Abstract
Objective:
To determine whether and to what extent preexisting medical comorbidities influence mortality risk and length of hospitalization in patients with acute burn injury.
Summary Background Data:
The effects on mortality and length of stay of a number of important medical comorbidities have not been examined in acute burn injury. Existing studies that have investigated the effects of medical comorbidities on outcomes in acute burn injury have produced inconsistent results, chiefly due to the use of relatively small samples from single burn centers.
Methods:
Records of 31,338 adults who were admitted with acute burn injury to 70 burn centers from the American Burn Association National Burn Repository, were reviewed. A burn-specific list of medical comorbidities was derived from diagnoses included in the Charlson Index of Comorbidities and the Elixhauser method of comorbidity measurement. Logistic regression was used to assess the effects of preexisting medical conditions on mortality, controlling for demographic and burn injury characteristics. Ordinal least squares regression with a logarithmic transformation of the dependent variable was used to assess the relationship of comorbidities with length of stay.
Results:
In-hospital mortality was significantly predicted by HIV/AIDS (odds ratio [OR] = 10.2), renal disease (OR = 5.1), liver disease (OR = 4.8), metastatic cancer (OR = 4.6), pulmonary circulation disorders (OR = 2.9), congestive heart failure (OR = 2.4), obesity (OR = 2.1), non-metastatic malignancies (OR = 2.1), peripheral vascular disorders (OR = 1.8), alcohol abuse (OR = 1.8), neurological disorders (OR = 1.6), and cardiac arrhythmias (OR = 1.5). Increased length of hospital stay among survivors was significantly predicted by paralysis (90% increase), dementia (60%), peptic ulcer disease (53%), other neurological disorders (52%), HIV/AIDS (49%), renal disease (44%), a psychiatric diagnosis (42%), cerebrovascular disease (41%), cardiac arrhythmias (40%), peripheral vascular disorders (39%), alcohol abuse (36%), valvular disease (32%), liver disease (30%), diabetes (26%), congestive heart failure (23%), drug abuse (20%), and hypertension (17%).
Conclusions:
A number of preexisting medical conditions influence outcomes in acute burn injury. Patients with preburn HIV/AIDS, metastatic cancer, liver disease, and renal disease have particularly poor prognoses.
Data from 31,338 patients from the American Burn Association National Data Repository were used to assess the effects of preexisting medical conditions on mortality and length of hospital stay in acute burn injury. A number of comorbidities predicted both mortality and length of stay. Patients with HIV/AIDS, liver disease, renal disease, and metastatic cancer had particularly poor prognoses.
Many studies have shown that age, burn size, and inhalation injury are important predictors of mortality and length of hospital stay following an acute burn injury.1–4 The effects of preexisting medical conditions on mortality and length of stay, however, are not well understood in burn injuries.
Studies that have investigated the effect of medical comorbidities on burn outcomes have generally been limited by relatively small samples from single burn centers with few total fatalities and a limited number of patients within each medical comorbidity category. They have also been limited by the lack of clearly defined comorbidity categories and diagnoses and, in most cases, by univariate analyses that do not control for important confounders, such as age. As a result, studies of the impact of the number of preexisting medical conditions on outcome4–7 or of the effects of specific medical comorbidities on outcome7–11 have produced contradictory results. Different studies, for instance, have reported that cardiovascular disease is not associated with increased mortality,7,8 predicts mortality on a univariate, but not a multivariate, basis,9 or predicts mortality even after controlling for burn-related risk factors.10,11 Findings on the effects of renal disease,10,11 neurologic disease,7,10,11 and chronic pulmonary disease8,9 are similarly discrepant. In addition, the effects on mortality and length of stay of a number of potentially important comorbid conditions, including liver disease, obesity, hypertension, and cancer, have not been examined in burn patients.
We analyzed data from the American Burn Association National Burn Repository (ABA-NBR) to address gaps and inconsistencies in this research. The objective of our study was to determine whether and to what extent preexisting medical comorbidities impact mortality risk and length of hospitalization in patients hospitalized with acute burn injury.
