Abstract
Objective:
To investigate the pattern of nodal metastasis, morbidity, recurrence rates of papillary thyroid carcinoma (PTC), and parathyroid hormone (PTH) responses following neck dissection (ND) plus total thyroidectomy (TT).
Summary Background Data:
While hypoparathyroidism develops after TT plus ND, little is known of postoperative PTH response.
Methods:
Of 155 PTC patients, 82 underwent TT plus bilateral central ND with/without lateral ND, while 73 underwent TT alone. The nodal metastasis pattern was determined and the recurrence, morbidity, and postoperative levels of serum calcium and PTH were compared between 2 groups.
Results:
Of the 82 node dissection patients, metastatic nodes were present in the central neck of 51 (62.2%) and the lateral neck of 21 (25.6%) patients, most frequently in the ipsilateral and pretracheal central nodes and lateral jugular nodes. Four regional recurrences (2.6%) were found in 3 patients of the no node dissection group and one of the node dissection group (P = 0.37) during the follow-up lasting a mean 52 months. Overall morbidity and hypocalcemia was higher in the node dissection group than the no node dissection group (41 of 82, 50%; vs. 9 of 73, 12.3%; P < 0.001; 25 of 82, 30.5%; vs. 7 of 73, 9.6%; P = 0.001). Serum PTH levels significantly decreased immediately postoperatively in the node dissection group and remained low for several weeks thereafter.
Conclusions:
Serum PTH levels were significantly reduced following ND in PTC patients. Our data suggest that, when performing therapeutic ND plus TT, particular effort should be made to preserve the parathyroid glands and to monitor their function.
The study examined 155 papillary thyroid carcinoma patients treated by either total thyroidectomy plus neck dissection (n = 82) or total thyroidectomy alone (n = 73). Overall, the nodal metastasis rate was high (53 of 82, 64.6%), but the recurrence rate was low (4 of 155, 2.6%). Hypocalcemia occurred far more commonly in node dissection than no node dissection patients (25 of 82, 30.5%; vs. 7 of 73, 9.6%; P = 0.001). These data indicate that parathyroid function monitoring is required during or after total thyroidectomy plus neck dissection surgery.
Controversy surrounds the prognostic relevance of lymph node metastasis in differentiated papillary thyroid carcinoma (PTC) cases.1–5 Subclinical lymph node metastasis is found in a high proportion of PTC patients at the time of surgery and in pathology specimens.6,7 Although lymph node metastasis has no major impact on survival,8–10 it has been suggested that the presence of nodal involvement was commonly associated with extrathyroidal invasion and the increased rate of local recurrence and distant metastasis.2,3,5,11
There remains debate as to whether lymph node dissection is indicated for all patients with PTC. Therapeutic neck dissection is well accepted as part of the surgical strategy for treating macroscopic nodal metastasis from PTC. However, elective neck dissection remains controversial due to the lack of clear data regarding its survival benefit and complications associated with the procedure.12 Recent reports indicate thyroidectomy plus nodal neck dissection resulted in 3% to 6% of PTC patients suffering permanent hypoparathyroidism and transient vocal cord paralysis.12–14 No reports to date have closely analyzed postoperative hypocalcemia and parathyroid hormone levels after thyroidectomy plus node dissection.
The present study investigated the pattern of nodal metastasis, morbidity and recurrence rates after bilateral central neck dissection (CND) with or without lateral neck dissection (LND) in a consecutive series of patients who underwent a total thyroidectomy for PTC diagnosed preoperatively. In addition, serum calcium and parathyroid hormone (PTH) levels were compared between patients undergoing thyroidectomy plus neck node dissection and those undergoing thyroidectomy alone.
PATIENTS AND METHODS
Patient Eligibility and Study Design
A total of 155 new patients who underwent a total thyroidectomy for PTC between 2001 and 2004 were reviewed. No patient had a history of thyroid or neck surgery. Patients undergoing a unilateral lobectomy, subtotal, or completion thyroidectomy were excluded, and only patients undergoing a total thyroidectomy were enrolled. Patient information regarding age, gender, pathology, surgical procedure, number of parathyroid glands preserved, or autotransplanted and presence of hypocalcemic symptoms were analyzed. All cases were preoperatively diagnosed as PTC following fine-needle aspiration, including 9 cases suspicious of PTC. The study involved 25 men and 130 women, with a mean age at initial treatment of 47 years (range, 18–75 years).
