Abstract
Objective:
To evaluate the impact of a cognitive training method on the performance of simulated laparoscopic cholecystectomy in laparoscopic training courses.
Summary Background Data:
Surgeons are like professional sportsmen in that they have to be able to perform complicated, fine-motor movements under stressful conditions. Mental training, systematically and repeatedly imagining a movement's performance, is a well-established technique in sports science, and this study aimed to determine its value in training surgeons.
Methods:
A total of 98 surgeons undergoing basic laparoscopic training participated in a randomized controlled trial; 31 received additional mental training, 32 additional practical training, and 35 received no additional training (control group). All used a Pelvi-Trainer simulator to perform laparoscopic cholecystectomy at baseline and follow-up, after any additional intervention. We used a modified Objective Structured Assessment of Technical Skills (OSATS) instrument to assess performance. Principle outcome variables were the OSATS task-specific checklist (11 procedural steps, scored as correctly [1] or wrongly [0] performed) and the global rating scale (an overall performance evaluation, scored 1–5).
Results:
Improvement in the task-specific checklist score between baseline and follow-up differed significantly between groups (P = 0.046 on ANOVA). Least significant difference tests yielded differences between the mental and practical training groups (P = 0.024) and between the mental training and control groups (P = 0.040), but not between the practical training and control groups (P = 0.789). Paired Student t test showed that performance at follow-up was significantly better in the mental training and control groups (mental training group, P = 0.001; control group, P = 0.018) but not the practical training group (P = 0.342). There were no significant intergroup differences in global rating scale results.
Conclusion:
Additional mental training is an effective way of optimizing the outcomes of further training for laparoscopic cholecystectomy. It is associated with fewer costs and with better outcomes in some crucial assessment scales than additional practical training.
This randomized controlled trial aimed to determine the value of additional mental training (MT) in laparoscopic training courses with 98 surgeons in three study groups performing laparoscopic cholecystectomy (assessed with modified version of Objective Structured Assessment of Technical Skills): MT, practical training, or no training. MT showed significantly higher improvements than practical or no training, and it is associated with fewer costs.
Surgeons have to perform many complicated fine-motor movements, which are not part of the normal repertoire of body movements, and they must do this under very stressful conditions. These demands are similar to those facing professional sportsmen. Striving to perfect complicated movements is the ultimate goal in surgery, and it is a goal shared with professional sports. Because of these common aspirations, it seemed logical to us to combine surgery and sports science in an interdisciplinary fashion when designing training methods in surgery.1
Mental training, systematically and repeatedly imagining a movement without actually performing it, has been validated and applied successfully in professional sports for a long time.2,3 We thought that including mental training in surgical training might confer appreciable advantages. This study aimed to determine whether additional mental training is more effective in optimizing the performance of laparoscopic cholecystectomy than standard training or additional practical training.
Mental Training
In addition to a detailed description of the procedure, which is readily available from an appropriate surgical atlas, mental training for surgery requires specific phrasing of instructions. Specific phrasing means that the procedure must first be broken down into its so-called nodal points, the necessary structural motor components that must be performed in sequence and are marked by a reduction in the degrees of freedom of action.4 Positive motor instructions and precise identification of potential hazards are then assigned to each nodal point, appropriate colored illustrations are included, and an “operation primer” is produced (Fig. 1).5,6
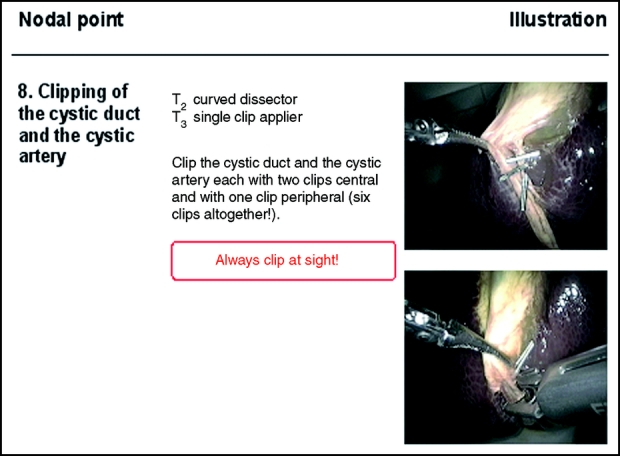
FIGURE 1. Page of operation primer for the laparoscopic cholecystectomy for nodal point 8.
