Abstract
Objective:
Review the evidence regarding methods to prevent wrong site operations and present a framework that healthcare organizations can use to evaluate whether they have reduced the probability of wrong site, wrong procedure, and wrong patient operations.
Summary Background Data:
Operations involving the wrong site, patient, and procedure continue despite national efforts by regulators and professional organizations. Little is known about effective policies to reduce these “never events,” and healthcare professional's knowledge or appropriate use of these policies to mitigate events.
Methods:
A literature review of the evidence was performed using PubMed and Google; key words used were wrong site surgery, wrong side surgery, wrong patient surgery, and wrong procedure surgery. The framework to evaluate safety includes assessing if a behaviorally specific policy or procedure exists, whether staff knows about the policy, and whether the policy is being used appropriately.
Results:
Higher-level policies or programs have been implemented by the American Academy of Orthopaedic Surgery, Joint Commission on Accreditation of Healthcare Organizations, Veteran's Health Administration, Canadian Orthopaedic, and the North American Spine Society Associations to reduce wrong site surgery. No scientific evidence is available to guide hospitals in evaluating whether they have an effective policy, and whether staff know of the policy and appropriately use the policy to prevent “never events.”
Conclusions:
There is limited evidence of behavioral interventions to reduce wrong site, patient, and surgical procedures. We have outlined a framework of measures that healthcare organizations can use to start evaluating whether they have reduced adverse events in operations.
The purpose of this study was to review the evidence for efforts aimed at reducing wrong site surgical procedures, and to propose a framework that healthcare organizations can use to evaluate whether their efforts are mitigating “never events.”
Despite a recent surge in patient safety awareness, preventable harm to surgical patients remains a problem. Wrong site, wrong procedure, and wrong person surgical procedures can be catastrophic to patients, healthcare professionals, and institutions.1 Following a sentinel event, a hospital typically conducts a root cause analysis to surface, and mitigate the hazards that caused the event. The result of this detailed investigation is usually a set of policies or programs intended to reduce or prevent these hazards from recurring. Nevertheless, the public, hospital leaders, and healthcare professionals often ask if these efforts have reduced the risk of similar events in the future.
Healthcare lacks a structured approach to evaluate whether safety efforts are reducing the risk of events that cannot be measured as rates.2 Most often, attention given to a sentinel event ends once the root cause analysis recommendations and ensuing policies are created.3 Few efforts have evaluated healthcare professionals' ongoing knowledge, or use of a policy to avert a similar future adverse event.
In addition, sentinel event investigations of wrong site, patient, or surgical procedures are typically covert because of liability concerns and a belief that these events should neither happen nor be known. As such, we lack national estimates of the true incidence of wrong site operations, and little is known about hospital efforts to mitigate these preventable events. Previous work4,5 has outlined a practical framework to investigate defects, such as sentinel events, by answering 4 questions. Little is known or published about the latter 2 questions: What will you do to reduce or prevent a similar future event?; and How do you know the probability for harm was reduced? (http://webmm.ahrq.gov).
The specific aims of this paper are to review the evidence regarding efforts to prevent wrong site surgical procedures, and present a framework that healthcare organizations can use to help evaluate whether they have reduced the risk of a patient suffering one of these sentinel events.
Defining “Never Events”
One of the National Quality Forum “Never Events” (www.qualityforum.org) and a focus of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is wrong site operations. This never event refers to operating on the incorrect side (eg, performing a right knee arthroscopy when the left knee arthroscopy was planned) or incorrect level (eg, operating on the incorrect vertebra).
Two additional never events, wrong procedure and wrong patient operations, are included in “wrong site surgery” since they share common root causes and prevention interventions. For example, performing a bilateral salpingo-oophorectomy when the surgical procedure was to only include a hysterectomy; or performing a nephrectomy on the incorrect patient when 2 patients share the same name, can have catastrophic repercussions. Finally, providers other than surgeons can be involved in a wrong site operation. Anesthesiologists have performed a nerve block contralateral to the intended surgical site;6 interventional radiologists could embolize the wrong renal artery, or place a stent in the wrong carotid artery.
