Abstract
Objective:
The aim of this study was to compare the morbidity of fixation of prosthetic meshes using Tissucol fibrin glue versus staples in laparoscopic transabdominal preperitoneal (TAPP) repair of inguinal and femoral hernias.
Summary Background Data:
In patients undergoing laparoscopic hernia repair, fixation of mesh prostheses with staples may affect inguinocrural nerves causing early postoperative neuralgia and chronic neuralgia.
Methods:
Between June 2003 and February 2005, 197 patients with inguinal or femoral hernia were enrolled in this prospective, randomized study, to assess morbidity following hernia repair with staples (n = 98) or Tissucol (n = 99). The primary outcomes were early postoperative and late neuralgia recorded using a visual analog scale (VAS). The effects of neuralgia on functional status were evaluated using the modified SF-36 questionnaire. Secondary outcomes included complications such as nonspecific pain and recurrence.
Results:
Assessments took place at 1, 3, 6, and 12 months, with all patients completing each follow-up visit. Mean VAS scores were significantly lower in the Tissucol group versus the staples group (MANOVA, P < 0.05). Higher scores for the modified SF-36 questionnaire at 1 month were demonstrated in the Tissucol group compared with the staples group (23.2 and 22.6, respectively; P < 0.05). The mean recovery time for normal physical activity was significantly shorter in the Tissucol group compared with the staples group (7.9 vs. 9.1 day, respectively; P < 0.001). One recurrence was seen in the fibrin glue group, which was attributable to a technical error in fixation of the mesh.
Conclusions:
The use of Tissucol provides distinct advantages in laparoscopic treatment of inguinal/femoral hernias compared with conventional TAPP, including a lower incidence of postoperative neuralgia and an earlier resumption of physical and social activities.
A total of 197 patients with inguinal or femoral hernias were randomly assigned to laparoscopic hernioplasty with either staples (n = 98) or fibrin glue (n = 99) used to fix the prosthesis. The primary outcome measure was occurrence of neuralgia. The fibrin glue group showed a significantly lower mean pain score (P < 0.05) and significantly shorter recovery time (7.9 vs. 9.1 days, P < 0.001) with respect to the staples group.
Surgery of the inguinal canal has improved in recent years, with various techniques introduced to reduce the incidence of recurrence and other complications. The development of minimally invasive procedures in the early 1990s, such as laparoscopic techniques, enabled new methods of hernia repair to be explored. Currently, the 2 most widely adopted laparoscopic procedures are totally extraperitoneal and transabdominal preperitoneal (TAPP).
The laparoscopic approach allows a reduction in the length of hospital stay and in the degree of postoperative impairment experienced by patients on their social life. The potential complications related to fixation of mesh prostheses using staples (especially postoperative neuralgia) prompted us to explore the use of human fibrin glue (Tissucol/Tisseel, Baxter Healthcare, Deerfield, IL) for mesh fixation. The aim of this study was to compare the morbidity associated with fixation of prosthetic meshes using Tissucol fibrin glue versus staples in laparoscopic TAPP repair of inguinal and femoral hernias.
METHODS
Patients presenting at the General Surgery Unit at Sesto San Giovanni Hospital who were 18 years of age or older, with a diagnosis of inguinal or femoral hernia, were eligible for random assignment to laparoscopic tension-free repair with mesh fixation by Endopath Multifeed Stapler 10 mm shaft (EMS, Ethicon Endo-Surgery, Inc., Cincinnati, OH) with titanium staples or fibrin glue (Tissucol/Tisseel, Baxter Healthcare). Patients gave written informed consent before inclusion into the study.
Patients in American Society of Anesthesiologists (ASA) class IV (ie, those who had life-threatening systemic disease) or class V (ie, those who were unlikely to survive for 24 hours, with or without an operation) were excluded. Further exclusion criteria were contraindications to general anesthesia, bowel obstruction, bowel strangulation, peritonitis, bowel perforation, local or systemic infection, contraindications to pelvic laparoscopy, a history of hernia repair with mesh, a history of open prostatectomy, or a life expectancy of less than 2 years. Patients affected by spondyloarthrosis with involvement of the dorsal lumbar nervous radices or by lumbar somatic discus hernia, with or without surgical correction, and patients with diabetic polyneuropathy were excluded from the trial. Patients who were participating in another trial were also excluded.
