Abstract
Objective: To compare the effects of epidural anesthesia with 1.5% lidocaine and 0.5% ropivacaine on propofol requirements, the time to loss of consciousness (LOC), effect-site propofol concentrations, and the hemodynamic variables during induction of general anesthesia guided by bispectral index (BIS) were studied. Methods: Forty-five patients were divided into three groups to receive epidurally administered saline (Group S), 1.5% (w/w) lidocaine (Group L), or 0.5% (w/w) ropivacaine (Group R). Propofol infusion was started to produce blood concentration of 4 μg/ml. Once the BIS value reached 40~50, endotracheal intubation was facilitated by 0.1 mg/kg vecuronium. Measurements included the time to LOC, effect-site propofol concentrations, total propofol dose, mean arterial blood pressure (MABP), and heart rate (HR) at different study time points. Results: During induction of anesthesia, both Groups L and R were similar for the time to LOC, effect-site propofol concentrations, total propofol dose, MABP, HR, and BIS. The total doses of propofol administered until 1 min post-intubation were significantly less in patients of Groups R and L compared with Group S. MABP and HR were significantly lower following propofol induction compared with baseline values in the three groups, or MABP was significantly increased following intubation as compared with that prior to intubation in Group S but not in Groups R and L while HR was significantly increased following intubation in the three groups. Conclusion: Epidural anesthesia with 1.5% lidocaine and 0.5% ropivacaine has similar effects on the time to LOC, effect-site propofol concentrations, total propofol dose, and the hemodynamic variables during induction of general anesthesia.
Keywords: Propofol, Lidocaine, Ropivacaine, Epidural anethesia, Bispectral index
INTRODUCTION
Combined epidural/general anesthesia technique has widely been used in major abdominal and thoracic surgery for decades. Our clinical experience is that there are reduced general anesthetics requirements during surgery when the two techniques are combined. Previous studies have sought to explore the effects of epidural anesthesia on general anesthesia and have demonstrated that epidural lidocaine (Lu et al., 2005) or bupivacaine (Agarwal et al., 2004) or ropivacaine (Kanata et al., 2006) reduced the requirements of volatile (Lu et al., 2005) or i.v. (Agarwal et al., 2004; Kanata et al., 2006) anesthetics in upper or lower abdominal surgery. Ishiyama et al.(2005) recently reported that epidural ropivacaine anesthesia decreased the bispectral index (BIS) during the awake phase and during general anesthesia. A new report by Gaughen and Durieux (2006) demonstrated that inadvertent overdose of i.v. lidocaine in a patient monitored with BIS. BIS decreased to 0 for 15 min, indicating that lidocaine and sevoflurance interact to decrease BIS. Laryngoscopy and tracheal intubation are thought to be the strongest noxious stimuli during the course of general anesthesia and are often associated with hemodynamic changes including tachycardia, hypertension and increases in the plasma concentration of catecholamines (Shribman et al., 1987; Achola et al., 1988). Nakatani et al.(2005) investigated hemodynamic changes following induction of anesthesia with propofol during tracheal intubation with or without epidural anesthesia and found that epidural anesthesia did not produce profound hypotentension following induction of anesthesia and produced a reduction in the hemodynamic response to tracheal intubation during a target controlled infusion of propofol.
In the present study, we compared the effects of epidural anesthesia using 1.5% (w/w) lidocaine and 0.5% (w/w) ropivacaine on propofol requirements, the time to loss of consciousness (LOC), predicted propofol concentrations, and hemodynamic variables during the induction of general anesthesia. We compared these two solutions because they are often used for upper abdomen epidural anesthesia during surgery in our institution and have approximately a 0.3 ratio, according to the results reported by Liu (1998) and Arakawa et al.(2003), these two anesthesia solutions should provide the same analgesic effect. As in previous studies (Ishiyama et al., 2005; Kearse et al., 1998), we used the BIS as a sensitive measure of drug hypnotic effect. The BIS has recently been introduced as an estimation of anesthetic effect. According to the results of previous clinical studies (Glass et al., 1997; Katoh et al., 1998; Kreuer et al., 2006), BIS could indicate adequate depth of anesthesia during surgery.