Risk Factors for “Never Events”
Risk factors for wrong site operations have been previously described.7 Briefly, several surgeons involved in the same operation, or multiple procedures for 1 operation are known risk factors.8 In addition, time pressure, emergency surgery, abnormal patient anatomy, and morbid obesity are thought to be risk factors. Finally, an American Academy of Orthopaedic Surgeons’ (AAOS) task force reviewed malpractice insurance claims from 22 insurers and found that 68% were related to orthopedic surgery cases.9 Although this finding is higher than JCAHO's report of 41% wrong site orthopedic surgical cases,7 it highlights the risk associated with orthopedic surgery. Arthroscopy of the knee, foot, or ankle and management of a hip fracture or slipped capital femoral epiphysis were the most common wrong site procedures. The greater percentage of events in orthopedics is likely due to a higher volume of cases compared with other specialties, and more opportunities for lateralization errors. In addition, the AAOS has a long history of efforts to reduce wrong site operations that may prompt an increased willingness to report events.
An example is Meinberg and Stern's survey of 1050 hand surgeons regarding wrong site surgical procedures.10 A total of 217 surgeons (21%) admitted to operating on the wrong site at least once, and another 173 (16%) reported recognizing they had prepared the wrong side immediately prior to incision. The most common locations noted were the fingers, then the hands and wrists. This instrument did not specify a time period but instead asked whether the surgeon had a “wrong-site surgery.” As such, the authors could not estimate the incidence of wrong site operations, or the impact of the “Sign Your Site” campaign instituted by the AAOS.
Literature Review of Effective Interventions
This literature review was conducted to identify effective interventions to prevent wrong site surgical procedures.
Study Selection Criteria
We sought to identify and review all original research that implemented novel techniques aimed at prevention of wrong site surgical procedures.
Citation Search Strategy
Studies were identified by searching PubMed (1965–2005), google.com, and bibliographic lists from literature pulled through these search strategies (last searched November 2005). The only MeSH heading related to wrong site, sided procedures, Medical Errors [N02.421.450] was far too broad. Thus, search terms used were wrong site surgery, wrong side surgery, wrong patient surgery, and wrong procedure surgery.
Study Selection
Seventy-six citations were identified through our electronic database search as referencing one of the key terms. No additional citations were identified in bibliographic lists of publications pulled for review. One author (R.K.M.) reviewed the abstracts of each citation and excluded 55. Reasons for exclusion were: non-English (n = 12), news article or announcement (n = 8), editorial-related (n = 14), quizzes (n = 2), and key term mentioned but not the publication's focus (n = 19). The remaining 21 publications were retrieved and independently reviewed by 2 authors (R.K.M., Y.D.) to confirm eligibility. A third reviewer (M.A.M.) resolved any discrepancies. Four peer-reviewed publications, one technical report, one sentinel event alert, and 2 websites (JCAHO and VHA) informed this analysis. There was exceedingly limited empiric evidence regarding how to prevent wrong site operations. None of the studies reviewed presented quantitative evaluations of strategies to prevent wrong site operations.
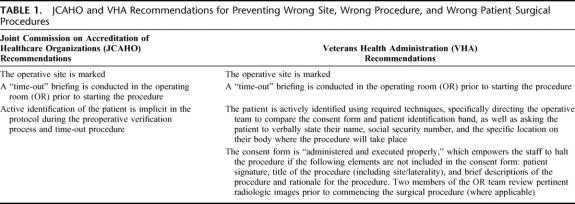
In the AAOS 1998 Task Force report, it was stated that the “literature concerning prevention of wrong-site surgery is virtually nonexistent.” This same disappointing statement holds true today. We found that the majority of evidence on preventing such medical errors remains at the level of expert opinion and consensus statements. The most notable consensus statement is JCAHO's “Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery,” which outlines 3 steps to reduce the risk of wrong site surgical procedures (Table 1).
TABLE 1. JCAHO and VHA Recommendations for Preventing Wrong Site, Wrong Procedure, and Wrong Patient Surgical Procedures
Joint Commission on Accreditation of Healthcare Organizations
Preoperative Verification
The first step in the JCAHO protocol is the “preoperative verification process.” A case from WebM&M describes a patient undergoing a hemivulvectomy in which a preoperative verification was not done (http://webmm.ahrq.gov/case.aspx?caseID=33). The resident physician assisting on the case prepped the patient's correct side, but the attending surgeon remembered performing the biopsy and was confident, but wrong, in his decision to operate on the opposite side. A preoperative verification is an information gathering process that involves real-time access to the patient's medical records, consent for the procedure, and pertinent laboratory, pathology, or radiologic results in the operating room (OR). If a disagreement between providers should occur,11 as illustrated above, a quick review of pertinent medical information can quickly resolve the discrepancy.
