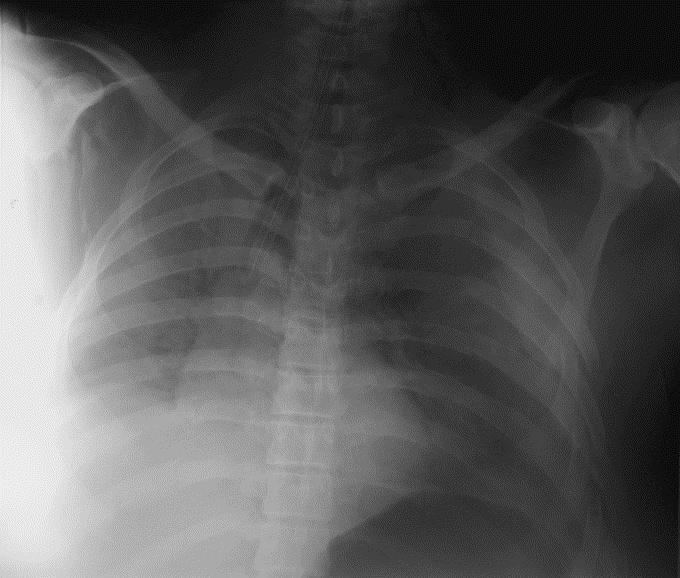
FIGURE 4. Chest x-ray of tension pneumothorax after fall from helicopter. This casualty also had other significant internal injuries and died 4.5 hours after injury.
DISCUSSION
Nothing in this review is meant to detract from the accomplishments of combat medics. The small number of fatal outcomes associated with TCCC training suggests that in most cases injuries were treated appropriately by SOF combat medics. In some instances, a medic may not have been present when the injuries occurred. At other times, the unit medic may have been killed or incapacitated. Critical review of deaths due to trauma is a cornerstone of the evolution of trauma care systems. This type of analysis defines the direction of future research and identifies areas in need of improvement, not only in the deployed medical care system, but in the civilian medical sector as well.
Some familiarity with the trauma care system analyzed in this paper is central to understanding the limitations of this study. SOF units are often deployed in small teams and in hostile environments. Extraction of wounded combatants may be difficult and delayed, placing a significant burden on care providers at the point of wounding. In the current study, injury, evacuation, and arrival times at a surgical facility are largely unknown. To prevent early deaths, SOF medics must be highly trained and expertly equipped and supported. This is in direct contrast to the “scoop and run” paradigm of most civilian emergency medical (EMS) systems. Civilian EMS systems in rural areas do, however, experience many of the same challenges experienced by SOF medics. These include long transportation times during which the paramedic must be able to manage obstructed airway, chest trauma, and hemorrhage.15 The long transportation times and delay from point of injury to a facility where definitive care can be provided place similar burdens on the paramedic to prevent early death. The lessons learned from this study are therefore applicable to EMS care. This is especially true for those casualties suffering truncal or noncompressible hemorrhage. Currently, there is no active intervention available to medics, who must be trained to practice hypotensive resuscitation to avoid over-resuscitation and increased hemorrhage.14,16 In any event, this analysis was significantly limited by incomplete data from the prehospital and hospital setting. The time between wounding and casualty evacuation and the time interval between wounding and arrival at a medical treatment facility or death was known only in a few of the cases. Also unknown in some cases were the specifics of care rendered on the scene and during evacuation, as well as whether or not body armor and helmets were worn by casualties.
Consistent with findings from previous conflicts,3 85% of the fatalities were from injuries that were not survivable. After analysis, and as evidenced by the distribution of the AIS and ISS scores (Figs. 1, 2), 70 fatalities were judged to have been wounded so severely that survival would have been impossible even within the immediate reach of civilian level 1 trauma care. The distribution of the ISS and AIS scores supports the claims of this study that the casualties with wounds considered to be potentially survivable were not injured to the same degree as their counterparts with injuries considered to be nonsurvivable. Only 12 (15%) of the deaths were categorized as potentially survivable.