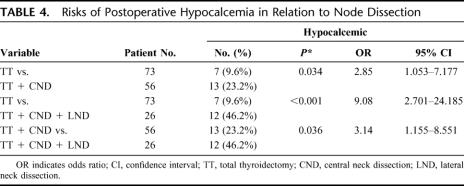
Patients were divided into 2 groups according to CND. Of the 155 patients, 82 underwent a total thyroidectomy plus bilateral CND, while 73 underwent a total thyroidectomy alone. Patient characteristics are summarized in Table 1. The gender, age, and MACIS scores were similar between the 2 groups. In 42 (27.1%) patients, lymph nodes were palpated in the central (n = 38, 24.5%) or lateral neck (n = 26, 16.8%) prior to or during surgery. Of the neck dissection group, 42 patients with macroscopically involved nodes underwent a total thyroidectomy and therapeutic neck dissection. Of them, 26 patients with palpable lateral nodes underwent a total thyroidectomy and neck dissection involving the bilateral central compartment as well as the affected lateral neck. Sixteen patients with palpable nodes only in the central compartment underwent a total thyroidectomy and bilateral CND. The remaining 40 patients underwent a total thyroidectomy and prophylactic CND despite no evidence of palpable cervical nodes. Seventy-three patients of the no neck dissection group presenting no palpable nodes underwent a total thyroidectomy alone. Whether the prophylactic CND was performed or not in 113 patients with no palpable cervical nodes was randomly assigned. The difference in the number of patients between the with and the without prophylactic CND resulted from considering the number of patients who underwent therapeutic neck dissection for comparing the morbidity of neck dissection among groups.
TABLE 1. Patient Demographics and Clinical Characteristics
Because of direct tumor invasion, 4 patients underwent a tracheal sleeve resection and 5 patients had their recurrent laryngeal nerve intentionally sectioned. The parathyroid status of each patient was determined after total thyroidectomy, and devascularized parathyroid glands, confirmed by frozen-section histologic analysis, were transplanted into the sternocleidomastoid muscle. Patient symptoms, serum calcium, and parathyroid hormone (PTH) levels were regularly monitored after surgery. Postoperative complications, pathology, and recurrence were compared between groups. Pathology of the primary tumor, frequency, and the pattern of lymph node metastasis were analyzed in the node dissection group. The study was approved by the Institutional Review Board of the Chungnam National University Hospital, including randomization.
Node Dissection
CND was carried out in a conventional manner, not using microdissection methods.15 Node clearance was performed cranially to both superior thyroid arteries and the pyramidal lobe, caudally to the innominate vein, laterally to the carotid sheaths, and dorsally to the prevertebral fascia.7 The thymus was commonly preserved by separation from the central nodes. The central compartment was divided into 4 node sites: pretrachea, ipsilateral and contralateral paratracheal, and superior mediastinal below the sternal notch. Particular attention was given to identifying the parathyroid glands, and parathyroid autotransplantation was carried out as required, not on principle. A modified radical neck dissection was performed on patients with clinically positive lateral neck nodes. The lateral compartment was delimited superiorly to the hypoglossal nerve, inferiorly to the subclavian vein, and laterally to the trapezius muscle.
Postoperative Hypocalcemia and Measurement of Serum Calcium and PTH Levels
A preoperative blood sample was drawn on the morning of surgery for baseline measurement of serum ionized calcium, total calcium and intact PTH levels. Postoperatively, serum calcium concentrations were obtained at 1, 8, 24, 48, and 72 hours after surgery. The reference ranges for ionized and total calcium were 1.2 to 1.38 mmol/L and 8.5 to 10.5 mg/dL, respectively. Serum calcium levels were corrected for measured abnormal serum albumin levels.16 Serum intact PTH levels were measured using a standard ELSA-PTH immunoradiometric assay (Cis Bio International, Gif-Sur-Yvette, Cedex, France) at 1 hour, and 1 and 3 days after surgery. The manufacturer's normal range was 8 to 76 pg/mL, the detection limit of the assay was 0.7 pg/mL, and the intra-assay and interassay coefficients of variation were below 7% at PTH concentrations between 6 and 95 pg/mL.
All patients were clinically evaluated for signs and symptoms of hypocalcemia. Hypocalcemia was defined as a symptomatic patient with an ionized calcium level <1.0 mmol/L during the hospital stay or at any time after discharge from hospital.17 Patients who developed hypocalcemia were administered oral calcium and vitamin D replacements. Intravenous calcium gluconate was administered for significant symptoms. The study protocol required hospitalization of all patients for a minimum of 3 days after surgery for blood tests. All patients were followed-up at 1 week and 1, 3, and 6 months after surgery, and serum ionized, total calcium and intact PTH levels were measured.
Statistical Analysis
SPSS 12.0 for windows (SPSS Inc., Chicago, IL) was used for statistical analysis. Student t test was used when comparing continuous variables between groups; paired t test was used for comparison of paired samples; the χ2 test was used to investigate differences between categorical data. Differences were considered significant when P < 0.05.