MATERIALS AND METHODS
After obtaining approval from the Human Investigation Committee of the First Affiliated Hospital, School of Medicine, Zhejiang University and informed written consent from all the patients, we studied 45 patients classified as American Society of Anesthesiologists physical status I or II undergoing elective surgery on the upper abdomen. Patients who were taking regular medication, or had a history of diabetes, hypertension, neuromuscular disease or bleeding diathesis or hypersensitivity to amide local anesthetics previous, or had lumber surgery were excluded. No patients had any sign of autonomic dysfunction or cardiovascular disease as detected by routine clinical laboratory tests.
All patients did not receive any premedication. In the operating room, one i.v. cannula was inserted into a large forearm vein for infusion of propofol only and the other in the contralateral arm for infusion of fluid and other anesthetics. A radial artery catheter was inserted for continuous measurement of arterial blood pressure. After i.v. prehydration with 500 ml of lactated Ringer’s solution (Pharmacia, Baxter, Shanghai, China), patients were placed in the flexed lateral position, the skin, subcutaneous tissue, and supraspinous ligament were anesthetized with 2 ml of 1% (w/w) lidocaine. The epidural space was identified with the loss of resistance to air technique at the T9~T10. Every puncture was performed with a 16-gauge Tuohy epidural needle (Pharmacia, Haitian, Zhejiang, China). A multiorifice epidural catheter was advanced 3 cm in a cephalad direction into epidural space. The catheter was aspirated to exclude intrathecal or i.v. placement and then secured. Following placement of the epidural catheter a test dose of 3 ml of 1% (w/w) lidocaine was given to exclude intrathecal position. The patient was then returned to the supine position.
Participants were randomly allocated into one of three groups using a random number table to receive epidural saline (Group S), 1.5% (w/w) lidocaine (Group L), or 0.5% (w/w) ropivacaine (Group R) (Pharmacia, AstraZeneca, Germany) with propofol (Pharmacia, AstraZeneca, Germany) general anesthesia. They received one of the above solution 10 ml (5 ml each time at interval of 3 min) through the epidural catheter. Fifteen minutes after injection, the upper and lower levels of loss of pinprick sensations were determined using a short beveled 25-gauge needle in the midclavicular line bilaterally. Motor strength was assessed in both legs using the modified Bromage scale: 0=able to perform a full straight leg raise over the bed for 5 s, 1=unable to perform the leg raise but can flex the leg on the knee articulation, 2=unable to flex the knee but can flex the ankle articulation, 3=complete motor blockade. Then a target-controlled infusion (TCI) of propofol was administered using the Diprifusor (software version 2; AstraZeneca, London, UK), which contains the Marsh pharmacokinetic model. The propofol infusion was set to produce a blood concentration of 4 μg/ml. Once the BIS value reached 40~50, endotracheal intubation was facilitated by 0.1 mg/kg vecuronium (Pharmacia, Xianju, Zhejiang, China). Ventilation was controlled manually using an anesthesia circuit and a facemask with oxygen 100% to maintain an end-tidal carbon dioxide concentration of 30~40 mmHg (4~5.3 kPa). After intubation, the target concentration of propofol was titrated to maintained BIS of 40~50. All the anesthetic procedures were conducted by an anesthetist who was blinded to the study group.
Monitoring included pulse oximetry (SpO2), end-tidal carbon dioxide concentration (EtCO2), electrocardiography (ECG), invasive arterial blood pressure, heart rate (HR), which were displayed on a multifunction monitor (Datex-Ohmeda, Hoevelaken, the Netherlands). BIS was monitored using a BIS sensor (Aspect, Medical System, Newtown, MA, USA) applied to the forehead as described by the manufacturer (BIS monitor Model A-2000™, Aspect Medical System, Natick, MA, USA). Six milligrams ephedrine was injected i.v. whenever there was a decrease in the systolic blood pressure of more than 30% of the pre-anesthetic value, or the systolic blood pressure fell to below 90 mmHg. Bradycardia (<55 beats/min) was treated by administering 0.5 mg of atropine i.v. During the study we recorded the time to LOC, effect-site propofol concentrations, and total propofol doses. Mean arterial blood pressure (MABP), HR and BIS were also recorded at the following study periods: T 1=baseline, T 2=15 min after the epidural injection, T 3=loss of consciousness, T 4=before laryngoscopy for intubation, T 5=1 min post-intubation.