Although a preoperative verification is important and sensible, its utility is likely contingent upon healthcare organizations creating a specific protocol to define this process. Guidelines that involve clear recommendations for specific behaviors will more likely be followed than general or ambiguous recommendations. For example, a hospital could create a checklist to define what documents are needed to appropriately complete a preoperative verification. In the absence of such a checklist or behavior-specific protocol, the impact of this recommendation will likely be minimal.
Site Marking
The second step is marking the “correct site,” which involves lateral (right/left) distinction, multiple structures (fingers, toes), or multiple levels (spine). JCAHO states the marking should be clearly observable after the surgical preparation and draping are completed. Site marking will likely have high impact in preventing wrong site operations because it is a well-defined behavior. The most common marking is the surgeons’ initials or a “YES.” Nevertheless, one method for marking the operative site must be agreed upon by all healthcare organizations and clinicians to decrease confusion regarding whether the mark means operate or do not operate here. A standard protocol is needed.5
The surgical site is marked before entering the OR, either during the preoperative evaluation office visit or in a preoperative holding area. Marking the site should be done while the patient is awake, which allows the surgeon to confirm the appropriate operative site with the patient. Ink that remains visible after the surgical preparation should be used. Fear that marking may jeopardize sterile preparation for surgery is unfounded,12 although adhesive site markers could jeopardize a sterile field and should not be used. The responsible surgeon or an assistant surgeon directly involved in the patient's care should mark the site. Marking may be omitted in single organ cases (eg, cardiac surgical procedures, most gastrointestinal procedures).
Time-out
The last step involves a “time-out,” which is an independent check to potentially identify and correct errors. This intentional pause before incision is a communication tool, and final safety check between the surgical, nursing, and anesthesia care teams. The time-out should occur immediately prior to initiating the procedure and must verify, at a minimum, the correct: patient name and medical record number (or social security number, date of birth, or other identifier), procedure, site and laterality (including visual verification), patient position, and implants or any special equipment necessary for the operation.
JCAHO recommends that a time-out be conducted in a “fail-safe” mode, whereby no procedure is started until all questions and concerns from all individuals involved are addressed. This appears wise. In most sentinel events, someone knew something was wrong but either did not speak up or spoke up but was ignored. Teams are more likely to make wise decisions when they have diverse and independent input.13
Veteran's Health Administration
The Veteran's Health Administration (VHA) expanded on JCAHO's Universal Protocol in their directive entitled, “Ensuring Correct Surgery and Invasive Procedures.”14 Briefly, the VHA provides a detailed set of behaviors to implement JCAHO's “preoperative verification” and “time-out” processes, which likely increases the probability that these behaviors will be enacted.
First, the VHA explicitly directs the operative team to do the following during the preoperative verification and time-out: compare the consent form and patient identification band, and ask the patient to verbally state their name, social security number, and the specific location on their body where the procedure should take place. In addition, the staff member who carries out the active identification stays with the patient until they are inside the OR.
Second, the directive calls for “appropriate execution/verification” of the consent form. This verification empowers staff to halt the procedure if the patient's (or legally authorized designee's) signature, title of the procedure (including site/laterality), and/or a brief description and rationale for the procedure are missing from the form. Finally, when imaging data are necessary to determine or confirm the operative site, this directive requires that two members of the OR team review pertinent radiologic images and agree on the operative site.
In addition to the mandated directives, the VHA offers suggestions to further safeguard patients. Call the patient 24 to 48 hours before the procedure to confirm the surgical site. Audit cases the evening prior or the morning of the operation to check the consent form against the OR schedule. Ask patients to touch the site during the verification process. This suggestion removes confusion on the patient's part over right and left, or counting of digits during a verbal verification. For example, operating on the “2nd digit” of the right hand could be misinterpreted by the patient to mean the middle finger if they fail to count their thumb. Finally, have teams write the patient's name, planned procedure and site, and details regarding use of any implants on a dry erase board in the OR. While these ideas are not foolproof, each provides a redundant and independent check to increase the likelihood of mitigating errors when used adjunctively with the 3 JCAHO steps.