The primer forms the basis for both motor training sessions using operation simulators and mental training sessions. Four kinds of mental training sessions can be distinguished7:
External observative training: the trainee observes a model while it is performing the movement to be learned.
Subvocal training: the trainee calls up a clear visual image of the movement through external or internal self-talk.
Internal observative training: the trainee visualizes himself or another person from the outer perspective performing the movement he or she wants to practice.
Ideomotoric training: the trainee imagines the movement from the inner perspective. He visualizes himself executing the movement and tries to feel it, including as many sensory aspects of the process as possible.
The combination of motor and mental training sessions forms the basis for building a functional mental representation of the surgical procedure. This can be seen as a determining quality marker in training; it integrates the half-conscious inner image of the movements that need to be performed and the conscious mental representation of the cognitive parts of the procedure.4
METHODS
Study and Participants
Mental training for laparoscopic cholecystectomy was tested in a randomized controlled trial using a prepost test design. Data were collected between August 2002 and June 2003 during ten 4-day training courses on basic laparoscopy offered by the European Surgical Institute, Norderstedt, Germany. All course participants, surgeons undertaking specialist training, were eligible for inclusion. They were given written information about the study 2 weeks before their course and during a short presentation at the end of the first day. Course members were asked to decide whether to participate at the start of day 2.
The study took place at the end of day 2 and the beginning of day 3. Each trainee was allowed to perform a laparoscopic cholecystectomy once before they undertook the baseline procedure so that they could familiarize themselves with the Pelvi-Trainer simulator. The Pelvi-Trainer comprises an oval plastic housing, which is sealed with a neoprene mat and contains a pig's liver and gallbladder. This training dummy has been well evaluated and meets the criteria for operation simulation in relation to: fidelity, organ properties, organ reaction, interactivity, and sensory feedback.8
During baseline procedures, trainees were assisted by medical students who were not told to which study group trainees would be assigned. Student assistants had undergone a 3-hour training course at the European Surgical Institute to learn how to hold the camera and the instruments. During baseline procedures, trainees had no instruction or supervision from course instructors or their assistants.
After the baseline procedure, trainees were randomly assigned by lot; each participant took 1 of 12 not identifiable papers out of a box (4 for each group): to a group given additional mental training, a group given additional practical training, or a control group given no additional training. Because each of the 10 laparoscopic training courses included a maximum of 12 surgeons, the randomization of course participants resulted in a maximum of 4 participants in each group. Participant flow is described in Figure 2.
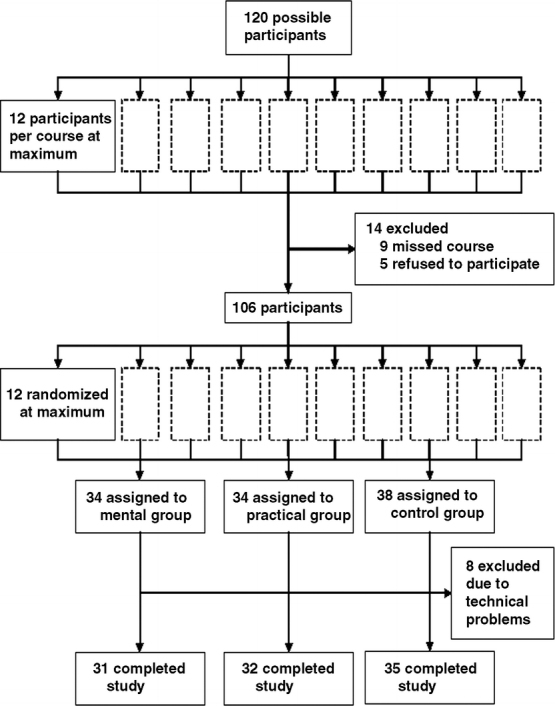
FIGURE 2. Trial participant flow.