METHODS
Patient Sample
Data were extracted from the ABA-NBR database for all adult patients 18 to 89 years of age who were admitted to 70 burn centers across the United States with thermal injuries (flame, contact, or scald) from 1995 through 2005. In addition to medical comorbidities, patient data in the ABA-NBR included age, sex, race, year of injury, hospital admission status (eg, direct admission or transfer), the etiology and circumstances of the burn injury, mortality status and cause, percent total body surface area (TBSA) burned, percent TBSA burned second degree, percent TBSA burned third degree, and the presence or absence of an inhalation injury. Data used in this study to assess the likelihood of mortality and length of stay reflect information available at the time of admission. Patients 90 years of age and older were not included in the study because their actual ages were not entered into the dataset due to patient privacy regulations. A more complete description of the ABA-NBR database is provided elsewhere.12
Development of Comorbidity List
A comorbid disease was defined as a clinical condition that predated the burn injury and admission to the hospital and that could reasonably be expected to impact mortality and course of treatment.13 The ABA-NBR codes both diagnoses at the time of admission and complications of treatment. Admission diagnoses in the ABA-NBR include premorbid medical diagnoses and diagnoses that result from the burn injury. In this study, comorbid diagnoses were included only if present at admission and not likely to be a result of the burn injury. There was no limit to the number of different medical comorbidities that could be coded in the database for a given patient.
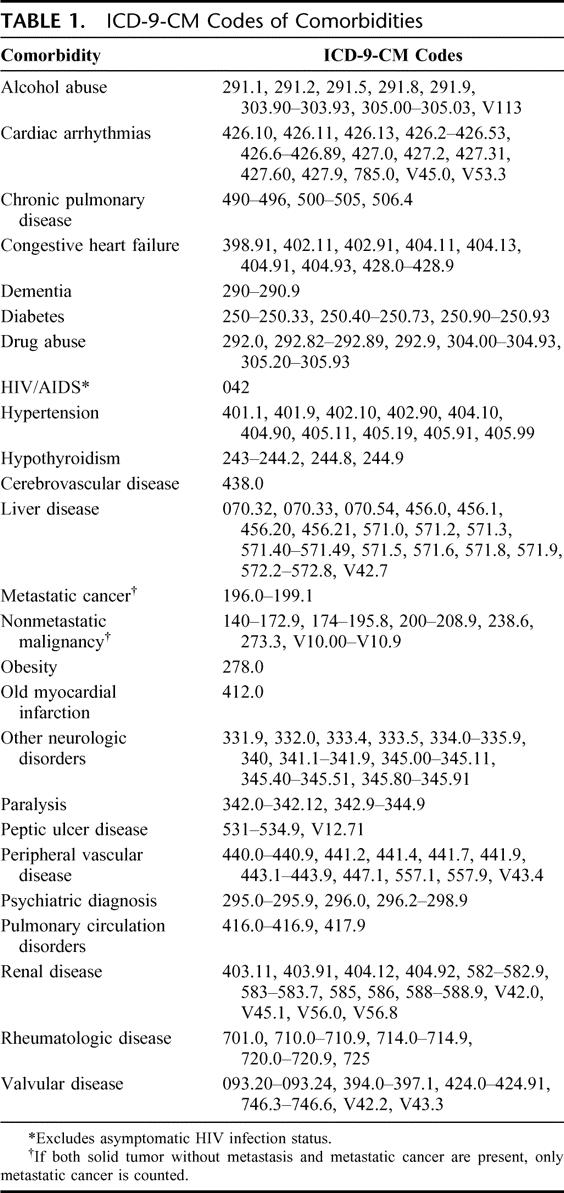
An initial list of potentially relevant comorbidities was selected from comorbidities included in the Deyo adaptation14 of the Charlson Index15 and the Elixhauser method of comorbidity measurement.13 Comorbidities were excluded if the diagnosis at admission could have been related to the burn injury (eg, fluid and electrolyte disorders, nutrition deficits, coagulation deficits, anoxic brain injury). The list of comorbidities included in analyses and their ICD-9-CM codes are shown in Table 1.
TABLE 1. ICD-9-CM Codes of Comorbidities
Data Presentation and Statistical Analysis
Outcome measures were in-hospital mortality and length of hospital stay. Prior to outcome assessment, χ2 tests were used to compare categorical variables, and Mann-Whitney U tests were used to compare continuous variables, between patients with different numbers of medical comorbidities (0, 1, 2, 3+). The association of medical comorbidities with in-hospital mortality was modeled using a forward stepwise logistic regression model, controlling for age, sex, percent TBSA burned, and presence or absence of inhalation injury. Length of hospital stay was modeled using forward stepwise ordinary least squares regression, also controlling for age, sex, percent TBSA burned, and inhalation injury. The length of stay outcome variable was transformed logarithmically due to the high degree of positive skew and long tail of the distribution. Antilog transformations of beta coefficients in the length of stay analysis were done to provide an estimate of the expected percent increase in length of stay related to having a particular comorbidity. Length of stay was modeled only for patients who survived the burn injury. This was done to avoid the potentially misleading situation in which a powerful predictor of mortality could appear to be unrelated to length of hospital stay because of high rates of mortality related to the predictor. Because of the very large sample size, variables were only entered into the model if they were statistically significant (P < 0.05). All analyses were conducted using SPSS version 13.0 (Chicago, IL).