Randomization was carried out using randomization tables. In patients with bilateral hernias, both sides were repaired simultaneously; one side was chosen randomly to be the “study hernia” to be included in the intention-to-treat analysis. Patients were not aware of their treatment group prior to surgery. During the consent process prior to the trial, patients were not informed of our hypothesis that fibrin glue fixation results in less postoperative pain and neuralgia than fixation with staples. The protocol was approved by the Ethical and Scientific Board of the Sesto San Giovanni Hospital.
Laparoscopic repairs were performed by a TAPP approach. All repairs involved the use of polypropylene mesh, and all patients underwent standardized repairs by surgeons with extensive experience in TAPP hernia repair. All participating surgeons (n = 4) were trained at the same surgery unit under the supervision of the leading skilled surgeon (no. 1), who also trained the surgeons in TAPP hernia repair with Tissucol. The first experience of tension-free TAPP was performed in January 2003, and each member of the surgical team had carried out more than 50 TAPP procedures with Tissucol before beginning the trial.
All the patients were given standardized postoperative instructions that did not restrict their activities unless the activities caused pain.
Surgical Technique
A Veress needle was used to induce pneumoperitoneum at an umbilical site and then was replaced by one 10- to 12-mm optical trocar. A 5-mm trocar was positioned unilaterally on the umbilical line and a 10-mm trocar was positioned in the iliac fossa contralateral to the hernia. In the presence of a bilateral hernia, both umbilical trocars were positioned bilaterally in the iliac fossa. An incision of the wall of the peritoneum was made starting at the level of the superior margin of the internal inguinal ring at the level of the epigastric vessels. It was extended medially up to the residue of the umbilical artery and laterally for 3 to 4 cm past the inguinal ring for a total length of 7 to 8 cm.
In the presence of direct hernias, the hernial sac was directly isolated and reduced. In the case of indirect or femoral hernias, the preperitoneal parapubic adipose tissue was carefully dissected medially to expose the horizontal pubic ramus and Cooper's ligament. Accurate dissection of the preperitoneal retrovesical tissue permits easier positioning of the mesh. The internal inguinal ring was then explored, isolating and reducing the hernial sac; this maneuver was performed to reveal the presence of perihernial lipomas, which could then be removed.
Once the spermatic cord had been freed from the peritoneal wall, the prosthesis was positioned. A monofilament polypropylene mesh with large pores was used (Bard Visilex mesh, C.R. Bard Inc.). This type of mesh allows the surgeon to view the underlying structures, thereby facilitating positioning of the prosthesis. The mesh was cut to a dimension of 10 × 13 cm and placed in the preperitoneal space such that it was in medial contact with the paravesical area, covering Cooper's ligament, resting on the inguinal region, and extending laterally over the epigastric vessels.
In the case of the use of staples (traditional TAPP), an Endopath Multifeed Stapler 10 mm shaft (EMS, Ethicon Endo-Surgery, Inc.) with titanium staples was used. The mesh was cut with a slit for the cord structures. The technique that we adopted involved positioning 3 metal clips at the level of Cooper's ligament and the pubic tubercle. Some fixations were carried out laterally at the level of the deep inguinal ring. The inferior branch of the mesh was passed beneath the spermatic cord to reconstruct the internal inguinal ring and was successively anchored to the superior branch with metal clips.
