Abstract
Objective: To study the diagnosis and treatment of pheochromocytoma in urinary bladder. Methods: Six cases of bladder pheochromocytoma were studied. Four cases showed hypertension, 3 of which were paroxysmal hypertension during urination. Catecholamine (CA) was increased in a case, and vanillymandelic acid (VMA) was increased in 2 cases. Bladder submucosal mass was detected by B-ultrasound in 5 cases (5/5), computerized tomography (CT) in 3 cases (3/3), cystoscopy in 5 cases (5/6). Four cases took α-receptor blocker for 2 weeks, 1 case took β-receptor blocker to decrease heart rate. All patients were treated with surgical operation including 4 partial cystectomies, 2 excavations. Results: Three cases had manifestations including headache, excessive perspiration and hypertension during cystoscopy. Four cases were confirmed before operation. Two cases showed hypertension during operation. All patients were pathologically diagnosed as pheochromocytoma postoperatively. In five cases followed up, blood pressure returned to normal. No patient had relapse and malignancy. Conclusions: Typical hypertension during urination comprised the main symptoms. We should highly suspect bladder pheochromocytoma if a submucosal mass was discovered with B-ultrasound, CT, 131I-MIBG (methyliodobenzylguanidine) and cystoscopy. The determination of CA in urine is valuable for qualitative diagnosis. The preoperative management of controlling blood pressure and expansion of the blood volume are very important. Surgical operation is a good method for effective treatment. Postoperative long-time followed up is necessary.
Keywords: Urinary bladder, Pheochromocytoma, Diagnosis, Therapeutics
INTRODUCTION
Pheochromocytoma is a neoplasm, which develops from cells of the chromaffin tissues that are derived from the ectodermic neural system and mostly situated within the adrenal medulla. Only approximate 15% pheochromocytoma develops from extra-adrenal chromaffin tissue, in which pheochromocytoma of the bladder is rare and accounts for less than 0.06% of all bladder neoplasm and less than 1% of all pheochromocytoma. We treated 226 cases of pheochromocytoma from Jan. 1988 to Dec. 2006, in which extra-adrenal pheochromocytoma are 31 cases, including 6 cases of bladder pheochromocytoma. We report and analyze clinical manifestation, diagnosis and treatment in 6 cases of bladder pheochromocytoma.
MATERIALS AND METHODS
Clinical patients
There were 6 cases (male 1, female 5). The average age was 36 (range 19 to 53) and the courses of disease ranged from 4 d to 1.5 years. Four cases had a history of paroxysmal hypertension, 3 cases suffered from headaches and dizziness during urination, the highest blood pressure was 190/105 mmHg. Two cases’ blood pressure decreased after urination, 1 case’s blood pressure decreased after taking hypotensive drugs, 1 case presented hypertension during bimanual examination, 1 case was associated with gross hematuria, 2 cases were associated with microscopic hematuria and 1 case had difficulty of urination. Two cases were found during physical examination, 5 cases were detected by B-ultrasound, 3 cases in trigone, 1 case in neck, 1 case in right lateral wall, and the tumors appeared as a submucosal mass, which turned into bladder like hemispheroid, with clear outline, smooth surface, continuous mucosa, and abundant blood. Three cases were detected by computerized tomography (CT) and the tumors appeared as a round mass covered by intact urothelium with smooth capsules. Six cases were detected by cystoscopy, of which 5 cases appeared as globular submucosa mass protruding prominently into bladder, 3 cases appeared as abundant blood in the mucosa surface, 2 cases appeared as normal mucosa. During cystoscopy, 3 cases showed increasing blood pressure, headache, dizziness, palpitation, with highest blood pressure being 195/110 mmHg, 2 cases’ symptoms were relieved and their blood pressure decreased gradually after the cystoscopy, 1 case’s blood pressure decreased after taking phenoxybenzamine. All of the six cases were not detected by biopsy. Catecholamine (CA) was increased in a case and vanillymandelic acid (VMA) was increased in 2 of three patients who underwent the test.
Therapies
Four cases were treated with preoperative phenoxybenzamine (30~45 mg/d) for two weeks. Of the 4 cases, 1 case’s blood pressure did not decrease prominently, whose pressure was controlled between 140~160 and 70~90 mmHg after taking captopril; 1 case presented tachycardia, with heart rate controlled under 90 min−1 after taking propranolol. The other 2 cases did not receive the preparation because they were not confirmed.