Assuming the epidural administration of ropivacaine will reduce the requirement of propofol by 30%, power analysis with α=0.05, β=0.8, showed that we would need to study 13 patients in each group. To exclude any dropouts, we included 15 patients in each group. Results are expressed as mean (SD) unless otherwise stated. Analysis of variance (ANOVA) was used to evaluate the differences in patient characteristics, HR, MABP, BIS values, and propofol requirements during induction of anesthesia between the groups. Data at different time within the groups were analyzed with repeated ANOVA measures. Medians (ranges) were analyzed by using Mann-Whitney test, and counts or proportions by using the Fisher’s exact test. A P-value of <0.05 was considered significant. The following software packages were used to performed analyses: Excel 2000 (Microsoft, Redmond, WA) and SPSS 11.0 (SPSS Inc., Chicago, IL).
RESULTS
Study groups were comparable with regard to age, sex, height, and weight. All the patients in Groups R and L while no patients in Group S developed sensory and motor blockade. There were no statistically significant differences with respect to cephalad sensory and motor levels between Groups R and L at 15 min after epidural injection of regional anesthetics.
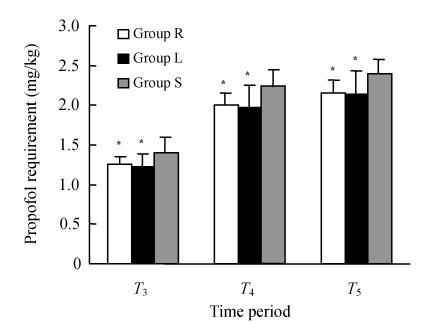
The time to LOC was significantly shorter in Groups R and L compared with Group S: (111±17), (112±14) and (134±22) s, respectively; P<0.05 between Groups R and S, and between Groups L and S (Table 1). None of the patients had awareness, bradycardia, or hypersensitivity reaction to ropivacaine, backache, or dural tap. Effect-site propofol concentration at the time to LOC was significantly lower (P<0.05) in Groups R and L than Group S: (1.44±0.16), (1.48±0.16), and (1.66±0.22) μg/ml, respectively (Table 1). Effect-site propofol concentrations before laryngoscopy for intubation were also significantly lower (P<0.05) in Groups R and L than in Group S: (2.85±0.20), (2.95±0.29), and (3.13±0.16) μg/ml, respectively (Table 1). The total doses of propofol administered until 1 min post-intubation were significantly less in these patients: (2.16±0.15), (2.14±0.29) and (2.39±0.19) mg/kg, respectively; P<0.05 between Groups R and S, and between Groups L and S (Fig.1). There was no statistical difference between Groups R and L regarding the time to LOC, effect-site concentration, and the total doses of propofol during the induction of anesthesia.
Table 1.
Demographic data, the time to LOC, the effect-site propofol concentration at different time during induction of anesthesia, and the upper level of sensory blockade and the level of motor blockade 15 min after epidural injection of ropivacaine in Group R, lidocaine in Group L, and saline in Group S
| Group R | Group L | Group S | |
| N | 15 | 15 | 15 |
| Age (year) | 46±8 | 47±7 | 44±8 |
| Female/male | 8/7 | 8/7 | 7/8 |
| Weight (kg) | 62±6 | 60±8 | 65±8 |
| Height (cm) | 164±7 | 164±6 | 164±7 |
| Cephalad sensory block level | T4 (T4~T6) | T4 (T4~T6) | None |
| Motor block level | 3 (2, 3) | 3 (2, 3) | None |
| Time to LOC (s) | 111±17* | 112±14* | 134±22 |
| Cp (μg/ml) | |||
| T3 | 1.44±0.16* | 1.48±0.16* | 1.66±0.22 |
| T4 | 2.85±0.20* | 2.95±0.29* | 3.13±0.16 |
| T5 | 2.95±0.22* | 3.05±0.29* | 3.24±0.15 |
All values reported as mean±SD, or the median (range), depending on the distribution. C p: Effect-site propofol concentration
P<0.05 vs Group S
Fig. 1.