A probability of survival score was not calculated for these patients as the utilization of the ISS as a predictive tool for outcomes in combat trauma has significant limitations. The ISS is obtained by summing the square value of the 3 highest AIS scores in up to 3 separate body regions. For example, a soldier wounded by an improvised explosive device may have an AIS 5 for an abdominal injury, AIS 4 for a chest injury and an AIS 3 for an extremity injury. The ISS would then be 50, representing a severe injury. The limitation here is that the ISS does not account for multiple injuries to the same body region. In our example, this same soldier may have had more than one AIS 5 injury or an AIS 4 injury to his abdomen in addition to multiple AIS 4 injuries in his chest, or bilateral AIS 3 extremity injuries; such wounding patterns are frequently observed in casualties from improvised explosive device explosions. The conventional ISS scoring system does not account for these highly significant injuries. In our population of deaths from potentially survivable injuries, 4 patients with AIS 5 injuries had AIS 4 injuries in the same body region, but these significant injuries remain unaccounted for in the calculation of the ISS for these casualties. A new military ISS system that will account for the differences between combat and civilian injuries is under development.
Comparing the percentage of potentially survivable injuries in this study with previously published reports15,17,18 of civilian trauma care in the United States is a testament to the training, skills, and battlefield successes of SOF combat medics. Those papers report 8% to 22% of prehospital deaths as preventable or potentially preventable. The 15% rate of this study falls within this range, despite more severe injuries, hostile environment, and the intent of this study to identify the upper bound of potentially survivable injuries. Taking the shortcomings of the ISS for combat casualties into consideration, the reported mean ISS of the potentially preventable deaths in one study was 25,17 while in our population deaths from potentially survivable injuries had a mean ISS of 35. The mean ISS of the 73 nonpreventable deaths from the same study was 52; ours was 56. But again, comparisons are difficult as the majority of patients reviewed in the civilian literature suffered blunt trauma from motor vehicle accidents, whereas in our study 71% of all deaths were the result of devastating penetrating trauma and only 2 potentially survivable deaths resulted from blunt trauma.
A study of 210 combat fatalities from Vietnam reported cases that were independently reviewed by 4 trauma surgeons and assessed as either “definitely preventable,” “possibly preventable,” “not salvageable,” or “cannot determine.”4 That study was done utilizing medical records; tactical information and autopsy data were unavailable. Among 210 cases, 5.4% (range 1.0%–11%) were noted as definitely preventable and 34.9% (range, 26.2%–41.9%) as possibly preventable. Although the percentage of fatalities with potentially survivable wounds in our study was lower, the results are difficult to compare with this study as the methodology was different.
Three cases were identified in which the casualty had hemorrhaged from a site that was amenable to placement of a tourniquet. Two of these 3 had no tourniquet placed and 1 was a case of tourniquet failure. Lack of tourniquet use and tourniquet failure has been thoroughly investigated, followed by a major initiative to field the Combat Application Tourniquet tourniquet.19,20 This device was tested by U.S. Army Special Operations Command operators, and trauma surgeons and found to be superior in function and feasibility to the traditional “cravat and stick” used in the period of this study.
Theoretically, all of the potentially survivable injured would have benefited from more expeditious evacuation to a medical treatment facility. However, tactical environment and availability of resources, beyond the control of the healthcare provider on the ground, govern evacuation. With this in mind, this study focused on identifying the measures that can be taken to sustain a casualty until evacuation is possible. It is during this time that interventions aimed at achieving hemostasis or mitigating hemorrhage must be used.
The 8 deaths from noncompressible hemorrhage demonstrate the importance of injectable hemostasis for all levels of care, but especially for medics during prehospital care. Currently, recombinant factor VIIa (rFVIIa) holds the most immediate promise, although the efficacy of this drug as a sole prehospital hemostatic adjunct is unknown. Fortunately, however, the safety and efficacy of rFVIIa in trauma patients have been established, making the prospect of prehospital noncompressible hemostasis tantalizingly close.21–23 Possibly, the combination of rFVIIa with other clotting factor concentrates will provide both the substrate and the thrombin burst required to accelerate clotting.24,25 Another potential intervention, hemoglobin-based oxygen carriers (HBOC), has just recently completed a phase III trials for prehospital administration. HBOC replaces the oxygen carrying capacity of shed blood allowing delivery of oxygen to vital organs during critical anemia.26 If current trials support this indication, HBOC may be added to the SOF armamentarium to maintain oxygen delivery before evacuation. Whatever interventions are settled on, stabilization sufficient to deliver the injured to medical treatment facilities for surgical intervention will improve outcomes. “Damage Control Resuscitation” which incorporates the use of a pro-hemostatic adjunct, such as rFVIIa and plasma, with hypotensive resuscitation and HBOCs may allow SOF casualty to tolerate the longer evacuation times observed in this population.27–29
This unique study identified areas in which medical care delivered in the field can be improved and assists in the allocation of resources for research and development. Broadly, these areas include combat casualty care training for nonmedical combatants, air evacuation and close air support resources, operational medical planning, improvements in postoperative care, and new medical interventions.
