Abstract
Objective:
To determine long-term quality of life after bilateral adrenalectomy for persistent Cushing's disease after transsphenoidal pituitary tumor resection.
Summary Background Data:
Bilateral adrenalectomy for symptomatic relief of persistent hypercortisolism appears to be an effective treatment option. However, few studies have examined long-term outcomes in this patient population.
Methods:
Retrospective review of 39 patients treated by bilateral laparoscopic adrenalectomy for Cushing's disease from 1994 to 2004. Patients completed a follow-up phone survey, including our Cushing-specific questionnaire and the SF-12v2 health survey. Patients then refrained from taking their steroid replacement for 24 hours, and serum cortisol and ACTH levels were measured.
Results:
Three patients died at 12, 19, and 50 months following surgery from causes unrelated to adrenalectomy. The remaining 36 patients all responded to the study questionnaire (100% response rate). Patients were between 3 months and 10 years post-adrenalectomy. We had zero operative mortalities and a 10.3% morbidity rate. Our incidence of Nelson's syndrome requiring clinical intervention was 8.3%; 89% of patients reported an improvement in their Cushing-related symptoms, and 91.7% would undergo the same treatment again. Twenty of 36 (55%) and 29 of 36 (81%) patients fell within the top two thirds of the national average for physical and mental composite scores, respectively, on the SF-12v2 survey. An undetectable serum cortisol level was found in 79.4% of patients.
Conclusions:
Laparoscopic bilateral adrenalectomy for symptomatic Cushing's disease is a safe and effective treatment option. The majority of patients experience considerable improvement in their Cushing's disease symptoms, and their quality of life equals that of patients initially cured by transsphenoidal pituitary tumor resection.
Bilateral laparoscopic adrenalectomy for refractory Cushing's disease is a safe and effective treatment option. The majority of patients experience considerable improvement in their Cushing's disease symptoms, and their quality of life equals that of patients initially cured by transsphenoidal pituitary tumor resection.
Harvey Cushing first described Cushing's disease (hypercortisolism caused by an ACTH-secreting pituitary adenoma) in 1912 in his book entitled: The Pituitary Body and its Disorders. Endogenous glucocorticoid excess causes devastating sequelae in the patient, including marked central obesity, facial fullness, proximal muscle weakness, hypertension, diabetes, hypogonadism, osteoporosis, mood disorders, and cognitive impairment.1–4 Transsphenoidal pituitary tumor resection is without dispute the best first line treatment option for these patients. Unfortunately, 10% to 30% of patients will fail to achieve long-term remission of their Cushing's disease.5 Four treatment options exist for these patients: 1) repeat transsphenoidal resection, 2) medical therapy, 3) radiation therapy, and 4) bilateral laparoscopic adrenalectomy. Optimum treatment or sequence of different treatments has not yet been established in the literature and often presents a considerable challenge to both the patient and the physician.5
Few studies examine long-term outcomes, including quality of life, in patients requiring additional therapy for persistent Cushing's disease.6,7 At our institution, patients who fail repeated transsphenoidal adenomectomy are offered bilateral laparoscopic adrenalectomy in the hopes of minimizing the adverse effects caused by chronic hypercortisolism.
The purpose of this study was to determine the safety, efficacy, and long-term outcomes in patients who underwent bilateral laparoscopic adrenalectomy for persistent Cushing's disease. We assessed all patients for biochemical cure of their Cushing's disease and evaluated their quality of life with both a general and a Cushing-specific questionnaire.
METHODS
Selection of Patients and Variables
After approval from our Institutional Review Board, all patients who underwent a bilateral laparoscopic adrenalectomy for persistent Cushing's disease were identified from Oregon Health & Science University (OHSU)'s centralized administrative hospital discharge database. As the first laparoscopic adrenalectomy was reported in 1992 by Gagner et al,8 our first patient dates back to November 1994. OHSU is an ideal setting for a study of this nature as there are large neuroendocrine and neurosurgical units subspecializing in Cushing's disease management. Therefore, patients in this study were accrued from direct referral from these 2 units, and include patients from adjacent and remote states as well as from Oregon. Inclusion criteria included: confirmed diagnosis of Cushing's disease, minimum of 3 months follow-up, and bilateral laparoscopic adrenalectomy (BLA) done at OHSU. Our surgical technique has been previously reported6 and is the standard transperitoneal approach in lateral decubitus position. Medical records were reviewed to obtain patient demographics, operative reports, pathologic data, and postoperative events.