Propofol requirement for patients in Group R, Group L, and Group S
Data are presented as mean±SD. * P<0.05 vs Group S
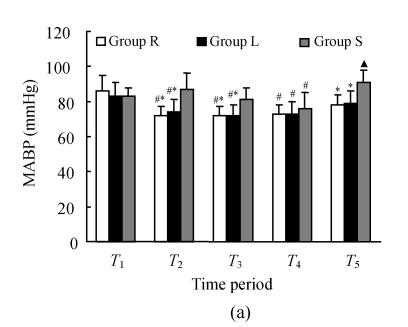
MABP significantly decreased and became lower at 15 min after injection and the time to LOC than that at baseline in Groups R and L but not in Group S. Before laryngoscopy for intubation MABP became significantly lower than at baseline in the three groups. Following intubation, MABP significantly increased as compared with that prior to intubation in Group S but not in Group L or R. Groups R and L differed from Group S in MABP at 15 min after injection, time to LOC, and 1 min post-intubation (Fig.2a).
Fig. 2.
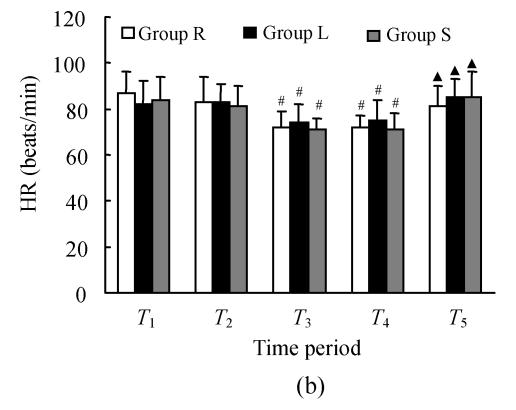
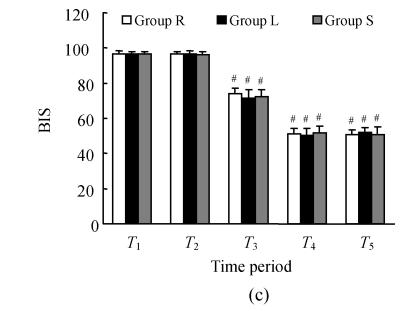
Changes in MABP (a), HR (b), and BIS (c) in patients in Group R, Group L, and Group S
Data are presented as mean±SD. * P<0.05 vs Group S, # P<0.05 vs study period T 1, ▲ P<0.05 vs study period T 4
HR significantly decreased after propofol infusion in patients in every group compared with the baseline values (P<0.05). Following intubation, HR increased in the three groups (P>0.05 vs time period T 4). There were no statistical differences in HR between three groups at any study time periods (Fig.2b).
Additionally, there was no statistical difference between Groups R and L regarding the MABP and HR at any study time period.
BIS values decreased similarly following start of the propofol infusion in the three groups (P<0.05 vs baseline values). There were no differences between the BIS values before and 15 min after epidural injection of local anesthesia/saline (P>0.05). There were also no differences between the three groups in BIS values at time to LOC, before laryngoscopy for intubation, or 1 min post-intubation (Fig.2c).
DISCUSSION
We compared different concentrations of epidural lidocaine (1.5%) and ropivacaine (0.5%) for combination with general anesthesia that were thought to be equipotent (Liu, 1998; Arakawa et al., 2003). The results demonstrated that 0.5% ropivacaine and 1.5% lidocaine administered epidurally had similar effects in the time to LOC, effect-site propofol concentrations, total propofol dose, and the hemodynamic variables during induction of general anesthesia. Patients with established epidural ropivacaine (0.5%) and lidocaine (1.5%) required a shorter time to LOC and had lower effect-site propofol concentrations at the time to LOC compared with epidural saline. It appears that the epidural administration of 0.5% ropivacaine and 1.5% lidocaine leads to the same reduction in general anesthetic requirements to maintain a similar BIS value. These findings confirm that ropivacaine may be more potent than lidocaine.