Interventions
The 3 groups of participants underwent the following training:
Control Group
These trainees completed the second day of the course and began the third without any additional training, as did surgeons who did not take part in the study at all.
Practical Training Group
During an additional practical training session of 90 minutes, these trainees performed another simulated laparoscopic cholecystectomy and spent time (30 minutes) at the beginning of the third day preparing for the follow-up by studying scientific articles and the surgical atlas for the procedure.
Mental Training Group
This group had one-to-one mental training lasting 90 minutes. Each participant was assigned by lot to one of 4 mental trainers (from a pool of 6). Mental trainers were senior surgeons from different surgical clinics in Hamburg. All had undergone a 2-day training course in mental training led by a sports psychologist and were allocated to the training courses according to their availability. Mental trainers introduced participants to the process of mental training and gave them the operation primer. Participants were then given 30 minutes on their own to learn the primer by heart. During subvocal training, participants recalled the wording of the primer through external self-talk under the supervision of the mental trainer. After a short relaxation exercise, subjects visualized their inner perception of the operation based on the primer (ideomotoric training), first under the tutelage of the mental trainer, then on their own. At the beginning of the third day, just before follow-up, participants repeated the subvocal and the ideomotoric training sequences in a shortened version under the supervision of the mental trainer (30 minutes).
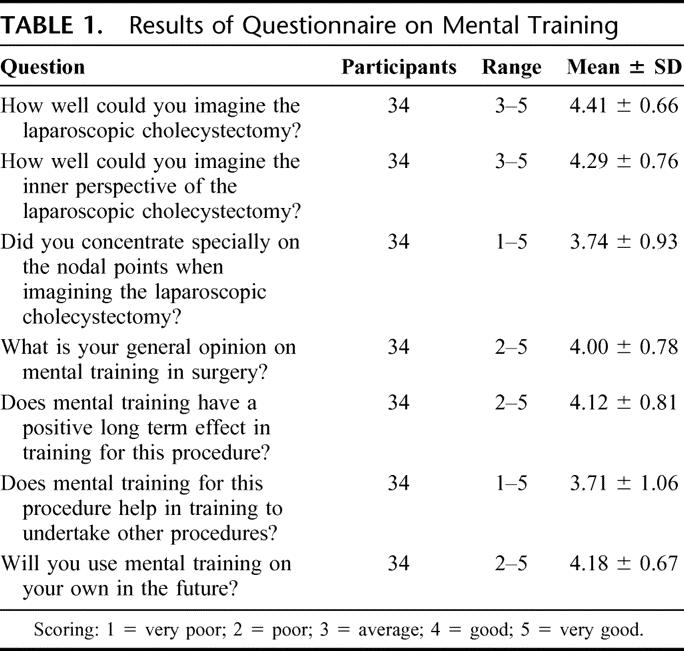
All participants were then asked to perform a follow-up laparoscopic cholecystectomy using the Pelvi-Trainer simulator. They were helped by the same assistants who had attended them for the baseline procedures. Finally, the mental training group was asked to complete a questionnaire designed to solicit their view of mental training (Table 1). Each question (eg, about the general opinion on mental training) had to be answered by the surgeon on a 5-point-scale (1 = very poor; 2 = poor; 3 = average; 4 = good; 5 = very good).
TABLE 1. Results of Questionnaire on Mental Training
Recording Data
All procedures were videotaped and encoded. Tapes were then evaluated by 4 independent surgeons from the University of Cologne. Evaluators underwent a 1-day training course at the European Surgical Institute to ensure the evaluations were consistent and standardized. Six weeks beforehand, they had each been given 10 videos of baseline and follow-up procedures from the 3 groups plus the evaluation instrument, the Objective Structured Assessment of Technical Skills (OSATS).9–12 At the beginning of the training course, the results of their evaluations were discussed. In addition, the evaluators' performance was calibrated by assessing 5 other videotaped baseline and follow-up procedures together.