Specific findings that will enable the military to continue to improve battlefield trauma care are:
A total of 85% of SOF fatalities resulted from injuries that were judged to be nonsurvivable.
Consistent application of the currently taught TCCC guidelines might have improved outcomes for 8 of the 12 fatalities with potentially survivable injuries.
Damage Control Resuscitation represents the most promising modality at present to improve outcomes in the 8 fatalities with noncompressible hemorrhage.
Inadequate anatomic coverage of the currently fielded SOF body armor was not documented in this study.
Improved methods to capture records of prehospital care rendered on the battlefield will greatly improve future efforts to perform similar studies.
These 82 deaths must be considered in the context of the over 500 SOF casualties who survived their injuries, sustained by SOF during the period encompassed by this study. That most of the SOF casualties from these 2 conflicts survived is a great credit to the courage and professionalism of the physicians, nurses, medical planners, pilots, aircrew, combat medics, and teammates who cared for our wounded warriors. Improvements in combat casualty care stem from the unfortunate repeated experience of war.30 This analysis is a focused effort to learn lessons that will help us save casualties in battles yet to be fought.
Footnotes
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Department of Defense or United States Government. The authors are employees of the U.S. government. This work was prepared as part of their official duties and, as such, there is no copyright to be transferred. These data were approved for public release by the U.S Special Operations Command Public Affairs Office on April 25, 2006.
Reprints: COL John B. Holcomb, MD, U.S. Army Institute of Surgical Research, 3400 Rawley E. Chambers Avenue, Fort Sam Houston, TX 78234. E-mail: John.Holcomb@amedd.army.mil.
REFERENCES
- 1.Cales RH, Trunkey DD. Preventable trauma deaths: a review of trauma care systems development. JAMA. 1985;254:1059–1063. [DOI] [PubMed] [Google Scholar]
- 2.Dubois RW, Brook RH. Preventable deaths: who, how often, and why? Ann Intern Med. 1988;109:582–589. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy RF, Maningas PA, Vayer JS. Epidemiology of trauma: military experience. Ann Emerg Med. 1986;15:1384–1388. [DOI] [PubMed] [Google Scholar]
- 4.Blood CG, Puyana JC, Pitlyk PJ, et al. An assessment of the potential for reducing future combat deaths through medical technologies and training. J Trauma. 2002;53:1160–1165. [DOI] [PubMed] [Google Scholar]
- 5.Carey ME. Analysis of wounds incurred by U.S. Army Seventh Corps personnel treated in Corps hospitals during Operation Desert Storm, February 20 to March 10, 1991. J Trauma. 1996;40(suppl 3):165–169. [DOI] [PubMed] [Google Scholar]
- 6.Hoyt DB, Coimbra R, Potenza B, et al. A twelve-year analysis of disease and provider complications on an organized level I trauma service: as good as it gets? J Trauma. 2003;54:26–36; discussion 37. [DOI] [PubMed]
- 7.MacKenzie EJ, Shapiro S, Eastham JN. The Abbreviated Injury Scale and Injury Severity Score: levels of inter- and intrarater reliability. Med Care. 1985;23:823–835. [DOI] [PubMed] [Google Scholar]
- 8.Butler FK Jr. Tactical medicine training for SEAL mission commanders. Mil Med. 2001;166:625–631. [PubMed] [Google Scholar]
- 9.Butler FK Jr, Holcomb JB. The tactical combat casualty care transition initiative. Army Med Dept J. 2005;Apr/May/June:33–37.