Sensitivity Analysis
One potential shortcoming of large registries that are based on chart review of medical records is that coding of diagnoses may be imperfect, and patient records may not include all relevant comorbidities.13,16,17 The effect of failing to include all cases with a given comorbidity, however, would be expected to only minimally bias the estimates of odds ratios. This is because only a relatively few patients have each comorbidity and those incorrectly excluded from a comorbidity group due to incomplete data recording are subsumed into a very large pool of patients without the comorbidity. To test this assumption, we reran all outcome analyses after randomly selecting 25% of all patients within each comorbidity group to be incorrectly included among patients without the comorbidity.
RESULTS
Patient Characteristics
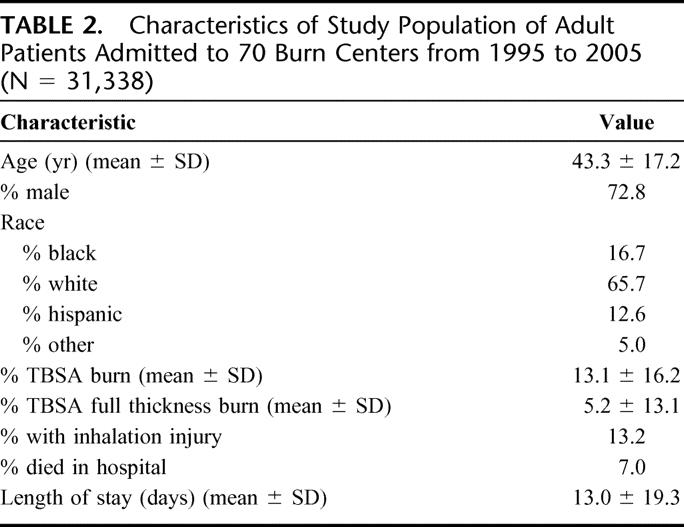
Demographic and burn injury characteristics, length of hospital stay, and the in-hospital mortality data are shown in Table 2. A total of 31,338 adult patients 18 to 89 years of age were admitted to 70 burn centers. The mean age of adult patients in the ABA-NBR was 43.4 ± 17.2 years, and the median was 40.6 years (interquartile range, 29.8–53.8 years; range, 18–89 years); 72.8% of patients were male, and 65.7% were white. The mean percent TBSA burned was 13.1% ± 16.2%, (median, 7.5%; interquartile range, 3.0%–16.2%; range, 0%–100%) and 13.2% of the sample incurred an inhalation injury.
TABLE 2. Characteristics of Study Population of Adult Patients Admitted to 70 Burn Centers from 1995 to 2005 (N = 31,338)
Comorbidities
As shown in Table 3, 26.4% of all patients had one or more medical comorbidities. Without controlling for confounding factors, such as age, a greater number of comorbidities was significantly related to a greater length of stay and a higher likelihood of death. The length of stay for patients with 3 or more comorbidities was approximately twice as high compared to patients with no comorbidities, and the likelihood of death was almost 4 times higher. The most commonly reported comorbidities among all patients were hypertension (9.6%), alcohol abuse (5.8%), chronic pulmonary disease (5.1%), diabetes (4.4%), drug abuse (3.3%), and psychiatric diagnoses (eg, schizophrenic disorders, bipolar disorders, major depressive disorders, 2.9%) (Table 4).