RESULTS
Pathology Examination
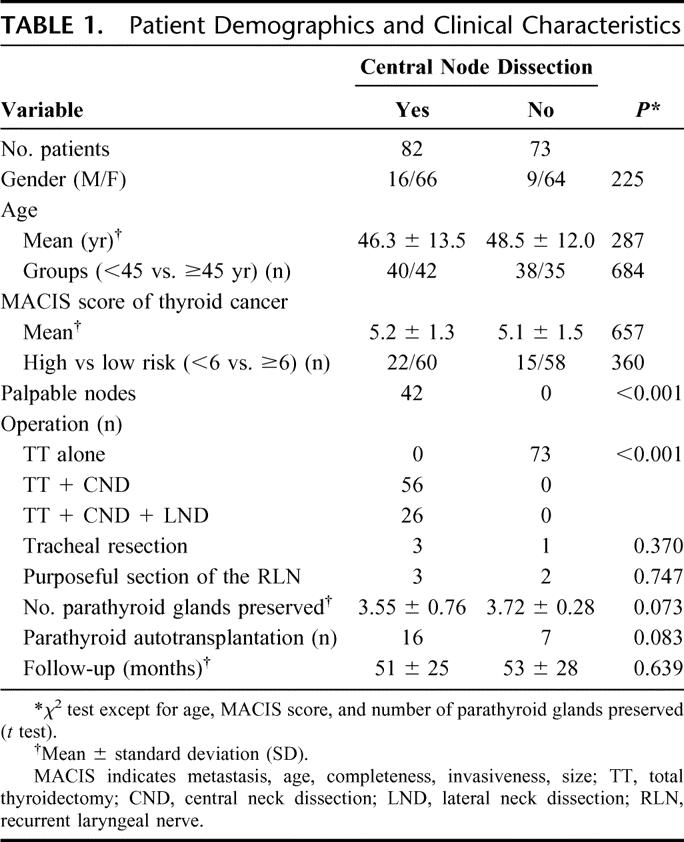
The mean size of the primary thyroid tumor was 24 mm (range, 2–75 mm) (Table 2). The number of patients with primary tumor size less than 10 mm did not differ between the with and the without node dissection groups (8 of 82, 9.8%; vs. 11 of 73, 14.7%; P = 0.446). They were preoperatively diagnosed as micropapillary carcinomas by ultrasound-guided fine needle aspiration cytology and one patient with 2-mm-sized carcinoma presented lateral nodal metastasis. Multifocality and extracapsular invasion were found in 28 (18.1%) and 67 (43.2%) patients, respectively. The mean size and frequency of multifocality and extracapsular invasion were similar for both with and without node dissection groups. Pathology showed metastatic nodes in the central neck of 51 (62.2%) and the lateral neck of 21 (25.6%) node dissection group patients. Rate of nodal metastasis was higher in patients with extracapsular invasion than in patients with no invasion (29 of 45, 64.4%; vs. 10 of 37, 27.0%; P = 0.001). All but 1 patient with lateral nodal metastasis had extracapsular invasion of primary tumor. There was a mean 5.6 metastatic central nodes, regardless of the size of the primary tumor. The frequency of lymph node metastasis in different sites varied.
TABLE 2. Comparison of Pathology Data Among Different Groups
The node dissection group was analyzed according to whether the primary tumor was located in the lobe (n = 70) or isthmus (n = 12). Forty-seven of the 70 (67.1%) lobe-arising tumors had central node metastases, which involved the ipsilateral paratracheal (62.8%), pretracheal (32.8%), superior mediastinal (20.0%), and contralateral (13.4%) sites. Only 4 of 12 (33.3%) isthmus-origin tumors showed central node metastases, and these involved the pretracheal (25.0%), paratracheal (16.7%), and superior mediastinal (8.3%) sites. In the lateral compartment, these involved the ipsilateral lower (21.9%), upper (20.7%), mid (18.3%), and posterior (1.2%) sites. Bilateral neck nodes were observed in 3 patients (3.7%), and lateral skip metastasis (no positive central nodes) was observed in 2 patients (2.4%). Five of 26 patients (6.1%) with palpable lateral neck nodes were pathology-negative.
Parathyroid glands were found in the thyroid or central nodal specimens of 16 patients (10.3%). The mean number of parathyroid glands incidentally removed was 1.2, and the frequency of incidental parathyroidectomy did not differ between with and without node dissection groups (P = 0.180).