A total of 39 patients qualified for our study. Their characteristics at study entry are listed in Table 1. The majority of patients were female (34 of 39), and mean age at time of BLA was 41.5 years. Our follow-up ranged from 3 months to 10 years, with a mean follow-up of 3.6 years following BLA. Three patients died at 12, 19, and 50 months after BLA from cardiac failure (1), pneumonia (1), and stroke (1) as reported by Hawn et al.6 These patients were more than 65 years of age at the time of BLA, and their deaths occurred well outside of the perioperative time period. Patients with Cushing's disease have a high prevalence of atherosclerosis and maintain increased cardiovascular risk even 5 years after cure.2–4
TABLE 1. Patient Characteristics
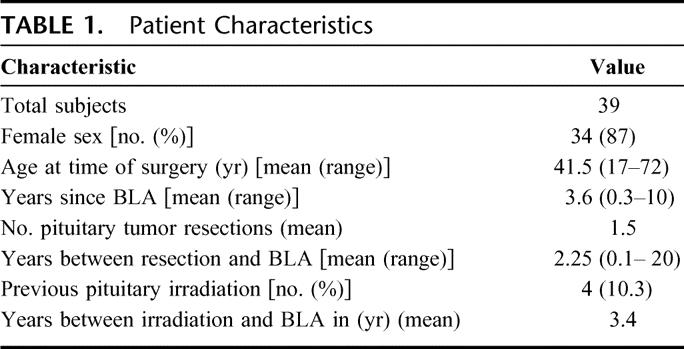
The remaining 36 patients all responded to our phone questionnaire (100% response rate). We achieved a 100% response rate by contacting patient's primary physician, their endocrinologist, and/or their next-of-kin contact (in case of emergency) if a patient was not available at their listed phone number. Thirty-five of 36 patients complied with biochemical testing (97.2% of available study sample). All patients had undergone at least one transsphenoidal pituitary tumor resection, with the mean number of resections calculated at 1.5. Most patients had a time interval of at least 2 years between their last pituitary tumor resection and BLA. Four patients had had failed pituitary irradiation (10.3%).
Study Protocol
Once consented, patients were submitted to a two-step study:
Clinical Study
Patients were asked to complete a two-page phone questionnaire by an independent investigator (A.V.H.) that identified patient's preoperative and postoperative body mass index (BMI), comorbidities, preoperative and postoperative Cushing's disease symptoms, and satisfaction with surgery. Cushing's disease-specific symptoms were subcategorized into 4 categories: physical appearance (9 items), hematologic/immunologic (3 items), comorbidities (3 items), and neuropsychiatric (10 items) (questionnaire available upon request). Patients were asked to describe their symptoms both preoperatively and currently on a linear scale from 1 point (no symptom) to 5 points (extreme symptom). We then calculated the increase or decrease in number of points from preoperatively to the present time. This was reported as a mean increase or decrease in the overall number of points for each category of symptoms. The SF-12v2 questionnaire (QualityMetric Inc, Lincoln, NE) was also administered during the same interview.
Biochemical Study
Patients were instructed to cease their steroid replacement for 24 hours, and then have a morning serum cortisol level drawn to confirm biochemical cure. A serum cortisol level less than 1 μg/dL was considered a “cure.” Any patient who had a level over 1 μg/dL was asked to change their steroid replacement regimen to dexamethasone (0.5 mg orally once a day) and to undergo repeat cortisol level testing. If their serum cortisol levels were still detectable (>1 μg/dL) after continuing on dexamethasone replacement for 3 days, the patients were deemed to have endogenous cortisol production.