In patients undergoing Tissucol fixation (tension-free TAPP), the tails of the mesh were wrapped around the spermatic cord and the mesh was anchored with 1 mL of fibrin glue (Tissucol/Tisseel, Baxter Healthcare), applied both anterior and posterior to the mesh using a dedicated laparoscopic tool (Duplotip, Baxter Healthcare, Milan, Italy) inserted in a 5- or 10-mm trocar. To obtain optimal binding between the mesh, the peritoneal wall, and Tissucol, slight pressure was applied to the mesh using the Duplotip. The Tissucol was applied to the entire perimeter of the mesh and in particular at the level of the superior margin, the “triangle of disaster,” and in proximity of the prevesical fat to assure good adhesion. The peritoneal flaps were then closed using small, continuous, resorbable 2/0 sutures.
In patients with bilateral hernias, the same procedures were performed sequentially to repair the hernia on the other side (generally smaller).
Primary Outcome
The primary outcome of the trial was early and late postoperative neuralgia, defined by the presence of intermittent hyperesthesia, burning sensation and/or jabbing pain in the ipsilateral inguinal area nerves (genitofemoral nerve, lateral cutaneous femoral nerve, ilioinguinal and iliohypogastric nerve). Postoperatively, patients were examined at 1, 3, 6, and 12 months to determine the presence or absence of postoperative neuralgia using a 0- to 100-mm visual analog scale (VAS) by a surgeon who was not informed about each patient's treatment group and who had not been involved in the patient's operation.
Functional status was assessed with the medical outcomes Study 36-item Short-form General Survey (SF-36) questionnaire, version 2, modified (Fig. 1). For each patient, the replies to the questionnaire were used to obtain a final score representing the functional status of the patient (maximum score, 27; minimum score, 0). Before surgery, all patients completed a short form of the questionnaire that did not include item 2, which specifically refers to the surgical event. The survey was completed by the patient during the follow-up examination in the presence of the surgeon.

FIGURE 1. 36-item Short-form General Survey (SF-36) questionnaire, version 2, modified.
Secondary Outcomes
Secondary outcomes were complications such as early and late nonspecific postoperative pain, recurrence, and death. Early, nonspecific postoperative pain was assessed in areas other than those innervated by the inguinal nerves, and was strictly related to the abdominal distension due to the pneumoperitoneum and to surgical wound, characterized by pain localized at the incision sites. Late nonspecific pain described abdominal discomfort whose origin was not correlated to entrapment or injury of the inguinal area nerves. Complications were assessed intraoperatively and at specified intervals postoperatively. Long-term complications were assessed at the 1-, 3-, 6-, and 12-month visits. Life-threatening complications were defined before the start of the study and were assessed for 30 days after the procedure. Recurrences were confirmed by examination by a surgeon not involved in the trial, by ultrasound examination, or during a second intervention. Patients with bilateral hernias who had a recurrence on the side contralateral to the study hernia were considered not to have had a recurrence in the intention-to-treat analysis. All deaths and life-threatening complications were reviewed by an independent Endpoints Committee to determine whether the event was treatment related.
Statistics
The study was designed to detect a 20-mm difference in mean subjective pain scale scores between the groups with a sample of 200 patients, a power of 80% and alpha error of 5%. This was based on recent literature reports that a 9- to 13-mm difference is the clinically significant difference in patient-assigned visual analog scores.1,2 As 197 patients underwent surgery, this study had more than 90% power to distinguish a difference of 13 mm in mean subjective pain scale scores, allowing a two-sided type I error rate of 5%. The data from the postoperative pain and disability evaluation (SF-36 modified) were subjected to a multivariate analysis with the application of MANOVA test for repeated measures. Comparisons between the nominal variations were expressed as odds ratios. Continuous parametric variables were analyzed by MANOVA, and noncontinuous parametric variables were analyzed using the Mann-Whitney U test.