Postoperative Evaluation
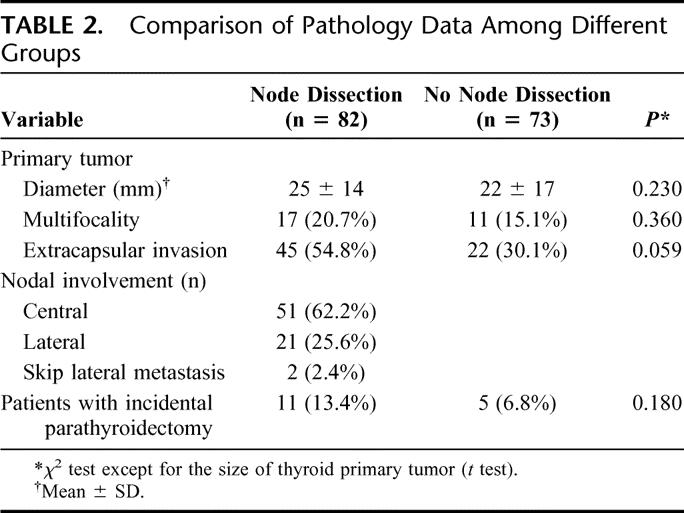
The incidence of postoperative complications was compared between the with and without node dissection groups (Table 3). The overall complication rate was higher in the node dissection group (50.0%) than in the no node dissection group (12.3%) (P < 0.001). Thirty-two of 155 patients (20.6%) developed postoperative hypocalcemia requiring calcium supplements. Analysis of these data showed more node dissection group patients (25 patients, 30.5%) developed postoperative hypocalcemia than no node dissection patients (7 patients, 9.6%) (P = 0.001). Four (4.9%) node dissection group patients had permanent hypocalcemia requiring calcium supplements one year after surgery.
TABLE 3. Comparison of Postoperative Complication Rates Between Different Groups
Vocal cord paralysis occurred in 9 patients (5.8%). Five patients underwent intentional section of the unilateral recurrent laryngeal nerve due to direct tumor invasion, and all had permanent paralysis of the affected vocal cord. However, the vocal quality in these patients was well preserved as they underwent arytenoids adduction (n = 3) and thyroplasty type 1 (n = 2) voice surgery in the affected side immediately after thyroidectomy. Two patients (1.3%) required resurgery due to immediate postoperative bleeding. Chyle leakage occurred in 3 (3.6%) neck dissection patients and was solved with conservative management. While 9 (34.6%) modified neck dissection patients complained of longstanding pain in the operated lateral neck and/or shoulder, none developed motion limitation of the neck or shoulder.
Time-Serial Observations and Risks of Postoperative Hypocalcemia
Preoperative levels of serum calcium and PTH were similar for both normocalcemic and hypocalcemic patients. The node dissection group showed a greater decline (12.0%) in mean serum calcium levels from preoperative to postoperative day one compared with the no node dissection group (7.6%) (P = 0.002). From 1 day after surgery, serum calcium levels were lower for the node dissection group compared with the no node dissection group (Fig. 1). For both groups, calcium levels slowly increased from 7 days, and had nearly completely recovered by 3 months after surgery. However, serum calcium level recovery was slower in the node dissection group than the no node dissection group.
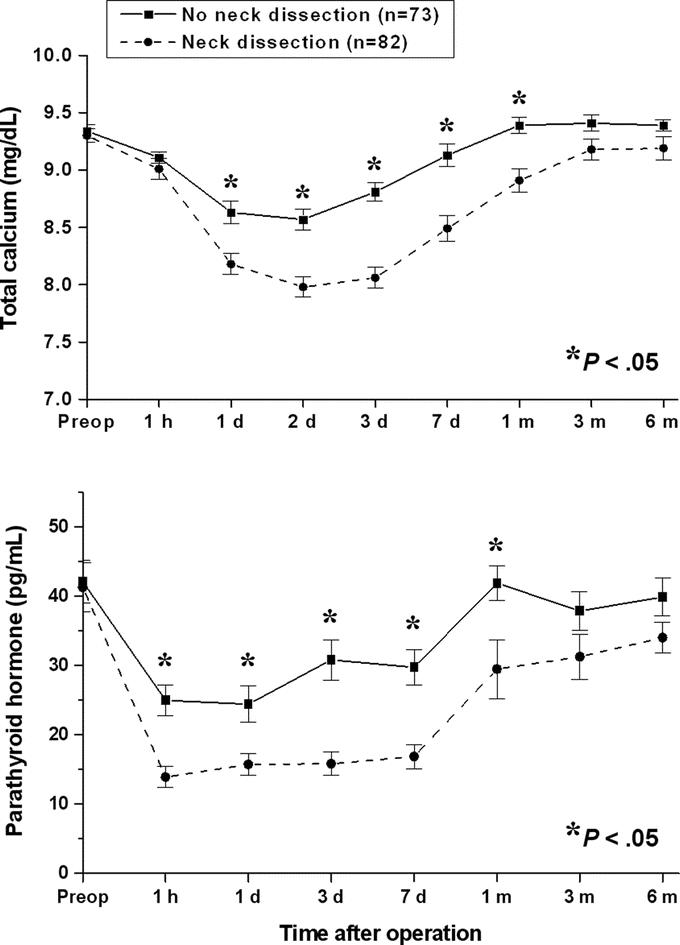
FIGURE 1. Changes in total calcium (upper panel) and intact parathyroid hormone (lower panel) levels before and after total thyroidectomy in the with or without neck dissection groups. Values represent mean ± SEM. *t test.