Statistical Analysis
SPSS for Windows, version 11.0 (SPSS Inc., Chicago, IL) was used to perform data analysis. Data were expressed as mean (range) or mean ± SD as appropriate. Results from the SF12v2 health survey were compared with published values for the U.S. population using t tests. Postoperative variables associated with an elevated cortisol level were evaluated by bivariate logistic regression.
RESULTS
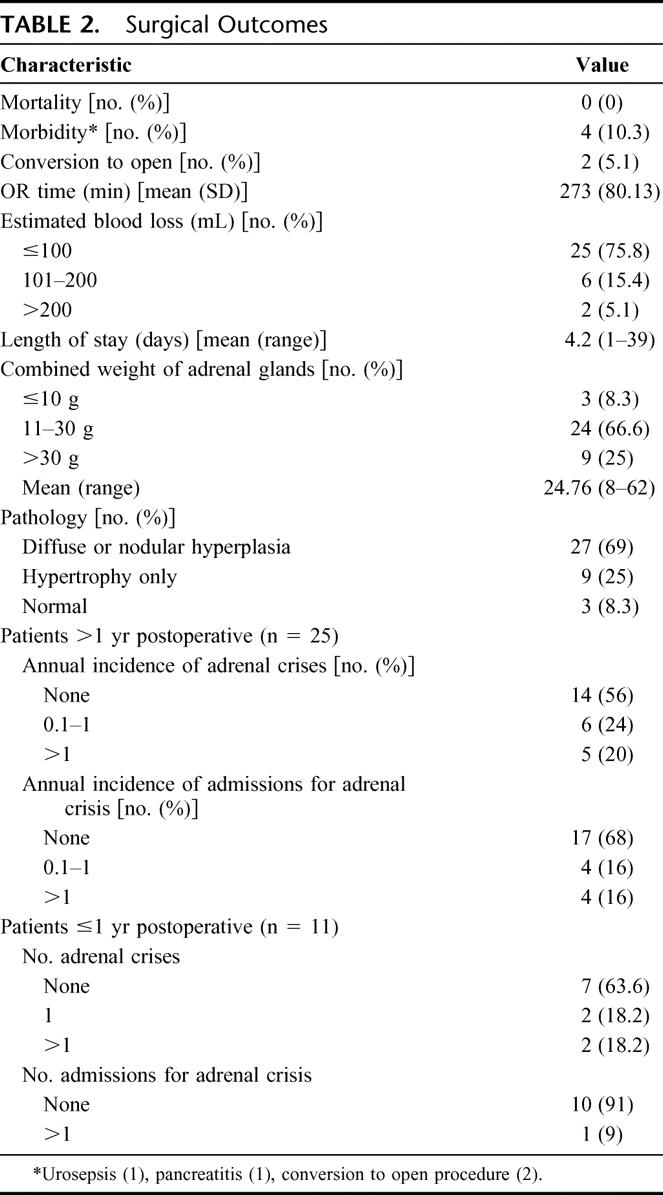
Surgical outcomes are listed in Table 2. We had no surgical mortalities, and 4 of 39 (10.3%) patients had significant complications, including urosepsis, distal pancreatitis, and 2 conversions to an open procedure. One patient was converted for bleeding from a splenic injury, and the second patient was converted to an open procedure for hepatomegaly and inability to visualize the adrenal vein safely. One patient had a minor vena caval injury requiring only pressure to control. Mean operating time was 273 minutes (excluding 35 minutes of repositioning time), and estimated blood loss was less than 100 mL for 25 of 39 (75.8%) patients. Mean length of stay was 4.2 days. Twenty-seven of 39 (69%) adrenal glands showed diffuse or nodular hyperplasia on pathology, while 9 of 39 (25%) adrenal glands were hypertrophic only. Three adrenal glands (8.3%) were normal on pathology. More than 50% of patients had never experienced an adrenal crisis. Approximately 20% had had one adrenal crisis, and the rest had had more than one episode of cortisol insufficiency.