OSATS integrates different assessment systems and was modified for this study. In the task-specific checklist, each of 11 nodal points of the laparoscopic cholecystectomy procedure was judged as correctly (1 point) or incorrectly (0 points) performed. Thus, a maximum of 11 points could be achieved. For the global rating scale, the entire procedure was evaluated in relation to 5 items (respect for tissue, time and motion, instrument handling, flow of operation, and forward planning and knowledge of specific procedure) and scored on a 5-point rating scale. Since evaluators could not clearly assess the items knowledge of instruments and use of assistants, which are part of original OSATS, we left them out.
The videos were assigned to the evaluators by lot. Each evaluator received the same number of videos from each group. The baseline and follow-up videos of each participant were evaluated by the same surgeon. Evaluation took place in a blinded way because the videos were not marked in relation to group and were mixed together. Thus, evaluating surgeons did not know to which group trainees belonged or whether the video represented a baseline or follow-up procedure.
Statistical Analysis
We based the total number of participants needed for the study on the results of a pilot study and a power calculation (Software Power13). The pilot study on mental training in surgery took place at the University of Cologne and included 16 surgeons.4 It indicated that a difference of 10% between baseline rating and follow-up was clinically relevant. We calculated that recruitment of at least 90 participants would provide sufficient power (80%) to detect an intergroup difference at a significance level of 5%.
Participants' baseline data and primary outcome variables between the groups were compared by analysis of variance (ANOVA). In the case of a significant difference, pairwise comparisons were performed at the same level of significance by t test. Adjustment of the significance level was not necessary because of the closed test principle. Intragroup follow-up and baseline values were compared by paired Student t test. Data were analyzed with SPSS (version 12.0) and P < 0.05 was considered significant.
RESULTS
Participants
A total of 120 trainees could have attended the course; in the event 111 were present and 106 (95.5%) volunteered. Eight were excluded because of technical problems with videos, leaving a total sample of 98 subjects. There were 31 participants in the mental training group, 32 in the practical training group, and 35 in the control group (Fig. 2).
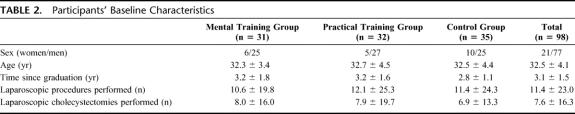
All participants were working as surgeons, so the 3 study groups were relatively homogeneous in terms of baseline characteristics (Table 2). Groups did not differ significantly with regard to age, years since graduation, number of laparoscopic operations performed, number of laparoscopic cholecystectomies performed, or the baseline scores achieved for the primary outcome variables (Table 3).
TABLE 2. Participants' Baseline Characteristics
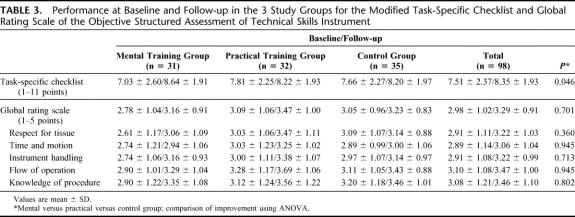
TABLE 3. Performance at Baseline and Follow-up in the 3 Study Groups for the Modified Task-Specific Checklist and Global Rating Scale of the Objective Structured Assessment of Technical Skills Instrument
Relative Costs
Additional costs were associated with the interventions. Practical training sessions cost approximately 300 € ($360) each [laboratory: 200 € ($240); organs and instruments: 100 € ($120)], while mental training session cost around 100 € ($120) for the mental trainer.
Task-Specific Checklist
ANOVA showed significant intergroup differences in the improvement between baseline and follow-up for the OSATS task-specific checklist (P = 0.046; Table 3). Tests of least significant differences showed statistically significant differences between the mental training and practical groups (P = 0.024) and between the mental training and control groups (P = 0.040) but not between the practical training and control groups (P = 0.789). Trainees' performances at follow-up were significantly better than at baseline in the mental training (P = 0.001) and control groups (P = 0.018), but no significant difference was found in the practical training group (P = 0.342) (paired Student t tests).