Serum PTH concentrations dropped in most patients as rapidly as 1 hour after thyroidectomy (Fig. 1). For the no node dissection group, PTH levels decreased to 24.9 pg/mL after surgery, remained low for 7 days, and then recovered to preoperative levels by 1 month after surgery. For the node dissection group, PTH levels decreased to 13.9 pg/mL after surgery, remained low for 7 days, and then slowly recovered by 6 months after surgery. The mean intact PTH decline for the node dissection group (66.3%) during the early postoperative days was greater than for the no node dissection group (40.8%) (P = 0.001).
Fifty-seven of the 82 (69.5%) node dissection patients were normocalcemic preoperatively, and 25 (30.5%) of these developed postoperative hypocalcemia. Serum calcium and intact PTH levels decreased in both normocalcemic and hypocalcemic groups, and recovered by 3 months after surgery (Fig. 2). The calcium and PTH declines during the early postoperative days were greater and the recovery of the serum levels was slower in the hypocalcemic patients compared with the normocalcemic patients.
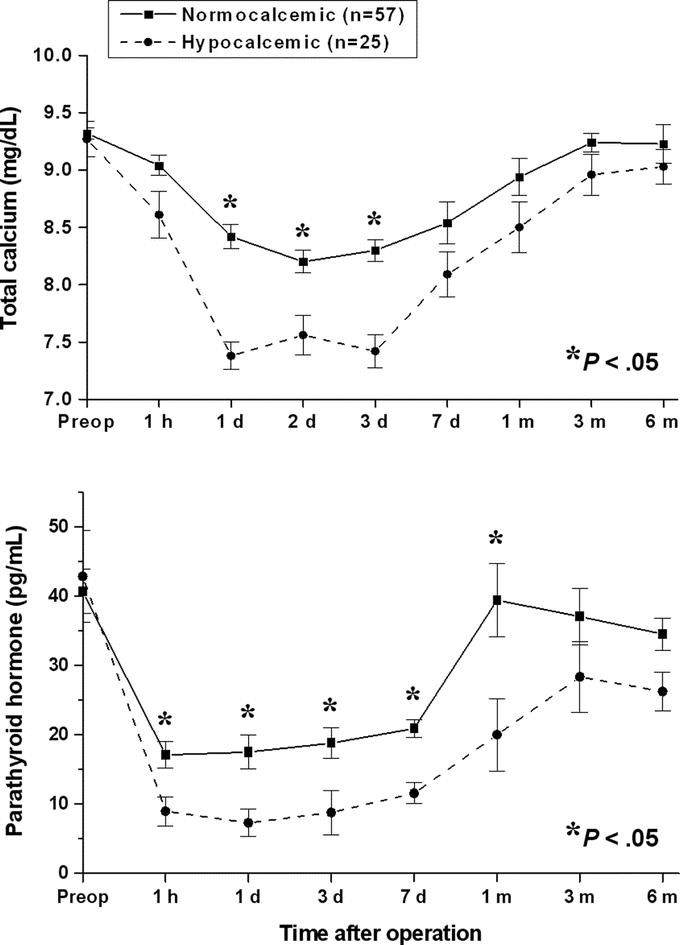
FIGURE 2. Changes in total calcium (upper panel) and intact parathyroid hormone (lower panel) levels before and after total thyroidectomy plus neck dissection in the with or without postoperative hypocalcemia groups. Values represent mean ± SEM. *t test.
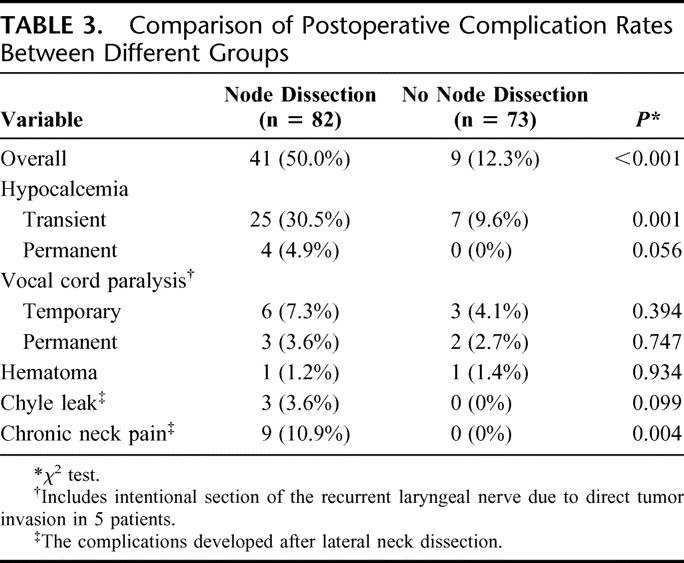
In the node dissection group, the incidence of postoperative hypocalcemia was compared according to LND and parathyroid gland status. The LND group had a higher incidence of hypocalcemia than the no LND group (12 of 26, 46.2%; vs. 13 of 56, 23.2%; P = 0.036). However, there were no significant differences in the number of parathyroid glands preserved (mean ± SD, 3.49 ± 0.89 vs. 3.69 ± 0.63), frequency of parathyroid autotransplantation (10 of 57, 17.5%; vs. 6 of 25, 24.0%) or incidental parathyroidectomy (7 of 57, 12.3%; vs. 4 of 25, 16.0%) between normocalcemic and hypocalcemic groups (P > 0.25). The risk of postoperative hypocalcemia in relation to node dissection was analyzed (Table 4). CND increased the risk of hypocalcemia compared with total thyroidectomy alone (P = 0.034). LND in addition to CND also raised the postoperative hypocalcemic risk compared with total thyroidectomy plus CND (P = 0.036). Total thyroidectomy plus combined CND and LND increased the risk of hypocalcemia compared with total thyroidectomy alone (P < 0.001). However, the complication rates and postoperative levels of serum PTH did not differ between 40 patients undergoing prophylactic CND and 16 patients undergoing therapeutic CND (P > 0.2).