RESULTS
Patient Characteristics
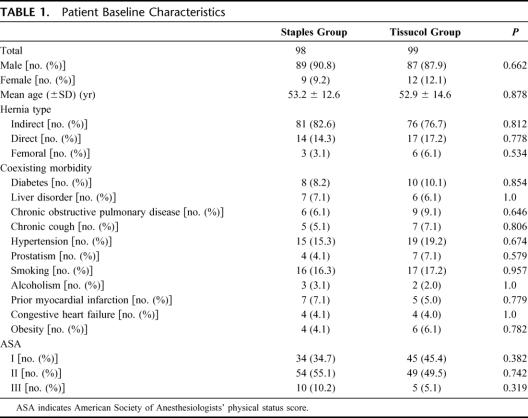
Our study included 176 male (89.3%) and 21 female (10.7%) patients with a mean age of 53 years (range, 18–79 years); 188 (95.4%) hernias were inguinal and 9 (4.6%) were femoral. Patient characteristics were similar in the 2 treatment groups (Table 1). All 197 patients completed follow-up visits at 1, 3, 6, and 12 months. No intraoperative complications were observed in either of the treatment groups. There were no significant differences in preoperative quality of life scores between the 2 groups.
TABLE 1. Patient Baseline Characteristics
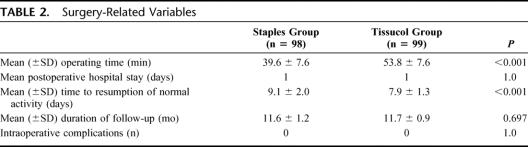
The mean duration of intervention was 54 minutes (range, 30–95 minutes) in the Tissucol group versus 40 minutes (range, 25–105 minutes) in the staples group (P < 0.001). The mean postoperative hospitalization time in each group was 1 day. The mean recovery time to normal physical activity was 7.9 days (range, 5–11 days) in the Tissucol group versus 9.1 days (range, 7–11 days) in the staples group (P < 0.001) (Table 2).
TABLE 2. Surgery-Related Variables
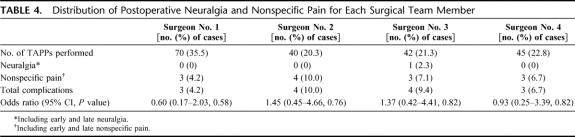
The number of TAPP procedures performed by each surgeon is reported in Figure 2. The leading surgeon who defined and standardized the TAPP technique is indexed as no. 1 and the other surgeons are referred to as nos. 2, 3, and 4.
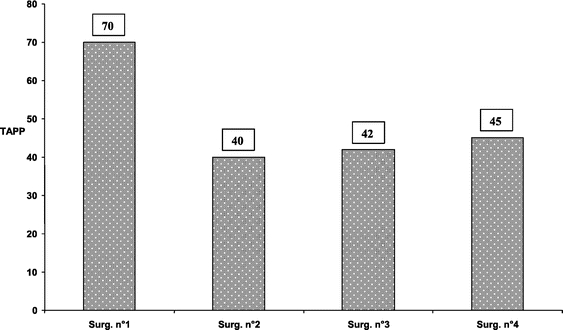
FIGURE 2. Number of TAPP procedures performed by each surgeon of the surgical team.
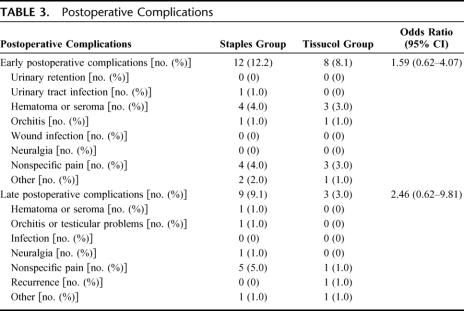
Postoperative Complications
Early postoperative complications occurred in 8% of patients in the Tissucol group and in 12% of patients in the staples group. Late postoperative complications occurred in 3% and 7% of patients in the Tissucol and staples groups, respectively. Relevant data are summarized in Table 3.
TABLE 3. Postoperative Complications
Only 1 patient in the Tissucol group reported chronic inguinal discomfort following intense and prolonged physical activity, for which analgesics were rarely taken. There were no cases of hernia recurrence in the staples group and 1 case in the Tissucol group, noted at 1 month follow-up and confirmed by echography.
Postoperative Neuralgia and Functional Status
In the staples group, there was 1 case of postoperative neuralgia (a VAS of 8 at 1 month postoperatively), which did not respond to treatment with nonsteroidal antiinflammatory drugs. This case was a recurrent inguinal hernia and required repeat laparoscopy to remove the clips; the mesh was fixed with Tissucol without any sequelae.