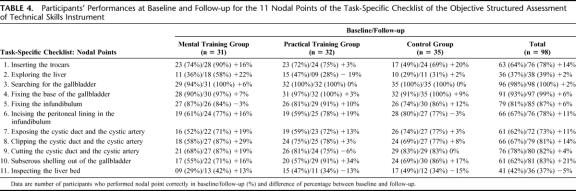
More detailed analysis of the results in Table 4 shows that most of the improvements in the mental training group occurred at nodal points 1 and 2 (16% and 22%) and from nodal point 6 to 11 (between 13% and 29%). In contrast, the control group improved most noticeably at nodal points 1, 5, and 10 (between 12% and 20%), while the practical group showed greatest improvement at nodal points 5, 6, 7, and 10 (between 10% and 34%).
TABLE 4. Participants' Performances at Baseline and Follow-up for the 11 Nodal Points of the Task-Specific Checklist of the Objective Structured Assessment of Technical Skills Instrument
Global Rating Scale
The improvement in the OSATS global rating scale seen between baseline and follow-up did not differ significantly between the groups (P = 0.701; Table 3). Results from paired Student t tests showed that no group improved significantly between baseline and follow-up (mental training group, P = 0.052; control group, P = 0.346; practical training group, P = 0.077). The improvements in the global rating scale subscales for the mental and practical training groups are, in contrast to the control group, nearly equivalent.
Questionnaire on Mental Training
The mental training group was generally well able to visualize performing the procedure (4.41 ± 0.66) and to imagine it from an inner perspective (4.29 ± 0.76; Table 1). Most trainees concentrated on the nodal points (3.74 ± 0.93). Their general opinion of mental training was favorable (4.00 ±0.78). They predicted that it could have a very positive long-term effect (4.12 ± 0.81) and believed that it was generalizable to other procedures (3.71 ± 1.06). Most of the surgeons wanted to use mental training in the future on their own (4.18 ± 0.67).
DISCUSSION
Mental training was effective in optimizing the performance of surgeons undergoing training in laparoscopic cholecystectomy. It achieved better outcomes than additional practical training or no additional training in the outcome variable, task-specific checklist. In the global rating scale and its subscales, the results for mental training were similar to those for practical training. In addition, mental training was regarded by trainees as a valuable tool in their education.
Baseline tests (Table 3) show that the mean task-specific checklist values for the 3 study groups differ, although not significantly. Since assignment to groups was randomized, these baseline differences may have happened by chance. However, the mean values at follow-up are more equal. Although this might be interpreted as a floor-effect, it is unlikely, since several surgeons reached scores of 9 points (baseline, 16; follow-up, 15), 10 points (baseline, 15; follow-up, 27), or 11 points (baseline, 8; follow-up, 8) in the task-specific checklist.
The study design meant that participants had contact with a number of people during study, which introduces the possibility of an experimenter effect. However, to avoid this bias, we were careful to adhere strictly to the principles of blinding. No course instructors, operation assistants, or test evaluators knew to which group participants had been assigned, but the mental trainers could not be blinded.
The quality of instruction given by the different mental trainers and their degree of engagement might have influenced the participants' performance and compliance, but we tried to minimize these effects by teaching the 6 mental trainers to provide exactly the same training. Five mental trainers carried out at least 4 each of the 31 training sessions (one trainer carried out only one session). In addition, participants were randomly assigned to their trainers. We think that these measures rule out the possibility of experimenter bias; the positive and significant effect of mental training is unlikely to be a result of any internal bias.
The varying results for the 2 OSATS scales are not unexpected (Table 3). Assuming that the task-specific checklist evaluates the more cognitive components of a surgical procedure and the global rating scale the more motor elements, our findings in surgery are comparable with previous reports in sports science. In the meta-analyses of Driskell et al2 and Feltz and Landers,3 mental training had a positive and significant effect on motor and cognitive tasks, but the greater the number of cognitive components, the stronger the effect. This means that the more mental processes and operations a task requires (for example, a labyrinth task), the more effective mental training becomes. Conversely, the more a task demands coordination, stamina, power or strength (for example, a balancing act, a marathon, or a weight-lifting task), the less effective mental training proves. Laparoscopic cholecystectomy, and any other surgical procedure, is an archetypal example of a task with high cognitive and motor components. Our study shows that mental training results in greater improvement in the cognitive aspects of a procedure, reflected in the task-specific checklist, than in the motor elements, scored by the global rating scale.