TABLE 3. Relationship Between Number of Comorbidities and Outcomes
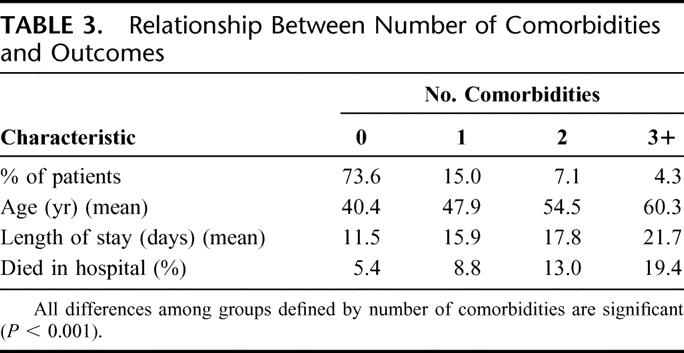
TABLE 4. Association of Comorbidities With In-Hospital Mortality After Controlling for Demographic and Burn Injury Characteristics
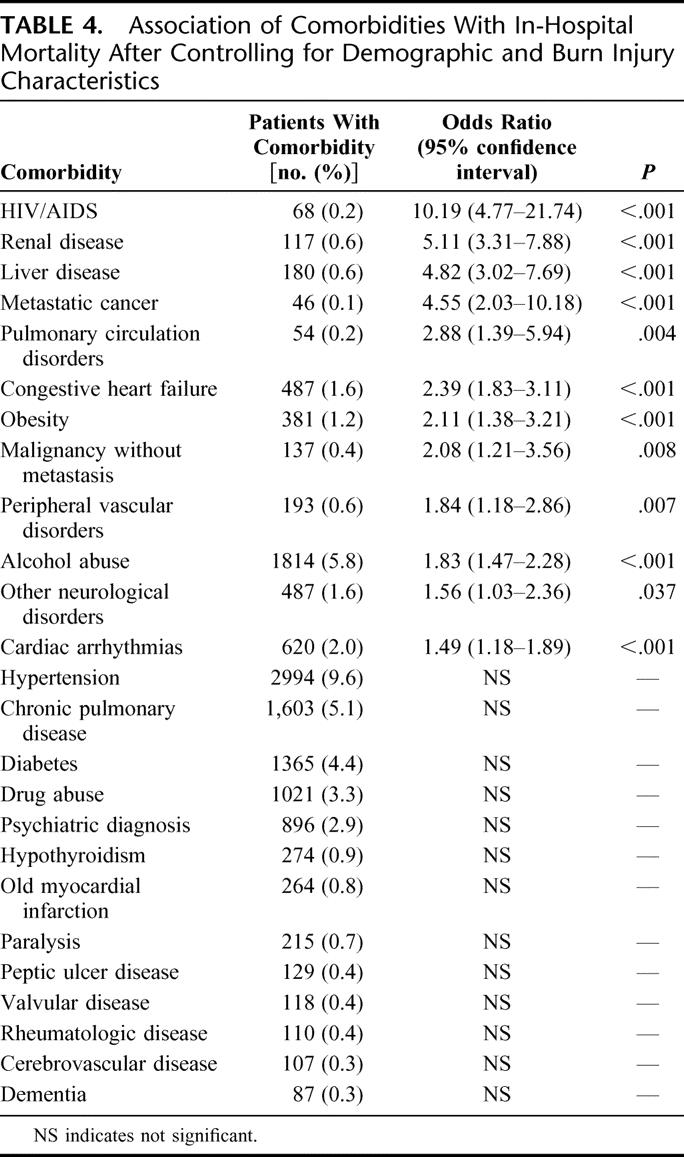
Association of Comorbidities with Mortality
There were 2203 total deaths (7.0%) among patients in the sample. Mortality was 9.0% (n = 769) in women and 6.3% (n = 1434) in men (P < 0.001). The independent effects of preexisting medical conditions on mortality after controlling for age, sex, percent TBSA burned, inhalation injury, and all other comorbidities are shown in Table 4. The comorbidities with the highest odds of mortality were HIV/AIDS (odds ratio [OR] = 10.2), renal disease (OR = 5.1), liver disease (OR = 4.8), and metastatic cancer (OR = 4.6) compared to patients who did not have those diseases, but who were similar on other variables in the model. Patients with histories of pulmonary circulation disorders, congestive heart failure, obesity, nonmetastatic malignancies, alcohol abuse, peripheral vascular disorders, cardiac arrhythmias, and neurologic disorders (eg, Parkinson disease, multiple sclerosis, epilepsy) were also at increased risk of mortality after controlling for demographic and burn variables and other comorbidities.
