Abstract
Objective:
To determine the nature of surgeon information transfer and communication (ITC) errors that lead to adverse events and near misses. To recommend strategies for minimizing or preventing these errors.
Summary Background Data:
Surgical hospital practice is changing from a single provider to a team-based approach. This has put a premium on effective ITC. The Information Transfer and Communication Practices (ITCP) Project is a multi-institutional effort to: 1) better understand surgeon ITCP and their patient care consequences, 2) determine what has been done to improve ITCP in other professions, and 3) recommend ways to improve these practices among surgeons.
Methods:
Separate, semi-structured focus group sessions were conducted with surgical residents (n = 59), general surgery attending physicians (n = 36), and surgical nurses (n = 42) at 5 medical centers. Case descriptions and general comments were classified by the nature of ITC lapses and their effects on patients and medical care. Information learned was combined with a review of ITC strategies in other professions to develop principles and guidelines for re-engineering surgeon ITCP.
Results:
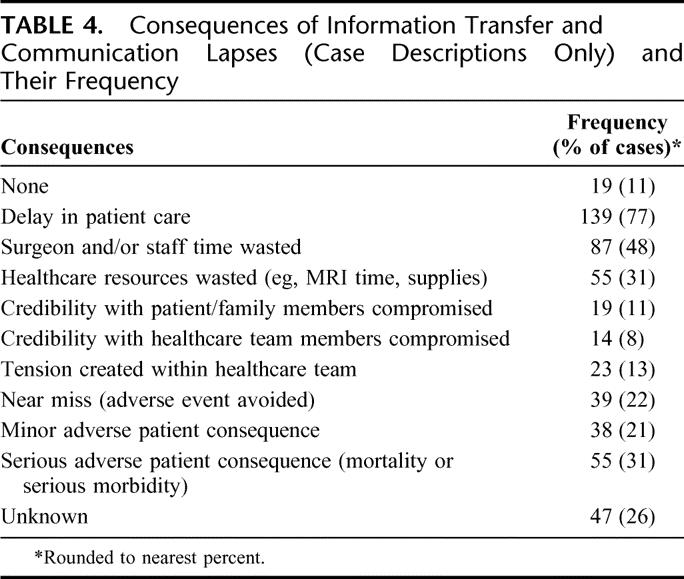
A total of 328 case descriptions and general comments were obtained and classified. Incidents fell into 4 areas: blurred boundaries of responsibility (87 reports), decreased surgeon familiarity with patients (123 reports), diversion of surgeon attention (31 reports), and distorted or inhibited communication (67 reports). Results were subdivided into 30 contributing factors (eg, shift change, location change, number of providers). Consequences of ITC lapses included delays in patient care (77% of cases), wasted surgeon/staff time (48%), and serious adverse patient consequences (31%). Twelve principles and 5 institutional habit changes are recommended to guide ITCP re-engineering.
Conclusions:
Surgeon communication lapses are significant contributors to adverse patient consequences, and provider inefficiency. Re-engineering ITCP will require significant cultural changes.
This manuscript provides a taxonomy of surgeon and surgical resident information transfer and communication practices associated with adverse events and near misses. It also recommends 12 principles and 5 institutional culture changes to guide the re-engineering of surgical hospital environments to foster improved surgeon information transfer and communication and to decrease associated costs, adverse events, and near misses in patient care.
The evolution of surgical care toward a team-based approach to service delivery1 places a premium on the quality of surgeon information transfer and communication (ITC) about the patient and the plan of care for that patient. A number of research reports have documented that communication lapses among physicians are a key factor in medical errors;2–7 however, little is known about the specifics of surgeon communication in hospital environments and few studies exist about surgeon communication outside of the operating room. The purposes of this study were to 1) better understand the current state of information transfer between and among surgical residents and attending surgeons, 2) understand the way that surgeon communication contributes both positively and negatively to the quality and efficiency of hospitalized patient care, and to 3) integrate this information with what has been learned about ITC in other professions into a series of principles and guidelines for use by surgeons desiring to re-engineer information transfer, communication, and related work flow practices.
PHASE 1. CURRENT STATE OF INFORMATION TRANSFER AND COMMUNICATION PRACTICES AND THE EFFECTS ON SURGICAL PRACTICE AND OUTCOMES
Methods
Research Setting
This study was approved by the Southern Illinois University School of Medicine Institutional Review Board and was conducted in accordance with the approved protocol. The study consisted of data collected through direct observation, focus groups, and a web-based survey. Observation was completed in the trauma and critical care services at one institution. Focus groups were conducted in 5 medical centers with general surgery residency programs of varied size and location within the United States. Case reports also were solicited from general surgery program directors via the list server of the Association of Program Directors in Surgery. All participants in the study read and signed written informed consent forms. Participants were instructed not to reveal information that could identify patients or providers, and no names, places, or dates were recorded. Investigators removed all information regarding data collection sites, making it impossible to trace an incident to any particular provider, patient, or location.
