Abstract
Background
Many people with diabetes continue to smoke despite being at high risk of cardiovascular disease. We examined the impact of a pay-for-performance incentive in the United Kingdom introduced in 2004 as part of the new general practitioner contract to improve support for smoking cessation and to reduce the prevalence of smoking among people with chronic diseases such as diabetes.
Methods
We performed a population-based longitudinal study of the recorded delivery of cessation advice and the prevalence of smoking using electronic records of patients with diabetes obtained from participating general practices. The survey was carried out in an ethnically diverse part of southwest London before (June–October 2003) and after (November 2005–January 2006) the introduction of a pay-for-performance incentive.
Results
Significantly more patients with diabetes had their smoking status ever recorded in 2005 than in 2003 (98.8% v. 90.0%, p <0.001). The proportion of patients with documented smoking cessation advice also increased significantly over this period, from 48.0% to 83.5% (p < 0.001). The prevalence of smoking decreased significantly from 20.0% to 16.2% (p < 0.001). The reduction over the study period was lower among women (adjusted odds ratio 0.71, 95% confidence interval 0.53–0.95) but was not significantly different in the most and least affluent groups. In 2005, smoking rates continued to differ significantly with age (10.6%–25.1%), sex (women, 11.5%; men, 20.6%) and ethnic background (4.9%–24.9%).
Interpretation
The introduction of a pay-for-performance incentive in the United Kingdom increased the provision of support for smoking cessation and was associated with a reduction in smoking prevalence among patients with diabetes in primary health care settings. Health care planners in other countries may wish to consider introducing similar incentive schemes for primary care physicians.
Diabetes is a growing public health concern worldwide, with prevalence rates increasing rapidly in most regions.1 People with diabetes experience considerably worse health outcomes and have a shorter life expectancy than the general population. This is largely attributable to a 2–4 times greater risk of cardiovascular disease, which accounts for two-thirds of deaths among people with diabetes.2–4
Smoking is an important modifiable risk factor for cardiovascular disease and microvascular complications in people with diabetes.5 Smoking also contributes to inequalities in diabetes outcomes and explains in part the variations in mortality between socioeconomic groups.6 Despite being at an increased risk of cardiovascular disease, many people with diabetes smoke, with the rate of smoking among people with diabetes approaching the rate in the general population.7,8
Comprehensive tobacco control strategies have been an integral component of public health policy in the United Kingdom, North America and Australia for many years.9–11 These strategies aim to reduce overall tobacco use and exposure and include interventions targeted at groups with high smoking rates, including young people, those of low socio-economic status and ethnic minorities. As part of these efforts, the UK government established a universal smoking cessation service (which combines psychological support and medication) for smokers who would like to quit. An important component of this service is the delivery of brief cessation advice and referral to “stop smoking clinics” by primary health care providers. However, despite evidence that cessation advice improves quit rates,12–14 studies have shown that primary health care providers are not routinely offering cessation advice during consultations.15,16 A systematic review published in 2005 suggested that this may be partly due to negative views held by some practitioners about discussing smoking with their patients.17 Vogt and colleagues17 found that many general practitioners felt that such discussions were too time consuming (42%) or were not effective (38%), or that they lacked the required skills to provide smoking cessation advice (22%).
Pay-for-performance incentives have been proposed as a method to improve the quality of care received by patients.18,19 Quality targets to identify and counsel patients with chronic disease who smoke were introduced in the United Kingdom as part of the new general practitioner contract in April 2004.20 These targets form part of one of the most radical shifts toward pay-for-performance seen in any health care setting. About one-quarter of general practice income is currently derived through the achievement of quality targets in managing chronic diseases such as diabetes and coronary artery disease. Six of the 10 disease indicator areas in the contract have a smoking cessation component, accounting for 13% (74/550) of points available in the clinical quality indicators.
In this article, we present the findings of a population-based longitudinal study that examined the impact of a pay-for-performance incentive on support for smoking cessation and on smoking prevalence among people with diabetes in a multiethnic population.