Chronic pulmonary disease (OR = 1.0, 95% confidence interval [CI], 0.8–1.3, P = 0.69), surprisingly, was not a significant independent predictor of in-hospital mortality. On an unadjusted basis, however, patients with chronic pulmonary disease were more than twice as likely to die compared to patients without chronic pulmonary disease (14.3% vs. 6.6%, OR = 2.3; 95% CI, 2.0–2.7, P < 0.001). They also had a significantly greater mean number of days in intensive care (7.0 vs. 4.4, P < 0.001), and days in the hospital (15.9 vs. 12.9, P < 0.001). These patients, however, were also significantly (P < 0.001) more likely to have at least one additional medical comorbidity (65.0% vs. 22.4%). Specifically, they were more likely (P < 0.001) to have a diagnosis of alcohol abuse (14.7% vs. 5.3%), congestive heart failure (11.2% vs. 1.0%), cardiac arrhythmias (8.8% vs. 1.6%), dementia (1.0% vs. 0.2%), other neurologic disorders (3.2% vs. 1.5%), diabetes (13.0% vs. 3.9%), hypertension (29.7% vs. 8.5%), liver disease (2.7 vs. 0.5%), obesity (4.6% vs. 1.0%), peptic ulcer disease (2.0% vs. 0.3%), valvular disease (1.1% vs. 0.3%), peripheral vascular disease (3.6% vs. 0.5%), pulmonary circulation disorders (0.8% vs. 0.1%), cerebrovascular disease (1.7% vs. 0.3%), old myocardial infarction (4.1% vs. 0.7%), renal disease (1.7% vs. 0.5%), metastatic cancer (0.9% vs. 0.1%), a nonmetastatic malignancy (1.9% vs. 0.4%), hypothyroidism (2.9% vs. 0.8%), rheumatologic disease (0.9% vs. 0.3%), and/or a psychiatric diagnosis (7.9% vs. 2.6%). Even after adjusting for age and sex, patients with chronic pulmonary disease were more likely to have each of these diagnoses (range of ORs, 1.7–6.6). In addition, patients with chronic pulmonary disease were more likely to have incurred an inhalation injury (24.3% vs. 12.6%), even after controlling for demographics and burn size (OR = 2.1, P < 0.001). When compared to other patients with inhalation injuries, however, patients with chronic pulmonary disease who had inhalation injuries were significantly more likely to have incurred a very small burn of TBSA ≤3% (29.7% vs. 13.0%, OR = 2.8, P < 0.001).
In terms of numbers of preexisting conditions, the odds of mortality increased 1.33 times (95% CI, 1.27–1.40, P < 0.001) for each additional medical comorbidity, controlling for demographic and burn characteristics. When only patients age 65 or older were considered, the increase in mortality risk per comorbidity was essentially the same (OR = 1.28; 95% CI, 1.20–1.37, P < 0.001).
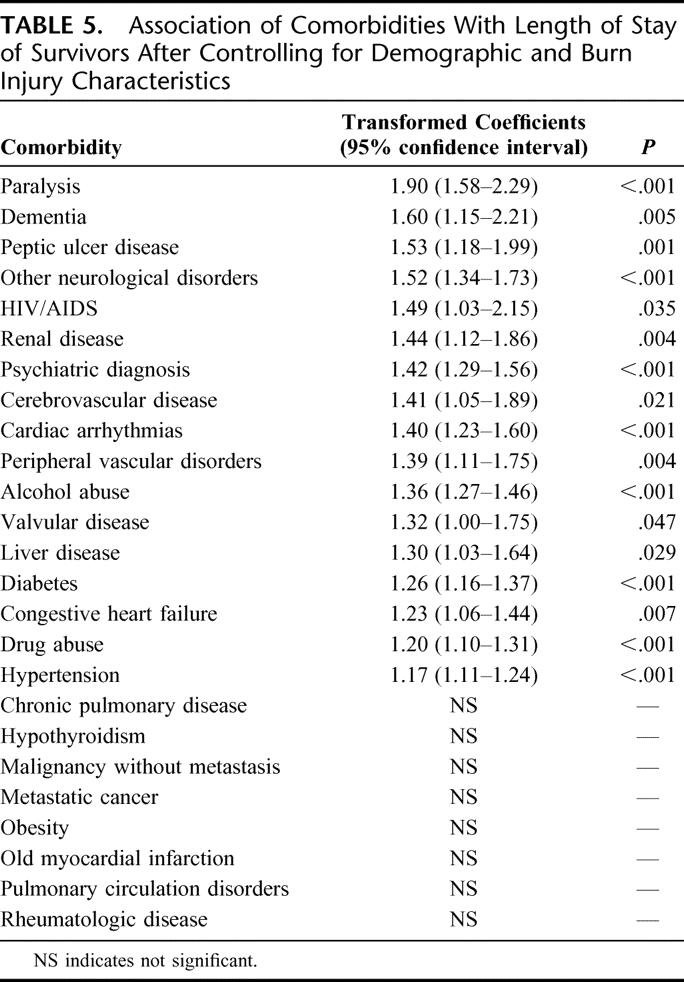
Association of Comorbidities With Length of Stay
The mean length of stay was 13.0 ± 19.3 (median, 7; interquartile range, 2–16; range, 1–450) days for all patients and 12.6 ± 18.6 (median, 7; interquartile range, 2–15; range, 1–450) days for patients who survived. In general, comorbidities that were significantly associated with mortality tended to predict length of stay among patients who survived to discharge. Three exceptions, however, were pulmonary circulation disorders, obesity, and nonmetastatic malignancies. Several conditions that were not significantly related to in-hospital mortality did predict longer lengths of stay in patients who survived, including paralysis (90% increase), dementia (60% increase), peptic ulcer disease (53% increase), a psychiatric diagnosis (42% increase), cerebrovascular disease (41% increase), valvular disease (32% increase), diabetes (26% increase), drug abuse (20% increase), and hypertension (17% increase). Patients with chronic pulmonary disease tended to have slightly, albeit nonsignificantly, shorter lengths of stay than otherwise comparable patients (5.9% decrease, 95% CI, 12.8% decrease to 1.6% increase, P = 0.12).