After 6 months, 5 patients in the staples group reported inguinal discomfort and required nonsteroidal antiinflammatory drugs (ketorolac, mean dosage: 120 ± 34 mg/weekly for patient) during physical activity; whereas in the Tissucol group, no cases of postoperative neuralgia were reported (P = not significant).
The distribution of cases of postoperative neuralgia for each surgical team member is shown in Table 4.
TABLE 4. Distribution of Postoperative Neuralgia and Nonspecific Pain for Each Surgical Team Member
At 1 month after surgery, the mean VAS score was significantly lower in the Tissucol group compared with the staples group (19 mm vs. 26 mm, respectively; P < 0.05). This difference was highly significant at 3 months (11 mm vs. 23 mm, respectively; P < 0.001) and 6 months (11 mm vs. 20 mm, respectively; P < 0.001) (Fig. 3). Multivariate analysis demonstrated that the 2 curves were significantly different at each time point analyzed (P < 0.05).
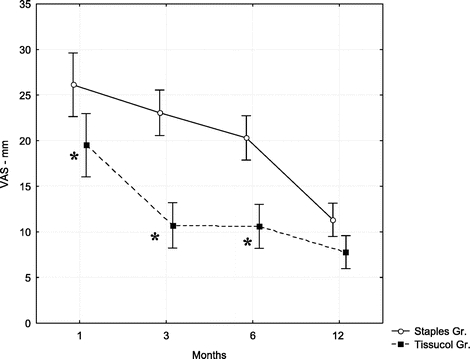
FIGURE 3. Mean VAS scores at 1, 3, 6, and 12 months of follow-up. VAS ranges from 0 (no pain) to 100 (maximum pain). Error bars represent SD. *P < 0.001 between the groups of study.
Based on scores for the modified SF-36 questionnaire at 1 month, postoperative morbidity was reduced in the Tissucol group compared with the staples group (Fig. 4), reflecting a quicker return to work and social life (23.2 vs. 22.6, respectively; P < 0.05). Total scores were similar for the treatment groups at 3, 6, and 12 months postoperatively.
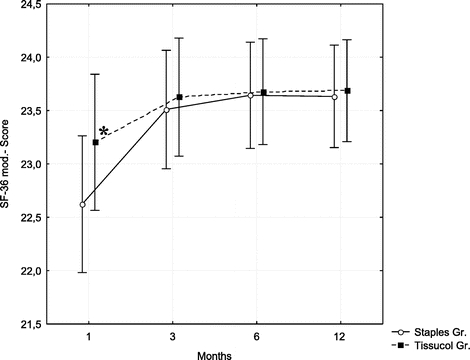
FIGURE 4. Mean scores for modified 36-item Short form General Survey (SF-36) questionnaire at 1, 3, 6, and 12 months of follow-up (SF-36 minimum score = 0, maximum score = 27). Error bars represent SD. *P < 0.001 between the groups of study.