Methods
Diabetes was 1 of 10 disease indicator areas within the clinical domain of the Quality and Outcomes Framework in the United Kingdom's general practitioner contract of April 2004 (the number of indicator areas was increased to 19 when the contract was revised in April 2006). Of the 99 points available for diabetes care, 50 are allocated for the achievement of treatment targets (blood pressure ≤ 145/85 mm Hg [17 points], glycosylated hemoglobin ≤ 7.4% [16 points], glycosylated hemoglobin ≤ 10% [11 points], cholesterol ≤ 5 mmol/L [6 points]). The remaining points are awarded for the recording of 14 process measures of care. These mea-sures of care include Diabetes Mellitus Indicator 3 (the proportion of patients with diabetes for whom there is a record of smoking status in the previous 15 months, except those who have never smoked, for whom smoking status should be recorded once [3 points]) and Diabetes Mellitus Indicator 4 (the proportion of patients with diabetes who smoke and whose notes contain a record that smoking cessation advice has been offered in the last 15 months [5 points]).
Wandsworth Primary Care Trust, located in southwest London, England, has established comprehensive primary care-based diabetes registers. Data for the Wandsworth Prospective Diabetes Study were collected before (June–October 2003) and after (November 2005–January 2006) the introduction of the new general practitioner contract in April 2004. Ethical approval for the study was granted by the Wandsworth Local Research Ethics Committee.
The study area contains 36 primary care practices and has a total registered population of 243 519. The population of the Wandsworth borough is younger than the average population of England; 74% of people in Wandsworth are under 45 years of age (compared with 60% nationally). About 1 in 5 Wandsworth residents (22%) belongs to a nonwhite ethnic group, and this borough has higher levels of socioeconomic deprivation relative to elsewhere in England.21
The methods used to develop our register of patients with diabetes in Wandsworth have been described previously.22 In brief, we asked all practices in the study area to participate. We identified all patients with type 1 or type 2 diabetes by searching computerized general practice records for “read codes” for diagnoses of diabetes (C10) or diabetes care (66A). [Read codes are the clinical classification system used in primary care in the United Kingdom.23] Patients who received repeat prescriptions for diabetic medications or whose glycosylated hemoglobin level was greater than 7.5% were also included in our study. Patients under 18 years of age and women with gestational diabetes or who received treatment for polycystic ovarian syndrome rather than diabetes were excluded. A unique patient identifier (National Health Service number) was used to link the patient records collected in both of the study periods.
We examined smoking status and cessation advice based on information recorded on practice computers during the 2003 and 2005 study periods. Patients self-identified their ethnic background (at registration or during a consultation) from closed categories based on the classifications used in the 2001 UK census.24 Socioeconomic status was assigned to individual patients based on their postal code using the 2004 Index of Multiple Deprivation.21 This index is the most commonly used method to determine neighbourhood socioeconomic status in the United Kingdom and is compiled from a variety of sources, including the 2001 UK census, and unemployment and social security benefit records. Patients were grouped into deprivation fifths; patients in group 1 resided in the least deprived areas, and those in group 5 resided in the most deprived areas.
Our statistical analyses were influenced by the study design, which included repeated measurements and practice-level clustering of participants. Therefore, we used the McNemar test to examine differences in the frequency distributions of indicators between 2003 and 2005. Intrapractice correlations for different variables were: recording of smoking status (2003, 0.10, 95% confidence intervals [CI] 0.05–0.16; 2005, 0.03, 95% CI 0.01–0.04), smoking cessation advice (2003, 0.05, 95% CI 0.02–0.08; 2005, 0.01, 95% CI 0.00–0.02) and actual smoking status (2003, 0.16, 95% CI, 0.05–0.26; 2005, 0.14, 95% CI 0.05–0.23).
We used conditional logistic regression with practice as the clustering variable to determine the association of the indicator variables with age, sex, ethnic background and deprivation group. Changes in achievement between the 2 study periods were assessed by conditioning 2005 achievements on 2003 achievements. All standard errors were robust to account for the clustering of patients within general practices.25 An adjusted odds ratio of >1 indicates that recording of smoking status, provision of cessation advice or prevalence of smoking was greater than in the reference group after adjusting for age, sex, ethnic background, deprivation group and practice level clustering.
Results
The European age-standardized prevalence of diabetes increased from 36.3 to 42.2 per 1000 population in all age groups between 2003 and 2005.26 Of the 36 practices in the study area, 32 agreed to participate in the study. We identified 4284 adults (≥ 18 years) with diabetes who were registered with the 32 practices in both the 2003 and 2005 study periods (2227 men, 2057 women). The percentage of missing data in patient records was low (2.9%). We therefore restricted our analyses to records with complete information; thus, missing data had little effect on our conclusions. The 4 practices that did not participate in our study accounted for less than 6% of the registered population in the study area. The practices that did not participate were smaller (3 had fewer than 3000 patients) and were located in more deprived areas than the participating practices.