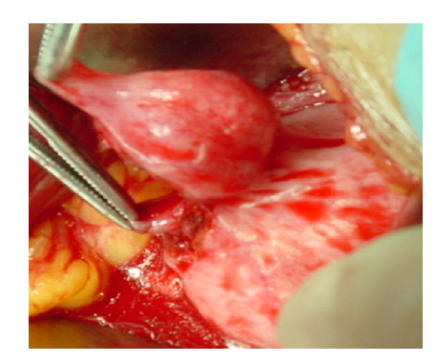
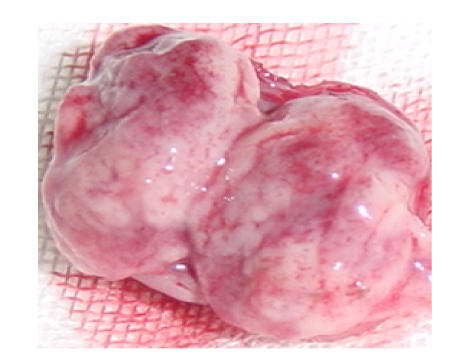
All of the 6 cases underwent surgical operation. Partial cystectomy was performed in 4 cases (1 case’s blood pressure fluctuated during the transurethral resection of the tumor, then partial cystectomy was performed) (Fig.1), while excavation was performed on the other 2 cases (Fig.2).
Fig. 1.
Operative view: the mass suited in submucosal
Fig. 2.
Postoperative specimen: the mass showed pink and inhomogeneity
RESULTS
In 4 cases that had a history of paroxysmal hypertension in preoperation, their blood pressure decreased from (180±10)/(90±15) mmHg to (140±10)/(75±5) mmHg after operation. In 3 cases that suffered from hypertension during preoperative urination, their blood pressure did not fluctuate during postoperative urination. Two cases’ blood pressure fluctuated during operation, but was controlled after management, and they were pathologically diagnosed as pheochromocytoma postoperatively, 5 cases were followed up, who did not have relapse or malignancy.
DISCUSSIONS
Urinary bladder pheochromocytoma is similar to adrenal pheochromocytoma, most of which can secrete catecholamines. They usually present two symptoms of the pheochromocytoma and bladder tumors, which are continuous or paroxysmal, and are especially associated with urination and hematuria (Walsh et al., 1998). In recent years, as we know more and more about the disease, misdiagnosis decreased apparently, although asymptomatic bladder pheochromocytoma is almost impossible to diagnose preoperatively. Main symptoms: during filling of bladder, the cases present tachycardia, paleness, headache, sweating and hypertension; during of urination, the symptoms are most prominent; after urination, the symptoms are gradually relieved. The cases may have difficulty urinating when the tumor is in trigone and if the cases urinate with straining, hypertension may be diagnosed easily (Wu, 2003). Of the 6 cases, 4 presented typical symptoms (66.67%). Pressing on the abdomen or bimanual examination may induce similar symptoms sometimes, 1 of the 6 cases presented the symptoms during bimanual examination and the tumor was detected by B-ultrasound. About 60% cases presented hemoturia, most of which are microscopic hematuria. In our group, 2 cases presented gross hematuria, 1 of whom was associated with hypertension, the other one was not. One case in our group was found during asymptomatic physical examination.
Preoperative location and qualitative analysis are very important in confirming the diagnosis. B-ultrasound, CT, and cystoscopy are utilized to locate the tumors. The tumors in B-ultrasound appeared as a submucosal homogeneous mass, having clear outline, continuous mucosa, and abundant blood. CT can show the relationship between the mass and the bladder mucosa, muscular and peri-tissue (Seki et al., 2001). Cystoscopy is more important in locating and qualitative diagnosis (Karpman et al., 2000). The blood pressure fluctuates because of the irrigation of the flush water and the sheath, which is determinative for the diagnosis. Some people suggested that to confirm the diagnosis preoperatively, we can irrigate the mass during cystoscopy; if the blood pressure fluctuates we can confirm the diagnosis. But we think that if there are no necessary medicines and instruments for salvage, we should not irrigate the mass repeatedly in case there is danger. The tumors in cystoscopy appear as globular submucosa mass protruding into the bladder, that has smooth surface, continuous mucosa, and abundant blood. In the group, blood pressure fluctuated in 3 cases during cystoscopy, so if you suspect pheochromocytoma of bladder, you should control the speed of flush water and turn the sheath slowly to reduce the irrigation to prevent the blood pressure from fluctuating greatly. We take negative attitude on cystoscope biopsy, because its positive rate is very low, bleeds easily and induces the blood pressure to fluctuate. Methyliodobenzylguanidine (MIBG) resembles norepinephrine in its molecular structure and can be taken up by the pheochromocytoma issue. It has been used in diagnosing the pheochromocytoma extensively, especially in the extra-adrenal pheochromocytoma. It is accurate for localizing a pheochromocytoma and has a specificity close to 100% (Ma et al., 1996). Measurements 24-h urine excretion of catecholamines and their metabolites are available in its qualitative screening (Onishi et al., 2003). With improvement of the measurement, its accurate rate continues increasing, which is more significant during attack. Converting enzyme lack in the extra-adrenal pheochromocytoma which can transform norepinephrine into epinephrine, so the bladder pheochromocytoma mainly excretes norepinephrine and it is increased in the urine prominently. So the test of the norepinephrine before and after 3 h of urination is valuable for the diagnosis.