The VHA recommendations are laudable because they define specific behaviors. However, the increased complexity of these recommendations may reduce their efficacy and potentially lead to a culture of noncompliance. As such, a balance must be achieved between feasibility and scientific rigor, and between central mandates and local wisdom. Efforts to find this balance must include input from the frontline staff who will implement the interventions so they: understand why the policy is important, surface barriers to implementation, identify teams who are doing it well, and surface potential hazards introduced by the practice.
Professional Medical Organizations
Over 50 professional medical organizations have joined efforts to reduce wrong site surgical procedures, with many endorsing the JCAHO policy. The Canadian Orthopaedic Association (http://www.coa-aco.org) implemented a 2-year educational program in 1994 called “operate through your initials.” At the start of this program, 7% of all settlements related to orthopaedic surgery in Canada included wrong site procedures. A similar program, called “Sign Your Site” (www5.aaos.org/wrong/setup.cfm) was adopted by the American Academy of Orthopaedic Surgeons. Finally, the North American Spine Society developed the Sign, Mark, and x-ray (SMaX) campaign (http://www.spine.org/forms/smaxchecklist.pdf). In addition to marking the incision area, SMaX requires a radiograph of the presumed spinal level for site verification before commencing with laminectomy, foraminotomy, and/or instrumentation. Like many of the other interventions, the radiograph is a protective “independent check,” a concept well rooted in safety science.15
At the Johns Hopkins Hospital, an OR briefing tool is used as part of an expanded “time-out.”16 In addition to confirming correct patient, procedure, and operative site, this tool prompts for additional dialogue between the anesthesia care team, nursing staff, and surgical team (Fig. 1). The timing of a briefing is specialty specific. For example, neurosurgery initiates a time-out after final positioning of the patient, but before drapes are placed. Team member names and roles are introduced and also written on a “white board” in each OR. The operative plan, required equipment, and any contingency plans are reviewed with all participants. In an attempt to surface and mitigate hazards, the surgeon is encouraged to discuss estimated blood loss, the need for cultures or biopsies, and any anticipated complications or risks. The nursing team confirms the availability of instrumentation and supplies and discusses any family issues. The anesthesiologist and/or certified registered nurse anesthetist (CRNA) review significant patient comorbidities, risks for complications, and anesthetic management (eg, antibiotic administration, patient allergies, vascular access, blood availability, etc). The briefing is concluded with open input to a question like, “If something were to go wrong, what would it likely be?”
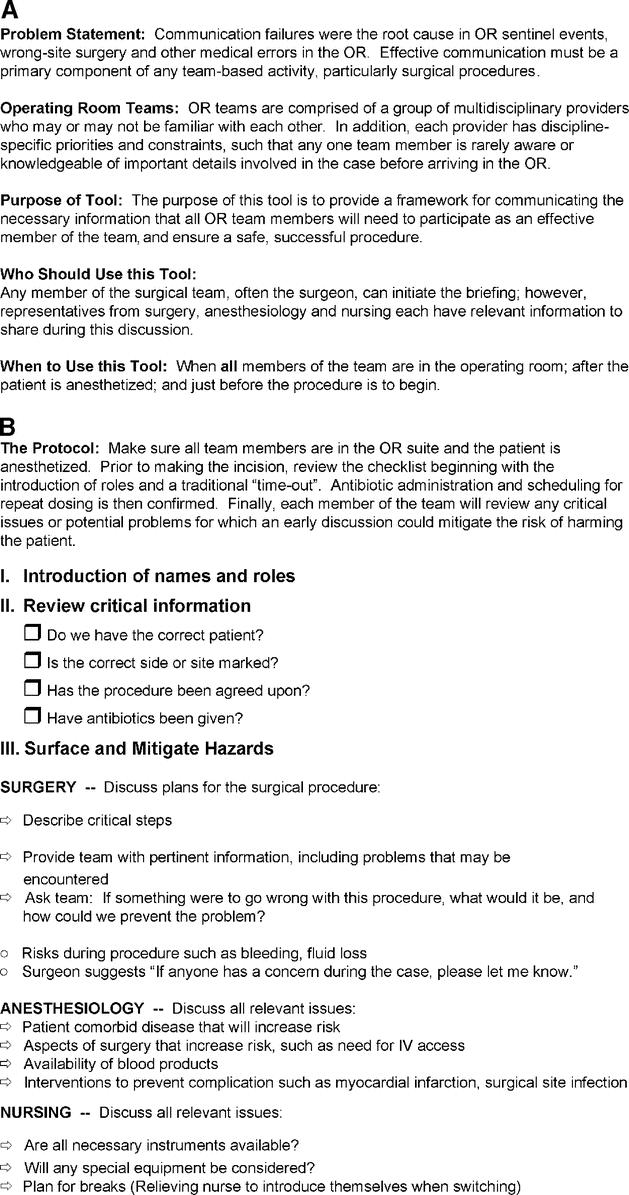
FIGURE 1. A, The instruction sheet that explains to the user, in this case operating room personnel, why a briefing is important, who should use a briefing, and when to use a briefing. Included on this page is a definition of operating room teams. B, The operating room briefing checklist to help guide OR personnel in conducting an appropriate briefing.