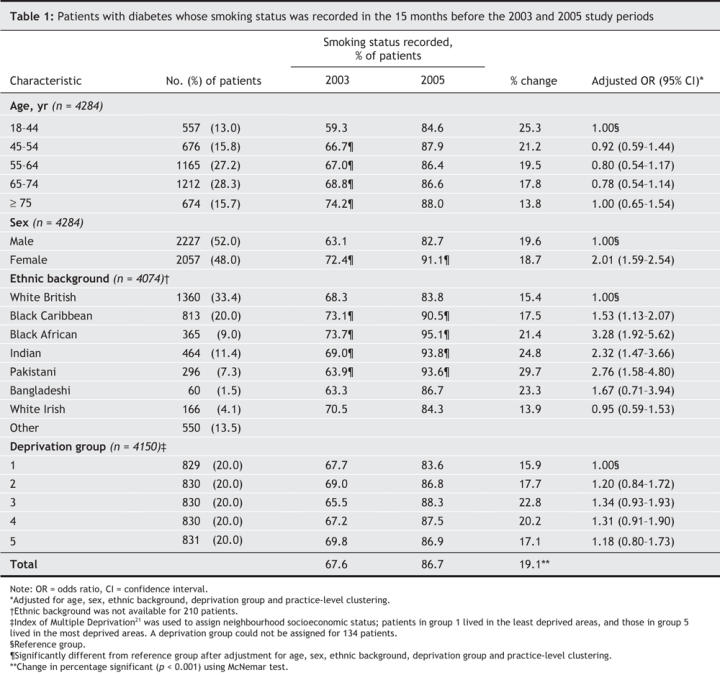
Smoking status was significantly more likely to be ever recorded in 2005 than in 2003 (98.8% v. 90.0%, p < 0.001). The proportion of patients whose smoking status was recorded in the 15 months before the study period was also greater in 2005 than in 2003 (86.7% v. 67.6%, p < 0.001, Table 1). The greatest improvements in the recording of smoking status were observed among women and nonwhite ethnic groups (except Bangladeshi) after adjustment for age, sex, ethnic background, deprivation status and practice-level clustering. The lower recording of smoking status in 2003 among men and among the white British, white Irish and Bangladeshi groups was not attenuated in 2005. However, lower recording of smoking status in 2003 among younger adult patients (18–44 years) was attenuated in 2005.
Table 1
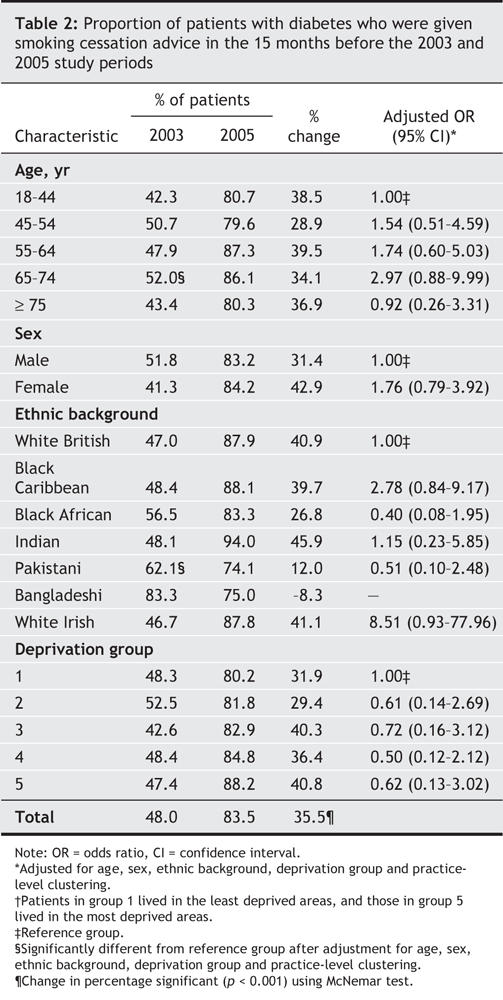
The proportion of patients with documented smoking cessation advice increased from 48.0% in 2003 to 83.5% in 2005 (p < 0.001, Table 2). This increase was not influenced by age, sex, ethnic background or deprivation status. The variation in the provision of smoking cessation advice evident between age and ethnic groups in 2003 was attenuated in 2005.