TABLE 4. Risks of Postoperative Hypocalcemia in Relation to Node Dissection
Follow-up and Recurrences
The mean duration of follow-up was 52 months (range, 12–69 months). Postoperative I131 ablation was undertaken and TSH suppression thyroxine therapy was administered to all patients. Recurrence developed in 4 patients (2.6%): 1 in the central neck only and 3 in both the central and lateral neck. Three of those patients were no node dissection patients, and they experienced recurrent cancers in the central compartment alone (n = 1) or the central and lateral compartments (n = 2). Those patients subsequently underwent LND or CND plus LND and were free of disease. The mean time elapsed from thyroidectomy to nodal recurrence was 48 months (range, 29–52 months). Two patients died of heart problems or lung cancer. All other patients were currently free of disease, except 1 patient who had a distant metastasis prior to initial surgery.
DISCUSSION
The present study involving 155 PTC patients compared morbidities including hypocalcemia between 82 patients who underwent a total thyroidectomy plus neck node dissection and 73 patients who underwent a total thyroidectomy alone (no neck node dissection). The study revealed that patients undergoing neck node dissection, which comprised 82 CNDs and 26 LNDs, experienced greater overall morbidity (50.0%) compared with patients who underwent a total thyroidectomy alone (12.3%) (P > 0.001). Postoperative hypocalcemia occurred far more commonly in node dissection than no node dissection patients (30.5% vs. 9.6%, P = 0.001). The study findings indicate significant morbidity occurs when CND is performed together with a total thyroidectomy, particularly if an LND is also performed.
Recent studies of nodal dissection in differentiated thyroid cancer patients reported the development of permanent hypoparathyroidism in 3% to 4% of patients, and transient vocal cord paralysis in 3% to 6%.12–14 Hypocalcemia was more commonly seen when neck dissection was combined with thyroidectomy than when it was not, and was especially high in patients undergoing combined CND. In the present study, hypocalcemia was also highest in patients who underwent combined CND plus LND with total thyroidectomy (46.2%). Addition of LND into the CND procedure also resulted in an increased risk of postoperative hypocalcemia compared with thyroidectomy plus CND. This implies that the extension of nodal dissection to include the central neck to lateral cervical compartment increased vascular compromise in the dissected central neck and the parathyroid glands, which caused a higher rate of hypoparathyroidism during the early postoperative weeks.
The current study found that increased hypoparathyroidism appeared not to be associated with incidental removal of the parathyroid glands or the number of parathyroid glands preserved during surgery. In addition, selective parathyroid autotransplantation did not appear to solve this problem since, despite more frequent use of this procedure in the node dissection group, 4.9% of patients experienced permanent hypocalcemia. Thus, better identification and careful preservation of parathyroid glands and routine autotransplantation of at least 1 gland may be advisable for prevention of permanent hypoparathyroidism.18 In addition, meticulous preservation of the vascular supply and the parathyroid gland drainage system during nodal dissection may reduce hypocalcemic morbidity.
Biochemical assays showed that serum calcium levels decreased in most patients in the early days after total thyroidectomy. The decrease in serum calcium levels following thyroid surgery is secondary to impairment of parathyroid function in most cases.19 The deceased levels of serum calcium begin to recover in parallel with the increase in PTH levels from several days after surgery. The biochemical assay results over time showed that parathyroid function was compromised in the node dissection group during the early weeks after surgery (Fig. 1). The hypocalcemic patients in the node dissection group experienced hypocalcemic symptoms as well as low serum calcium and PTH levels (Fig. 2). In addition, the PTH recovery in those patients was slow and did not reach preoperative levels. The high prevalence and consequences of postoperative hypocalcemia in node dissection patients suggests that early prediction of hypocalcemia and interventions such as parathyroid autotransplantation or early calcium supplementation are required.