Conduct of Initial Observations
To prepare for the focus groups, attending surgeons and a nurse monitored morning rounds within a trauma service for 1 month to identify problems that may have included ITC elements. The designated nurse and project staff members then acquired more information about each incident. Attending trauma surgeons also maintained notes on such events. At the end of each week, the trauma nurses presented these incident reports to the attending trauma surgeons and project investigators. Incidents were discussed, analyzed, and reduced to incident reports. An initial taxonomy of ITC problems was created and refined. A second 1-month observation period occurred later in the year to determine the extent to which earlier findings transfer across time, participants, and circumstances and to refine the taxonomy.
Conduct of Focus Group Sessions
Three focus group sessions were held at each participating surgical residency site: one each for general surgery residents, attending surgeons, and other health professionals who worked with surgeons (nurses, case managers, pharmacists). The focus group sessions were conducted separately to encourage open disclosure of information about events leading to adverse patient outcomes or near misses. The final participant sample consisted of 59 residents (PGY 1–5), 36 attending surgeons, and 42 nurses and allied health professionals.
The 15 focus group sessions were each approximately 90 minutes in length and used a semi-structured interview approach. The primary focus was to develop an inventory of situation descriptions where incomplete or inaccurate ITC involving surgical residents and surgeons led to situations that either compromised patient care or had the potential to do so. The focus group moderator conducted the discussion with a goal of acquiring a description of what happened, how it affected patient care or had the potential to do so, and how inaccurate and incomplete ITC practices contributed to this incident. Emphasis was on acquiring descriptions of the events that participants recalled without regard to when those incidents occurred.
Data Collection During Focus Groups
The focus group leader and 2 observers took notes during each focus group. The sessions were tape recorded to assist observers and tapes were subsequently destroyed. Two observers integrated all 3 sets of notes for each incident. One observer then created a written incident description based on the consensus statement.
Conduct of Web-Based Survey Requesting Submission of Case Reports
A web-based survey was conducted inviting surgery program directors to submit case reports describing incidents where ITC practices led to adverse patient events or near misses. Participants were assured anonymity for themselves and their hospitals.
Data Analysis
Incident reports were classified as case descriptions or general comments (comments about frequently occurring ITC incidents without a specific case example). Incident reports were analyzed by 3 investigators in a constant comparative manner8,9 to identify and characterize factors that compromised or enhanced surgeon and surgical resident communication about patients. The constant comparative approach involves reading individual incident reports, and comparing groups of instances, both similar and different, to develop a sense of pattern and relations. This analysis was informed by the initial trauma service observation and by analysis of known articles on ITC practices both within and outside the field of medicine. An initial set of dimensions for classifying incident descriptions was formulated. One investigator then completed a preliminary classification of all incidents. In this stage, each incident was assigned to as many classifications as fit the incident. The incident classifications were subsequently reviewed and refined by 3 investigators. To provide a test of these classifications and ensure trustworthiness of analysis, incidents were then reviewed by groups of surgeons and nurses who were familiar with the hospital work environment of surgeons. This process included a 2-day meeting where surgeons from all 5 participating sites reviewed and discussed incidents and either validated or changed their classification. Incidents judged to be excellent examples of the classification were identified for use as illustrations. The discussion resulted in refinement of the classifications and of the inclusion criteria for incidents.
One investigator then reviewed all of the incidents again and created a purified classification of each. Most incidents were placed into 1 or 2 classifications that best characterized that incident; a few incidents were placed in 3 categories. This process of independent analysis, followed by group discussion among investigators and then analysis for trustworthiness, was repeated multiple times.
Results
Categorization of Incidents
A total of 328 communication incident reports were collected. A total of 180 (55%) were case descriptions and 148 (48%) were general comments. Thirteen incident reports (3 case descriptions, 10 general comments) either were not related to the topic of ITC practices or were not developed sufficiently to allow classification. The nature of incident reports and general comments elicited at the 5 sites were very similar.
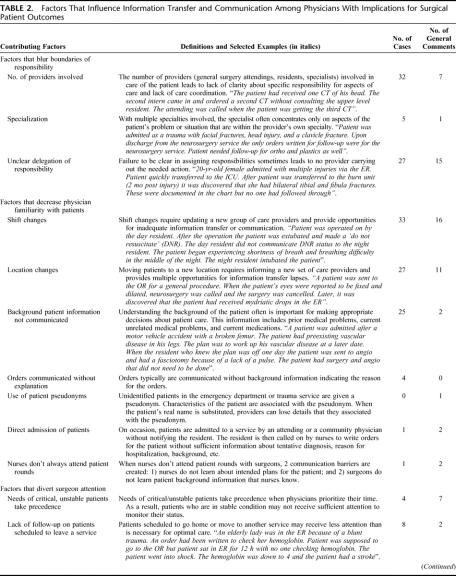
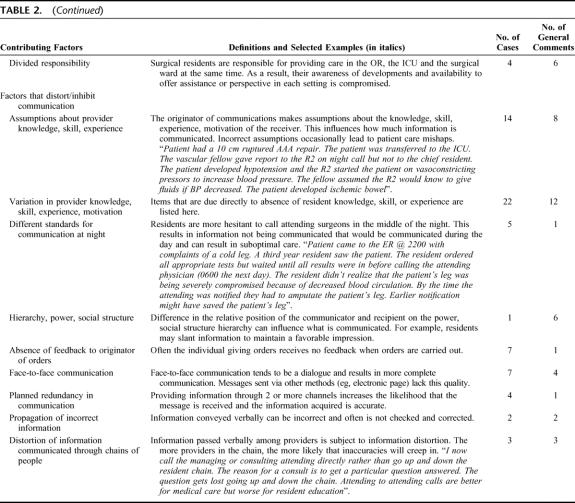
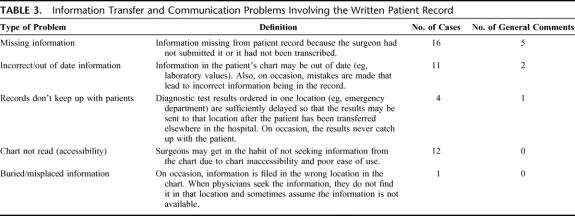
Table 1 provides a summary of the communication events classified broadly by their proximate effects on surgeons and surgical residents. Table 2 provides a more detailed classification with a breakdown of contributing factors, a definition for each, and examples for selected contributing factors. Table 3 provides information about communication problems that involved the written patient record. We also found that certain structural factors affected (both positively and negatively) ITC problems among surgeons and surgical residents. Specifically, the addition of physicians and nurse practitioners to the team solved some problems and created others (6 case reports, 13 general comments). Introduction of communication and information technology had similar positive and negative effects (15 general comments). Finally, the 80-hour workweek was mentioned as a contributor to the problems, but only 3 times. Table 4 shows the consequences of ITC lapses on patients and on the efficiency and effectiveness of patient care. When there were multiple consequences this is reflected in the table.