TABLE 2. Surgical Outcomes
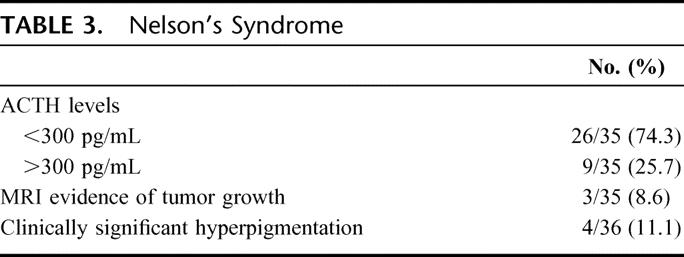
Nelson syndrome is characterized by: 1) growing residual pituitary adenoma, 2) ACTH concentration >300 mg/dL, and 3) hyperpigmentation of the skin following bilateral adrenalectomy.9,10 Twenty-six of 35 patients (74.3%) had a serum ACTH level less than 300 pg/mL and 9/35 patients (25.7%) had an elevated ACTH level (Table 3). Three of 35 patients (8.6%) had MRI evidence of growing residual pituitary adenoma, and 4 of 36 patients (11.1%) complained of significant skin darkening (and an additional 7 of 36 patients, 19.4%, noted mild skin darkening). In our patient population, 3 of 36 (8.3%) required further pituitary surgery or irradiation for some or all of these components of Nelson syndrome.
TABLE 3. Nelson's Syndrome
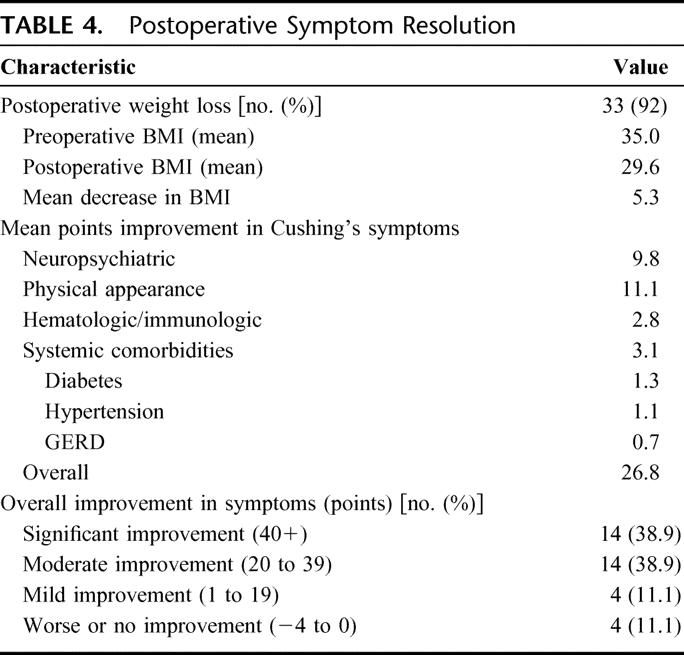
Postoperative Cushing's disease symptom resolution postadrenalectomy is listed in Table 4. Thirty-three of 36 patients (92%) experienced weight loss following BLA, with a mean decrease in BMI from 35 to 29.6. The highest mean points improvement in Cushing symptoms was reported for physical appearance and neuropsychiatric complaints, 11.1 and 9.8 points, respectively. Patients also reported some improvement in their hematologic/immunologic complications and systemic comorbidities, 2.8 and 3.1 points, respectively. Twenty-eight of 36 patients (78%) reported a moderate or significant improvement in their symptoms, while 4 of 36 (11.1%) experienced only mild improvement, and 4 of 36 (11.1%) had no improvement or were worse.