The most effective management is surgical resection. Preoperative confirmed diagnosis and adequate preparation are very important to make the surgery safe (Naqiyah et al., 2005). Although the surgery difficulty in bladder pheochromocytoma and the intraoperative changes are not as prominent as adrenal pheochromocytoma, the preoperative preparation, intraoperative and postoperative treatment cannot be simplified, especially in the cases whose blood pressure fluctuates during urination. The cases began to take phenoxybenzamine 30~45 mg/d two weeks before operation, if the blood pressure cannot be controlled, calcium channel blockers can be added which block the calcium from entering into pheochromocytoma to inhibit the release of catecholamine. When the cases present tachycardia, β-blockade (propranolol) can be added. It was reported that some cases underwent transurethral resection (TUR) of bladder tumors or laparoscopic partial cystectomy (Baima et al., 2000), but we mainly performed open operation. There are three reasons: (1) Transurethral resection (TUR) can irrigate the tumors to induce the blood pressure to fluctuate, to increase the dangers and it is very difficult to control its depth and extent. In this group 1 case’s blood pressure fluctuated during the transurethral resection of the tumor, then partial cystectomy was performed. (2) Pheochromocytoma is easy to recur if the tumor cannot be resected completely. There are clear borders between the normal bladder organism and most of the pheochromocytoma, but the muscular tissues close to the tumor are often destroyed, so if the tumor can be resected completely, it is easy to recur. (3) The proportion of malignant extra-adrenal pheochromocytoma is higher by 30% than that of adrenal pheochromocytoma, so we should resect the tumor and its peri-tissue completely. In our group the 6 cases are all benign; none recurred in our follow-up.
References
- 1.Baima C, Casetta G, Vella R, Tizzani A. Bladder pheochromocytoma: a 3-year follow-up after transurethral resection (TURB) Urol Int. 2000;65(3):176–178. doi: 10.1159/000064868. [DOI] [PubMed] [Google Scholar]
- 2.Karpman E, Zvara P, Stoppacher R, Jackson TL. Pheochromocytoma of urinary bladder: update on new diagnostic modalities plus case report. Ann Urol. 2000;34:113–119. [PubMed] [Google Scholar]
- 3.Ma JX, Zhu RS, Yu JF, Ding CD, Jing CQ. The value of diagnosis of aberrant and (or) malignant pheochromocytoma with 131I-MIBG imaging. Chinese Journal of Nuclear Medicine. 1996;16:101–102. [Google Scholar]
- 4.Naqiyah I, Dohaizak M, Meah FA, Nazri MJ, Sundra M, Amram AR. Pheochromocytoma of the urinary bladder. Singapore Med J. 2005;46(7):344–346. [PubMed] [Google Scholar]
- 5.Onishi T, Sakata Y, Yonemura S, Suqimura Y. Pheochromocytoma of urinary bladder without typical symptoms. Int J Urol. 2003;10(7):398–400. doi: 10.1046/j.1442-2042.2003.00645.x. [DOI] [PubMed] [Google Scholar]
- 6.Seki N, Mukai S, Gamachi A, Migita T, Maeda K, Ogata N. A case of bladder pheochromocytoma. Urol Int. 2001;66(1):57–60. doi: 10.1159/000056569. [DOI] [PubMed] [Google Scholar]
- 7.Walsh PC, Petik AB, Vanghan ED. Capbell’s Urology. 7th Ed. Philadelphia, Sauders: 1998. [Google Scholar]
- 8.Wu JP. Wujieping’s Urology. 1st Ed. Ji’nan: Shandong Science and Technology Press; 2003. pp. 987–989. [Google Scholar]