TABLE 1. Summary of Communication-Related Incidents Reported and Their Effects on Surgeons, Surgical Residents, and Other Providers
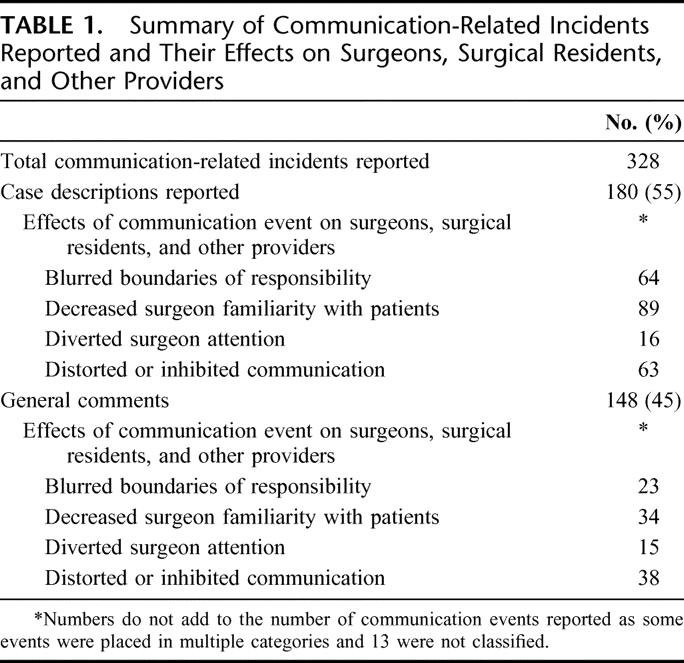
TABLE 2. Factors That Influence Information Transfer and Communication Among Physicians With Implications for Surgical Patient Outcomes
TABLE 2. (Continued)
TABLE 3. Information Transfer and Communication Problems Involving the Written Patient Record
TABLE 4. Consequences of Information Transfer and Communication Lapses (Case Descriptions Only) and Their Frequency
Discussion
The primary purpose of this phase of the research was to develop a taxonomy of surgeon and surgical resident ITC lapses and errors and their effects on patient care processes and outcomes. These communication lapses and errors resulted in 4 primary proximate outcomes for surgeons and surgical residents: 1) Blurring boundaries of surgeon and surgical resident responsibility for aspects of care, 2) decreasing surgeon familiarity with aspects of the patient's situation potentially resulting in compromised patient care, 3) diverting surgeon attention away from the patient's situation and the surgeon's patient care tasks, and 4) distorting or inhibiting the amount and/or nature of information communicated among care providers.
Blurred Boundaries of Responsibility
We identified 3 primary factors that blurred the boundaries of responsibility for surgeons and surgical residents: 1) number of providers involved in caring for the patient (resident involvement increased this number); 2) number of specialties involved in care (tasks that did not clearly belong to one specialty tended to be ignored); and 3) failure to explicitly assign patient care tasks to an identified member of the care team or to one patient care team. Examples include an attending surgeon on rounds saying, “We ought to order an x-ray” without identifying a provider to do that; or confusion regarding whether the orthopedics team or the general surgery team will order antibiotics.
The example in Table 2 under “unclear delegation of responsibility” describes a patient with leg fractures that were not treated during a 2-month hospital stay. More than one surgeon maintained that this should not be listed as a communication problem but rather a single provider's irresponsibility. We have retained this as a communication problem since responsibility is shared among team members and communication is needed to assure that all tasks are completed.
Decreased Patient Familiarity
We identified 7 factors that contributed to decreased surgeon familiarity with patients and with patient care activities (Table 2). Most often noted were: 1) moving patients to different locations in the hospital and the associated need to continually educate new providers about patient details (38 reports); 2) shift changes (49 reports) for the same reasons; and 3) absence of recorded background information about the patient (eg, medication allergies) (27 reports) and about reasons for patient orders (4 reports).