As compared with similar patients with no medical comorbidities, the length of stay increased 22.9% (95% CI, 20.5%–25.3%, P < 0.001) for each preexisting condition. For patients age 65 or older, length of stay increased 16.6% (95% CI, 11.8%–21.6%, P < 0.001) per comorbidity. Results from the length of stay analysis are shown in Table 5.
TABLE 5. Association of Comorbidities With Length of Stay of Survivors After Controlling for Demographic and Burn Injury Characteristics
Sensitivity Analysis
The ORs for mortality for each comorbidity when 25% of patients with the comorbidity were randomly selected to be miscoded as not having the diagnosis were very close to estimates using the entire sample: HIV/AIDS = 10.1, renal disease = 6.2, liver disease = 4.8, metastatic cancer = 5.6, pulmonary circulation disorders = 3.3, congestive heart failure = 2.4, obesity = 2.0, malignancy without metastasis = 2.5, alcohol abuse = 1.9, peripheral vascular disorders = 1.7, cardiac arrhythmias = 1.9, and other neurologic disorders = 1.3. The estimated percent increase in length of stay of patients due to comorbidities among patients who survived the burn injury were also relatively unchanged when 25% of patients with each diagnosis were miscoded: paralysis = 95%, dementia = 49%, other neurologic disorders = 51%, peptic ulcer disease = 63%, HIV/AIDS = 52%, a psychiatric diagnosis = 45%, peripheral vascular disorders = 42%, renal disease = 46%, cardiac arrhythmias = 38%, liver disease = 54%, cerebrovascular disease 49%, alcohol abuse = 36%, valvular disease = 54%, congestive heart failure = 32%, diabetes = 29%, drug abuse =19%, and hypertension = 20%. These results suggest that if there is incomplete diagnostic coding in the ABA-NBR, it did not likely impact risk estimates substantially.
DISCUSSION
This is the first study to use a large, representative sample from multiple burn centers to investigate the effect of preexisting medical conditions on mortality from burn injury and length of hospital stay among survivors. We used data from over 31,000 adult admissions to 70 burn centers and found that patients with more preexisting medical conditions at admission have a greater risk of mortality and require longer hospital stays than patients of similar age, sex, and burn injury characteristics, but fewer comorbidities. No previous study has used such a large sample or investigated the effects of a broad range of medical comorbidities in patients with acute burn injury.
Preexisting medical conditions were recorded in almost 27% of patients in the sample. Medical comorbidities that predicted mortality, after controlling for age, sex, percent TBSA burned, and inhalation injury included HIV/AIDS, renal disease, metastatic cancer, liver disease, pulmonary circulation disorders, congestive heart failure, obesity, nonmetastatic malignancies, alcohol abuse, peripheral vascular disorders, cardiac arrhythmias, and neurologic disorders. The most striking result was the very high risk of mortality among patients with HIV/AIDS (OR = 10.2), renal disease (OR = 5.1), liver disease (OR = 4.8) and metastatic cancer (OR = 4.6). All preexisting conditions that predicted mortality, with the exceptions of obesity, pulmonary circulation disorders and non-metastatic malignancies also predicted longer hospital stays. In addition, patients with paralysis, dementia, peptic ulcer disease, a psychiatric diagnosis, cerebrovascular disease, valvular disease, diabetes, drug abuse, and hypertension required significantly longer hospital stays.