State-of-the-Art Technology
Technology such as radiofrequency identification (RFID) could help reduce wrong site operations. The Food and Drug Administration approved use of an RFID tag called a SurgiChip in November 2004 (SurgiChip, Inc., Palm Beach Gardens, FL). The SurgiChip is a temporary tag placed close to the surgical site.17 Such tags can hold medical history, prescribed medications, allergies, and other pertinent information. Data are read remotely using an RFID scanner (reading device). Although conceptually appealing, we found few examples of how this has been broadly applied.
A less invasive technology is a procedure specific wristband with an embedded microchip that sets off a sensor if the chip remains activated (Smart WristBand, CheckSite Medical, St. Louis, MO). The sensor is typically placed in the hallway between the preoperative area and the OR suites. To deactivate the chip, the surgeon must sign the site with the marking pen packaged with the wristband, remove the label affixed to the pen, and place it over the microchip. Both the RFID scanner and the Smart WristBand are relatively early in their development. The efficacy and cost-effectiveness of these technologies have yet to be assessed. Nevertheless, while technology may protect against some hazards, it will likely introduce new hazards.18,19
Framework to Evaluate Safety
How Do We Know We Are Safer?
Fortunately, events such as wrong site operations are too rare to measure as rates. Indeed, the impression may be that the incidence is increasing because reporting is more vigilant than in the past. Nevertheless, healthcare organizations need a method to evaluate the effectiveness of interventions in reducing the probability that another patient will be harmed. There are generally 3 things we can measure for safety events that cannot be calculated as rates. First, we can ask whether a behaviorally specific policy or procedure exists. Second, we can measure staff's knowledge of the policy or procedure. Finally, we can assess whether the policy or procedure is being used appropriately—generally through a direct observation audit.
Multiple methods of measurement exist for wrong site operations, each with particular strengths and weaknesses. As with any measure, we must balance the scientific rigor of the measure with the resources necessary to produce the data. Perhaps the simplest way to measure risk for wrong site surgical procedures is to evaluate whether healthcare organizations follow JCAHO recommendations and, like the VHA, have explicitly defined processes for the preoperative verification and time-out. Existence of a policy is generally easier to measure, but presence may not correlate with its use. As such, hospitals may have a false sense of security if they only evaluate whether they have a wrong site surgical procedure policy.
Evaluating healthcare provider's knowledge of the policy is more difficult. In most hospitals, an infrastructure to gauge and monitor healthcare professional's, especially physician's, knowledge of a policy is underdeveloped. Nevertheless, professional societies or hospitals could develop a simple process to test healthcare professionals’ knowledge of policies to prevent wrong site operations to better ensure all perioperative providers are competent.
Perhaps the most valid measure is to ensure that the policy is being used appropriately. If the policy involves communication among multiple providers or teams, the most valid but resource-intensive method of measurement is direct observation. If a procedure involves just one provider, compliance can be assessed by querying the medical record. For example, time-out procedures involve communication among the surgical, nursing, and anesthesia care teams. A note in the medical record would not evaluate whether communication was effective during the time-out. Similarly, when a procedure has more than one dimension, simply asking a categorical yes/no response can provide positive responses for incompletely performed tasks. In addition, some operations involve multiple incisions and therefore may require more than a standardized time-out. Measurement tools should be designed to evaluate individual behaviors and provide feedback to the care teams. Moreover, direct observation is an opportunity to surface hazards introduced by the policy and to revise the policy based on feedback from front-line staff.