- 10.Holcomb JB, Stansbury LG, Champion HR, et al. Understanding combat casualty care statistics. J Trauma. 2006;60:397–401. [DOI] [PubMed] [Google Scholar]
- 11.Baker SP, O’Neill B, Haddon W Jr, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 12.MacKenzie EJ, Steinwachs DM, Bone LR, et al. Inter-rater reliability of preventable death judgments: the Preventable Death Study Group. J Trauma. 1992;33:292–302; discussion 303. [DOI] [PubMed]
- 13.Department of Defense. DOD Personnel & Procurement Statistics, 2005. Washington, DC: Department of Defense, 2005. [Google Scholar]
- 14.Salomone JP, Pons PT, eds. PHTLS Basic and Advanced Prehospital Trauma Life Support: Military Edition, 6th ed. St. Louis: Mosby, 2006. [Google Scholar]
- 15.Esposito TJ, Sanddal ND, Hansen JD, et al. Analysis of preventable trauma deaths and inappropriate trauma care in a rural state. J Trauma. 1995;39:955–962. [DOI] [PubMed] [Google Scholar]
- 16.Holcomb JB. Fluid resuscitation in modern combat casualty care: lessons learned from Somalia. J Trauma. 2003;54(suppl 5):46–51. [DOI] [PubMed] [Google Scholar]
- 17.Maio RF, Burney RE, Gregor MA, et al. A study of preventable trauma mortality in rural Michigan. J Trauma. 1996;41:83–90. [DOI] [PubMed] [Google Scholar]
- 18.Esposito TJ, Sanddal TL, Reynolds SA, et al. Effect of a voluntary trauma system on preventable death and inappropriate care in a rural state. J Trauma. 2003;54:663–669; discussion 669–670. [DOI] [PubMed]
- 19.Walters TJ, Wenke JC, Kauvar DS, et al. Effectiveness of self-applied tourniquets in human volunteers. Prehosp Emerg Care. 2005;9:416–422. [DOI] [PubMed] [Google Scholar]
- 20.Wenke JC, Walters TJ, Greydanus DJ, et al. Physiological evaluation of the U.S. Army one-handed tourniquet. Mil Med. 2005;170:776–781. [DOI] [PubMed] [Google Scholar]
- 21.Boffard KD, Riou B, Warren B, et al. Recombinant factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients: two parallel randomized, placebo-controlled, double-blind clinical trials. J Trauma. 2005;59:8–15; discussion 18. [DOI] [PubMed]
- 22.Lynn M, Jerokhimov I, Jewelewicz D, et al. Early use of recombinant factor VIIa improves mean arterial pressure and may potentially decrease mortality in experimental hemorrhagic shock: a pilot study. J Trauma. 2002;52:703–707. [DOI] [PubMed] [Google Scholar]
- 23.McMullin NR, Kauvar DS, Currier HM, et al. The clinical and laboratory response to recombinant factor VIIa in trauma and surgical patients with acquired coagulopathy. Curr Surg. 2006;63:246–251. [DOI] [PubMed] [Google Scholar]
- 24.Hedner U. Dosing with recombinant factor VIIa based on current evidence. Semin Hematol. 2004;41(suppl 1):35–39. [DOI] [PubMed] [Google Scholar]
- 25.Wolberg AS, Allen GA, Monroe DM, et al. High dose factor VIIa improves clot structure and stability in a model of haemophilia B. Br J Haematol. 2005;131:645–655. [DOI] [PubMed] [Google Scholar]
- 26.Moore EE, Johnson JL, Cheng AM, et al. Insights from studies of blood substitutes in trauma. Shock. 2005;24:197–205. [DOI] [PubMed] [Google Scholar]
- 27.Hess JR, Holcomb JB, Hoyt DB. Damage control resuscitation: the need for specific blood products to treat the coagulopathy of trauma. Transfusion. 2006;46:685–686. [DOI] [PubMed] [Google Scholar]
- 28.Holcomb JB, Jenkins D, Rhee P, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62:307–310. [DOI] [PubMed] [Google Scholar]
- 29.McMullin NR, Holcomb JB, Sondeen JL. Hemostatic resuscitation. In: Yearbook of Intensive Care and Emergency Medicine. Berlin: Springer-Verlag, 2006:265–278. [Google Scholar]
- 30.Eastridge BJ, Jenkins D, Flaherty S, et al. Trauma system development in a theater of war: experiences from Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma. 2006;61:1366–1372; discussion 1372–1373. [DOI] [PubMed]