Improvements in the task-specific checklist seen in the mental training group (Table 4) were particularly noticeable at nodal points 1 and 2 (inserting the trocars and exploring the liver) and from nodal point 6 (incising the peritoneal lining of the infundibulum) to nodal point 11 (inspecting the liver bed). These nodal points, and particularly nodal points 6 to 11, are pivotal procedural steps in laparoscopic cholecystectomy. Thus, mental training resulted in improvements to crucially important stages. We think that these improvements can be attributed to the higher functional mental representation of the procedure provided by mental training. These positive and significant effects of mental training in surgery are not only comparable with results in studies of sports science, they are also seen in aviation14, and dentistry, both of which have demands similar to those of surgery.
This randomized controlled trial was carefully planned by an interdisciplinary group of experts. A randomized controlled trial delivers the highest quality of evidence. Nevertheless, there are factors that may have reduced the external validity or generalizability of our findings. First, our study took place during training courses on basic laparoscopic methods and not in the normal setting of a surgical clinic. Second, our participants were not very experienced in laparoscopic surgery in general. Finally, we focused on laparoscopic cholecystectomy using the Pelvi-Trainer simulator. Thus, we cannot generalize our results to well-trained surgeons in surgical clinics undertaking procedures on real patients. However, the study aimed to evaluate mental training as a tool in an international-standard course in surgical laparoscopy for surgeons in further education. Mental training should lead to an improvement in the skills which these courses attempt to instill: theoretical knowledge of and practical techniques in basic laparoscopy and procedures such as laparoscopic cholecystectomy using the Pelvi-Trainer. Our participants possessed already competency of performing a laparoscopic cholecystectomy when they entered the study. The task-specific checklist pretest result was 7.51 ± 2.37 points of maximally 11 for the 3 study groups. Thus, the main effect of mental training as applied in the present approach was not an accelerated acquisition of basic skills but rather an advance in careful performance.
We are unaware of any factors that could greatly affect the external validity of our findings for other basic laparoscopic procedures and tasks in other similar training courses. Further research is needed to determine whether mental training can also improve the performance of advanced surgeons operating on patients in surgical clinics.
Our results show that additional mental training is more effective than additional practical training or no additional training in a laparoscopic course for surgeons with limited experience. Mental training can be learned easily by surgeons in 2 hours and can be carried out independently from the mental trainer. This cognitive rehearsal is cheaper than practical training, especially when we consider the fact that a mental trainer is only necessary for the first mental training session. Once he has the skills, the surgeon can carry out mental training on his own. In addition, mental training can easily be transferred to other procedures without great expenditure. However, mental training cannot and should not replace practical training in laparoscopic training courses. Rather, mental and practical training should be combined, as happens in sports,2,3 and should be viewed as a relevant and valuable part of training.
ACKNOWLEDGMENTS
The authors thank our colleagues for their help:
Karim Gawad, MD (Department of Surgery, University Medical Center Hamburg-Eppendorf), Andreas Hackethal, MD (University Clinic for Gynaecology Giessen), Stefan Meierling, MD (General, Vascular and Thoracic Surgery, General Hospital of Hamburg-Harburg), Henning Niebuhr, MD (Department of General Surgery, Clinical Practice Hamburg-Bergedorf), Dörte Sievers, MD (Department of Surgery, General Hospital Hamburg-Barmbek), and Hilke Weichert, MD (Department of Surgery, General Hospital Hamburg-Altona) for carrying out mental training sessions.
Leo Adamek, MD, Stefan Saad, MD, Nedim Yuecel, MD (2nd Department of Surgery, University of Cologne), and Jürgen Treckmann, MD (Department of General Surgery and Transplantation, University Hospital Essen) for evaluating test videos.