The need to evaluate whether policies and procedures are being appropriately implemented is important. JCAHO has received reports of wrong site operations occurring, even though a time-out was reportedly done. It could be that the time-out was done and the error could not be prevented, or the team went through the motions but did not execute an effective time-out. Unfortunately, the latter is not surprising given the low incidence of this type of error, and a current system that is devoid of independent checks (ie, checks are done collectively, thereby encoding the error). As such, directly observing the process could raise clinical provider's awareness regarding the importance of briefings in the face of rare wrong site operations.
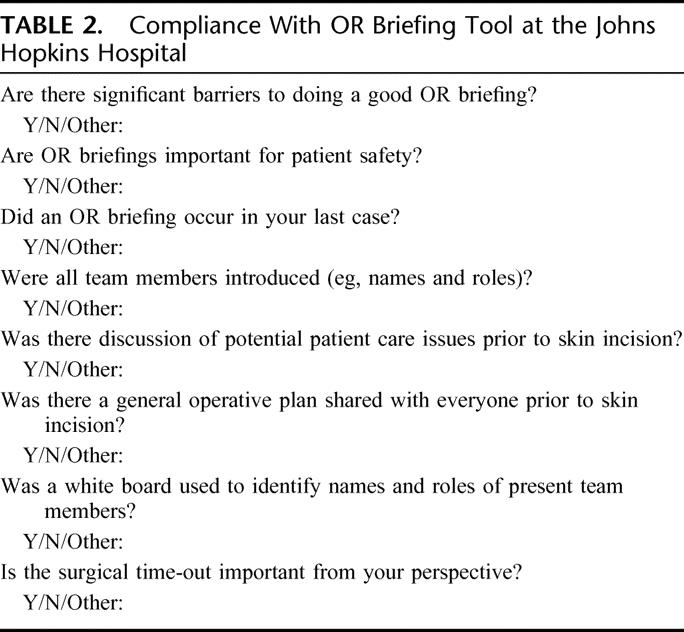
We developed and implemented a compliance tool to evaluate whether briefings and time-outs were conducted appropriately in the OR (Table 2). We also queried staff attitudes and beliefs regarding OR briefings to better understand the barriers, and further refine the process for an effective briefing. Since it takes significantly greater resources to measure the use rather than the existence of a policy, healthcare organizations will need to prioritize what they measure.
TABLE 2. Compliance With OR Briefing Tool at the Johns Hopkins Hospital
Recommendations
Our recommendations for preventing wrong site surgical procedures are informed by patient safety theory and the existing evidence. This theory includes creating a culture of safety, standardizing processes, creating independent checks for key processes, and learning from mistakes.3,20 We have divided these recommendations into prevention interventions and measures to evaluate whether these interventions are mitigating events.
Interventions
Implement JCAHO recommendations.
Create a specific and detailed preoperative verification process and time-out that includes a checklist with explicit behaviors; model after Veterans Health Administration.
Implement OR briefings and debriefings.
Measures
Evaluate the presence of a detailed policy or procedure for preoperative verification.
Evaluate staff knowledge of the process for preoperative verification and time-out.
Evaluate appropriate use of the time-out through direct observation using the compliance instrument (Table 2).
CONCLUSION
Wrong site operations are preventable adverse events that often result in patient harm. While recent evidence suggests that wrong site operations are rare and injuries minimal, incidence of such catastrophic events can likely be significantly reduced.21 We summarized the evidence regarding strategies to reduce the risk for wrong site surgical procedures, and we presented a framework healthcare organizations can use to start evaluating whether they are reducing this adverse event. Although the evidence is limited, using the recommendations informed by patient safety theory can provide guidance in designing interventions. Indeed, the recent study by Kwaan et al of malpractice claims alone found that two thirds of wrong site operations could have been prevented by a site-verification protocol.21 We hope this manuscript spurs further research to develop standardized interventions and measures to help eliminate wrong site surgical procedures.
ACKNOWLEDGMENTS
The authors thank Christine G. Holzmueller for her editing expertise.
Footnotes
Reprints will not be available. Correspondence: Martin Makary, MD, MPH, 1909 Thames Street, 2nd floor, Baltimore, MD 21231. E-mail: mmakary1@jhmi.edu.