Table 2
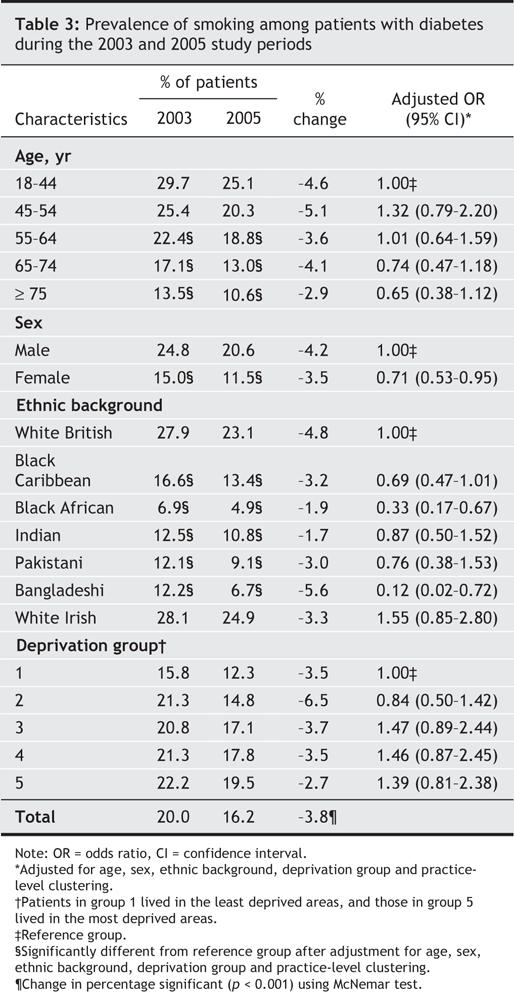
The prevalence of smoking among patients with diabetes decreased significantly from 20.0% in 2003 and to 16.2% in 2005 (p < 0.001, Table 3). Reductions in smoking prevalence were lower among women than among men (adjusted odds ratio 0.71, 95% CI 0.53–0.95) and lower in the black African and Bangladeshi groups than in the white British group. In 2005, the smoking rates differed significantly with age (10.6%–25.1%), sex (women, 11.5%; men, 20.6%) and ethnic background (4.9%–24.9%). The higher smoking rates observed in 2003 among younger adults (18–44 years), men and in both the white British and white Irish groups were not attenuated in 2005.
Table 3
Interpretation
Our study showed that the implementation of a pay-for-performance initiative in the United Kingdom increased the provision of support for smokers with diabetes in primary care settings. Both the recording of smoking status and the documented delivery of smoking cessation advice increased significantly between 2003 and 2005. The prevalence of smoking decreased significantly over this period, although these reductions were lower among women than among men.
The effectiveness of smoking cessation interventions in primary care has been demonstrated through randomized controlled trials in both the general population and among people with diabetes.12–14,27 However, few studies have examined whether such interventions have a differential impact across socioeconomic and ethnic groups and whether such an effect contributes to health inequalities.12 We found no evidence to suggest that pay-for-performance incentives increased variation in support for smokers and smoking rates across key demographic variables such as age, sex, ethnic background and deprivation status.
Evaluating the effectiveness of pay-for-performance programs is important given that previous studies have suggested that the rate of smoking among patients with diabetes is similar to the rate in the general population and may not have declined in recent years. For example, the prevalence of smoking in the United States among adults with diabetes remained virtually static between 1988–1994 (16.3%) and 1999–2000 (15.9%).28 Similarly, in Sweden the prevalence of smoking among patients with diabetes who were less than 60 years of age increased slightly, from 21.5% in 1996 to 23.8% in 2003.29 A recent British study found that the prevalence of smoking among white Europeans with diabetes (men, 22.2%; women, 20.0%) was similar to the prevalence in the general population.8 Our findings indicate that smoking rates are comparable among people with and without diabetes within many ethnic minority communities in Britain.30
Most previous studies that compared smoking prevalence over time used data from 2 or more cross-sectional surveys of groups of patients that may systematically differ.28,29 We are cautious in attributing the changes observed in our study to pay-for-performance incentives given the limitations of our study design. Some of the reduction in smoking prevalence may have been attributable to other cessation interventions, to improved recording of smoking status or to a secular trend of reduced tobacco use. The new contract for general practitioners in the United Kingdom was introduced nationally; thus, evaluation of its impact by more rigorously designed studies, such as randomized controlled trials, was not feasible. We were unable to confirm smoking status using objective methods such as salivary cotinine measurement, because these methods are not in routine use in clinical practice in the United Kingdom. We were also unable to assess the quality of cessation advice that was offered. All but 4 practices in the study area participated in our survey. Hence, our findings are representative of the care provided in this diverse, inner-city location.