The present study revealed that postoperative hypocalcemia developed as late as at least 24 hours after surgery. Serum PTH levels were more sensitive and were an earlier predictor of postoperative hypocalcemia than serum calcium levels, as reported previously.20,21 Recent studies22,23 reported that postoperative hypocalcemia can be predicted as early as at the end of thyroidectomy. Thus, measurement of serum PTH levels can encourage more active assessment of parathyroid gland vascularity with a view for autotransplantation and early supplementation of oral calcium.24,25 The current study is the first to reveal the decline and recovery of PTH levels after thyroidectomy plus neck dissection in the management of PTC. Intraoperative or perioperative PTH measurements assist in managing postoperative hypoparathyroidism, especially in patients undergoing neck dissection combined with bilateral thyroid surgery. Additionally, the present findings regarding the time-frame of serum PTH level decrease will assist in future determination of the duration of postoperative calcium administration.
Pathology examination of the 82 node dissections showed that both the central and ipsilateral lateral compartments were frequently affected by lymphatic nodal metastasis from the PTC. Within the central compartment, the pretracheal and ipsilateral paratracheal sites were commonly involved, and within the lateral compartment, the ipsilateral jugular nodes (levels II, III, and IV) were commonly involved. The posterior triangle (level V) or contralateral lateral neck, on the other hand, was rarely involved. Similarly, skip lesions, involving lateral lymph nodes without central lymph nodes, were also rare. This pattern of node involvement is similar to that previously reported.6,7,26,27 The location of the primary tumor does not predict the pattern of lymph node metastasis.6 Patients with multifocal or extrathyroidal cancers are more likely to have nodal metastases.7,11 Neck dissection including the posterior triangle can result in morbidity of the spinal accessory nerve or cervical root branches, which may cause postoperative shoulder dysfunction or chronic neck pain.28 The present study found that nodal recurrence preferentially occurred in the ipsilateral jugular nodes or central nodes, as has been reported elsewhere.6,7,26,27 Thus, therapeutic node dissection should concentrate on the jugular and central nodes to avoid recurrence, sparing the posterior triangle.
While CND modification to involve only the ipsilateral central neck may prevent postoperative hypocalcemia, it remains controversial in terms of simultaneous or skipped metastasis to contralateral central nodes that occurs in a considerable number of PTC cases. Considering the recurrence pattern, overall survival, and morbidity, prophylactic node dissection of the central or lateral neck is not recommended if there is no macroscopic nodal metastasis.1,3,7,29 Any lateral cervical recurrence of PTC requires at least subsequent ipsilateral CND as well as comprehensive neck dissection of the involved lateral neck because lymph node metastasis in the central compartment appears to be a valuable indicator of lymphatic invasion of the lateral compartment.
Careful preservation of parathyroid vascularity or autotransplantation of devascularized parathyroid glands may reduce postoperative hypoparathyroidism in PTC cases involving macroscopic nodal metastasis where aggressive neck management is required. Biochemical monitoring of serum calcium and PTH levels can assist in initiating early management for postoperative hypocalcemia and reducing hypocalcemic symptoms during the early weeks after surgery.
CONCLUSION
PTH levels were significantly reduced following bilateral CND and lateral neck dissection in PTC patients. The present analysis of lymph node metastasis pattern, recurrence, and morbidity leads us to conclude that prophylactic neck node dissection for PTC is not recommended. When performing therapeutic neck dissection of central and lateral compartments, the present results highlight the advantages associated with monitoring serum calcium and PTH levels, parathyroid preservation and routine parathyroid autotransplantation, particularly where macroscopic nodal metastasis is detected preoperatively or intraoperatively.
Footnotes
Reprints will not be available from the authors.
Correspondence: Jong-Lyel Roh, MD, PhD, Department of Otolaryngology, Asan Medical Center, University of Ulsan College of Medicine, 388-1, Pungnap-dong, Songpa-gu, Seoul 138-736, Republic of Korea. E-mail: rohjl@amc.ac.kr.