REFERENCES
- 1.Makary MA, Sexton JB, Freischlag JA, et al. Patient safety in surgery. Ann Surg. 2006;243:628–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: an elusive target. JAMA. 2006;296:696–699. [DOI] [PubMed] [Google Scholar]
- 3.Pronovost PJ, Holzmueller CG, Martinez E, et al. A practical tool to learn from defects in patient care. Jt Comm J Qual Saf. 2006;32:102–108. [DOI] [PubMed] [Google Scholar]
- 4.Pronovost PJ, Holzmueller CG, Sexton JB, et al. How will we know patients are safer? An organization-wide approach to measuring and improving patient safety. Crit Care Med. 2006;34:1988–1995. [DOI] [PubMed] [Google Scholar]
- 5.Pronovost PJ, Berenholtz SM, Goeschel CA, et al. Creating high reliability in healthcare organizations. Health Serv Res. 2006;41:1599–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edmonds CR, Liguori GA, Stanton MA. Two cases of a wrong-site peripheral nerve block and a process to prevent this complication. Reg Anesth Pain Med. 2005;30:99–103. [DOI] [PubMed] [Google Scholar]
- 7.Joint Commission on Accreditation of Healthcare Organizations. Sentinel Event Alert. A follow-up review of wrong site surgery. Report No. 24;2001. Available at: http://www.jcaho.org. [PubMed]
- 8.Wachter RM, McDonald KM. Making health care safer: a critical analysis of patient safety practices [Report Evidence Report/Technology Assessment No. 43]. Rockville, MD: Agency for Healthcare Research and Quality, 2001. [PMC free article] [PubMed] [Google Scholar]
- 9.Cowell HR. Wrong-site surgery. J Bone Joint Surg Am. 1998;80:463. [DOI] [PubMed] [Google Scholar]
- 10.Meinberg RG, Stern PJ. Incidence of wrong-site surgery among hand surgeons. J Bone Joint Surg Am. 2003;85:193–197. [DOI] [PubMed] [Google Scholar]
- 11.Sexton JB, Makary MA, Tersigni AR, et al. Teamwork in the operating room: frontline perspectives among hospitals and operating room personnel. Anesthesiology. 2006;105:877–884. [DOI] [PubMed] [Google Scholar]
- 12.Cronin G, Ringus V, Sigle G, et al. Sterility of surgical site marking. J Bone Joint Surg Am. 2005;87:2193–2195. [DOI] [PubMed] [Google Scholar]
- 13.Surowiecki J. The Wisdom of Crowds: Why the Many Are Smarter Than the Few and How Collective Wisdom Shapes Business, Economics, Societies and Nations. New York: Random House, 2004. [Google Scholar]
- 14.Veterans Health Administration. Ensuring correct surgery and invasive procedures. VHA Directive 2004–28. July 25, 2004. Available at: http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=1106. Accessed September 14, 2006.
- 15.Pronovost P, Berenholtz S, Dorman T, et al. Improving communication in the ICU using daily goals. J Crit Care. 2003;18:71–75. [DOI] [PubMed] [Google Scholar]
- 16.Makary MA, Holzmueller CG, Thompson DA, et al. Operating room briefings: working on the same page. Jt Comm J Qual Saf. 2006;32:351–355. [DOI] [PubMed] [Google Scholar]
- 17.Food and Drug Administration. FDA clears new surgical marker; Uses RFID to protect patients. FDA Talk Paper [serial online]. November 19, 2004; Available from: http://www.fda.gov/bbs/topics/ANSWERS/2004/ANS01326.html. Accessed April 11, 2006.
- 18.Han Y, Carcillo J, Venkataraman S, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;116:1506–1512. [DOI] [PubMed] [Google Scholar]
- 19.McDonald CJ. Computerization can create safety hazards: a bar-coding near miss. Ann Intern Med. 2006;144:510–516. [DOI] [PubMed] [Google Scholar]
- 20.Pronovost PJ, Thompson DA, Holzmueller CG, et al. Defining and measuring patient safety. Crit Care Clin. 2005;21:1–19. [DOI] [PubMed] [Google Scholar]
- 21.Kwaan MR, Studdert DM, Zinner MJ, et al. Incidence, patterns, and prevention of wrong-site surgery. Arch Surg. 2006;141:353–358. [DOI] [PubMed] [Google Scholar]