Pay-for-performance incentives appear to be effective in increasing the delivery of cessation advice given by primary care physicians and in reducing the prevalence of smoking among patients with diabetes. However, financial incentives are likely to be most effective in reducing the prevalence of smoking when combined with other quality improvement initiatives within a comprehensive tobacco control strategy. These other initiatives include active dissemination of clinical guidelines on smoking cessation, such as those recently published in the United Kingdom,31 and ongoing training and support for front-line staff. Health care planners in other countries may wish to consider the introduction of similar pay-for-performance incentives for primary care physicians.
@ See related article page 1717
Acknowledgments
The Wandsworth Primary Care Research Centre is funded by the UK Department of Health. Sonia Saxena holds a National Postdoctoral Award from the UK Department of Health Research Capacity Development Program. We thank the practices that participated in the study.
Footnotes
This article has been peer reviewed.
Contributors: Christopher Millett conceived the study. He and Gopalakrishnan Netuveli performed the statistical analyses. All of the authors contributed to the data interpretation. Christopher Millett wrote the first draft of the manuscript and all of the authors contributed to revising it and approved the final version.
Competing interests: None declared for Christopher Millett, Jeremy Gray, Sonia Saxena and Gopalakrishnan Netuveli. Azeem Majeed is Associate Director of the English Diabetes Research Network.
Correspondence to: Christopher Millett, Specialist Trainee in Public Health, Department of Primary Care and Social Medicine, 3rd floor, Reynolds Building, Imperial College Faculty of Medicine, St Dunstan's Road, London UK W6 8RP; fax 44 20 7594 0866; c.millett@imperial.ac.uk
REFERENCES
- 1.International Diabetes Federation. Diabetes Atlas: prevalence. Brussels: The Federation; 2005. Available: www.eatlas.idf.org/prevalence (accessed 2007 Mar 26).
- 2.Garcia M, McNamara P, Gordon T, et al. Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow up. Diabetes 1974;23:105-11. [DOI] [PubMed]
- 3.Geiss L, Herman W, Smith P. Mortality in non-insulin-dependent diabetes. NIH Pub no 95-1468. In: National Diabetes Data Group. Diabetes in America. 2nd ed. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health; 1995. p. 233–58.
- 4.Abraham W. Preventing cardiovascular events in patients with diabetes mellitus. Am J Med 2004;116(Suppl 5A):39S-46S. [DOI] [PubMed]
- 5.Turner R, Millns H, Neil H, et al. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom prospective diabetes study (UKPDS:23). BMJ 1998;316:823-8. [DOI] [PMC free article] [PubMed]
- 6.Chaturvedi N, Jarrett J, Shipley M, et al. Socioeconomic gradient in morbidity and mortality in people with diabetes: cohort study findings from the Whitehall study and the WHO multinational study of vascular disease in diabetes. BMJ 1998;316:100-6. [DOI] [PMC free article] [PubMed]
- 7.Malarcher A, Ford E, Nelson D, et al. Trends in cigarette smoking and physicians' advice to quit smoking among people with diabetes in the US. Diabetes Care 1995;18:694-7. [DOI] [PubMed]
- 8.Gulliford M, Sedgwick J, Pearce A. Cigarette smoking, health status, socio-economic status and access to health care in diabetes mellitus: a cross-sectional study. BMC Health Serv Res 2003;3:4. [DOI] [PMC free article] [PubMed]
- 9.UK Department of Health. Smoking kills: a white paper on tobacco. London (UK): The Department; 1998. Available: www.archive.official-documents.co.uk/document/cm41/4177/4177.htm (accessed 2007 Mar 26).
- 10.The Federal Tobacco Control Strategy (FTCS): a framework for action. Ottawa: Health Canada; 2002. Available: www.hc-sc.gc.ca/hl-vs/pubs/tobac-tabac/ffa-ca/introduction_e.html (accessed 2007 Mar 26).