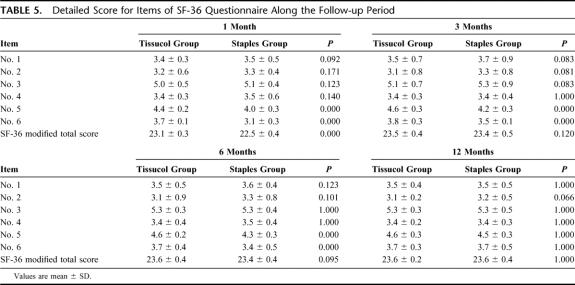
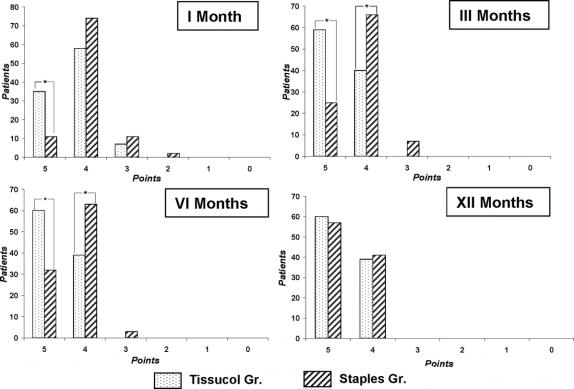
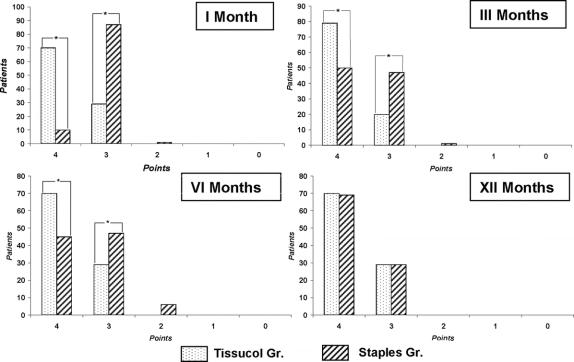
The detailed scores for each item of the SF-36 questionnaire are reported in Table 5. The mean scores of items 5 and 6 reached a significant difference between the 2 groups at 1, 3, and 6 months (P < 0.01). No other item mean scores reached significance at any time-point. The distribution of the score assigned to items 5 and 6 over the population is reported in Figures 5 and 6. A greater proportion of patients in the Tissucol group reached the highest score for item 5 at 1, 3, and 6 months (P < 0.001) and for item 6 at 1, 3, and 6 months (P < 0.001).
TABLE 5. Detailed Score for Items of SF-36 Questionnaire Along the Follow-up Period
FIGURE 5. Distribution of the treated patients according to the multiple choice item no. 5 (minimum score, point 0; maximum score, point 5). *P < 0.001 between the groups of study.
FIGURE 6. Distribution of the treated patients according to the multiple choice item no. 6 (minimum score, point 0; maximum score, point 4). *P < 0.001 between the groups of study.
DISCUSSION
Laparoscopy is a valid alternative to traditional open techniques for the treatment of hernias: the method is associated with a lower incidence of postoperative pain and, furthermore, permits rapid recovery of normal physical activity.3–6 In conventional TAPP, the prosthesis is anchored using metal clips. This is a critical step that requires the utmost attention to avoid damaging the surrounding nerves and blood vessels. Lesions arising due to such intraoperative damage can lead to complications, including hemorrhage, or painful neuralgia during follow-up.5,7,8
The nerves in the inguinal area that are most frequently involved in postoperative pain following TAPP hernia repair include the genitofemoral, lateral cutaneous femoral, and ilioinguinal and iliohypogastric nerves. According to several authors, lesions of the lateral cutaneous femoral nerve are the most frequent postoperative neurologic complications associated with laparoscopy, involved in between 0.1% and 10% of cases.3,4,6,9,10 Such lesions are the result of damage or entrapment of the nerve during lateral fixation of the mesh to the deep inguinal ring, with pain in the lateral region of the thigh.
Our experience has revealed that some patients who undergo TAPP with staples report postoperative neuralgia, with pain at the pubic or suprapubic level rather than on the lateral side of the thigh. This may be associated with the positioning of 3 metal clips at the level of Cooper's ligament and the pubic tubercle. Some fixations are carried out laterally at the level of the deep inguinal ring, thus eliminating the risk of damaging the lateral cutaneous femoral nerve. In addition, at each point, the mesh is raised so that it does not impede the nerve branches of the abdominal wall, which are possible sources of paresthesia or pain.
A number of techniques have been proposed for further reducing the incidence of neuralgia following TAPP, including the vertical application of staples or reduction in the number of staples used.3,7,11 Smith et al12 and Ferzli et al13 proposed that the mesh need not be secured; however, the need for anchoring the prosthesis has been demonstrated by Katkhouda et al11 as well as by our own clinical experience.