TABLE 4. Postoperative Symptom Resolution
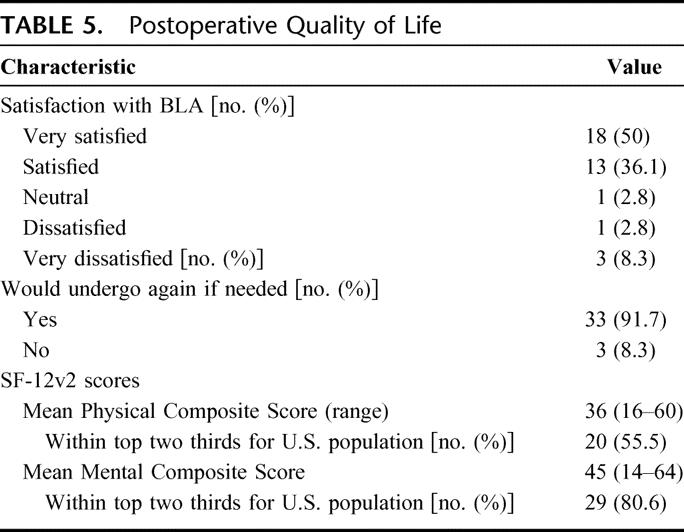
Thirty-one of 36 patients (86.1%) were either satisfied or very satisfied with their BLA (Table 5). Four patients (11.1%) were dissatisfied or very dissatisfied with BLA. An overwhelming 33 of 36 patients (91.7%) said they would undergo the same treatment again if needed. The mean Physical Composite Score for the SF-12v2 was 36 (range, 16–60) compared with 48 for U.S. women 45 to 54 years of age. The mean Mental Composite Score was 45 (range, 14–64) compared with 49 for U.S. women 45 to 54 years of age. Six of 36 patients (16.7%) were above the 50th percentile for U.S. population in physical categories, while 16 of 36 patients (44.4%) were above the 50th percentile in mental categories. Twenty of 36 (56%) and 29 of 36 (81%) patients fell within the top two thirds of the national average for physical and mental composite scores, respectively. By comparison with another chronic disease, namely diabetes, 23 of 36 (64%) and 28 of 36 (78%) of the BLA patients fell within the top two thirds of the diabetic patient average for physical and mental composite scores, respectively.
TABLE 5. Postoperative Quality of Life
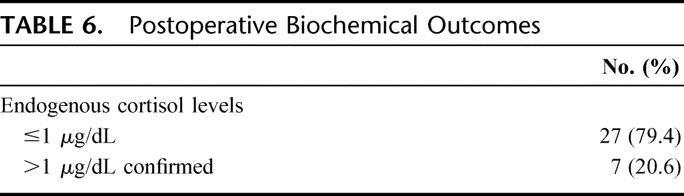
Postoperative biochemical results are listed in Table 6. Twenty-seven of 34 patients (79.4%) had no detectable endogenous cortisol after ceasing exogenous steroids for 24 hours. Seven of 34 patients (20.6%) were confirmed to have endogenous cortisol production with a detectable serum cortisol level after both cessation of steroids for 24 hours and after 3 days of dexamethasone.
TABLE 6. Postoperative Biochemical Outcomes
DISCUSSION
The main objective of this study was to evaluate quality of life (QOL) after bilateral laparoscopic adrenalectomy for persistent Cushing's disease. Thirty-nine patients have had this therapy for chronic hypercortisolism over the past 10 years at OHSU and, of those patients still alive, we had a 100% response rate. To our knowledge, this is the largest series of long-term follow-up of patients with persistent Cushing's disease treated by BLA. The degree of willingness of this patient group to assist the medical community in studying this disease likely reflects the impact Cushing's disease has had on these patients and the enormity of the decisions they have had to make regarding their health over the course of their disease.
Our center published preliminary QOL results on our initial 18 patients.6 In this study, there was a 66% response rate, and scores on all 8 parameters of the SF-36 were significantly reduced from general population values. We significantly improved our response rate by doing telephone surveys as opposed to mail-out questionnaires, and by contacting all those necessary to locate a “missing patient.” In the present study, we though it would be more representative to compare our patient's SF-12 values to U.S. women 45 to 54 years of age as well as to patients with diabetes (a patient population also with a chronic disease). In both cases, Cushing's disease patients that are treated with BLA have significant improvement in their Cushing-related problems and most have regained a relatively normal QOL. Furthermore, we created a Cushing-specific symptom questionnaire as there is no disease-specific QOL questionnaire available for Cushing's disease. This Cushing-specific questionnaire shows that 89% of patients experience improvement in their symptoms after BLA and, consequently, marked improvement in their QOL.