- 11.Ministerial Council on Drug Strategy, Australian Government Department of Health and Ageing. National tobacco strategy 2004–2009: the strategy. Canberra: Commonwealth of Australia; 2005. Available: www.health.gov.au/internet/wcms/publishing.nsf/content/E955EA2B5D178432CA256FD30017A522/$File/tobccstrat2.pdf (accessed 2007 Mar 26).
- 12.Health Development Agency. Smoking and public health: a review of reviews of interventions to increase smoking cessation, reduce smoking initiation and prevent further uptake of smoking. London (UK): National Health Service; 2004. Available: www.nice.org.uk/page.aspx?o=502729 (accessed 2007 Mar 26).
- 13.NIH State-of-the-Science Panel. National Institutes of Health State-of-the-Science conference statement: tobacco use: prevention, cessation, and control. Ann Intern Med 2006;145:839-44. [DOI] [PubMed]
- 14.Ranney L, Melvin C, Lux L, et al. Systematic review: smoking cessation intervention strategies for adults and adults in special populations. Ann Intern Med 2006;145:845-56. [DOI] [PubMed]
- 15.Coleman T, Wynn A, Barrett S, et al. Discussion of NRT and other antismoking interventions in UK general practitioners' routine consultations. Nicotine Tob Res 2003;5:163-8. [DOI] [PubMed]
- 16.Ellerbeck E, Choi W, McCarter K, et al. Impact of patient characteristics on physician's smoking cessation strategies. Prev Med 2003;36:464-70. [DOI] [PubMed]
- 17.Vogt F, Hall S, Marteau T. General practitioners' and family physicians' negative beliefs and attitudes towards discussing smoking cessation with patients: a systematic review. Addiction 2005;100:1423-31. [DOI] [PubMed]
- 18.Pink G, Brown A, Studer M, et al. Pay-for-performance in publicly financed healthcare: some international experience and considerations for Canada. Healthc Pap. 2006;6:8-26. [DOI] [PubMed]
- 19.Petersen L, Woodard L, Urech T, et al. Does pay-for-performance improve the quality of health care? Ann Intern Med 2006;145:265-72. [DOI] [PubMed]
- 20.British Medical Association. General Medical Services contract. Available: www.bma.org.uk/ap.nsf/Content/Hubthenewgmscontract (accessed 2007 Mar 26).
- 21.Social Disadvantage Research Centre. Index of multiple deprivation 2004. London (UK): University of Oxford; 2004. Available: www.communities.gov.uk/index.asp?id=1128444 (accessed 2007 Mar 26).
- 22.Gray J, Orr D, Majeed A. Use of Read codes in diabetes management in a south London primary care group: implications for establishing disease registers. BMJ 2003;326:1130-3. [DOI] [PMC free article] [PubMed]
- 23.Information Authority. Clinical terms (the read codes) version 3 reference manual. United Kingdom: National Health Service; 2000. Available: www.connectingforhealth.nhs.uk/terminology/readcodes/publications (accessed 2007 Mar 26).
- 24.UK 2001 Census. Available: www.statistics.gov.uk/census2001/profiles/commentaries/ethnicity.asp (accessed 2007 April 30).
- 25.Huber P. The behavior of maximum likelihood estimates under nonstandard conditions. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability; June 21–July 18 1965, Dec 27 1965–Jan 7 1966; Berkeley (CA). Berkeley (CA): University of California Press; 1967. p. 221–3.
- 26.World Health Organization (WHO). World health statistics annual 1989. Geneva: WHO 1990.
- 27.Canga N, De Irala J, Vara E, et al. Intervention study for smoking cessation in diabetic patients. A randomized controlled trial in both clinical and primary care settings. Diabetes Care 2000;23:1455-60. [DOI] [PubMed]
- 28.Saydah S, Fradkin J, Cowie C. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004;291:335-42. [DOI] [PubMed]
- 29.Eliasson B, Cederholm J, Nilsson P, et al. The gap between guidelines and reality: type 2 diabetes in a national diabetes register 1996-2003. Diabet Med 2005;22:1420- 6. [DOI] [PubMed]
- 30.Health and Social Care Information Centre. Health survey for England 2004. Health of ethnic minorities. London (UK): National Health Service; 2005. Available: www.ic.nhs.uk/pubs/hlthsvyeng2004ethnic (accessed 2007 Mar 26).
- 31.National Institute for Health and Clinical Excellence. Brief interventions and referral for smoking cessation in primary care and other settings. London (UK): National Health Service; 2006. Available: www.nice.org.uk/download.aspx?o=299608 (accessed 2007 Mar 26).