Previous studies reported conflicting findings concerning the interaction of local and general anesthetics. In 1977, Himes et al.(1977) demonstrated that i.v. lidocaine infusion has a minimal alveolar concentration (MAC)-sparing effect of 10%~28%. In a later study (Senturk et al., 2002), an i.v. anesthetic was used instead of inhalational anesthetics, and lidocaine was administered via the i.m. route. Their results showed that the induction and the maintenance doses of propofol were significantly less in lidocaine group compared with control group and that the hemodynamic response to both induction and intubation was attenuated. They therefore concluded that systemic general anesthesia effects of absorbed local anesthetics play an important role in the reduction dose of general anesthetic. Our results do not support this conclusion. Another study showed that the MAC-sparing effect of epidural anesthesia in combination with general anesthesia is most likely caused by central effects of spinal deafferentation, not to the systemic effects of lidocaine nor to direct neural block of spinal nerves (Hodgson et al., 1999). Inagaki et al.(1994) demonstrated that i.v. lidocaine did not produce sedation while epidural lidocaine did, suggesting that the sedative effect was more likely to be caused by the anesthetic block rather than the effect of the local anesthetic on the central nervous system. Our study found that there was no significant decrease in BIS values compared with the baseline values between the three groups 15 min after epidural injection regional anesthetics/saline and before propofol infusion (Fig.2c), indicating that the direction of ropivacaine and lidocaine via systemic uptake was also unlikely.
Our study used the BIS index as a sensitive and continuous measure of drug hypnotic effect. The BIS monitor is a signal-processing technology that determines the harmonic and phase relations among the various frequencies measured during electroencephalography (Rampil, 1998). BIS index is a combination of 3 parameters derived from analysis of the EEG. The recommended BIS ranges are 65~85 for sedation and 40~60 for general anesthesia. The current version of the BIS index is the result of a search to identify features of the EEG that would reflect the clinical end-points of sedation and hypnosis (Jonsson and Karlsson, 1999). It offers several experimental advantages over other clinical measures of drugs, and it is a nearly instantaneous, continuous, objective and reproducible measure of drug effect. This BIS score has been reported to correlate well with other clinical end-points and may be useful during propofol anesthesia (Irwin et al., 2002). In this study, we titrated the anesthetics to achieve a target BIS of 45~50 and did not find any patient undergoing awareness during general anesthesia.
Propofol induction in patients with and without 1.5% lidocaine or 0.5% ropivacaine epidural anesthesia produced similar degree of bradycardia in the present study. Both 1.5% lidocaine and 0.5% ropivacaine were associated with a reduced increase in MABP post-intubation. Our findings of hemodynamic changes during general anesthesia combined epidural/general anesthesia are consistent with the recent work of Nakatani et al.(2005). The mechanism of hemodynamic changes caused by laryngoscopy and intubation is considered to be somato-visceral reflexes (Hassan et al., 1991), associated with catecholamines releasing from the adrenal gland. Hemodynamic changes resulting from tracheal intubation may be attenuated by epidural blockade itself that reduces sympathetic activity. The efferent sympathetic nerves to the vascular bed are from the spinal between T1 and L2, and those to the adrenal glands from between T6 and L2, and those to the heart from between T1 and T5 (Bonica, 1968). Wattwil et al.(1987) reported that epidural anesthesia produced blockade of T1~L2 nerves and reduced the increase in blood pressure seen following laryngoscopy and intubation. In our study, the efferent sympathetic fibers to the major part of the vascular bed, the adrenal gland and to the heart appeared to be blocked in most patients given epidural ropivacaine and lidocaine.
There are several limitations to this study design. First, despite prestudy power analysis, given the variability in reduction of propofol requirement, 15 were small sample size, and error as a result of inadequate power cannot be disregarded. Second, in this study, we did not insert the epidural catheter the day before surgery and had to wait with induction for anesthesia until the epidurally injected local anesthetics acted sufficiently just for study purpose. In our clinical practice, we start the induction of general anesthesia just after insertion of epidural catheter rather than wait until epidural blockade is sufficient for the effects demonstrated in the study.