Diverting Surgeon Attention From Patients
Three factors were noted that diverted surgeon and surgical resident attention from patients and tasks at hand. Eleven incident reports noted that surgeons and surgical residents give priority to the needs of critical and unstable patients. Those cases documented patient events where something went wrong and was not detected as patients were monitored less frequently because they appeared stable and were scheduled to go home or be transferred to another service.
Ten reports highlighted that surgical residents are responsible for providing concomitant care in the OR, in the ICU, and on the surgical ward. Such residents are less aware of developments in any one location. Further, they are less available to offer assistance to nurses and other healthcare providers in distant locations.
Distorting Communication Among Providers
A number of factors were identified that can distort or inhibit communication among surgeons and surgical residents. Two of these concern disparities in the relative knowledge/skill/motivation of the sender and the recipient of the communication. In some cases, communication lapses were attributable to incorrect sender assumptions about the knowledge of the recipient (Table 2). Inadequate knowledge on the part of the sender also may result in incomplete or inaccurate reporting of a patient's situation.
A second factor distorting or inhibiting communication was that communication practices differed between day and night as has also been cited in internal medicine residencies.10 The example report in Table 2 highlights adverse outcomes that occurred as a result of a resident failing to call the attending surgeon at night. Another incident report documented an occasion where an attending surgeon was not informed of a patient's overnight death before meeting family members in the morning. Efforts should be addressed to establishing systematic rules about when residents should call attending surgeons.
The third factor that contributed to distorted or inhibited communication was the hierarchical status of the communicator and the recipient. Residents may withhold or distort information in an effort to make themselves look good in the eyes of superiors, or may not confront superiors with an alternate point of view for fear of compromising their standing. Sutcliffe et al5 documented this factor in their study of medicine residents. We found relatively few examples of this phenomenon but enough to document its presence in surgical settings as well.
The “telephone game” documents the degradation of information accuracy that occurs when information is passed verbally through chains of people. We found this effect among surgical residents as well (Table 2, “Distortion of information communicated through chains of people”).
Table 3 includes a subcategory “chart not read.” We have had colleagues argue that this is not a failure of the written record just a failure to use it when appropriate. We have included this subcategory because we found that “not read” was often a symptom of poorly organized information in charts and of poor chart accessibility.
Table 4 documented that surgical resident and surgeon communication lapses and problems were significant contributors to inefficiency, cost, and adverse patient consequences. The most common consequence reported was delay in patient care (present in 77% of the incidents) followed by wasted surgeon and staff time (48% of incidents). While not reflected in Table 4, reading the incident reports makes it clear that the amount of staff time wasted per incident was significant, often amounting to hours of time expended. One recurring example involved residents trying to determine whether a patient's C spine had been cleared.
A significant number of reports included serious adverse patient consequences (31%). This, combined with the percent of cases reporting minor adverse consequences (21%) and near misses (22%), documents the important role that surgeon and surgical resident communication plays in surgical patient care and outcomes. These results are consistent with other studies addressing the importance of communication as a factor in adverse patient events and near misses.6,7 The importance of understanding and improving physician communication practices is underscored by the degree to which physicians depend on face to face and real-time communication to support their work.11
The number of medication related errors was smaller than we expected given the concentration of articles on this topic in the medical literature.12,13 We offer 3 possible explanations for this finding. First, it is possible that medication errors with surgical patients are less common. Second, our data collection methods are based on retrospective recall of events. Most published studies about medication errors involve documentation based on chart review. The 2 methods may simply highlight different types of errors. Finally, it is possible, though unlikely, that fewer medication-related errors are attributable to communication factors.
As mentioned earlier, the goal of this study phase was to develop an inventory and taxonomy of incidents that led to adverse events or near misses and had a communication component to them. While we report frequencies of incident types, our research methods are subject to recall bias. Recalled incidents reflect prominence in respondents’ memories (eg, dramatic events) and perceptions of frequency. Accurate frequencies remain to be determined through prospective observational studies.
While much of the attention in the literature has been on improving patient safety, the results of this phase of the study make it clear that improving ITC practices has an equally important part in minimizing wasted staff time and healthcare resources.
PHASE 2. ESTABLISHING PRINCIPLES AND GUIDELINES FOR USE BY SURGEONS DESIRING TO RE-ENGINEER INFORMATION TRANSFER, COMMUNICATION, AND RELATED WORK FLOW PRACTICES
Methods
Review of Literature on Safety and Communication
The second phase of the study involved determining what had been learned about ITC practices in other professions where information transfer lapses and communication failures have serious consequences. A search of the patient safety literature was conducted looking for articles from surgery and other medical professions that addressed communication issues. A broader search was conducted for articles involving safety in non–patient-related professions. The work of Patterson et al14 describes handoff strategies in 4 professions where there are high consequences for information transfer failure, providing concrete ideas for improving ITC practices in surgery and a framework for thinking about these problems.