The results of this study show that, while the mean physical composite score was significantly lower than that of age- and gender-matched U.S. citizens (36 vs. 48), the mean mental composite score was close to that of U.S. women 45 to 54 years of age (45 vs. 49). A recent paper by van Aken et al7 reports similar findings in patients successfully treated by transsphenoidal surgery. They found, using 4 different questionnaires including the SF-36, that several aspects of QOL are reduced, particularly in areas of physical ability. It would seem, therefore, that patients who undergo BLA for persistent Cushing's disease have, at the very least, an equal QOL to those patients who are successfully treated by initial transsphenoidal pituitary tumor resection.
Two other findings are worthy of discussion in this study. First, the surgical outcomes for these patients were favorable, with zero mortalities, and a 10% morbidity rate. Our operative times (mean, 273 minutes), and length of stay (mean, 4.2 days) were longer than most other series of laparoscopic adrenalectomies.11,12 However, this can be explained by a Canadian study that compared surgical outcomes in 3 different categories of patients13: 1) Cushing's disease, 2) pheochromocytoma, and 3) unilateral adrenalectomy for nonpheochromocytoma. Poulin et al13 found that patients in the first group had longer operating time (median, 255 minutes) and a long postoperative stay (median, 4 days). This is likely secondary to the high BMI of this patient population and the added operative time inherent in repositioning the patient. The extended postoperative stay is in part due to the need to establish homeostasis in fluids and electrolytes following removal of both adrenal glands. It is also due to the need for steroid taper and regulation, as well as the delayed healing these patients experience due to the catabolic nature of cortisol. Our results show that this is a safe, effective option for patients with persistent Cushing's disease after transsphenoidal pituitary tumor resection.
Second, approximately 20% of our study sample had evidence of endogenous cortisol production following BLA. Evidence of detectable cortisol levels after BLA is reportedly rare; however, there is a paucity of literature on this subject. Possible etiologies include incomplete adrenal resection or functional ectopic adrenal remnants in the adrenal fossa or elsewhere. In 2 patients undergoing BLA for Cushing's disease (from this current series), we have documented extracortical adrenal tissue remote from the adrenal gland in the retroperitoneal fat. Since then, we have changed our operative conduct to include complete removal of the retroperitoneal fat in the adrenal bed to avoid inadvertently leaving behind extracortical adrenal tissue. Since changing our technique, we have identified one other patient with an extracortical adrenal rest in the left adrenal fossa.
We have also done reoperative laparoscopic explorations in 2 of 7 patients with detectable serum cortisol levels, clinical evidence of hypercortisolism (and subsequent loss of postoperative need for steroid replacement), and positive NP-59 radioscintigraphy scans. The source of alleged endogenous cortisol production, as directed by NP-59 scanning, was in the adrenal fossa in one patient and on the left ovary in the second patient. Pathology demonstrated only fibrous tissue. The source of cortisol production following BLA remains to be determined and will be the subject of future investigation. We currently do not advise routine reexploration for symptomatic endogenous cortisol production without a positive NP-59 scan.
The present study does have one important limitation. We do not have preoperative QOL surveys on the majority of our patients. Therefore, we are relying on patients to remember their preoperative status and compare it with their current state of health. However, bias toward the patient feeling obliged to report a positive outcome was avoided by using an independent investigator (A.V.H.) with no involvement in the patient's perioperative care to complete all telephone questionnaires. As well, there was no variation in response according to time interval between BLA and our study or between number of preoperative transsphenoidal treatments and BLA, suggesting that memory (or lack thereof) is not an independent predictor of postoperative improvement.