In conclusion, epidural anesthesia with 1.5% lidocaine and 0.5% ropivacaine has similar effects on the time to LOC, effect-site propofol concentrations, total propofol dose, and the hemodynamic variables during induction of general anesthesia. Two solutions of epidural anesthesia reduced the propofol dose during the induction of anesthesia using propofol in a target-controlled infusion. Reduced requirement of propofol produces adequate depth of anesthesia during combined epidural-general anesthesia. We also found these two solution epidural anesthesia decreased the hemodynamic responses to laryngoscopy and tracheal intubation, and it is suggested that these effects may be beneficial to patients. These findings suggest that combining with general anesthesia, 1.5% lidocaine is equally effective as 0.5% ropivacaine. It can be used in operations lasting less than 2 h clinically due to its short duration of effect.
Footnotes
Project (No. 419200-584602) supported by the Start Foundation for Introducing Talent of Zhejiang University, China
References
- 1.Achola KJ, Jones MJ, Mitchell RW, Smith G. Effects of beta-adrenoceptor antagonism on the cardiovascular and catecholamine responses to tracheal intubation. Anaesthesia. 1988;43(6):433–436. doi: 10.1111/j.1365-2044.1988.tb06624.x. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal A, Pandey R, Dhiraaj S, Singh PK, Raza M, Pandey CK, Gupta D, Choudhury A, Singh U. The effect of epidural bupivacaine on induction and maintenance doses of propofol (evaluated by bispectral index) and maintenance doses of fentanyl and vecuronium. Anesth Analg. 2004;99(6):1684–1688. doi: 10.1213/01.ANE.0000136422.70531.5A. [DOI] [PubMed] [Google Scholar]
- 3.Arakawa M, Avoyama Y, Ohe Y. Efficacy of 1% ropivacaine at sacral segments in lumbar epidural anesthesia. Reg Anesth Pain Med. 2003;28(3):208–214. doi: 10.1053/rapm.2003.50053. [DOI] [PubMed] [Google Scholar]
- 4.Bonica JJ. Autonomic innervation of the viscera in relation to nerve block. Anesthesiology. 1968;29(4):793–813. doi: 10.1097/00000542-196807000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Gaughen CM, Durieux M. The effect of too much intravenous lidocaine on bispectral index. Anesth Analg. 2006;103(6):1464–1465. doi: 10.1213/01.ane.0000247700.71278.70. [DOI] [PubMed] [Google Scholar]
- 6.Glass PSA, Bloom M, Kearse L, Rosow C, Sebel P, Manberg P. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology. 1997;86(4):836–847. doi: 10.1097/00000542-199704000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Hassan HG, El-Sharkawy TY, Renck H, Mansour G, Fouda A. Hemodynamic and catecholamine responses to laryngoscopy with vs without endotracheal intubation. Acta Anaesthesiol Scand. 1991;35(5):442–447. doi: 10.1111/j.1399-6576.1991.tb03325.x. [DOI] [PubMed] [Google Scholar]
- 8.Himes RS, DiFazio CA, Burney RG. Effects of lidocaine on the anesthetic requirements for nitrous oxide and halothane. Anesthesiology. 1977;47(5):437–440. doi: 10.1097/00000542-197711000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Hodgson P, Liu SS, Gras TW. Does epidural anesthesia have general anesthetic effects? Anesthesiology. 1999;91(6):1687–1692. doi: 10.1097/00000542-199912000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Inagaki Y, Mashimo MT, Kuzukava A, Tsuda Y, Yoshiya T. Epidural lidocaine delays arousal from isoflurane anesthesia. Anesth Analg. 1994;79(2):368–372. doi: 10.1213/00000539-199408000-00030. [DOI] [PubMed] [Google Scholar]