Our results are in agreement with studies that have identified greater risk with higher numbers of medical comorbidities,5 that have identified alcohol abuse as a risk factor for mortality and longer hospital stays,10,18–22 and that have found patients with diabetes23 and psychiatric disorders to require longer hospital stays.19,24 Our findings also provide a degree of clarity in areas where previous studies have not been in agreement, including cardiovascular disease, renal disease, and neurologic disorders.
We were surprised to find that chronic pulmonary disease was not a significant independent predictor of mortality or longer hospital stays, although there was a trend toward greater risk of mortality. Traditionally, patients with chronic pulmonary disease have been considered to be at high risk for mortality, particularly in the context of inhalation injury. There may be two interrelated explanations for the findings in this study. First, patients with chronic pulmonary disease tended to have multiple medical comorbidities at much greater rates than other patients, even after controlling for age. Thus, the independent effect of chronic pulmonary disease may have been diminished. Second, it could be the case that there is a lower threshold for admission to the hospital for patients with chronic pulmonary disease who may have incurred an inhalation injury. Among all patients with inhalation injuries, those with chronic pulmonary disease were much more likely to have a very small burn (TBSA ≤3%). Many patients with chronic pulmonary disease who are on home oxygen, for instance, are admitted after sustaining superficial facial burns in the context of smoking near an open oxygen source. A lower threshold for admission would result in comparatively less severe burn injuries among patients in the database who had chronic pulmonary disease. If this were the case, it is possible that the multivariate models used in this study underestimated the independent effects of chronic pulmonary disease on mortality and length of hospital stay.
There are limitations that should be taken into consideration in interpreting the results from this study. The data are from a large registry and are to some degree flawed in their ability to capture patient illness severity. Patient comorbidity and injury variables, such as TBSA burned or the presence or absence of inhalation injury, were extracted by chart review, and diagnoses were documented with ICD-9 coding rather than by more precise methods. In some cases, it is difficult to determine from ICD-9 coding whether a diagnosis predated the burn injury. Thus, diagnoses were included as preexisting medical comorbidities only when they were unlikely to have resulted from the injury or its treatment. It is possible, however, that including only diagnoses of “old myocardial infarction,” for instance, and not “myocardial infarction” might have resulting in missed cases. It is not known if results would have differed if they had been based on more detailed clinical information, although our sensitivity analyses showed that diagnostic omissions would not likely alter results substantially. From a practical perspective, however, this is a moot point. Given the large number of patients that would need to be followed across many burn centers to obtain enough patients in each comorbidity category, it is doubtful that a nonregistry study could realistically be achieved. A second limitation is that, despite the large overall size of the ABA-NBR database, there were not enough patients with each comorbid condition to generate risk estimates based on patient characteristics, such as age or sex. It is possible, however, that risk of mortality and longer length of stay related to specific comorbid conditions differs based on these factors.
An additional limitation is that differences in mortality across burn care centers related to differences in standard burn management or differences in patient characteristics were not explicitly incorporated into the analysis. The ABA-NBR does not include data on important factors that may differ across centers, such as time from burn to admission or fluid resuscitation. To the extent that a large number of burn centers were included in the current study, however, it is not unreasonable to think that the model is a fair representation of typical patterns across burn centers in the United States.
CONCLUSION
We found that patients with acute burn injury with preburn medical conditions are at greater risk for mortality and require longer hospital stays prior to discharge. In particular, patients with HIV/AIDS, metastatic cancer, renal disease, and liver disease are at very high risk for mortality as compared with patients without those diseases who have similar burn injuries.
Footnotes
The current address of Dr. Thombs is Department of Psychiatry, Sir Mortimer B. Davis-Jewish General Hospital and McGill University, Montreal, Quebec, Canada.
The National Burn Repository of the American Burn Association is the source of the data contained in this document. The conclusions and opinions derived from National Burn Repository data represent the authors’ views and are not necessarily those of the American Burn Association. No outside funding was received for this study.
Reprints: Brett D. Thombs, PhD, Institute of Community and Family Psychiatry, SMBD-Jewish General Hospital, 4333 Cote, St. Catherine Road, Montreal, Quebec H3T 1E4. E-mail: brett.thombs@mcgill.ca.