Integration of Phase 1 Results With Data Regarding Possible Solutions
We integrated what we learned through phase 1 data collection activities, study of communication strategies and problems in other professions and study of general articles on communication and work flow management, and created an initial set of principles and guidelines for re-engineering surgeon ITC and associated work flow practices. The principles were then reformulated into possible solutions. The most promising solutions were prioritized by using a protocol we developed that considered possible implementation strategies, benefits, amount of culture change (anticipated types of resistance, barriers to implementation), costs, level of technology, and environments most amenable to each solution.
Field Testing of Possible Solutions
Approximately 60 individuals attending 2 Association of Program Directors in Surgery workshops on this topic during the 2005 annual meeting evaluated the most promising solutions and offered solutions of their own. The new solutions subsequently were evaluated using the protocol we developed for this purpose.
Refinement of Analysis
The principal investigative team filtered and translated the information acquired into the series of principles and institutional habits described below.
Results and Discussion
Circumstances That Complicate and Place Added Demands on Effective Information Transfer and Communication Practices
Our data revealed that there are 2 major hospital environment and practice characteristics that increase the demand for effective information transfer to optimize the quality of patient care:
Shift Changes (temporal separation of providers). Shift changes were raised as a contributory factor to adverse events and near misses in 49 of the 328 incidents (Table 2). These changes raised the stakes for high quality information transfer if adverse events are to be avoided.
Patient Location Changes (geographic separation of providers) also placed increased ITC demands on surgeons and surgical residents (38 incidents, Table 2). Efforts to minimize the number of times a patient is moved will minimize the need to continually educate new teams of providers. Increasing emphasis on routine, systematic and thorough communication during handoffs will improve those handoffs that must occur.
Communication Principles That Should Guide the Re-engineering of Information Transfer and Communication Practices
Based on phase 1 data and our review of ITC practices within and outside the healthcare environment, we propose the following communication principles to guide re-engineering of ITC practices among surgeons and residents in the hospital environment.
Principle: Actions and their reasons should be documented in a manner that is easily accessible to cross-covering surgeons. The documentation should describe what prompted the action, what the action was, and what follow-through is needed. Orders frequently do not include an explanation as to why they are being given and an explanation often conveys a great deal of information about the patient's condition and the plan of care. An example from our data illustrates this concern: A patient was being weaned from narcotics; however, the chief resident failed to inform the covering resident of this, and the information was not in the patient record. The patient was placed back on narcotics and had to stay extra days in the hospital. Patterson et al14 noted that providing background information, including reasons for actions, is handled in other professions by providing annotations to official records and by briefing incoming providers regarding the outgoing provider's stance toward changes in plans.
Principle: There should be redundant sources for important information. Important information should be available from a variety of sources to increase the likelihood that providers have access to key information when needed. Some sources include: the official patient chart, sign-out system notes, nurses, and patients. Van Eaton et al15,16 described an institution-wide centralized computerized system, UWCores, to facilitate surgical team members exchanging personal notes about patients. These notes pose questions, provide clarifications and explanations, highlight unfinished tasks and provide asides regarding patient or family dynamics. By providing explanations the system also helps accomplish Principle 1. In the professions studied by Patterson et al,14 there are copious records documenting all decisions made and actions taken. Further, in National Aeronautics and Space Administration mission control handoffs, the incoming controller monitors handoffs of other controllers involved in operating the system (eg, ground operations controllers monitor flight operations controllers) as well as participating in the handoff involving their own area of responsibility. This is analogous to an incoming resident checking on patients and checking with nurses in addition to receiving a handoff from the resident who is being relieved. In medicine, this type of checking is hampered by the absence of systematic and up to date records of many actions.
Principle: Assigned responsibility for patient care should be clear. The team member who is responsible for a task should be made explicit. When multiple teams are participating in care of a patient, the team responsible for a particular task should be clarified. Increasing clarity of responsibility is an objective in all of the professions studied by Patterson et al.14
Principle: The person giving orders should receive timely notice that orders have been carried out and by whom. At the very least, the person giving orders should be notified if the order cannot be carried out for some reason. One example of this problem reported during focus groups follows: An order written for a specific antibiotic was not carried out because the hospital was out of this antibiotic. The physician was not notified and the patient did not receive antibiotic medication for 3 days.
Principle: Processes for surgeon-to-surgeon briefings about patients should be designed to assure that the briefing was received, understood, and if action is needed, no immediate barriers to completing the action are known. Possible barriers include the recipient not: having the skill to complete that task, understanding the plan, agreeing with the plan, having time to complete the task. Weick17 describes a 5-part briefing protocol used by crew chiefs in the U.S. Forest Service to give directions to firefighting crews, which meets the requirements described above: 1) here's what I think we face, 2) here's what I think we should do, 3) here's why, 4) here's what we should keep our eye on, and 5) now talk to me (ie, tell me if you do not understand, cannot do it, see something I do not). Adopting such a framework would help minimize problems due to not understanding the background of the patient (raised 27 times) and/or the reasons for orders (raised 4 times). This practice is directly tuned to help prevent problems due to misconceptions about resident knowledge, skill, or beliefs (raised 56 times during focus groups). The recent addition of requirement 2E to the Joint Commission on Accreditation of Health Care Organizations (JCAHO) National Patient Safety Goals (“Implement a standardized approach to ‘Handoff’ communications, including an opportunity to ask and respond to questions”) and the requirement's associated implementation expectations, will encourage systematization of handoffs and improvement of communication.