- 11.Irwin MG, Hui TW, Milne SE, Kenny N. Propofol effective concentration 50 and its relationship to bispectral index. Anaesthesia. 2002;57(3):242–248. doi: 10.1046/j.0003-2409.2001.02446.x. [DOI] [PubMed] [Google Scholar]
- 12.Ishiyama T, Kashimoto S, Oguchi T, Yamaguchi T, Okuyama K, Kumazawa T. Epidural ropivacaine anesthesia decreases the bispectral index during the awake phase and sevoflurane general anesthesia. Anesth Analg. 2005;100(3):728–732. doi: 10.1213/01.ANE.0000159868.06847.47. [DOI] [PubMed] [Google Scholar]
- 13.Jonsson EN, Karlsson MO. Xpose—an S-PLUS based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Comput Methods Programs Biomed. 1999;58(1):51–64. doi: 10.1016/S0169-2607(98)00067-4. [DOI] [PubMed] [Google Scholar]
- 14.Kanata K, Sakura S, Kushizaki H, Nakatani T, Saito Y. Effects of epidural anesthesia with 0.2% and 1% ropivacaine on predicted propofol concentrations and bispectral index values at three clinical end points. J Clin Anesth. 2006;18(6):409–414. doi: 10.1016/j.jclinane.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Katoh T, Suzuki A, Ikeda K. Electroencephalographic derivatives as a tool for predicting the depth of sedation and anesthesia induced by sevoflurane. Anesthesiology. 1998;88(3):642–650. doi: 10.1097/00000542-199803000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Kearse LAJr, Rosow C, Zaslavsky A, Connors P, Dershiwitz M, Denman W. Bispectral analysis of electroencephalogram predicts conscious processing of information during propofol sedation and hypnosis. Anesthesiology. 1998;88(1):25–34. doi: 10.1097/00000542-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Kreuer S, Bruhn J, Larsen R, Buchinger H, Wilhelm W. A-line, bispectral index, and estimated effect-site concentrations: a prediction of clinical end-points of anesthesia. Anesth Analg. 2006;102(4):1141–1146. doi: 10.1213/01.ane.0000202385.96653.32. [DOI] [PubMed] [Google Scholar]
- 18.Liu SS. Local Anesthetics and Analgesia. In: Ashburn MA, Rice LJ, editors. The Management of Pain. New York: Churchill Livingstone Inc; 1998. pp. 141–169. [Google Scholar]
- 19.Lu CH, Borel CO, Wu CT, Yeh CC, Jao SW, Chao PC, Wong CS. Combined general-epidural anesthesia decreases the desflurane requirement for equivalent A-line ARX index in colorectal surgery. Acta Anaesthesiol Scand. 2005;49(8):1063–1067. doi: 10.1111/j.1399-6576.2005.00726.x. [DOI] [PubMed] [Google Scholar]
- 20.Nakatani T, Saito Y, Sakura S, Kanata K. Haemodynamic effects of thoracic epidural anesthesia during induction of anesthesia: an investigation into the effects of tracheal intubation during target-controlled infusion of propofol. Anaesthesia. 2005;60(6):530–534. doi: 10.1111/j.1365-2044.2005.04182.x. [DOI] [PubMed] [Google Scholar]
- 21.Rampil IJ. A primer for EEG signal processing in anesthesia. Anesthesiology. 1998;89(4):980–1002. doi: 10.1097/00000542-199810000-00023. [DOI] [PubMed] [Google Scholar]
- 22.Senturk M, Pembeci K, Menda F, Ozkan T, Gucyetmez B, Tugrul M, Camci E, Akpir K. Effects of intramuscular administration of lidocaine or bupivacaine on induction and maintenance doses of propofol evaluated by bispectral index. Br J Anaesth. 2002;89(6):849–852. doi: 10.1093/bja/aef287. [DOI] [PubMed] [Google Scholar]
- 23.Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59(3):295–299. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 24.Wattwil M, Sundberg A, Olsson J, Nordstrom S. Thoracolumbar epidural anaesthesia blocks circulatory response to laryngoscopy and intubation. Acta Anaesthesiol Scand. 1987;31(6):529–531. doi: 10.1111/j.1399-6576.1987.tb02616.x. [DOI] [PubMed] [Google Scholar]