REFERENCES
- 1.Ryan CM, Schoenfeld DA, Thorpe WP, et al. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–366. [DOI] [PubMed] [Google Scholar]
- 2.Smith DL, Cairns BA, Ramadan F, et al. Effect of inhalation injury, burn size, and age on mortality: a study of 1447 consecutive burn patients. J Trauma. 1994;37:655–659. [DOI] [PubMed] [Google Scholar]
- 3.Griffe O, Gartner R, Captier G, et al. Evaluation of prognostic factors in the burned patient. Ann Chir Plast Esthet. 2001;46:167–172. [DOI] [PubMed] [Google Scholar]
- 4.O'Keefe GE, Hunt JL, Purdue GF. An evaluation of risk factors for mortality after burn trauma and the identification of gender-dependent differences in outcomes. J Am Coll Surg. 2001;192:153–160. [DOI] [PubMed] [Google Scholar]
- 5.Covington DS, Wainwright DJ, Parks DH. Prognostic indicators in the elderly patient with burns. J Burn Care Rehabil. 1996;17:222–230. [DOI] [PubMed] [Google Scholar]
- 6.Wibbenmeyer LA, Amelon MJ, Morgan LJ, et al. Predicting survival in an elderly burn patient population. Burns. 2001;27:583–590. [DOI] [PubMed] [Google Scholar]
- 7.Barret JP, Gomez P, Solano I, et al. Epidemiology and mortality of adult burns in Catalonia. Burns. 1999;25:325–329. [DOI] [PubMed] [Google Scholar]
- 8.Stassen NA, Lukan JK, Mizuguchi NN, et al. Thermal injury in the elderly: when is comfort care the right choice? Am Surg. 2001;67:704–708. [PubMed] [Google Scholar]
- 9.Horbrand F, Schrank C, Henckel-Donnersmarck G, et al. Integration of preexisting diseases and risk factors in the Abbreviated Burn Severity Index (ABSI). Anasthesiol Intensivmed Notfallmed Schmerzther. 2003;38:151–157. [DOI] [PubMed] [Google Scholar]
- 10.Raff T, Germann G, Barthold U. Factors influencing the early prediction of outcome from burns. Acta Chir Plast. 1996;38:122–127. [PubMed] [Google Scholar]
- 11.Germann G, Barthold U, Lefering R, et al. The impact of risk factors and preexisting conditions on the mortality of burn patients and the precision of predictive admission-scoring systems. Burns. 1997;23:195–203. [DOI] [PubMed] [Google Scholar]
- 12.American Burn Association. National Burn Repository: 2005 Report. Chicago, IL: American Burn Association, 2006. [Google Scholar]
- 13.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 14.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 16.Hughes JS, Iezzoni LI, Daley J, et al. How severity measures rate hospitalized patients. J Gen Intern Med. 1996;11:303–311. [DOI] [PubMed] [Google Scholar]
- 17.Steiner CA, Bass EB, Talamini MA, et al. Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med. 1994;330:403–408. [DOI] [PubMed] [Google Scholar]
- 18.McGill V, Kowal-Vern A, Fisher SG, et al. The impact of substance use on mortality and morbidity from thermal injury. J Trauma. 1995;38:931–934. [DOI] [PubMed] [Google Scholar]
- 19.Berry CC, Patterson TL, Wachtel TL, et al. Behavioural factors in burn mortality and length of stay in hospital. Burns Incl Therm Inj. 1984;10:409–414. [DOI] [PubMed] [Google Scholar]
- 20.Haum A, Perbix W, Hack HJ, et al. Alcohol and drug abuse in burn injuries. Burns. 1995;21:194–199. [DOI] [PubMed] [Google Scholar]
- 21.Jones JD, Barber B, Engrav L, et al. Alcohol use and burn injury. J Burn Care Rehabil. 1991;12:148–152. [DOI] [PubMed] [Google Scholar]
- 22.Grobmyer SR, Maniscalco SP, Purdue GF, et al. Alcohol, drug intoxication, or both at the time of burn injury as a predictor of complications and mortality in hospitalized patients with burns. J Burn Care Rehabil. 1996;17:532–539. [DOI] [PubMed] [Google Scholar]
- 23.McCampbell B, Wasif N, Rabbitts A, et al. Diabetes and burns: retrospective cohort study. J Burn Care Rehabil. 2002;23:157–166. [DOI] [PubMed] [Google Scholar]
- 24.Tarrier N, Gregg L, Edwards J, et al. The influence of preexisting psychiatric illness on recovery in burn injury patients: the impact of psychosis and depression. Burns. 2005;31:45–49. [DOI] [PubMed] [Google Scholar]