Principle: The mode of transmission should be appropriate for the information transmitted. For example, it is difficult to determine and document the spread of infection verbally. A line drawn on the limb to demarcate the infected area with a time and date makes it easier to determine whether the infection is getting better or worse. One example reported during our focus groups involved an attending posting a baseline photograph of a musculocutaneous flap above the patient's bed with orders to call if the appearance of the flap changes.
Principle: Asynchronous channels of communication (eg, e-mail, text pagers, fax machines with acknowledgment) should be refined and used whenever appropriate as they do not interrupt other patient care activities. With asynchronous communication, the recipient can choose when to attend to the message. Spencer et al11 found that 85% of emergency department physician communications were synchronous (face-to-face or telephone) conversations and that 33% of these synchronous communication events were interruptive of other patient care activities. This amounted to an average of 15 interruptions per hour. We think that physicians prefer face to face communication for 2 reasons. First, it assures the sender that the message has been received and attended to by the intended person. The need for face-to-face communication can be reduced if asynchronous communication methods provide these assurances. Asynchronous communication is common in the professions studied by Patterson et al.14 The second reason surgeons prefer face-to-face communication is that they believe face-to-face communication facilitates clarification of information about complex and poorly defined clinical cases through interactive conversation. Weick's view of communication as public sense-making17 and Coiera’ s view of communication as creating common ground18 supports this benefit of face to face communication.
Principle: There should be an efficient way of contacting the person serving a particular role (eg, single pager for surgeon on call) without knowing who is occupying that role. Coiera18 found that up to 25% of calls in the hospital are associated with attempting to identify the name of an individual occupying a specific role at a specified time. We had multiple reports at all sites about the time involved in determining who is on call or who the back-up is when the primary on-call person is in the OR. This appears to be one of the activities that waste the most surgeon and surgical resident time presently. Accomplishing this goal was also a clear focus in the professions studied by Patterson et al.14
Principle: Information transferred verbally among a number of people is error prone. As mentioned in the phase 1 results, verbally transmitting a message serially through a line of people results in serious degradation of information accuracy. Precautions must be taken both to shorten the number of links in the communication chain as much as possible and to assure accurate transmission among each of the links.
Principle: Hierarchical and power differences lead to information transfer and communication problems. Sutcliffe et al5 noted that residents did not want to appear incompetent in front of those with more power and thus hesitated to communicate information that reflected poorly on themselves. Further, resident physicians did not want to offend or bother those in power. Thus, they were hesitant to call attending physicians in the middle of the night. This characteristic also discouraged residents from disagreeing with more powerful physicians when they had a different point of view. In all of these conditions, communication is likely to be distorted or withheld. Our results support these conclusions (7 reports in focus groups). The examples described in Table 2 and Part 1 of this manuscript demonstrate the impact of these dynamics on patient care. Further, we found that these problems are accentuated when residents deal with attending physicians they don't know well (eg, attending physicians in other specialties).
Principle: Surgeons and surgical residents need timely access to a summary of the patient's baseline condition. Often, the baseline condition is unknown or requires lengthy exploration of the medical record to discover. The absence of this information can lead to suboptimal treatment. This was an issue raised 27 times in our focus groups. Table 2 provides an example. Further, since surgeons and residents must move about the hospital, a summary of the patient information must be available to the surgeon, where the surgeon is and not only where the patient is. The study by Patterson et al14 documented that the need for timely access to current, accurate information was a primary focus of the professions they studied.
Principle: More experienced surgeons and surgical residents often assume too much about the knowledge base and/or skill level of junior residents. In Coiera's terms,18 they have not established common ground. This issue was raised 56 times during our focus groups. The example in Table 2, describing a junior resident who started a AAA patient on vasoconstricting pressors to increase blood pressure rather than giving fluids, demonstrates this principle. When assigning tasks, surgeons and surgical residents should be in the habit of confirming: recipient understanding of the plan and comfort with her or his ability to do the assigned task. This practice will empower the individual receiving the assignment to ask questions. This recommendation goes beyond JCAHO Patient Safety Goal 2E,19 at least in emphasis.
Toward an Action Plan for Avoiding and/or Minimizing Information Transfer Problems Among Surgeons
In this section, we propose 5 comprehensive institutional habit changes that should help minimize many of the identified ITC problems. We recommend placing priority on these habit changes as they: a) address multiple problems identified during the data collection portion of this study, b) adhere to one or more of the principles summarized earlier in this paper, c) have been used in other information intensive professions, and d) were viewed as feasible (sociologic resistance and cost barriers were relatively low) by residency program directors and surgical residents (Williams RG, Schwind CJ, Silverman RD, et al. Improving ITC among surgical residents and surgeons. Workshop presented at Association of Program Directors in Surgery. New York, April 1, 2005). Other changes based on the 12 principles can be considered as well.