Rolf Lefering, PhD (2nd Department of Surgery, University of Cologne) for supporting the statistical analysis and interpretation.
Thorsten Berg, MD (Ethicon Endo-Surgery Europe) for revising the manuscript.
Maike Aukstinnis, Silke Geider, Anja Kypke, Sabine Meier, Sabine Schroeder, Connyl Wuensche, and Claudia Wulff (Course instructors, European Surgical Institute) for carrying out the 10 training courses on basic laparoscopic methods.
Fevzi Cebe, MD, and Wido Wilke, MD (2nd Department of Surgery, University of Cologne) for conceptualizing of mental training in surgery and designing the study in the early beginning of the project.
Footnotes
Supported by grants from European Surgical Institute, Ethicon Endo-Surgery, Norderstedt, Germany.
Reprints: Marc Immenroth, PhD, Ethicon Endo-Surgery Europe; Hummelsbütteler Steindamm 71, 22851 Norderstedt, Germany. E-mail: M.Immenroth@gmx.de or mimmenro@ethde.jnj.com.
REFERENCES
- 1.Holden JG, Flach JM, Donchin Y. Perceptual-motor coordination in an endoscopic surgery simulation. Surg Endosc. 1999;13:127–132. [DOI] [PubMed] [Google Scholar]
- 2.Driskell J, Copper C, Moran A. Does mental practice enhance performance? J Appl Sport Psychol. 1994;79:481–492. [Google Scholar]
- 3.Feltz DL, Landers DM. The effects of mental practice on motor skill learning and performance: a meta-analysis. J Sport Psychol. 1983;5:25–57. [Google Scholar]
- 4.Immenroth M. Mental practice in surgery: some facts. In: Meyer G, Schildberg FW, eds. Complications in Minimal Invasive Surgery: Prevention, Detection, and Treatment. Heidelberg: Springer, In press.
- 5.Jänes A. Clipples Laparoscopic Cholecystectomy with Harmonic™. In: Immenroth M, Berg T, Bürger T & Brenner J, eds. Operation Primer (Volume 1). London: Euromed Communications, 2006. [Google Scholar]
- 6.Miller K. Laparoscopic Gastric Banding with the Swedish Adjustable Gastric Banding Band (SAGB Quick Close). In: Immenroth M, Berg T, Bürger T & Brenner J, eds. Operation Primer (Volume 3). London: Euromed Communications, 2006. [Google Scholar]
- 7.Eberspächer H, Immenroth M. Mental practice: an innovative theoretical and practical approach in surgery. In: Meyer G, Schildberg FW, eds. Complications in Minimal Invasive Surgery: Prevention, Detection, and Treatment. Heidelberg: Springer, In press.
- 8.Satava RM. Virtual reality, telesurgery, and the new world order of medicine. J Image Guid Surg. 1995;1:12–16. [DOI] [PubMed] [Google Scholar]
- 9.Martin JA, Regehr G, Reznick R, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997;84:273–278. [DOI] [PubMed] [Google Scholar]
- 10.Reznick R, Regehr G, MacRae H, et al. Testing technical skill via an innovative ‘Bench Station' examination. Am J Surg. 1997;173:226–230. [DOI] [PubMed] [Google Scholar]
- 11.Dupont WD, Plummer WD. Power and sample size calculations: a review and computer program. Control Clin Trials. 1990;11:116–128. [DOI] [PubMed] [Google Scholar]
- 12.Prather DC. Prompted mental practice as a flight simulator. J Appl Psychol. 1973;57:353–355. [Google Scholar]
- 13.Tokumaru O, Mizumoto C, Takada Y, et al. EEG activity of aviators during imagery flight training. Clin Neurophysiol. 2003;114:1926–1935. [DOI] [PubMed] [Google Scholar]
- 14.Welk A, Immenroth M, Eberspächer H, et al. Mental training in dental education. Eur J Dent Educ. 2003;7:96. [Google Scholar]