REFERENCES
- 1.Hughes CJ, Shaha AR, Shah JP, et al. Impact of lymph node metastasis in differentiated carcinoma of the thyroid: a matched-pair analysis. Head Neck. 1996;18:127–132. [DOI] [PubMed] [Google Scholar]
- 2.Coburn MC, Wanebo HJ. Prognostic factors and management considerations in patients with cervical metastases of thyroid cancer. Am J Surg. 1992;164:671–676. [DOI] [PubMed] [Google Scholar]
- 3.Sellers M, Beenken S, Blankenship A, et al. Prognostic significance of cervical lymph node metastases in differentiated thyroid cancer. Am J Surg. 1992;164:578–581. [DOI] [PubMed] [Google Scholar]
- 4.Beasley NJ, Lee J, Eski S, et al. Impact of nodal metastases on prognosis in patients with well-differentiated thyroid cancer. Arch Otolaryngol Head Neck Surg. 2002;128:825–828. [DOI] [PubMed] [Google Scholar]
- 5.Noguchi S, Murakami N, Yamashita H, et al. Papillary thyroid carcinoma: modified radical neck dissection improves prognosis. Arch Surg. 1998;133:276–280. [DOI] [PubMed] [Google Scholar]
- 6.Mirallie E, Visset J, Sagan C, et al. Localization of cervical node metastasis of papillary thyroid carcinoma. World J Surg. 1999;23:970–973. [DOI] [PubMed] [Google Scholar]
- 7.Wada N, Duh QY, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003;237:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McConahey WM, Hay ID, Woolner LB, et al. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986;61:978–996. [DOI] [PubMed] [Google Scholar]
- 9.Shah JP, Loree TR, Dharker D, et al. Prognostic factors in differentiated carcinoma of the thyroid gland. Am J Surg. 1992;164:658–661. [DOI] [PubMed] [Google Scholar]
- 10.Lundgren CI, Hall P, Dickman PW, et al. Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer. 2006;106:524–531. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz S, Rodriguez JM, Soria T, et al. Extrathyroid spread in papillary carcinoma of the thyroid: clinicopathological and prognostic study. Otolaryngol Head Neck Surg. 2001;124:261–265. [DOI] [PubMed] [Google Scholar]
- 12.Henry JF, Gramatica L, Denizot A, et al. Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg. 1998;383:167–169. [DOI] [PubMed] [Google Scholar]
- 13.Goropoulos A, Karamoshos K, Christodoulou A, et al. Value of the cervical compartments in the surgical treatment of papillary thyroid carcinoma. World J Surg. 2004;28:1275–1281. [DOI] [PubMed] [Google Scholar]
- 14.Cheah WK, Arici C, Ituarte PH, et al. Complications of neck dissection for thyroid cancer. World J Surg. 2002;26:1013–1016. [DOI] [PubMed] [Google Scholar]
- 15.Tisell LE, Nilsson B, Molne J, et al. Improved survival of patients with papillary thyroid cancer after surgical microdissection. World J Surg. 1996;20:854–859. [DOI] [PubMed] [Google Scholar]
- 16.Demeester-Mirkine N, Hooghe L, Van Geertruyden J, et al. Hypocalcemia after thyroidectomy. Arch Surg. 1992;127:854–858. [DOI] [PubMed] [Google Scholar]
- 17.Bentrem DJ, Rademaker A, Angelos P. Evaluation of serum calcium levels in predicting hypoparathyroidism after total/near-total thyroidectomy or parathyroidectomy. Am Surg. 2001;67:249–251. [PubMed] [Google Scholar]
- 18.Olson JA Jr, DeBenedetti MK, Baumann DS, et al. Parathyroid autotransplantation during thyroidectomy: results of long-term follow-up. Ann Surg. 1996;223:472–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pattou F, Combemale F, Fabre S, et al. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg. 1998;22:718–724. [DOI] [PubMed] [Google Scholar]
- 20.Lombardi CP, Raffaelli M, Princi P, et al. Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery. 2004;136:1236–1241. [DOI] [PubMed] [Google Scholar]
- 21.Lindblom P, Westerdahl J, Bergenfelz A. Low parathyroid hormone levels after thyroid surgery: a feasible predictor of hypocalcemia. Surgery. 2002;131:515–520. [DOI] [PubMed] [Google Scholar]
- 22.Lo CY, Luk JM, Tam SC. Applicability of intraoperative parathyroid hormone assay during thyroidectomy. Ann Surg. 2002;236:564–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richards ML, Bingener-Casey J, Pierce D, et al. Intraoperative parathyroid hormone assay: an accurate predictor of symptomatic hypocalcemia following thyroidectomy. Arch Surg. 2003;138:632–635. [DOI] [PubMed] [Google Scholar]
- 24.Friedman M, Vidyasagar R, Bliznikas D, et al. Intraoperative intact parathyroid hormone level monitoring as a guide to parathyroid reimplantation after thyroidectomy. Laryngoscope. 2005;115:34–38. [DOI] [PubMed] [Google Scholar]
- 25.Bellantone R, Lombardi CP, Raffaelli M, et al. Is routine supplementation therapy (calcium and vitamin D) useful after total thyroidectomy? Surgery. 2002;132:1109–1112. [DOI] [PubMed] [Google Scholar]
- 26.Gimm O, Rath FW, Dralle H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg. 1998;85:252–254. [DOI] [PubMed] [Google Scholar]
- 27.Sivanandan R, Soo KC. Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg. 2001;88:1241–1244. [DOI] [PubMed] [Google Scholar]
- 28.van Wilgen CP, Dijkstra PU, van der Laan BF, et al. Shoulder and neck morbidity in quality of life after surgery for head and neck cancer. Head Neck. 2004;26:839–844. [DOI] [PubMed] [Google Scholar]
- 29.Pereira JA, Jimeno J, Miquel J, et al. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery. 2005;138:1095–1100. [DOI] [PubMed] [Google Scholar]