The 5 institutional habits are as follows:
Establish clarity about who is responsible, and make it easy to reach the responsible person. Make it possible to contact people in designated roles at all levels of the patient care hierarchy (eg, first call resident, chief resident, attending) without needing to know the name of the person serving in that role. Also, have a backup plan and an easy way to reach the back-up provider when necessary. Use of a team (service) pager is an effective way of accomplishing this for the first call resident. Other providers will need to be educated to follow the procedures, for example, to call the first call resident not the person who wrote the order. There should be an unambiguous signal that responsibility for patient care has been transferred. Handing over the team pager serves the dual functions of announcing the change in responsibility to other surgical team members and making it possible for people in remote locations to contact the person serving the designated role without knowing who that person is. A first responder should always be available and easy to contact. Optimal hospital environments should be organized so that surgical residents are responsible for patients in only one area (ward, ICU, OR) at a time. Absent this ideal, more needs to be done to facilitate effective monitoring of and communication about patients by providers who are distributed across hospital environments. When the designated first responder goes to the operating room, the service pager should be handed to an accessible alternate care provider.
Assign specific patient care tasks and responsibilities to providers in a clear and unambiguous manner. Criteria and subsequent actions associated with these tasks should be specified. If studies are pending, specify who is to look for results and what is to be done in the event of normal, abnormal or no results within a specified time frame. For example, “if the CT is normal do nothing. If abnormal or not completed by a certain time call the attending.”
-
Designate one patient care team as the primary team for each patient. The primary team writes or confirms all orders for a single patient. This practice should increase continuity of care and may help prevent narrow specialty-oriented perspectives. For example, it will prevent orthopedics from discontinuing a Foley catheter without considering that the patient also had a bladder repair 2 days ago. This recommendation requires cooperation at the hospital administration level and a significant culture shift.
For this plan to work, there will need to be a mechanism in place for a consultant's recommendations or orders to be quickly communicated to the primary team and for needed actions to be taken rapidly.
-
Routinize and formalize the sign out procedure among incoming and outgoing surgical resident team members to facilitate effective exchange of information and patient care responsibilities.
The sign-out should occur routinely at a designated time and in a designated place. Sign-out should take priority over all activities other than emergencies. Other providers (eg, nurses) should know and respect the priority given to sign-out activities. This recommendation is consistent with the 2006 JCAHO Patient Safety Goals handoff requirement. An optimal sign-out would include the junior and senior resident from the incoming and outgoing teams meeting in a face-to-face conversation. When it comes to routine tasks, the junior residents know more details than the senior residents. When it comes to patient trajectory, the senior residents are critical to an effective information transfer. At the very least, the senior resident needs to audit (review and provide feedback about) the information exchange between junior residents. We realize that this sign-out procedure may create feasibility problems. However, efforts should be made to optimize sign-out considering both feasibility and effectiveness.
A standard briefing protocol (for both process and information) should be used by incoming and outgoing surgical team members for handing off responsibility for patients. Minimally, this protocol should: establish the identity of the patient, indicate what is wrong with the patient, what is expected to happen (ie, needs to be monitored), and what needs to be done. The protocol should also determine whether the receiver understands what is required (“Does this make sense to you?”) and can do what is needed. A survey of general surgery residents that we completed during the ITC practices project indicated that 45% of general surgery residents reported spending less than 15 minutes on handoffs for all their patients at the beginning and end of the day.
A standard system should be provided to facilitate surgical team members exchanging personal notes about patients. These notes are clinician-to-clinician commentaries and are entirely ad hoc. This notes system would provide a means of assuring that both actions and the reasons for those actions are available to all providers in a permanent form throughout the patient visit. The notes usually include questions, provide clarifications and explanations, highlight unfinished tasks, and provide asides regarding patient or family dynamics. The notes would be at high risk for misinterpretation if included in the official medical record. However, they often represent the most important information for assuring patient care continuity. For these reasons, personal notes should be immediately accessible to all providers from any location, not be part of the medical record and be exempted from discovery.
Include in patient care handoffs all patients expected to come under or be released from the care of a patient care team. This includes patients expected to arrive from the OR, recovery room, ER, outpatient setting; and patients expected to be transferred or discharged. Adopting this practice would likely offer significant cost savings by accelerating patient movement through the arrival and departure stages of a hospital stay.
CONCLUSION
Our findings highlight the increased demands that the transition from a single dedicated care provider tradition to a team-based care model have placed on surgeons and surgical residents. This change requires more efficient and effective work flow, and, as highlighted in the JCAHO's new safety goal concerning patient “handoffs,” demands improved ITC processes. In hospital settings, there are circumstances that complicate work flow coordination and put a premium on effective communication among surgical residents and surgeons. First, patients are moved from location to location within the hospital requiring more frequent briefing of surgeons. Second, surgical residents and surgeons also move from location to location within the hospital and engage in multiple simultaneous tasks with many different patients and healthcare workers. As a result, they have problems associated with multitasking (eg, competition for time and attention) and need access to information about patients from multiple locations. Third, since many patients spend multiple days in the hospital, there are shift changes and associated added handoffs and briefings of patient care teams. Fourth, surgical patients are often managed by a number of relatively independent work groups each bringing special expertise. For example, trauma patients may be cared for by a general surgery team, an orthopedics team, a burn team, and a neurosurgery team simultaneously. There typically are team leaders for each of those specialty teams rather than a single leader for all teams caring for the patient.