Considering historical data from our own unit between March 1992 and May 2003, reintervention for recurrence in patients who undergo TAPP with staples (12 cases; incidence, 0.6%) showed that in all cases, migration of the mesh at the suprapubic level, due to loss of fixation at Cooper's ligament, arose from improper positioning of the staples.
To reduce the risk of postoperative neuralgia while ensuring mesh fixation, together with classic laparoscopy, we adopted the use of Tissucol for fixation of prosthetic meshes. Fibrin is a protein with adhesive properties involved in the final steps of coagulation. Surgical fibrin glue is a solution of human plasma proteins, mainly fibrinogen, that are activated by the addition of human thrombin and calcium chloride. When applied to tissue surfaces, fibrinolysis occurs and the glue is substituted by fibrotic tissue, facilitating repair. Its adhesive and hemostatic properties have been demonstrated in a number of experimental studies and clinical trials.14–16
In our study, no cases of neuralgia were observed in the Tissucol group, during a mean of 11.9 months' follow-up. Patients in the Tissucol group had lower mean VAS scores than patients in the staples group. Although the multivariate analysis revealed a statistical difference at each time point in the trial, the clinical difference was marked, especially between 3 and 6 months from the intervention when the score difference was higher and clinically relevant (9 and 11 points for Tissucol and staples, respectively).
The data collected at 1 month from intervention revealed only a 7-point difference between the groups. When integrated with the functional status data, this measure achieved a clinical significance. The analysis of the SF-36 modified scores provides additional information on the clinical effects observed with the 2 different procedures. The mean scores of the SF-36 revealed a significant difference only at 1 month; however, evaluation of mean scores of single items favored Tissucol treatment throughout the follow-up period for postoperative pain (item 5) and its influence over the working activities (item 6). This difference was marked at 1, 3, and 6 months (P < 0.001) but was less pronounced at 12 months. These data indicated that the use of Tissucol for mesh fixation reduced postoperative pain compared with the use of staples. This was supported by a significantly faster resumption of physical or normal activities in comparison with the staples group (7.9 days vs. 9.1 days, respectively; P < 0.001).
Only 1 case of pain was reported in the Tissucol group. This occurred after intense and prolonged exercise and for which analgesics were rarely required. The only hernial recurrence occurred in 1 of the first patients subjected to TAPP using Tissucol, and was attributed to technical errors. Importantly, it was the only case in which a mesh with large netting was not used. It is therefore probable that the incomplete integration between Tissucol and the mesh reduced the adhesive properties of the Tissucol and allowed the mesh to migrate. Second, as this case was a direct hernia, a mesh of larger dimensions should have been used to better reinforce the posterior wall of the inguinal canal as was used in the other 13 (30%) cases of direct hernia. Subsequently, the patient underwent surgery to repair the hernia and remains free of recurrence at 12 months of follow-up.
In our view, our progressive surgical experience and standardization of the technique prevented such complications in successive cases, and this facilitated a reduction in the cost of the operating-room time through reduction in the surgery time. Based on the experience gained in this study and historical data from our unit, the use of Tissucol in laparoscopic treatment of inguinal and femoral hernias was found to have several advantages. From a mechanical standpoint, fixation of the mesh was equivalent to that obtained with clips but prevented complications related to the application of staples (bleeding and hematomas in Retzius' space, neuralgia, and chronic pain). An additional advantage was cost: as of 2005, 1 mL of Tissucol for repair of a unilateral hernia costs about U.S. $100, while staples cost around U.S. $170. On a larger scale, considerable cost savings can be expected if postoperative complications (neuralgias, seromas, and hematomas) are reduced and hospital recovery periods are shortened.8,15,17
Although our study included only a modest number of cases, in our opinion, the use of human fibrin glue for fixation of mesh in TAPP is valid and warrants investigation in larger, controlled clinical trials. Compared with historical data from our own unit, this method provides results that are comparable to standard laparoscopic techniques in terms of duration of intervention and rate of recurrence, with the advantage of reducing the incidence of postoperative neuralgia.