CONCLUSION
Our study shows that BLA for persistent Cushing's disease provides patients with considerable improvement in their Cushing-related symptoms with concordant increase in their quality of life. After BLA, patients may attain the same (or better) quality of life as patients initially cured by transsphenoidal pituitary tumor resection. We think that BLA is a safe and effective treatment of the 10% to 30% of patients who fail initial therapy for Cushing's disease, and should be considered preferentially over other available therapies.
ACKNOWLEDGMENTS
The authors thank Karin Miller and Chris Yedinak for all their help in coordinating and collecting biochemical data on our patients.
Footnotes
Reprints: Brett C. Sheppard, MD, Department of Surgery, Oregon Health & Science University, Mail Code: L223A, Portland, OR 97239. E-mail: sheppard@ohsu.edu.
REFERENCES
- 1.Di Somma C, Pivonella R, Loche S, et al. Effect of 2 years of cortisol normalization on the impaired bone mass and turnover in adolescent and adult patients with Cushing's disease: a prospective study. Clin Endocrinol. 2003;58:302–308. [DOI] [PubMed] [Google Scholar]
- 2.Colao A, Pivonello R, Spiezia S, et al. Persistence of increased cardiovascular risk in patients with Cushing's disease after five years of successful cure. J Clin Endocrinol Metab. 1999;84:2664–2672. [DOI] [PubMed] [Google Scholar]
- 3.Faggiano A, Pivonello R, Spiezia S, et al. Cardiovascular risk factors and common carotid artery caliber and stiffness in patients with Cushing's disease during active disease and 1 year after disease remission. J Clin Endocrinol Metab. 2003;88:2527–2533. [DOI] [PubMed] [Google Scholar]
- 4.Albiger N, Testa RM, Almoto B, et al. Patients with Cushing's syndrome have increased intimal media thickness at different vascular levels: comparison with a population matched for similar cardiovascular risk factors. Horm Metab Res. 2006;38:405–410. [DOI] [PubMed] [Google Scholar]
- 5.Locatelli M, Vance ML, Laws ER. The strategy of immediate reoperation for transsphenoidal surgery for Cushing's disease [Clinical Review]. J Clin Endocrinol Metab. 2005;90:5478–5482. [DOI] [PubMed] [Google Scholar]
- 6.Hawn MT, Cook D, Deveney C, et al. Quality of life after laparoscopic bilateral adrenalectomy for Cushing's disease. Surgery. 2002;132:1064–1069. [DOI] [PubMed] [Google Scholar]
- 7.van Aken MO, Pereira AM, Biermasz NR, et al. Quality of life in patients after long-term biochemical cure of Cushing's disease. J Clin Endocrinol Metab. 2005;90:3279–3286. [DOI] [PubMed] [Google Scholar]
- 8.Gagner M, Lacroix A, Prinz RA, et al. Early experiences with laparoscopic approach for adrenalectomy. Surgery. 1993;114:1120–1124. [PubMed] [Google Scholar]
- 9.van Aken MO, Pereira AM, van den Berg G, et al. Profound amplification of secretory-burst mass and anomalous regularity of ACTH secretory process in patients with Nelson's syndrome compared with Cushing's disease. Clin Endocrin. 2004;60:765–772. [DOI] [PubMed] [Google Scholar]
- 10.Assie G, Bahurel H, Bertherat J, et al. The Nelson's syndrome … revisited. Pituitary. 2004;7:209–215. [DOI] [PubMed] [Google Scholar]
- 11.Zeh HJ, Udelsman R. One hundred laparoscopic adrenalectomies: a single surgeon's experience. Ann Surg Oncol. 2003;10:1012–1017. [DOI] [PubMed] [Google Scholar]
- 12.Gagner M, Pomp A, Heniford BT, et al. Laparoscopic adrenalectomy: lessons learned form 100 consecutive procedures. Ann Surg. 1997;226:238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poulin EC, Schlachta CM, Burpee SE, et al. Laparoscopic adrenalectomy: pathologic features determine outcome. Can J Surg. 2003;46:340–344. [PMC free article] [PubMed] [Google Scholar]