The results from this study document the important role that communication plays in delivering high-quality care to hospitalized patients and characterize the types of communication lapses and errors that occur in a hospital setting. The incident reports we obtained clearly show that effective communication and work flow coordination among surgeons are inextricably related when caring for hospitalized patients.
We offer a series of principles designed to guide the effective re-engineering of ITC practices among surgical residents and surgeons. To put the principles into context, we described adverse events or near-miss situations that would be avoided or moderated if the environment were re-engineered in accordance with the principle. Finally, we recommend changes in 5 institutional habits that incorporate many of the principles and have the potential to moderate many of the key information transfer problems. These changes should improve collective surgeon and resident understanding of the patient's medical condition, trajectory, and plan for care. We have not provided specific suggestions for implementing either the principles or the 5 institutional habits because the applications need to be tailored to the varied clinical environments where they will be implemented.
Efforts should be directed first toward changing work flow patterns to minimize the need for handoffs wherever possible and then to improve the quality of handoffs when they are necessary. Further, our results documented that ITC practices have a large impact on patient care throughout the working day (eg, passing information about patients in the hall, transferring responsibility for patients when going to the operating room), not just at the time when formal handoffs occur. The results demonstrate the importance of educating surgery residents about ITC issues and their role in effective patient care.
ACKNOWLEDGMENTS
The authors wish to recognize the contributions of Robert H. Bower MD to this study. Dr. Bower was an active collaborator in this research who died prior to completion and submission of this manuscript. Prior to his death, he was Professor of Surgery at the University of Cincinnati. The authors thank the members of the SIU Surgical Education and Performance Group for their assistance in interpreting the focus group results that underlie this study and creating the taxonomy. The authors also thank the General Surgery Program Directors and Coordinators at the Universities of Cincinnati, New Mexico, Southern Illinois, Texas at Houston, and Washington for their assistance in organizing and supporting the focus group activities at their respective institutions. Finally, the authors thank all of the surgical residents, attending surgeons, nurses, and case managers at the 5 participating institutions who took the time to participate in the focus groups and provide us with insight into ITC issues involving surgeons and surgical residents.
Footnotes
Supported in part by a grant from the Center for Excellence in Surgical Education, Research and Training of the Association for Surgical Education Foundation and from United States Surgical. These organizations had no role in the design, conduct, or reporting of the study or in the decision to submit the manuscript for publication.
Reprints will not be available from the authors.
Correspondence: Reed G. Williams, PhD, Department of Surgery, 800 North Rutledge Street, P.O. Box 19638, Springfield, IL 62794-9638. E-mail: rwilliams@siumed.edu.
REFERENCES
- 1.Van Eaton EG, Horvath KD, Pellegrini CA. Professionalism and the shift mentality: how to reconcile patient ownership with limited work hours. Arch Surg. 2005;140:230–235. [DOI] [PubMed] [Google Scholar]
- 2.Gandhi TK. Fumbled handoffs: one dropped ball after another. Ann Intern Med. 2005;142:352–358. [DOI] [PubMed] [Google Scholar]
- 3.Petersen LA, Brennan TA, O'Neil AC, et al. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–872. [DOI] [PubMed] [Google Scholar]
- 4.Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care. 2004;13:330–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79:186–194. [DOI] [PubMed] [Google Scholar]
- 6.Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. [DOI] [PubMed] [Google Scholar]
- 7.Donchin Y, Gopher D, Olin M, et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23:294–300. [DOI] [PubMed] [Google Scholar]
- 8.Creswell J. Qualitative Inquiry and Research Design: Choosing Among Five Traditions. Thousand Oaks, CA: Sage, 1998. [Google Scholar]
- 9.Strauss A, Corbin J. Basics of Qualitative Research, 2nd ed. Thousand Oaks, CA: Sage, 1998. [Google Scholar]
- 10.Tabas G, Rubin F, Hanusa BH, et al. Expectations of groups versus pairs of attendings and residents about phone communications and bedside evaluation of hospitalized patients. Teach Learn Med. 2005;17:217–227. [DOI] [PubMed] [Google Scholar]
- 11.Spencer R, Coiera E, Logan P. Variation in communication loads on clinical staff in the emergency department. Ann Emerg Med. 2004;44:268–273. [DOI] [PubMed] [Google Scholar]
- 12.Forster AJ, Murff HJ, Peterson JF, et al. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20:317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: implications for prevention. ADE Prevention Study Group. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 14.Patterson ES, Roth EM, Woods DD, et al. Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16:125–132. [DOI] [PubMed] [Google Scholar]
- 15.Van Eaton EG, Horvath KD, Lober WB, et al. Organizing the transfer of patient care information: the development of a computerized resident sign-out system. Surgery. 2004;136:5–13. [DOI] [PubMed] [Google Scholar]
- 16.Van Eaton EG, Horvath KD, Lober WB, et al. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200:538–545. [DOI] [PubMed] [Google Scholar]
- 17.Weick KE. Puzzles in organizational learning: an exercise in disciplined imagination. Br J Manage. 2002;13(suppl):7–15. [Google Scholar]
- 18.Coiera E. When conversation is better than computation. J Am Med Inform Assoc. 2000;7:277–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joint Commission on Accreditation of Healthcare Organizations. National patient safety goals for 2006. <http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals> (Accessed: April 17, 2005). [PubMed]