ACKNOWLEDGMENTS
The authors thank Ms. Rowena McMenamin for careful review of the manuscript as well as Mrs. Milena Ruggeri for her precious and irreplaceable help.
Footnotes
Reprints: Federico Lovisetto, MD, Istituto di Chirurgia Epatopancreatica, IRCCS Policlinico S.Matteo, P.le Golgi n°1, 27100 Pavia, Italy. E-mail: fedelovi@yahoo.com.
REFERENCES
- 1.Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38:633–638. [DOI] [PubMed] [Google Scholar]
- 2.Kelly AM. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med. 1998;5:1086–1090. [DOI] [PubMed] [Google Scholar]
- 3.Bueno J, Serralta A, Planells M, et al. Inguinodynia after two inguinal herniorrhaphy methods. Surg Laparosc Endosc Percutan Tech. 2004;14:210–214. [DOI] [PubMed] [Google Scholar]
- 4.Mahon D, Decadt B, Rhodes M. Prospective randomized trial of laparoscopic (transabdominal preperitoneal) vs open (mesh) repair for bilateral and recurrent inguinal hernia. Surg Endosc. 2003;17:1386–1390. [DOI] [PubMed] [Google Scholar]
- 5.Onofrio L, Cafaro D, Manzo F, et al. Tension-free laparoscopic versus open inguinal hernia repair. Minerva Chir. 2004;59:369–377. [PubMed] [Google Scholar]
- 6.Smith JR, Demers ML, Pollack R, et al. Prospective comparison between laparoscopic preperitoneal herniorrhaphy and open mesh herniorrhaphy. Am Surg. 2001;67:11–17. [PubMed] [Google Scholar]
- 7.Katkhouda N. A new technique for laparoscopic hernia repair using fibrin sealant. Surg Technol Int. 2004;12:120–126. [PubMed] [Google Scholar]
- 8.Langrehr JM, Schmidt SC, Neuhaus P. Initial experience with the use of fibrin sealant for the fixation of the prosthetic mesh in laparoscopic transabdominal preperitoneal hernia repair. Rozhl Chir. 2005;84:399–402. [PubMed] [Google Scholar]
- 9.Quilici PJ, Greaney EM Jr, Quilici J, et al. Laparoscopic inguinal hernia repair: optimal technical variations and results in 1700 cases. Am Surg. 2000;66:848–852. [PubMed] [Google Scholar]
- 10.Totte E, Van Hee R, Kox G, et al. Surgical anatomy of the inguinal region: implications during inguinal laparoscopic herniorrhaphy. Eur Surg Res. 2005;37:185–190. [DOI] [PubMed] [Google Scholar]
- 11.Katkhouda N, Mavor E, Friedlander MH, et al. Use of fibrin sealant for prosthetic mesh fixation in laparoscopic extraperitoneal inguinal hernia repair. Ann Surg. 2001;233:18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith AI, Royston CM, Sedman PC. Stapled and nonstapled laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair: a prospective randomized trial. Surg Endosc. 1999;13:804–806. [DOI] [PubMed] [Google Scholar]
- 13.Ferzli GS, Frezza EE, Pecoraro AM Jr, et al. Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg. 1999;188:461–465. [DOI] [PubMed] [Google Scholar]
- 14.Canonico S. The use of human fibrin glue in the surgical operations. Acta Biomed Ateneo Parmense. 2003;74:21–25. [PubMed] [Google Scholar]
- 15.Fernandez Lobato R, Garcia Septiem J, Ortega Deballon P, et al. Tissucol application in dermolipectomy and incisional hernia repair. Int Surg. 2001;86:240–245. [PubMed] [Google Scholar]
- 16.Zieren J, Castenholz E, Baumgart E, et al. Effects of fibrin glue and growth factors released from platelets on abdominal hernia repair with a resorbable PGA mesh: experimental study. J Surg Res. 1999;85:267–272. [DOI] [PubMed] [Google Scholar]
- 17.McCormack K, Wake B, Perez J, et al. Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess. 2005;9:1–203. [DOI] [PubMed] [Google Scholar]